Abstract
Background
The late endosomal LAMTOR complex serves as a convergence point for both the RAF/MEK/ERK and the PI3K/AKT/mTOR pathways. Interestingly, both of these signalling cascades play a significant role in the aetiology of breast cancer. Our aim was to address the possible role of genetic polymorphisms in LAMTOR2 and LAMTOR3 as genetic risk factors for breast cancer.
Methodology/Results
We sequenced the exons and exon–intron boundaries of LAMTOR2 (p14) and LAMTOR3 (MP1) in 50 prospectively collected pairs of cancerous tissue and blood samples from breast cancer patients and compared their genetic variability. We found one single nucleotide polymorphism (SNP) in LAMTOR2 (rs7541) and two SNPs in LAMTOR3 (rs2298735 and rs148972953) in both tumour and blood samples, but no somatic mutations in cancerous tissues. In addition, we genotyped all three SNPs in 296 samples from the Risk Prediction of Breast Cancer Metastasis Study and found evidence of a genetic association between rs148972953 and oestrogen (ER) and progesterone receptor negative status (PR) (ER: OR = 3.60 (1.15–11.28); PR: OR = 4.27 (1.43–12.72)). However, when we additionally genotyped rs148972953 in the MARIE study including 2,715 breast cancer cases and 5,216 controls, we observed neither a difference in genotype frequencies between patients and controls nor was the SNP associated with ER or PR. Finally, all three SNPs were equally frequent in breast cancer samples and female participants (n = 640) of the population-based SAPHIR Study.
Conclusions
The identified polymorphisms in LAMTOR2 and LAMTOR3 do not seem to play a relevant role in breast cancer. Our work does not exclude a role of other not yet identified SNPs or that the here annotated polymorphism may in fact play a relevant role in other diseases. Our results underscore the importance of replication in association studies.
Introduction
Scaffold proteins were originally identified in yeast and are now recognized to contribute to the specificity of MEK/ERK pathways in mammalian cells. LAMTOR3 (MP1) was identified in a yeast two-hybrid screen as a specific binding partner of MEK1 [1], that is recruited to late endosomes by the adaptor protein LAMTOR2 (p14) [2]. MP1 and p14 are structurally almost identical and form a very stable heterodimeric complex that is required for ERK activation on endosomes [3], [4]. Using conditional gene disruption of p14, it was previously shown that the p14/MP1-MEK1 signalling complex regulates late endosomal traffic, EGFR degradation and cellular proliferation [5]. This function is essential for early embryogenesis and during tissue homeostasis as revealed by epidermis-specific deletion of p14 [5]. Taken together, endosomal p14/MP1-MEK1 signalling has a specific and essential function in vivo: it contributes to the regulation of late endosomal traffic by extra-cellular signals, that in turn is required to maintain tissue homeostasis.
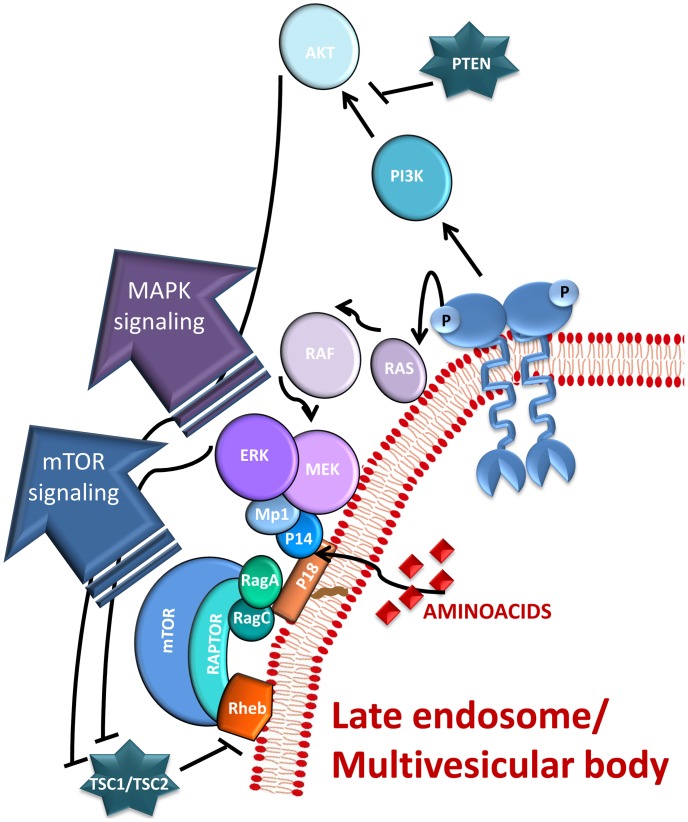
Anchorage of the p14/MP1/MAP kinase pathway to late endosomes is mediated by a small lipid raft adaptor called LAMTOR1 (p18), which directly binds endosomal lipids [6]. The trimeric complex p18/p14/MP1 was recently shown to mediate the translocation of mTORC1 to lysosomal membranes, a critical event in amino acid signalling to mTORC1 [7]. The mTORC1 kinase promotes growth in response to growth factors, energy levels, and amino acids, and its activity is often deregulated in disease conditions. In brief, these data highlight the role of the endosomal scaffold complex p18/p14/Mp1 as a convergence point of signalling pathways controlling proliferation (Figure 1).
Figure 1. The LAMTOR complex as a convergence point of MAPK and mTORC1 pathways (Schematic overview).
Internalized activated receptors keep their ability to signal while they traffic through the endocitic compartment. The arrival at late endosomes/multivesicular bodies of the activated receptor and the detection of aminoacids in the lumen of the organelle, trigger a cascade of phosphorylation events leading to the local activation of both mTORC1 and ERK1/2. The p18/Mp1/p14 complex, also known as the LAMTOR complex was shown to function as a convergence point for both pathways. Both signaling cascades were simplified for didactic reasons.
Progression, proliferation, and hormone independent growth of breast cancer cells is dependent on MAP kinase (ERK) activity [8]. Furthermore, there are consistent reports that primary breast tumors and tissues display elevated expression and activity levels of ERK [9]. In most breast cancers, ERK hyper-activation is due to over-expression and/or constitutive activation of upstream regulators like ErbB2, c-Src or GrB2 [10], [11], [12]. Sustained ERK1/2 signalling in cooperation with transforming growth factor ß (TGFß) activation promote epithelial mesenchymal transition (EMT) and increase invasiveness and metastatic potential of cultured mammary epithelial cells [13]. In brief, ERK activation induces matrix metalloproteinases that degrade collagen, it can inactivate integrin-meditated cell adhesion and activates the myosin light chain thereby eliciting cell migration. Importantly, the Ets-1 transcription factors are key ERK substrates that have been shown to induce EMT and invasiveness in a number of breast cancer cell lines [14], [15]. Several anti-cancer therapies result in the induction of the Raf/MEK/ERK pathway that may provide a survival signal for the tumour, thereby potentiating resistance to treatment. For example, ERK1/2 phosphorylates Ser118 of oestrogen receptor alpha, providing a mechanism by which the oestrogen receptor can be activated in a ligand independent manner [16].
The PI3K/AKT signalling cascade is another major player in cancer progression. Mutations in the PI3K subunit p110 are found in roughly 25% of breast cancers [17], [18]. Furthermore, loss of the tumour suppressor protein PTEN has been directly implicated in hereditary breast cancer [19]. Both the RAF/MEK/ERK and the PI3K/AKT pathways modulate several key apoptotic players thereby transducing a survival signal. The ERK pathway regulates BcL-2, Bad, Mcl-1, Bim, Survivin and Caspase 9 [20], [21], [22]. The PI3K/AKT pathway phosphorylates Bim, Bad, XIAP and p21 [23], [24], [25].
It has been recently shown that treatment of breast cancer cells with MEK or mTOR inhibitors and either Doxorubicin or Tamoxifen results in a synergistic response that highlights the advantages of combining classical chemotherapy with targeted adjuvant treatments [19]. For example, Tamoxifen resistant breast cancer cells with overexpressed/activated v-akt murine thymoma viral oncogene homolog (AKT) or lack of phosphatase and tensin homologue (PTEN) may benefit from Rapamycin treatment, a highly specific mTOR inhibitor. In addition, the complementary use of RAF/MEK/ERK inhibitors may provide an added value in the treatment of this type of tumours since ERK is known to phosphorylate TSC2. The TSC1/TSC2 complex, also known as the tuberous sclerosis complex, controls the small G-protein Rheb through its GAP activity, thereby functioning as a critical negative regulator of mTORC1.
Interestingly, in 2007, Conrad et al. submitted a patent on LAMTOR3 (Mp1) as a diagnostic and therapeutic target for breast cancer treatment and prevention (United States patent Application No. US 2007/0172843 A1; International publication nr. W = 2007/033118 A2). In addition, a recent publication from the same group reports that LAMTOR3 (Mp1) is required for the survival of estrogen receptor positive breast cancer cell lines [26].
Taking into consideration the above report and recent findings identifying the LAMTOR complex as a convergence point for both the ERK and mTORC1 pathways, we aimed to investigate the potential role of mutations in LAMTOR3 and LAMTOR2 in the aetiology of breast cancer.
Materials and Methods
Ethics Statement
This study was approved by the ethics committee of the Innsbruck Medical University (study code UN3377).
Patient Characteristics at the Screening Stage
For mutation screening, tissue samples of 50 consecutive breast cancer patients were prospectively collected at the Innsbruck Medical University starting in July 2009. Patients aged 18 or older, who had signed an informed consent, were consecutively included in the study. The following clinical parameters were collected: age; menopausal status; tumour histology; tumour size; tumour grade; lymph node status; oestrogen receptor status; progesterone receptor status; HER2 (human epidermal growth factor receptor 2) status; and presence of metastasis.
Sequencing of Exons in LAMTOR2 (p14) and LAMTOR3 (MP1)
Genomic DNA was extracted from frozen tumour tissue or from peripheral blood collected on EDTA on a BioRobot EZ1 advanced Workstation with the EZ1 DNA tissue or blood kit (QIAGEN, Hilden, Germany) and quantified with a NanoDrop spectrophotometer (Thermo Fisher Scientific Inc., Waltham, MA). Amplification and sequencing primes were designed with Visual OMP (DNA Software, Inc., Ann Arbor, MI).
All four exons of the LAMTOR2 gene (following the nomenclature of transcript ENST00000368305, Ensembl Release 52; www.ensembl.org) were amplified in 2 PCR reactions and sequenced with 8 primers (Table S1). An overview of the amplification and sequencing strategy of the exons within LAMTOR2 is given in Figure S1.
Five out of seven exons of the LAMTOR3 gene (following the nomenclature of transcript ENST00000226522, Ensembl Release 52; www.ensembl.org) were amplified in 4 PCR reactions and sequenced with 14 primers (Table S2). The genomic region including Exon 1 and Exon 2 could be amplified in one PCR reaction. Exon 3, Exon 4, Exon 5 and Exon 6 were each very short and had long intronic stretches between each other, so that none of these exons could be targeted with another PCR reaction. Exon 3 codes for the first alpha helix of LAMTOR3, is only 35bp long, lacks putative protein binding sites and shows low amino acid conservation [4]; therefore, it was not of particular structural interest and was excluded from sequencing. Exon 6 codes for two of the central β-strands of LAMTOR3. Non-synonymous mutations in Exon 6 (64bp) are assumed to have two possible consequences: if the properties of the amino acids were maintained, LAMTOR3 would fold correctly and the protein would be as functional as the wild type. If the amino acid properties significantly changed, the correct assembly of the central β-sheet would be impaired, thereby completely abolishing LAMTOR3 function, with the consequence that LAMTOR3 molecules would be degraded by quality control mechanisms. If such mutations existed, they would lead to embryonic lethality as was observed in LAMTOR2 knockout mice [5]. Therefore, we also excluded Exon 6 from sequencing. An overview of the amplification and sequencing strategy of the selected exons within LAMTOR3 is given in Figure S2.
All fragments except for MP1-1 were amplified in a total reaction volume of 25 µl, containing 70–130 ng of DNA, 0.5 µl of Herculase II Fusion DNA Polymerase (Stratagene, La Jolla, USA), 5 µl of PCR reaction buffer, 250 µM each dNTP, and 0.25 µM each primer. The reaction cocktails were heated to 95°C (2 min) and then put through 35 amplification cycles: 95°C for 20 s, 55°C for 20 s, and 72°C for 60 sec and a final extension phase at 72°C for 10 min. Fragment MP1-1 was amplified in a total reaction volume of 25 µl, containing 60 ng of DNA, 0.5 µl of KAPA HiFi HotStart DNA Polymerase (KAPA Biosystems, Boston, USA), 5 µl of 5X KAPA HiFi GC Buffer, 0.5 µl KAPA dNTP Mix (10 mM each dNTP), and 0.3 µM each primer. The reaction cocktails were heated to 95°C (5 min) and then put through 30 amplification cycles: 98°C for 20 s, 56.7°C for 15 s, and 72°C for 45 sec and a final extension phase at 72°C for 5 min.
PCR products were purified using QIAvac vacuum manifolds (QIAGEN) and eluted in 50µl distilled water according to the manufacturer’s protocol. For cycle sequencing, 3 µl of purified PCR product were combined with the sequencing master mix (containing 2 µl BigDye Terminator v1.1 Cycle Sequencing RR mix [AB], 2 µl Sequencing Buffer [AB], 0.3 µM primer, and distilled water up to 10 µl) and cycled (after a first denaturation step of 96°C, 2 min) for 30 cycles of 30 s at 96°C, 20 s at 55°C, and 1 min at 60°C. Purification of cycle-sequencing products with Sephadex (GE Healthcare) was performed according to the procedure described in Brandstätter et al. [27].
Electrophoretic separation was carried out on an ABI3130xl capillary sequencer with POP-7 and a 36 cm capillary array.
Risk Prediction of Breast Cancer Metastasis Study
For studying the effects of the identified variants in a breast cancer sample, one single nucleotide polymorphism (SNP) in LAMTOR2 (rs7541) and two SNPs in LAMTOR3 (rs2298735 and rs148972953) were genotyped using a TaqMan® SNP Genotyping Assay on a 7900HT Fast Real-Time PCR System (Applied Biosystems, Foster City, CA) in 296 samples of the Risk Prediction of Breast Cancer Metastasis Study. This study is a multicenter study including prospectively collected breast cancer samples from the cities Innsbruck (Austria), Salzburg (Austria) and Meran (Italy). Patients aged 18 or older, who had signed an informed consent, were consecutively included in the study. Detailed information on tumour characteristics (e.g., hormone receptor status) and treatment (e.g. chemotherapy, endocrine therapy, and radiotherapy) were collected using clinical and pathological records. The Risk Prediction of Breast Cancer Metastasis Study was approved by the ethics committee of the Innsbruck Medical University (study code AM330a). The genotyping success rates were 97.3% for rs7541, 99.3% for rs2298735, and 97.3% for rs148972953.
Replication: MARIE Study
For a more detailed analysis, the SNP rs148972953 was genotyped using a TaqMan® SNP Genotyping Assay on a 7900HT Fast Real-Time PCR System (Applied Biosystems, Foster City, CA) in 7,931 samples of the MARIE Study. The MARIE (Mammary carcinoma Risk factor Investigation) study population comprises breast cancer patients who participated in a population-based case-control study conducted in two German study regions (Hamburg and Rhine-Neckar-Karlsruhe) [28]. The study was approved by the ethics committees of the University of Heidelberg and the University of Hamburg. Patients were eligible if they had a histologically confirmed primary invasive (stage I-IV) or in situ breast tumour, were 50 to 74 years old, resident in the study region, and German-speaking. Of the 6,114 eligible patients, 3,919 (64.1%) participated in the study. Detailed information on tumour characteristics (e.g., hormone receptor status) and treatment (e.g. chemotherapy, endocrine therapy, and radiotherapy) were collected using clinical and pathological records/attending physicians. Two controls per case were randomly selected from population registries frequency-matched by year of birth and study region. Of the 17,093 eligible controls, 7,421 (43.3%) participated in the study. For the present analyses, 2,767 cases and 5,324 controls were included, excluding subjects without blood samples and genotype information. Information on socio-economic and lifestyle factors was collected at baseline by means of a personal interview. An overview of all three breast cancer populations is given in Table 1. The genotyping success rates were 98.1% for cases, and 98.0% for controls. The fraction of samples that were genotyped twice for quality assurance were 9.5%, the genotyping discordance rate was 0%. Therefore genotype information was available for 2,715 cases and 5,216 controls.
Table 1. Characteristics of the breast cancer studies.
| Sequencing | RPBCMS | MARIE cases | |
| n | 50 | 296 | 2,715 |
| Age at diagnosis (years) | 58.3±13.4 | 59.7±13.3 | 62.4±6.1 |
| Percentage of premenopausal women | 31.3% | 34.3% | 9.2% |
| Histology | |||
| IDC | 74.0% | 75.0% | 66.3% |
| ILC | 16.0% | 15.5% | 19.9% |
| DCIS | 1.7% | 6.3% | |
| other | 10.0% | 7.8% | 7.3% |
| Tumour size | |||
| with the diameter lessthan 2 cm | 54.0% | 58.0% | 51.5% |
| with the diameter morethan 2 cm | 46.0% | 42.0% | 42.2% |
| Tumour grade | |||
| I | 4.0% | 8.0% | 17.4% |
| II | 78.0% | 69.5% | 48.1% |
| III | 18.0% | 22.5% | 28.1% |
| Oestrogen receptor status | |||
| positive | 84.0% | 86.3% | 79.0% |
| negative | 16.0% | 13.7% | 21.0% |
| Progesterone receptor status | |||
| positive | 76.0% | 75.2% | 67.0% |
| negative | 24.0% | 24.8% | 33.0% |
Notes: the age at diagnosis is indicated as mean value ± standard deviation.
Abbreviations:
IDC… infiltrative ductal carcinoma.
ILC… infiltrative lobular carcinoma.
DCIS… ductal carcinoma in situ.
RPBCMS… Risk Prediction of Breast Cancer Metastasis Study.
SNP Frequencies in a Healthy Working Population: SAPHIR Study
For studying the frequency of the identified variants in a healthy working population, one SNP in LAMTOR2 (rs7541) and two SNPs in LAMTOR3 (rs2298735 and rs148972953) were genotyped using a TaqMan® SNP Genotyping Assay on a 7900HT Fast Real-Time PCR System (Applied Biosystems, Foster City, CA) in female participants of the SAPHIR Study. The Salzburg Atherosclerosis Prevention Program in Subjects at High Individual Risk (SAPHIR) is an observational study conducted in the years 1999–2002 involving 1,770 healthy unrelated subjects: 663 females from 39 to 67 years of age and 1,107 males from 39 to 66 years of age [29]. Study participants were recruited by health screening programs in large companies in and around the city of Salzburg. DNA was available for 640 female samples. The fraction of samples that were genotyped twice for quality assurance were 4%, the genotyping discordance rate was 0%. The genotyping success rates were 99.1% for rs7541, 97.3% for rs2298735, and 97.2% for rs148972953.
Statistical and Bioinformatic Analysis
The genotype distribution was used to calculate minor allele frequencies and deviations from Hardy-Weinberg equilibrium were evaluated using a Chi-square test. Due to the low minor allele frequency of rs148972953, heterozygous and homozygous minor allele carriers were assessed combined in comparison to major allele carriers. Differences in allele frequencies between carriers and non-carriers of rs148972953 by oestrogen receptor status, progesterone receptor status, metastasis at baseline and metastasis after treatment were calculated by using a Chi-squared test. Odds ratios with a 95% confidence interval were calculated for estimating the relationship between rs148972953 and oestrogen receptor status (ER), progesterone receptor status (PR) and metastasis [30]. Statistical analyses were performed with SPSS (version 19), R (version 2.15.0) and SAS (version 9.2).
Following functional considerations based on the SNP position, the potential effects of the three SNPs were investigated using selected bioinformatic applications [31]. Especially, the SNPs were checked for exonic splicing regulators (ESRs) with F-SNP [32] and miRNA binding sites with Patrocles [33] and mirRBase [34].
Results
Search for Genetic Variability in LAMTOR2 and LAMTOR3
Sequencing of the exons and exon-intron boundaries of both LAMTOR2 and LAMTOR3 revealed three SNPs to occur in a sequencing sample of 50 breast cancer patients, but no novel mutations. One SNP was found in LAMTOR2 (rs7541) and two SNPs within LAMTOR3 (rs2298735 and rs148972953) (Table 2). Our hypothesis that LAMTOR2 and LAMTOR3 gene regions would harbour somatic mutations in tumour tissue was not confirmed; all SNPs that were found were present in both benign (DNA derived from whole blood) and cancerous tissue.
Table 2. Genotype frequencies of the analyzed SNPs by study population.
| LAMTOR2 | LAMTOR3 | ||
| rs7541 | rs2298735 | rs148972953 | |
| Chromosome: Base pair position | 1∶156,025,096 | 4∶100,815,617 | 4∶100,802,946 |
| Located in: | Exon 2 | 5′UTR | 3′UTR |
| Ancestral/derived allele | C/T | T/G | A/G |
| SNP effect | Synonym | – | – |
| GD: AA/Aa/aa: Sequencing | 66.0/28.0/6.0% | 28.0/40.0/32.0% | 92.0/8.0/0.0% |
| GD: AA/Aa/aa: RPBCMS | 75.4/22.2/2.4% | 39.1/45.2/15.7% | 96.5/3.5/0.0% |
| GD: AA/Aa/aa: SAPHIR women | 70.3/27.0/2.7% | 39.5/44.5/16.0% | 96.0/3.9/0.1% |
| GD: AA/Aa/aa: MARIE cases | n.a. | n.a. | 97.1/2.9/0.0% |
| GD: AA/Aa/aa: MARIE controls | n.a. | n.a. | 97.3/2.7/0.0% |
| MAF: Sequencing (n = 50) | 20.0% | 52.0% | 4.0% |
| MAF: RPBCMS (n = 296) | 13.5% | 38.3% | 1.7% |
| MAF: SAPHIR women (n = 640) | 16.2% | 38.2% | 2.1% |
| MAF: MARIE cases (n = 2,715) | n.a. | n.a. | 1.5% |
| MAF: MARIE controls (n = 5,216) | n.a. | n.a. | 1.4% |
| HWE p-value: Sequencing | 0.376 | 0.159 | 0.768 |
| HWE p-value: RPBCMS | 0.387 | 0.466 | 0.764 |
| HWE p-value: SAPHIR women | 0.900 | 0.140 | 0.153 |
| HWE p-value: MARIE cases | n.a. | n.a. | 0.435 |
| HWE p-value: MARIE controls | n.a. | n.a. | 0.316 |
Notes:
Call rates in all study populations were above 98%.
MAF… Minor allele frequency.
HWE… p-value for test for Hardy-Weinberg-Equilibrium (Chi-Square test).
GD… Genotype distribution (in %).
RPBCMS… Risk Prediction of Breast Cancer Metastasis Study.
Bioinformatic Analysis
Bioinformatic analysis indicated that the synonymous SNP rs7541 in exon 2 of LAMTOR2 could possibly affect splicing regulation (predicted by both F-SNP [32] and PupaSuite [35]) by deletion of a splicing silencer element. However, none of the annotated NCBI transcripts actually shows splicing in this region. The SNP rs2298735, which is located in the 5′UTR of LAMTOR3, had a very low functional score in F-SNP, and we also did not find transcription factor binding sites (as predicted with FASTSNP [36]).
Interestingly however, the rare allele of SNP rs148972953 in the 3′UTR of LAMTOR3 abolishes a putative binding site for the miRNA mir-126* (“TAATAATA”) (as analyzed with Patrocles [33] and miRBase [34]). mir-126* and its complement mir-126, which are encoded by intron 7 of the egfl7 gene, have been reported to impair cancer progression through signalling pathways that control tumour cell proliferation, migration, invasion, and survival in a wide variety of cancers [37], [38], [39], [40], [41], [42], [43], especially in breast cancer [44], [45].
Genetic Association Studies and Comparison with Healthy Controls
As our sequencing sample was relatively small (n = 50), and as the SNP rs148972953 in LAMTOR3 had a minor allele frequency (MAF) of 4%, we investigated whether a healthy working population sample would show different genotype distributions than the breast cancer sample. Therefore, we genotyped all three SNPs in female participants of the SAPHIR population (n = 640). The allele and genotype frequencies in SAPHIR women were similar to those in our sequencing sample (p>0.05; Table 2).
For the analysis of genetic association, we combined the samples for sequencing and those in the Risk Prediction of Breast Cancer Metastasis Study since they were collected at the same University Clinic in the same manner. In the combined breast cancer sample, rs148972953 in LAMTOR3 was found to be strongly associated with negative progesterone receptor status (OR = 4.27 (1.43–12.72); Table 3) and with negative oestrogen receptor status of the tumour (OR = 3.60 (1.15–11.28); Table 3).
Table 3. Genetic association of rs148972953 with tumour characteristics (oestrogen and progesterone receptor status and metastases).
| Oestrogen receptor | Progesterone receptor | ||||
| Study population | rs148972953 | positive | negative | positive | negative |
| Sequencing + | Wild-type (GG) | 266 | 41 | 234 | 73 |
| RPBCMS | Carrier (AG or AA) | 9 | 5 | 6 | 8 |
| Combined | p-value | 0.035 | 0.006 | ||
| (n = 321) | OR (95% CI) | 1 | 3.60 (1.15–11.28) | 1 | 4.27 (1.43–12.72) |
| MARIE cases | Wild-type (GG) | 1919 | 504 | 1610 | 809 |
| (n = 2,499) | Carrier (AG or AA) | 58 | 18 | 51 | 25 |
| p-value | 0.543 | 0.920 | |||
| OR (95% CI) | 1.18 (0.69–2.02) | 1 | 0.97 (0.60–1.58) | ||
Notes:
Due to the low minor allele frequency of rs148972953, heterozygous and homozygous mutation allele carriers were assessed combined in comparison to wild-type allele carriers assuming a dominant mode of inheritance.
For this analysis, only samples with complete information on ER, PR and an rs148972953 genotype were taken into consideration.
OR … odds ratio.
95% CI … 95% confidence interval.
RPBCMS… Risk Prediction of Breast Cancer Metastasis Study.
Replication in the MARIE Study
Encouraged by the findings from the combined breast cancer sample and the bioinformatic analyses we performed a replication in the MARIE Study. The minor allele of rs148972953 was not found to show differential association by oestrogen receptor or progesterone receptor status (ER: OR = 1.18 (0.69–2.02); PR: OR = 0.97 (0.60–1.58); Table 3). In addition, cases and controls of the MARIE Study did not differ in the genotype frequency of rs148972953 (Chi-Square Test; p = 0.60).
Based on the results of the bioinformatics analysis, we hypothesized that rs148972953 could be associated with tumour metastasis. However, our assumption was not supported in the MARIE Study. Compared to patients carrying the wildtype of rs148972953 polymorphism, carriers of the minor allele of rs148972953 were neither more likely to have metastasis at baseline (OR = 1.76 (0.62–4.96)) nor were they at higher risk of distant disease-free survival (HR = 0.96 (0.75–1.23)) (Table 4). The genetic status at rs148972953 did not modify the response to primary hormone therapy (overall survival: HR = 0.83 (0.35–2.07); distant disease free survival: HR = 0.96 (0.72–1.29); recurrence-free survival: HR = 1.01 (0.76–1.35)). Carrying the minor allele of rs148972953 was also not associated with the time until tumour relapse (Mann-Whitney test; p = 0.947).
Table 4. Genetic association of rs148972953 with risk of having metastasis in MARIE breast cancer cases.
| Wild-type(GG) | Carrier(AG or AA) | ||
| Metastasis at | Yes | 73 | 4 |
| baseline | No | 2221 | 69 |
| p-value | 0.276 | ||
| OR (95% CI) | 1 | 1.76 (0.62–4.96) | |
| Metastasis after | Yes | 203 | 8 |
| primary treatment | No | 2252 | 66 |
| p-value | 0.435 | ||
| OR (95% CI) | 1 | 1.34 (0.63–2.84) |
Notes:
The analysis was only performed in breast cancer cases of the MARIE Study. At baseline, 2367 patients suffered from a primary invasive breast cancer and 159 patients suffered from in situ breast cancer; those 159 patients were excluded for this analysis. In the Risk Prediction of Breast Cancer Metastasis Study, information on metastasis was either missing in most patients or the follow-up time was too short for the development of metastasis after primary treatment.
OR … odds ratio.
95% CI … 95% confidence interval.
Discussion
Bioinformatic analysis of high-throughput cancer microarrays available on the public domain Oncomine [46], [47] revealed that LAMTOR2 (p14) is significantly up-regulated in breast cancer cells. Interestingly, two independent publications also reported an up-regulation of p14 in invasive ductal breast carcinomas [46], [48]. In addition, LAMTOR3 (Mp1) was also found to be up-regulated in invasive ductal breast carcinomas [49]. Invasive ductal breast carcinoma is the most common type of breast cancer, comprising 70% to 80% of all cases. It commonly spreads to the regional lymph nodes and carries a poor prognosis. Interestingly, LAMTOR3 (Mp1) was also reported to exhibit reduced levels in the stroma of invasive breast carcinoma [50]. The apparently opposing observations may indicate that Mp1 is differentially regulated in stroma and tumour cells. In addition, a recent publication reported that LAMTOR3 (Mp1) was required for the survival of oestrogen receptor positive breast cancer cell lines [26]. Taking into consideration the above data, we hypothesized that LAMTOR components may indeed play a relevant role in breast cancer progression and are not simply innocent bystanders. Changes in intracellular protein levels can depend on variation in the rates of transcription, translation and degradation. In this project, we searched for mutations in the genomic regions of LAMTOR2 and LAMTOR3 that could contribute to the aetiology of breast cancer by altering any of the above mentioned processes.
We initially hypothesized that somatic, cancer-tissue-specific mutations in LAMTOR2 and LAMTOR3 could be associated with breast cancer progression and metastasis. We additionally expected that several rare instead of common variants would be detected and those rare variants were not expected to be already listed in databases. Therefore, we applied a discovery stage by sequencing the exons of LAMTOR2 and LAMTOR3 in 50 cancerous tissues and the corresponding peripheral leukocyte DNA and observed no differences in the identified mutations between the two tissues. The identified mutations were investigated in two different case samples (Risk Prediction of Breast Cancer Metastasis Study and MARIE cases) as well as two different control samples (SAPHIR women and MARIE controls).
Despite the promising results in the initial study, the replication study failed to support an association between the SNP rs148972953 in LAMTOR3 and both oestrogen and progesterone receptor status and metastasis. The present work does not exclude that the observed polymorphisms may play a role in other disease contexts or that other not yet identified polymorphisms in LAMTOR2 and LAMTOR3 may in fact contribute to breast cancer aetiology. We would also like to emphasize that genetic variation is not the only factor contributing to disease progression. Many regulatory aspects, in particular those controlling protein stability, posttranslational modifications and association with binding partners, play a fundamental role in determining how much and how active a protein actually is. As discussed before, previous publications identified the LAMTOR complex as a convergence point of key signalling pathways: MAPK and mTOR. Due to the well established role of both signalling cascades in breast cancer progression, and the recent implication of LAMTOR3 in oestrogen receptor positive breast cancer, we leave open the possibility of therapeutically targeting the complex as previously proposed by others [26].
Although the LAMTOR complex was independently demonstrated to be involved in breast cancer [46], [48], [49], [50], neither LAMTOR2 nor LAMTOR3 came up as hits in genome-wide association studies (GWAS) with any kind of disease or trait as indexed by the catalogue of published GWAS [51]. One reason for this could be that some gene regions are poorly covered by recent SNP arrays; e.g. rs148972953 is currently neither available on any commercial genotyping array nor can it be imputed based on HapMap data. However, the region 4q23, in which LAMTOR3 is located, showed signals of associations with upper aerodigestive tract cancers [52] and oesophageal cancer [53] indicating that the region per se is interesting for cancer. Therefore, future studies including a dense map of SNPs from the LAMTOR complex including the regulatory regions might reveal implications of genetic associations of LAMTOR2 and LAMTOR3 with breast cancer.
The present study constitutes a good example for the necessity and importance of replication in genetic association studies. Small cohorts intrinsically increase the number of false positives that are accepted. Replication in larger populations is therefore fundamental to separate the wheat from the chaff.
Supporting Information
Amplification and sequencing strategy of LAMTOR2.
(DOC)
Amplification and sequencing strategy of LAMTOR3.
(DOC)
Primers used for amplification and sequencing of LAMTOR2.
(DOC)
Primers used for amplification and sequencing of LAMTOR3.
(DOC)
Acknowledgments
We appreciate the help of several colleagues for collecting samples and clinical data: Günter Daxenbichler, Christian Marth, Christine Brantner, Martina Chamson (Department of Obstetrics and Gynaecology, Innsbruck Medical University); Christina Wilhelm (Breast Center Salzburg, Paracelsus Medical University); and Herbert Heidegger (Department of Gynecology and Obstetrics, Hospital Meran).
Funding Statement
The project was supported by the COMET Centre ONCOTYROL (which is funded by BMVIT, BMWFJ, the Tiroler-Zukunftsstiftung and the Styrian Business Promotion Agency), by the Innsbruck Medical University, by the Verein Sanitätsbetrieb Autonome Provinz-Bozen, by the Tiroler-Landeskrankenanstalten-GmbH (TILAK), and by the Sequencing & Genotyping Unit of the Innsbruck Medical University. Work in the Huber laboratory was supported by the FWF (Austria) funded special research program "cell proliferation and cell death in tumors"-SFB021. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Schaeffer HJ, Catling AD, Eblen ST, Collier LS, Krauss A, et al. (1998) MP1: a MEK binding partner that enhances enzymatic activation of the MAP kinase cascade. Science 281: 1668–1671. [DOI] [PubMed] [Google Scholar]
- 2. Wunderlich W, Fialka I, Teis D, Alpi A, Pfeifer A, et al. (2001) A novel 14-kilodalton protein interacts with the mitogen-activated protein kinase scaffold mp1 on a late endosomal/lysosomal compartment. J Cell Biol 152: 765–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Teis D, Wunderlich W, Huber LA (2002) Localization of the MP1-MAPK scaffold complex to endosomes is mediated by p14 and required for signal transduction. Dev Cell 3: 803–814. [DOI] [PubMed] [Google Scholar]
- 4. Kurzbauer R, Teis D, de Araujo ME, Maurer-Stroh S, Eisenhaber F, et al. (2004) Crystal structure of the p14/MP1 scaffolding complex: how a twin couple attaches mitogen-activated protein kinase signaling to late endosomes. Proc Natl Acad Sci U S A 101: 10984–10989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Teis D, Taub N, Kurzbauer R, Hilber D, de Araujo ME, et al. (2006) p14-MP1-MEK1 signaling regulates endosomal traffic and cellular proliferation during tissue homeostasis. J Cell Biol 175: 861–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nada S, Hondo A, Kasai A, Koike M, Saito K, et al. (2009) The novel lipid raft adaptor p18 controls endosome dynamics by anchoring the MEK-ERK pathway to late endosomes. EMBO J 28: 477–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sancak Y, Bar-Peled L, Zoncu R, Markhard AL, Nada S, et al. (2010) Ragulator-Rag complex targets mTORC1 to the lysosomal surface and is necessary for its activation by amino acids. Cell 141: 290–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Atanaskova N, Keshamouni VG, Krueger JS, Schwartz JA, Miller F, et al. (2002) MAP kinase/estrogen receptor cross-talk enhances estrogen-mediated signaling and tumor growth but does not confer tamoxifen resistance. Oncogene 21: 4000–4008. [DOI] [PubMed] [Google Scholar]
- 9. Adeyinka A, Nui Y, Cherlet T, Snell L, Watson PH, et al. (2002) Activated mitogen-activated protein kinase expression during human breast tumorigenesis and breast cancer progression. Clin Cancer Res 8: 1747–1753. [PubMed] [Google Scholar]
- 10. Harari D, Yarden Y (2000) Molecular mechanisms underlying ErbB2/HER2 action in breast cancer. Oncogene 19: 6102–6114. [DOI] [PubMed] [Google Scholar]
- 11. Biscardi JS, Ishizawar RC, Silva CM, Parsons SJ (2000) Tyrosine kinase signalling in breast cancer: epidermal growth factor receptor and c-Src interactions in breast cancer. Breast Cancer Res 2: 203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Malaney S, Daly RJ (2001) The ras signaling pathway in mammary tumorigenesis and metastasis. J Mammary Gland Biol Neoplasia 6: 101–113. [DOI] [PubMed] [Google Scholar]
- 13. Janda E, Lehmann K, Killisch I, Jechlinger M, Herzig M, et al. (2002) Ras and TGF[beta] cooperatively regulate epithelial cell plasticity and metastasis: dissection of Ras signaling pathways. J Cell Biol 156: 299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Prescott JD, Koto KS, Singh M, Gutierrez-Hartmann A (2004) The ETS transcription factor ESE-1 transforms MCF-12A human mammary epithelial cells via a novel cytoplasmic mechanism. Mol Cell Biol 24: 5548–5564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gilles C, Polette M, Birembaut P, Brunner N, Thompson EW (1997) Expression of c-ets-1 mRNA is associated with an invasive, EMT-derived phenotype in breast carcinoma cell lines. Clin Exp Metastasis 15: 519–526. [DOI] [PubMed] [Google Scholar]
- 16. Murphy LC, Weitsman GE, Skliris GP, Teh EM, Li L, et al. (2006) Potential role of estrogen receptor alpha (ERalpha) phosphorylated at Serine118 in human breast cancer in vivo. J Steroid Biochem Mol Biol 102: 139–146. [DOI] [PubMed] [Google Scholar]
- 17. Kang S, Bader AG, Zhao L, Vogt PK (2005) Mutated PI 3-kinases: cancer targets on a silver platter. Cell Cycle 4: 578–581. [DOI] [PubMed] [Google Scholar]
- 18. Hollestelle A, Elstrodt F, Nagel JH, Kallemeijn WW, Schutte M (2007) Phosphatidylinositol-3-OH kinase or RAS pathway mutations in human breast cancer cell lines. Mol Cancer Res 5: 195–201. [DOI] [PubMed] [Google Scholar]
- 19. Steelman LS, Navolanic PM, Franklin RA, Bonati A, Libra M, et al. (2008) Combining chemo-, hormonal and targeted therapies to treat breast cancer (Review). Mol Med Report 1: 139–160. [PubMed] [Google Scholar]
- 20. Troppmair J, Rapp UR (2003) Raf and the road to cell survival: a tale of bad spells, ring bearers and detours. Biochem Pharmacol 66: 1341–1345. [DOI] [PubMed] [Google Scholar]
- 21. Ley R, Balmanno K, Hadfield K, Weston C, Cook SJ (2003) Activation of the ERK1/2 signaling pathway promotes phosphorylation and proteasome-dependent degradation of the BH3-only protein, Bim. J Biol Chem 278: 18811–18816. [DOI] [PubMed] [Google Scholar]
- 22. Domina AM, Vrana JA, Gregory MA, Hann SR, Craig RW (2004) MCL1 is phosphorylated in the PEST region and stabilized upon ERK activation in viable cells, and at additional sites with cytotoxic okadaic acid or taxol. Oncogene 23: 5301–5315. [DOI] [PubMed] [Google Scholar]
- 23. del Peso L, Gonzalez-Garcia M, Page C, Herrera R, Nunez G (1997) Interleukin-3-induced phosphorylation of BAD through the protein kinase Akt. Science 278: 687–689. [DOI] [PubMed] [Google Scholar]
- 24. Gottlieb TM, Leal JF, Seger R, Taya Y, Oren M (2002) Cross-talk between Akt, p53 and Mdm2: possible implications for the regulation of apoptosis. Oncogene 21: 1299–1303. [DOI] [PubMed] [Google Scholar]
- 25. Dan HC, Jiang K, Coppola D, Hamilton A, Nicosia SV, et al. (2004) Phosphatidylinositol-3-OH kinase/AKT and survivin pathways as critical targets for geranylgeranyltransferase I inhibitor-induced apoptosis. Oncogene 23: 706–715. [DOI] [PubMed] [Google Scholar]
- 26. Marina M, Wang L, Conrad SE (2012) The scaffold protein MEK Partner 1 is required for the survival of estrogen receptor positive breast cancer cells. Cell Commun Signal 10: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Brandstätter A, Niederstätter H, Pavlic M, Grubwieser P, Parson W (2007) Generating population data for the EMPOP database - an overview of the mtDNA sequencing and data evaluation processes considering 273 Austrian control region sequences as example. Forensic Sci Int 166: 164–175. [DOI] [PubMed] [Google Scholar]
- 28. Flesch-Janys D, Slanger T, Mutschelknauss E, Kropp S, Obi N, et al. (2008) Risk of different histological types of postmenopausal breast cancer by type and regimen of menopausal hormone therapy. Int J Cancer 123: 933–941. [DOI] [PubMed] [Google Scholar]
- 29. Brandstätter A, Lamina C, Kiechl S, Hunt SC, Coassin S, et al. (2010) Sex and age interaction with genetic association of atherogenic uric acid concentrations. Atherosclerosis 210: 474–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bland JM, Altman DG (2000) Statistics notes. The odds ratio. BMJ 320: 1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coassin S, Brandstätter A, Kronenberg F (2010) Lost in the space of bioinformatic tools: A constantly updated survival guide for genetic epidemiology. The GenEpi Toolbox. Atherosclerosis 209: 321–335. [DOI] [PubMed] [Google Scholar]
- 32. Lee PH, Shatkay H (2008) F-SNP: computationally predicted functional SNPs for disease association studies. Nucleic Acids Res 36: D820–D824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Georges M, Clop A, Marcq F, Takeda H, Pirottin D, et al. (2006) Polymorphic microRNA-target interactions: a novel source of phenotypic variation. Cold Spring Harb Symp Quant Biol 71: 343–350. [DOI] [PubMed] [Google Scholar]
- 34. Kozomara A, Griffiths-Jones S (2011) miRBase: integrating microRNA annotation and deep-sequencing data. Nucleic Acids Res 39: D152–D157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Reumers J, Conde L, Medina I, Maurer-Stroh S, Van DJ, et al. (2008) Joint annotation of coding and non-coding single nucleotide polymorphisms and mutations in the SNPeffect and PupaSuite databases. Nucleic Acids Res 36: D825–D829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yuan HY, Chiou JJ, Tseng WH, Liu CH, Liu CK, et al. (2006) FASTSNP: an always up-to-date and extendable service for SNP function analysis and prioritization. Nucleic Acids Res 34: W635–W641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Santarelli L, Strafella E, Staffolani S, Amati M, Emanuelli M, et al. (2011) Association of MiR-126 with soluble mesothelin-related peptides, a marker for malignant mesothelioma. PLoS One 6: e18232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Png KJ, Halberg N, Yoshida M, Tavazoie SF (2012) A microRNA regulon that mediates endothelial recruitment and metastasis by cancer cells. Nature 481: 190–194. [DOI] [PubMed] [Google Scholar]
- 39. Watahiki A, Wang Y, Morris J, Dennis K, O'Dwyer HM, et al. (2011) MicroRNAs associated with metastatic prostate cancer. PLoS One 6: e24950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Musiyenko A, Bitko V, Barik S (2008) Ectopic expression of miR-126*, an intronic product of the vascular endothelial EGF-like 7 gene, regulates prostein translation and invasiveness of prostate cancer LNCaP cells. J Mol Med (Berl) 86: 313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Meister J, Schmidt MH (2010) miR-126 and miR-126*: new players in cancer. ScientificWorldJournal 10: 2090–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Li Z, Lu J, Sun M, Mi S, Zhang H, et al. (2008) Distinct microRNA expression profiles in acute myeloid leukemia with common translocations. Proc Natl Acad Sci U S A 105: 15535–15540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Li Z, Chen J (2011) In vitro functional study of miR-126 in leukemia. Methods Mol Biol 676: 185–195. [DOI] [PubMed] [Google Scholar]
- 44. Zhang J, Du YY, Lin YF, Chen YT, Yang L, et al. (2008) The cell growth suppressor, mir-126, targets IRS-1. Biochem Biophys Res Commun 377: 136–140. [DOI] [PubMed] [Google Scholar]
- 45. Tavazoie SF, Alarcon C, Oskarsson T, Padua D, Wang Q, et al. (2008) Endogenous human microRNAs that suppress breast cancer metastasis. Nature 451: 147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rhodes DR, Yu J, Shanker K, Deshpande N, Varambally R, et al. (2004) ONCOMINE: a cancer microarray database and integrated data-mining platform. Neoplasia 6: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rhodes DR, Kalyana-Sundaram S, Mahavisno V, Varambally R, Yu J, et al. (2007) Oncomine 3.0: genes, pathways, and networks in a collection of 18,000 cancer gene expression profiles. Neoplasia 9: 166–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhao H, Langerod A, Ji Y, Nowels KW, Nesland JM, et al. (2004) Different gene expression patterns in invasive lobular and ductal carcinomas of the breast. Mol Biol Cell 15: 2523–2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Karnoub AE, Dash AB, Vo AP, Sullivan A, Brooks MW, et al. (2007) Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 449: 557–563. [DOI] [PubMed] [Google Scholar]
- 50. Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, et al. (2008) Stromal gene expression predicts clinical outcome in breast cancer. Nat Med 14: 518–527. [DOI] [PubMed] [Google Scholar]
- 51. Hindorff LA, Sethupathy P, Junkins HA, Ramos EM, Mehta JP, et al. (2009) Potential etiologic and functional implications of genome-wide association loci for human diseases and traits. Proc Natl Acad Sci U S A 106: 9362–9367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. McKay JD, Truong T, Gaborieau V, Chabrier A, Chuang SC, et al. (2011) A genome-wide association study of upper aerodigestive tract cancers conducted within the INHANCE consortium. PLoS Genet 7: e1001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Cui R, Kamatani Y, Takahashi A, Usami M, Hosono N, et al. (2009) Functional variants in ADH1B and ALDH2 coupled with alcohol and smoking synergistically enhance esophageal cancer risk. Gastroenterology 137: 1768–1775. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Amplification and sequencing strategy of LAMTOR2.
(DOC)
Amplification and sequencing strategy of LAMTOR3.
(DOC)
Primers used for amplification and sequencing of LAMTOR2.
(DOC)
Primers used for amplification and sequencing of LAMTOR3.
(DOC)