Abstract
Background
Pain catastrophizing is a powerful predictor of pain adaptation, and both stable and time-varying aspects may influence overall emotional well-being.
Purpose
Test the independent influences of state and trait pain catastrophizing on the relationship between daily intensity and negative affect, positive affect, and depressive symptoms.
Method
Daily diary data were collected for 30 days from a sample of 231 adults with a diagnosis of rheumatoid arthritis (RA).
Results
State pain catastrophizing accounted for a significant proportion of the relationship between daily pain and each of the 3 examined daily outcomes. Greater trait pain catastrophizing significantly increased the effect of state pain catastrophizing on the relationship between pain intensity and the outcome variables in cross-sectional and time-lagged models.
Conclusions
The results of the current study indicate that state pain catastrophizing plays a prominent role in the adaptation to daily pain fluctuations, particularly for those with a propensity to catastrophize.
Keywords: pain catastrophizing, emotion, depression, chronic pain
Chronic pain and affective distress are twin burdens of rheumatoid arthritis (1). This auto-immune disorder, characterized by joint swelling and tenderness at multiple sites in the body (2), carries with it a rate of depression 2 to 3 times the normal prevalence rate (3). Prior research has indicated that episodic elevations in chronic pain predict greater negative emotion and lower levels of positive emotion in individuals with rheumatoid arthritis (4, 5). The relationship between pain and affective distress has been explained by the use of maladaptive pain coping strategies like catastrophizing (6, 7). Pain catastrophizing is defined as a cognitive and affective overreaction to painful episodes (8) and predicts greater negative affect (9) and decreased positive affect in individuals with chronic pain (10). Pain catastrophizing may also explain the cognitive and emotional aspects of depression that are exacerbated during pain flares (11).
The literature examining cognitive sets like catastrophizing often has not distinguished between the trait and state aspects of these states of mind. Individuals with recurrent pain may vary in their tendencies to catastrophize about pain, and examining how people respond to painful experiences on average can reasonably account for the stable aspects of these ways of thinking. Pain catastrophizing also demonstrates significant within-person variation across time, which suggests that pain catastrophizing has a state component, as well (12). Indeed, changes in pain intensity reliably predict fluctuations in catastrophizing about pain, independent of average levels of pain catastrophizing (13), and pain catastrophizing levels that change early in pain-focused psychological interventions predict more pronounced decreases in pain intensity, disability, and depression (14). It is worthwhile to consider whether the impact of catastrophizing from moment to moment may vary between habitual and less-frequent catastrophizers; more frequent catastrophizing may exacerbate the consequences of momentary pain catastrophizing, worsening the dysregulated emotional state. This phenomenon has been observed in individuals with depression; prolonged use of a ruminative attribution style appears to amplify the negative effects of depression (15). The current study tested this phenomenon by examining whether stable levels of catastrophizing about pain moderated the effects of daily pain catastrophizing.
Cross-sectional studies have lacked sufficient statistical and methodological power to examine this dynamic interplay of pain and cognitive and affective processes. Examination of state processes using hierarchical time series data allows for the modeling of both stable and time-varying aspects of this dynamic interplay of pain flares and cognitive and affective processes. Trait measurements are stable and allow for accurate predictions across time and between individuals. State measurements allow for the detection of important influences that vary within persons over time (16), which may be due to affective, cognitive, or behavioral fluctuations (5). This distinction has been suggested for constructs like positive and negative affect (17), pain intensity (17) and pain catastrophizing (13). The current study examined state and trait pain catastrophizing and assessed how the dynamic interplay of pain intensity and maladaptive cognitive responses to pain may exacerbate affective disturbance. Diary datasets have been used to examine the day-to-day consequences of social interactions for negative emotional states and self-reported fatigue in individuals with chronic pain (18). The current study expanded upon these findings by examining how the experience of physical pain and consequent cognitive reactions to pain may serve to exacerbate emotional distress.
The current study utilized an existing daily diary dataset (18, 19) from a sample of 231 individuals with a diagnosis of rheumatoid arthritis to test the interactions of stable and time-varying aspects of pain catastrophizing and their relationships with pain-related affective disturbance in 2 distinct models. First, cross-sectional models were constructed to test the extent to which levels of state pain catastrophizing mediated same-day pain-affect relationships. Additionally, lagged models tested the mediating effects of pain catastrophizing on pain-affect relationships. In both models, it was expected that state pain catastrophizing would significantly mediate the relationships between daily pain intensity and daily reports of positive affect, negative affect, and depressive symptoms. The mediating effects of state pain catastrophizing were expected to vary by trait pain catastrophizing scores, with state pain catastrophizing accounting for a larger proportion of the relationship between daily pain intensity and measures of affective disturbance for those with higher trait pain catastrophizing.
Method
Participants
A sample of 231 individuals with rheumatoid arthritis recruited between 2001 and 2005 was included in this study; women constituted 69.6% of the sample. Participants were recruited from the Phoenix, AZ region via solicitations at health fairs, Arthritis Foundation members, and local physician offices as well as the Veterans Administration Hospital. Participants were required to provide written confirmation of rheumatoid arthritis from a rheumatologist. In order to prevent the confounding of physiological mechanisms of rheumatoid arthritis, participants taking cyclical estrogen replacement or who had Lupus were excluded from the study, as these conditions were likely to alter functioning on the hypothalamic-pituitary-adrenal axis. The average duration of rheumatoid arthritis in the sample was 13.6 years for the male participants and 11.5 years for the females. The mean age was 53.0 for women and 60.7 for men, and 85% of the women and 87% of the men were Caucasian. The average yearly family incomes for both men and women fell in the $25,000 to $29,000 range. Of the 231 participants who confirmed a rheumatoid arthritis diagnosis, 48 also reported a diagnosis of osteoarthritis, 16 also reported a diagnosis of fibromyalgia, and 23 reported co-morbid diagnoses of rheumatoid arthritis, osteoarthritis and fibromyalgia. The effects of pain catastrophizing in those with co-morbid osteoarthritis diagnoses were analyzed and demonstrated no notable differences from the overall sample of individuals with rheumatoid arthritis, and differential effects of fibromyalgia diagnosis were due to a greater overall level of trait pain catastrophizing in participants with fibromyalgia. As a result, these analyses were not reported in the current paper, and individuals with co-morbid osteoarthritis and/or fibromyalgia diagnoses were deemed appropriate to be included in all analyses. In the current sample, 15 participants (6.5% of the sample) reported taking at least 1 antidepressant medication, 90 participants (39.0% of the sample) reported taking at least one non-steroidal anti-inflammatory drug, and 57 participants (24.7% of the sample) reported taking corticosteroids regularly.
Procedure
Participants who were successfully screened into the study completed and returned by mail an informed consent form, as well as documents permitting researchers to seek confirmation of a rheumatoid arthritis diagnosis from their rheumatologists. Participants were allowed to participate in the study only after providing proof of a physician diagnosis of rheumatoid arthritis. Upon receiving this confirmation, researchers sent each participant an initial packet of questionnaires for demographic information, which were subsequently completed and returned by mail. Participants were then instructed to complete daily diaries once per day. Each person received by mail a packet of 30 paper diary questionnaires, as well as 30 postage-paid envelopes. A researcher then contacted each participant and provided instructions on the procedure. Participants filled out the diaries 30 minutes before bedtime each day. To maintain compliance, participants mailed out the completed diaries from the previous day in the postmarked envelopes, and verification of postmarks allowed researchers to confirm protocol adherence. Participants received up to $90 as compensation for successfully completing the diary study. Each completed diary was worth $2, as well as a bonus $1 for each diary completed, after 25 diaries were completed. The rate of diary completion was 94% overall. Research assistants monitored postmarks to ensure that diaries were completed and postmarked in succession each day. Participants were contacted immediately and urged to comply with the time-sensitive demands of the study if any discrepancies were detected. 97.3% of diaries were received with a verified postmark. Of those with a verified postmark, 82.3% of diaries were mailed on the morning after completion. This estimate reflects the actual number of diaries that were postmarked on the day subsequent to diary completion (58%), adjusted for the percent of diaries completed on Saturday and postmarked on Monday (≈1/7, or 14.3%), as well as diaries postmarked late due to holiday, late drop-off at the mailbox, or postal service error (approximately 10%).
Measures
Daily pain was measured in each diary with the standard instruction for a numerical rating scale (20, 21), “Please choose a number between 0 and 100 that best describes the average level of pain you have experienced today due to your rheumatoid arthritis. A zero (0) would mean ‘no pain’ and a one hundred (100) would mean “pain as bad as it can be.”
Positive affect and negative affect were measured in each diary through the use of the Positive and Negative Affect Schedule (22). Participants were given a list of 10 positive mood adjectives and 10 negative mood adjectives and asked to rate the extent to which they had experienced each mood on a 5-point scale from 1 “Very slightly or not at all” to 5 “Extremely.” The reliability of the negative affect scale was acceptable (α= .867), and the reliability for the positive affect scale was also acceptable (α = .929).
Depressive symptoms were assessed in each diary as a sum total of the responses on 6 “yes or no” questions: lack of interest in the day’s activities, increase or decrease in appetite, feeling “restless” or “slowed down,” fatigue or loss of energy, feeling down on oneself, and difficulty concentrating or making decisions (23). Following the methods utilized in the Conner et al. paper (23), the symptom of depressed mood was omitted in order to minimize overlap with mood measures. Also similar to the Conner et al. paper (23), reliability in the depressive symptoms scale was modest when alpha reliabilities were computed at the daily level (α = .662), but when daily number of depressive symptoms were aggregated for each individual across the 30 days, reliability was acceptable (α = .823). These reliability estimates indicate that although there was notable variability in the co-occurrence of depressive symptoms on any given day, there was a significant degree of consistency in the symptoms reported by each participant over the 30-day interval of the study. It should also be noted that the daily total of depressive symptoms was intended to be an indicator of immediate subclinical distress, and not intended as an indicator of the occurrence of a major depressive episode. As we did not examine changes in diagnosed depressive disorders across the current study and desired not to mislead readers to draw conclusions about clinical diagnoses based on our results, depressive symptoms were included as an indicator of distress, rather than a rating of severity of depression.
Daily pain catastrophizing was assessed in the daily diaries with 2 questions from the Coping Strategies Questionnaire (24). Participants rated their level of agreement with 2 statements for that day: “I worried about whether my pain would ever end” and “I felt my pain was so bad I couldn’t stand it anymore.” Ratings were on a Likert scale of 1 to 5, from “Strongly Disagree” to “Strongly Agree.” Daily catastrophizing scores were computed by averaging the 2 items. Reliability of the 2-item pain catastrophizing scale was acceptable (α = .812).
Kenny and Zautra (25) proposed a temporal structure for time-series data (called STARTS) in which any momentary observation contains 3 components: a stable trait component, a semi-stable autoregressive process in which state observations at any given point are predicted by both the previous state measurement and a random process, and a state component that is random and does not carry over from one time point to the next. Following the STARTS framework, a measure of trait pain catastrophizing was calculated by aggregating individual pain catastrophizing scores across the 30-day interval, yielding a stable estimate of an individual’s pain catastrophizing level. This 30-day aggregate score was then subtracted from the observed pain catastrophizing score on each day of the diaries, yielding a residual measure of state pain catastrophizing. As expected, these measures of trait and state pain catastrophizing were uncorrelated (r = 0.00). The state component of pain catastrophizing yielded by this method contained a significant auto-regressive component, which required modeling of a first-order auto-regressive process, AR(1), in all models in order to account for auto-correlation between time points. The AR(1) component accounted for autocorrelation in variables in the lagged models, yielding unique estimates of cross-day effects, independent of same-day effects. To probe the convergent validity of this trait measure with other measures of trait pain catastrophizing, the trait pain catastrophizing scores from the diaries were compared with those in the pain catastrophizing subscale of the Vanderbilt Multidimensional Pain Coping Inventory (VMPCI; 26), which was assessed one time prior to the start of the diary assessments. The VMPCI subscale correlated moderately (r = .462) with the trait pain catastrophizing measure used in the current study, and the VMPCI moderator yielded similar largely results when entered in the moderated mediation models under investigation.
Trait neuroticism was measured once, prior to the diary assessments, using the 12-item Neuroticism subscale of the NEO Five Factor Inventory (27), and was entered as a potential covariate. The reliability of the Neuroticism subscale was acceptable (α = .79).
Participants were administered the Hamilton Depression Inventory one time prior to beginning the diaries (28). 46.8% of the sample reported no depression, 12.4% reported subclinical levels of depression, and the remainder of the sample (41%) reported at least mild depression. Subsequent analyses indicated that participants reporting no depression had significantly lower levels of trait pain catastrophizing than participants reporting subclinical or clinical depression, but there was no difference in catastrophizing scores among participants reporting subclinical or more severe clinical depression.
Results
Overview of Analyses
Analysis of multilevel moderated-mediation models took place in 2 steps for both cross-sectional and time-lagged effects. First, non-moderated multilevel mediation models were estimated to test the role of state pain catastrophizing as a statistical mediator of the relationship between daily pain intensity and 3 different daily outcomes (negative affect, positive affect, and number of depressive symptoms reported). Descriptive statistics for all variables are found in Table 1. Next, the moderating effects of trait pain catastrophizing were tested for each mediation model. Interactions of the moderator with pain intensity or state pain catastrophizing were tested for each path (estimation of the a and b paths, respectively; see Figure 1). As trait pain catastrophizing was comprised of only level-2 (i.e., stable) variance, this measure was identical in both cross-sectional and lagged models. Path models and moderation effects were estimated both cross-sectionally and with 2 1-day lags, such that the path coefficients estimated the mediated effect on an outcome measured the same day, as well as an estimated mediated effect over a 3-day span, with a 1-day lag between pain intensity and state pain catastrophizing, and another 1-day lag between state pain catastrophizing and the observed outcome (see Figure 2). These 1-day lags were introduced in order to test models with stronger evidence of temporal precedence. As we could not establish evidence for the temporal ordering of the variables in the cross-sectional models, it is more appropriate to describe the mediators in these models using the broader term “intervening variable” (29). With this caution in mind, however, the analytic approach for both model types was identical and henceforth will be referred to as mediation analyses. As bidirectional causality was likely in these models, each mediation model was also tested in reverse, with each affective distress variable predicting state pain catastrophizing, and state pain catastrophizing predicting pain intensity.
Table 1.
Descriptive statistics
| Mean | Standard Deviation | |
|---|---|---|
| Pain intensity | 32.5 | 23.3 |
| State pain catastrophizing (CSQ) | 0.0 | 0.6 |
| Trait pain catastrophizing (CSQ) | 2.1 | 0.9 |
| Trait pain catastrophizing (VMPCI) | 2.0 | 0.7 |
| Negative affect | 1.3 | 0.5 |
| Positive affect | 2.7 | 0.9 |
| Depressive symptoms | 1.2 | 1.4 |
| Neuroticism | 2.6 | 0.6 |
| Age | 55.0 | 13.2 |
Observations were made based on 231 participants, with daily diary assessments across 30 days.
Note: CSQ = Coping Strategies Questionnaire Pain Catastrophizing Subscale, VMPCI = Vanderbilt Multidimensional Pain Coping Questionnaire Pain Catastrophizing Subscale
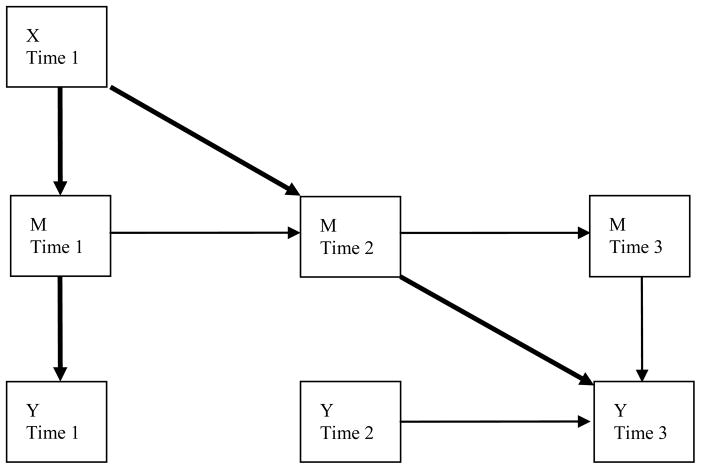
Figure 1.
Conceptual model depicting mediation. X = predictor, M = mediator, Y = outcome variable
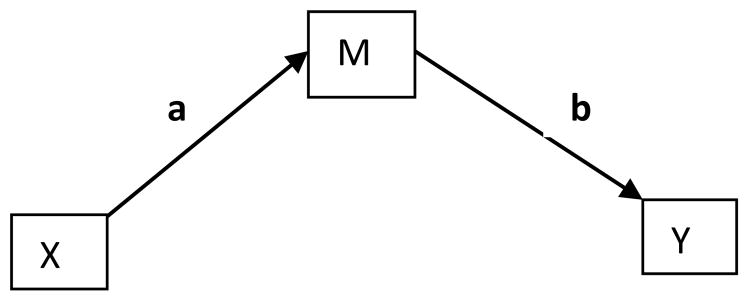
Figure 2.
Conceptual model depicting cross-sectional and time-lagged moderated mediation. X = predictor, M = mediator, Y = outcome variable
Note: Bolded paths represent paths tested for moderation
Path coefficient estimates were calculated using the SAS PROC MIXED program, and significance of mediation effects were determined using the PRODCLIN program (30). The PRODCLIN program computes asymmetric confidence limits to correct for non-normal distributions in the indirect effect (30). The distribution of confidence limits is preferable to the calculation of the difference of effects of the direct and indirect paths (c′-c), due to concerns about the requirement of normality in the multivariate distributions of the direct and indirect effects (31). Confidence limits were calculated at an alpha level of .05. Moderation effects were deemed significant if there was a significant predictor-by-moderator interaction in either the a or b path. 3 covariates (age, gender, and trait neuroticism) were also modeled to test whether these variables substantially altered the significance of observed moderating effects. When positive and negative affect were modeled as outcome variables, the opposing affect score was also entered as a covariate in order to obtain a purer measure of either positive or negative affect (i.e., negative affect was predicted with positive affect scores modeled as a covariate, and vice-versa).
For level-1 predictors (e.g., daily pain intensity, state pain catastrophizing), scores were centered using the cluster (or person) mean, not the grand mean. This centering procedure yields predictors containing only within-person variance by removing the influence of between-person (level-2) variance in the predictor (32). The trait pain catastrophizing moderator was centered on the grand mean (across all data clusters), in order to permit interpretability of the intercepts and slopes. As level-2 variables contain only level-2 variance and do not vary across lower-level (i.e., level-1) observations, they cannot be centered using individual cluster means (32). Centering on a grand mean yields more interpretable results by making a score of 0 equivalent to the average score across all clusters, with negative scores signifying “below-average” scores on a variable and positive scores signifying “above-average” scores (33). Outcome variables were not centered, as modeling of cross-level interactions may alter both level-1 and level-2 variance in outcomes (33). Changes in level-1 and level-2 variance were computed as an effect size measure using a proportional reduction of variance (PRV) statistic. PRVs were computed by comparing level-1 and level-2 variance from a null model (modeling only the intercept as a predictor of the outcome variable) to a full model, including both the intercept and the predictors of interest in each path, and dividing the difference by the null model variance (33). This approach yielded estimates of the proportional reduction of variance for level-1 and level-2 intercept variances separately. Effect size estimates were calculated for all models under examination, excluding covariate analyses.
In each analysis, there was significant variance among individual slopes on the daily pain intensity predictor, so pain intensity was modeled as a predictor with random, rather than fixed, effects. Modeling of random effects allowed for the effects of the pain intensity variable to vary across individuals, thereby increasing the generalizability of the results by accounting for a greater level of individual differences in pain reactivity.
Cross-sectional mediation models
Daily pain intensity was found to be a significant predictor of daily pain catastrophizing; this parameter estimate represented the a path. State pain catastrophizing significantly predicted each of the 3 outcome measures: daily negative affect, daily positive affect, and number of daily depressive symptoms. Asymmetric confidence limits from the PRODCLIN program indicated that state pain catastrophizing partially mediated the relationship between daily pain intensity and each of the level-1 dependent variables examined (see Table 2). Trait pain catastrophizing interacted significantly with both pain intensity and state pain catastrophizing predicting each outcome variable (see Table 3). The interactions with the moderator consistently increased the magnitude of the effects in the a and b paths for each of the outcome variables, such that there was a larger mediated effect of state pain catastrophizing in each statistical relationship for people who were high in trait pain catastrophizing. The addition of covariates modeling age and gender did not significantly alter the moderating effect of trait pain catastrophizing in the prediction of any of the outcome variables. The addition of a covariate for neuroticism affected the results of one analysis. The trait pain catastrophizing-by-state pain catastrophizing interaction predicting negative affect became non-significant, when controlling for neuroticism. No other results were affected by the inclusion of neuroticism as a covariate. When the VMPCI trait pain catastrophizing variable was modeled as a moderator, the direction and significance of the moderating effects were similar, except that the state pain catastrophizing-by-trait pain catastrophizing interaction predicting same-day positive affect reached only marginal significance (p < .10) with the VMPCI moderator.
Table 2.
Asymmetric Confidence Limits for the Mediated Effect of Daily Pain Intensity through Pain Catastrophizing in Cross-Sectional and Lagged Models
| Outcome | Cross-Sectional Models | Lagged Models |
|---|---|---|
| Negative Affect | [.00097, .00149] | [−.00003, .00008] |
| Positive Affect | [−.00239, −.00156] | [−.00019, 0] |
| Depressive Symptoms | [.00379, .00551] | [.00015, .00059] |
Note: Significant mediation was found when asymmetric confidence limits did not include 0.
Table 3.
Cross-Sectional Models: Moderating Effects of Trait Pain Catastrophizing on State Pain Catastrophizing Mediation
| Outcome | Predictor | B | Level-1 PRV | Level-2 PRV |
|---|---|---|---|---|
| Daily Pain Catastrophizing |
DP | .00436 | ||
| TPC | .9991** | |||
| DP* TPC | .005065** | .2873 | N/A | |
|
| ||||
| Negative Affect | SPC | .02967 | ||
| TPC | .1823** | |||
| SPC* TPC | .03544** | .0438 | .1352 | |
|
| ||||
| Positive Affect | SPC | −.02267 | ||
| TPC | −.3853** | |||
| SPC* TPC | −.06715** | .0505 | .1373 | |
|
| ||||
| Depressive Symptoms | SPC | .05797 | ||
| TPC | .6646** | |||
| SPC* TPC | .1106** | .0481 | .2308 | |
p < .10.
p < .05.
p < .01.
DP= Daily Pain, SPC = State Pain Catastrophizing, TPC = Trait Pain Catastrophizing Observations were made based on 231 participants, with daily diary assessments across 30 days.
Note. Asterisks (*) indicate tests of interactions between predictors and moderators.
Note: PRV stands for “Proportional Reduction of Variance”
Note: No level-2 PRV available for a path due to cluster-mean centering of pain catastrophizing
When the cross-sectional mediation models were tested in reverse, each path and mediated effect remained significant. Increased daily levels of negative affect and number of depressive symptoms significantly predicted greater levels of pain catastrophizing, while increased levels of positive affect significantly predicted lower levels of pain catastrophizing. State pain catastrophizing significantly and positively predicted same-day pain intensity. State pain catastrophizing partially mediated each path in the reversed cross-sectional models. Trait pain catastrophizing significantly moderated the path from pain catastrophizing to same-day pain intensity and the paths from daily positive affect and negative affect to same-day state pain catastrophizing, such that these relationships were greater in magnitude for individuals higher in trait pain catastrophizing.
Time-lagged mediation models
Daily pain intensity significantly predicted next-day state pain catastrophizing, and state pain catastrophizing significantly predicted next-day depressive symptoms, but not next-day negative or positive affect. Asymmetric confidence limits indicated that state pain catastrophizing partially mediated the relationship between daily pain intensity and depressive symptoms for the lagged model (see Table 2). Trait pain catastrophizing significantly interacted with pain intensity in predicting next-day state pain catastrophizing, such that the relationship between pain intensity and next-day state pain catastrophizing was greater in magnitude for individuals with greater levels of trait pain catastrophizing (see Table 4). Trait pain catastrophizing did not interact with state pain catastrophizing in predicting any of the outcomes in the lagged models. The addition of covariates modeling neuroticism, age, and gender did not significantly alter the moderating effect of trait pain catastrophizing in the prediction of any of the outcome variables. When the VMPCI variable was modeled as a moderator, the direction and significance of the moderating effects were similar, except that the previously significant daily pain intensity-by-trait pain catastrophizing interaction predicting next-day state pain catastrophizing did not reach statistical significance with the VMPCI moderator.
Table 4.
Time-Lagged Models: Moderating Effects of Trait Pain Catastrophizing on State Pain Catastrophizing Mediation
| Outcome | Predictor | B | Level-1 PRV | Level-2 PRV |
|---|---|---|---|---|
| Pain Catastrophizing at Time 2 |
DP1 | .00452** | ||
| TPC | .9968** | |||
| DP1* TPC | .002731* | .1461 | N/A | |
|
| ||||
| Negative Affect at Time 3 | SPC2 | .0016 | ||
| TPC | .1108** | |||
| SPC* TPC | .0214† | .1216 | .0902 | |
|
| ||||
| Positive Affect at Time 3 | SPC2 | −.0251* | ||
| TPC | −.288** | |||
| SPC2* TPC | .0046 | .1130 | .0834 | |
|
| ||||
| Depressive Symptoms at Time 3 | SPC2 | .0865* | ||
| TPC | .6497** | |||
| SPC2* TPC | .03237 | .2412 | .2663 | |
p < .10.
p < .05.
p < .01.
DP= Daily Pain at Time 1, SPC2 = State Pain Catastrophizing at Time 2, TPC = Trait Pain Catastrophizing Observations were made based on 231 participants, with daily diary assessments across 30 days.
Note. Asterisks (*) indicate tests of interactions between predictors and moderators.
Note: PRV stands for “Proportional Reduction of Variance”
Note: No level-2 PRV available for a path due to cluster-mean centering of pain catastrophizing
When the lagged mediation models were reversed, no significant mediated effects were found. Greater state pain catastrophizing levels significantly predicted greater next-day lower levels of pain intensity, but daily depressive symptoms, negative affect, and positive affect were unrelated to next-day state pain catastrophizing. Trait pain catastrophizing significantly moderated only the relationship between negative affect and next-day state pain catastrophizing, such that the relationship between negative affect and next-day state pain catastrophizing was greater in magnitude for individuals with greater levels of trait pain catastrophizing.
Discussion
When pain intensity, state pain catastrophizing and outcome variables were measured concurrently in cross-sectional models, state pain catastrophizing was found to be a significant intervening variable in the relationship between daily pain intensity and daily negative affect, daily positive affect, and daily number of depressive symptoms. Daily fluctuations in pain catastrophizing levels were related to daily fluctuations in daily pain, such that exacerbations in pain were accompanied by more intense catastrophizing. When pain catastrophizing increased, individuals reported greater concurrent emotional distress and depressive symptoms. When these paths were examined in a time-lagged mediation model, state pain catastrophizing mediated the relationship between pain and depressive symptoms, but not negative or positive affect. This finding establishes a more specific causal effect than in previous observational studies. Indeed, these results provide evidence that state pain catastrophizing can be considered a mediator of the observed day-to-day pain-depression relationship.
It was also hypothesized that greater trait pain catastrophizing scores would enhance the mediating effect of state pain catastrophizing on the relationship between daily pain and each of the daily outcomes. This hypothesis was supported by analyses of the cross-sectional mediation models and, to a lesser extent, in the time-lagged models. Results indicated that pain catastrophizing levels explained a greater proportion of the relationship between pain and emotional distress for individuals who catastrophized more on average about their pain. Individuals high in trait pain catastrophizing reported greater same-day increases in state pain catastrophizing in response to increases in pain intensity, as well as greater increases in negative affect and depressive symptoms and greater decreases in positive affect as a consequence of their pain catastrophizing on the same day. The time-lagged models indicated that changes in state pain catastrophizing also explained the relationship between pain intensity and depressive symptoms, but not between pain intensity and positive or negative affect, 2 days later. Individuals high in trait pain catastrophizing were susceptible to greater increases in their pain catastrophizing due to the previous day’s pain intensity, but the consequences of pain catastrophizing on next-day emotional states did not vary across individuals with high- and low-trait pain catastrophizing, nor did state pain catastrophizing play a greater role in the relationship between pain intensity and emotional distress 2 days later.
In prior studies pain catastrophizing has been identified as a key predictor of pain disability (34), distress (34) and overall adjustment to chronic pain (35), and the current study provides further evidence of the need to consider both state and trait components of this variable. Further clarification of the mechanisms through which catastrophizing influences affective reactions to pain may contribute a greater level of understanding to how to bolster individual attempts to adapt to pain. We found that individuals with a greater propensity to catastrophize about their pain appeared to be more vulnerable to the effects of their catastrophic thoughts. Our results suggest that the nature of maladaptive cognitive coping attempts mirrors the effects of rumination on increasing vulnerability to depression (15). More specifically, it appears that individuals may develop a “habit” of catastrophizing about their pain, thereby increasing the intensity of their catastrophic thought and consequently amplifying the deleterious effects that accompany these thoughts at each occurrence.
These results invite speculation about interventions that can effectively reduce pain catastrophizing (5, 36). Effective interpretations might operate through two distinct channels. An intervention could reduce the frequency of intrusive pain-related cognitions and thus serve to reduce the affective burden of frequent pain catastrophizing. In addition, additional guidance could be given to those with predispositions to adopt the helplessness and hopelessness cognitive style that is reflected in trait catastrophizing. By reducing individual attempts to use catastrophizing as a source of self-inoculation against pain and promoting a more adaptive perspective on pain (e.g., promoting acceptance of pain), it may be possible to reduce the impact of each occurrence of catastrophic thoughts about pain. In this study we focused on individual differences that are likely to increase vulnerability. Also left unexamined here are potential positive features of personality that would promote more resilient responding, such as the preservation of positive emotion on days when pain is elevated and quicker recovery following pain exacerbations (37). We urge attention to the positive features of the person, and their daily lives as a complement to the current focus on vulnerabilities in this paper.
Although the data collection method of nightly diaries does capture substantial within-person variation beyond the traditional approach of cross-sectional research, more frequent diaries (i.e., within-day assessments) could further improve our ability to capture day-to-day and, indeed, even hour-to-hour fluctuations in physical, cognitive, and affective states. Research is needed to examine whether such within-day assessments are feasible for the variables studied here, and, if so, whether they successfully capture state variance not accounted for by daily assessments. Assessments that are measured more frequently may better detect the causal effects of pain and pain catastrophizing on affective distress that were absent from the current findings. Additionally, the interpretation of the current findings may be limited by our use of only 2 items used to assess pain catastrophizing from the Coping Strategies Questionnaire. Though these items were chosen because they appeared to adequately reflect the construct of pain catastrophizing and in the interest of maintaining a brief daily assessment, they may not have reflected every aspect of pain catastrophizing; previous researchers have reported that pain catastrophizing appears to have a more complex factor structure, comprised of 3 subscales, that may not have been completely represented in our assessment (7).
As was noted previously, the measure of daily depressive symptoms was intended as a measure of subclinical distress and not as an indicator of a major depressive episode. Though the current results indicate that daily catastrophizing about pain does influence the occurrence of symptoms related to depression, the assessment of depressive symptoms in the current study is insufficient to draw a definitive conclusion regarding pain catastrophizing and the onset of clinical levels of depression (e.g., major depressive episode). Similarly, it is likely that pre-existing psychiatric disorders may have significant implications for how individuals cope with their chronic pain. A significant proportion of our sample self-reported subclinical or clinical levels of depression and these individuals reported greater trait levels of pain catastrophizing. Though it was beyond the scope of our study to do so, it would be valuable to determine if individuals with chronic pain and with clinician-diagnosed mood disorders (e.g., depression, anxiety) are more susceptible to the deleterious effects of pain catastrophizing. Evidence suggests that many mood disorders are more prevalent in individuals with chronic pain (3), and examining the cognitive reactions of those individuals with and without a mood disorder to their pain may further clarify the role of chronic pain in vulnerability to psychiatric disorders.
Like previous research that has examined day-to-day physical and emotional changes in individuals with chronic pain (18), the current study adopted a more precise approach to examining the interplay of pain-related factors while also clarifying these relationships by modeling a cognitive process (pain catastrophizing) that is well-known to be a powerful predictor of well-being in individuals with chronic pain. The use of daily assessments provides a greater level of observation of the effects of pain on cognition and emotion within a more precise time frame, and drawing a distinction between state and trait sources of variance allows for the delineation between stable and labile influences of daily pain on affective outcomes. To our knowledge, this study is the first to examine a state form of pain catastrophizing as a mediator, which may have implications for future research and psychological treatment of pain. Chronic pain is a wide-ranging and often life-altering stressor that affects a broad range of people, and conceptual and methodological extensions such as those attempted in this study should help to promote greater understanding of this affliction in its various forms in the future.
Acknowledgments
The authors wish to acknowledge grant support from the National Institute of Arthritis, Musculoskeletal, and Skin Diseases (2R01 AR/AG 41687), Stress and Adaptation in Rheumatoid Arthritis.
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
References
- 1.Magni G, Moreschi C, Rigatti-Luchini S, Merskey H. Prospective study on the relationship between depressive symptoms and chronic musculoskeletal pain. Pain. 1994;56:289–297. doi: 10.1016/0304-3959(94)90167-8. [DOI] [PubMed] [Google Scholar]
- 2.Hochberg M. Adult and juvenile rheumatoid arthritis: Current epidemiologic concepts. Epidemiol Rev. 1981;3:27–44. doi: 10.1093/oxfordjournals.epirev.a036238. [DOI] [PubMed] [Google Scholar]
- 3.Dickins C, McGowan L, Clark-Carter D, Creed F. Depression in rheumatoid arthritis: A systematic review of the literature with meta-analysis. Psychosom Med. 2002;64:52–60. doi: 10.1097/00006842-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Affleck G, Tennen H, Urrows S, Higgins P. Neuroticism and the pain-mood relation in rheumatoid arthritis: Insights from a prospective daily study. J Consult Clin Psychol. 1992;60:119–126. doi: 10.1037//0022-006x.60.1.119. [DOI] [PubMed] [Google Scholar]
- 5.Zautra AJ, Marbach JJ, Raphael KG, Dohrenwend BP, Lennon MC, Kenny DA. The examination of myofascial face pain and its relationship to psychological distress among women. Health Psychol. 1995;14:223–231. doi: 10.1037//0278-6133.14.3.223. [DOI] [PubMed] [Google Scholar]
- 6.Brown GK, Nicassio PM, Wallston KA. Pain coping strategies and depression in rheumatoid arthritis patients. J Consult Clin Psychol. 1989;57:652–7. doi: 10.1037//0022-006x.57.5.652. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- 8.Sullivan MJL, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Janssen SA. Negative affect and sensitization to pain. Scand J Psychol. 2002;43:131–137. doi: 10.1111/1467-9450.00278. [DOI] [PubMed] [Google Scholar]
- 10.Jones DA, Rollman GB, White KP, Hill ML, Brooke RI. The relationship between cognitive appraisal, affect, and catastrophizing in patients with chronic pain. J Pain. 2003;4:267–277. doi: 10.1016/s1526-5900(03)00630-8. [DOI] [PubMed] [Google Scholar]
- 11.Geisser ME, Robinson ME, Keefe FJ, Weiner ML. Catastrophizing, depression and the sensory, affective and evaluative components of chronic pain. Pain. 1994;59:79–83. doi: 10.1016/0304-3959(94)90050-7. [DOI] [PubMed] [Google Scholar]
- 12.Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: A critical review. Expert Rev Neurother. 2009;9:745–758. doi: 10.1586/ERN.09.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turner JA, Mancl L, Aaron LA. Pain-related catastrophizing: A daily process study. Pain. 2004;110:103–111. doi: 10.1016/j.pain.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 14.Burns JW, Kubilus A, Bruehl S, Harden NH, Lofland K. Do changes in cognitive factors influence outcome following multidisciplinary treatment for chronic pain? A cross-lagged panel analysis. J Consult Clin Psychol. 2003;71:81–91. doi: 10.1037//0022-006x.71.1.81. [DOI] [PubMed] [Google Scholar]
- 15.Ciesla JA, Roberts JE. Rumination, negative cognition, and their interactive effects on depressed mood. Emotion. 2007;7:555–565. doi: 10.1037/1528-3542.7.3.555. [DOI] [PubMed] [Google Scholar]
- 16.Hertzog C, Nesselroade JR. Beyond autoregressive models: Some implications of the trait-state distinction for the structural modeling of developmental change. Child Dev. 1987;58:93–109. [PubMed] [Google Scholar]
- 17.Gaskin ME, Greene AF, Robinson ME, Geisser ME. Negative affect and the experience of chronic pain. J Psychosom Res. 1992;36:707–713. doi: 10.1016/0022-3999(92)90128-o. [DOI] [PubMed] [Google Scholar]
- 18.Finan PH, Okun MA, Kruszewski D, Davis MC, Zautra AJ, Tennen H. The interplay of concurrent positive and negative interpersonal events in the prediction of daily negative affect and fatigue for rheumatoid arthritis patients. Health Psychol. 2010;29:429–437. doi: 10.1037/a0020230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zautra AJ, Davis MC, Reich JW, et al. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J Consult Clin Psychol. 2008;76:408–421. doi: 10.1037/0022-006X.76.3.408. [DOI] [PubMed] [Google Scholar]
- 20.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 21.Zautra AJ, Smith B, Affleck G, Tennen H. Examinations of chronic pain and affect relationships: Applications of a dynamic model of affect. J Consult Clin Psychol. 2001;69:786–795. doi: 10.1037//0022-006x.69.5.786. [DOI] [PubMed] [Google Scholar]
- 22.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 23.Conner TS, Tennen H, Zautra AJ, Affleck G, Armeli S, Fifield J. Coping with rheumatoid arthritis pain in daily life: Within-person analyses reveal hidden vulnerability for the formerly depressed. Pain. 2006;126:198–209. doi: 10.1016/j.pain.2006.06.033. [DOI] [PubMed] [Google Scholar]
- 24.Rosentiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: the relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 25.Kenny DA, Zautra AJ. Trait-state models for longitudinal data. In: Collins LM, Sayer AG, editors. New methods for the analysis of change: Decade of behavior. Washington, DC: American Psychological Association; 2001. pp. 243–263. [Google Scholar]
- 26.Smith CA, Wallston KA, Dwyer KA, Dowdy SW. Beyond good and bad: A multidimensional examination of coping with pain in persons with rheumatoid arthritis. Ann Behav Med. 1997;19:11–20. doi: 10.1007/BF02883422. [DOI] [PubMed] [Google Scholar]
- 27.Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and the NEO Five-Factor Inventory (NEO-FFI): Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc; 1992. [Google Scholar]
- 28.Reynolds WM, Kobak KA. Hamilton Depression Inventory. A self-report version of the Hamilton Depression Rating Scale (HDRS) Odessa, TX: Psychological Assessment Resources; 1995. [Google Scholar]
- 29.Mackinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behav Res Methods. 2007;39:384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kenny DA, Korchmaros JD, Bolger N. Lower level mediation in multilevel models. Psychol Methods. 2003;8:115–128. doi: 10.1037/1082-989x.8.2.115. [DOI] [PubMed] [Google Scholar]
- 32.Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: A new look at an old issue. Psychol Methods. 2002;12:121–138. doi: 10.1037/1082-989X.12.2.121. [DOI] [PubMed] [Google Scholar]
- 33.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Newbury Park, CA: Sage; 2002. [Google Scholar]
- 34.Severeijns R, Vlaeyen JW, Van Den Hout MA, Weber WE. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain. 2001;17:165–172. doi: 10.1097/00002508-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Nieto R, Raichle KA, Jensen MP, Miro J. Changes in pain-related beliefs, coping, and catastrophizing predict changes in pain intensity, pain interference, and psychological functioning in individuals with myotonic muscular dystrophy and facioscapulohumeral dystrophy. Clin J Pain. doi: 10.1097/AJP.0b013e31822019b1. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain. 2006;7:261–271. doi: 10.1016/j.jpain.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 37.Sturgeon JA, Zautra AJ. Resilience: A new paradigm for adaptation to chronic pain. Curr Pain Headache Rep. 2010;14:105–112. doi: 10.1007/s11916-010-0095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]