Abstract
Purpose
To assess the compliance of Chinese urologists with China's benign prostatic hyperplasia (BPH) clinical practice guideline and to explore the diagnosis and therapy modalities for geriatric patients with BPH.
Methods
A cross-sectional survey study was carried out in 33 medical centers in 11 different cities in China. A total of 190 urologists participated in a survey to record their preferences for diagnostic tests and treatment options for BPH outpatients. Diagnostic test results as well as health care demands were collected by surveying 2,027 outpatients aged 60 years and older.
Results
The survey response rate was 97.4%. The respondents generally used the diagnostic tests recommended in China's BPH clinical practice guideline at varying rates. The used rates for medical history, ultrasonography, and urinalysis were above 90.0%; that for uroflowmetry was 31.2%. In addition, the rate of use of recommended tests was higher among doctors in the north than among those in the south. Combination therapy with α-adrenoceptor antagonists and 5α-reductase inhibitors was the preferred treatment option for BPH, and was increasingly used with worsening lower urinary tract symptoms. Finasteride was the most prescribed medication (48.0%), followed by tamsulosin (22.7%).
Conclusions
This study assessed the preferences of urologists in the diagnosis and treatment of BPH, which will serve as an important reference for updating and improving China's current BPH clinical practice guideline.
Keywords: Prostatic hyperplasia, Diagnosis, Practice guideline, Therapy
INTRODUCTION
Benign prostatic hyperplasia (BPH), one of the most common diseases of aging men, is associated with bothersome lower urinary tract symptoms that affect quality of life [1]. The prevalence of histopathologic BPH is age-dependent, with initial development usually after 40 years of age [2,3]. It has been reported that approximately 4.5 million visits were made to a physician's office for a primary diagnosis of BPH in 2000, with almost 8 million visits made with a primary or secondary diagnosis of BPH; the direct cost of BPH treatment was estimated to be $1.1 billion exclusive of outpatient pharmaceuticals in 2000 [4]. The huge BPH population and high medical cost require greater attention to appropriate management of BPH. Thus, it is necessary to standardize clinical practice for BPH. The first BPH clinical practice guideline (CPG) was produced by the Agency for Health Care Policy and the American Urological Association in 1994 [5]. Urological Associations in Europe, Australia, and Japan subsequently issued their own BPH CPGs, which are periodically updated.
China's first BPH CPG was drafted in 2006 and was approved by the China Urological Association in 2007. The present study investigated the compliance of urologists with China's BPH CPG and explored the diagnostic and treatment modalities for geriatric patients with BPH. This was the first multi-center epidemiological investigation into how China's BPH CPG is implemented in domestic clinical practice.
MATERIALS AND METHODS
Participants
This multi-center, cross-sectional survey study was undertaken in 2011 throughout China by use of stratified random sampling. The primary sampling units were cities: 11 cities were selected in north (Lanzhong, Beijing, Shenyang, and Jinan) and south (Chendu, Guangzhou, Changsha, Wuhan, Hangzhou, Nanjing, and Shanghai) China. The secondary sampling units were medical centers: 3 medical centers were randomly selected in each city, resulting in a total of 33 centers. The final sampling units were subjects, including doctors and patients selected from the outpatient department at each medical center during the study period.
Among 190 urologists from the 33 participating medical centers, 185 doctors completed the survey. The patient sample size was determined according to the 95% confidence interval. A total of 2,027 outpatients aged ≥60 years with a clinical diagnosis of BPH (prostate size greater than 20 mL and a maximum flow rate less than 15 mL/sec) were enrolled at random. Patients with any other diseases (including severe heart disease, renal disease, neurological disease, urinary tract infection, or previous transurethral surgery) that were likely to affect urinary symptoms were excluded from the study.
Methods
The survey contained 2 sections. Section I assessed the doctors' preferences in recommended diagnostic tests, including medical history, International Prostate Symptom Score (IPSS), quality of life index, digital rectal examination, partial nervous system examination, urinalysis, prostate-specific antigen (PSA), ultrasonography, and uroflowmetry. Section II assessed the doctors' preferences in treatment on the basis of the patient's diagnosis.
Statistical Analysis
The database was managed with Epidata 3.0 and the statistical analyses were performed with SAS 9.1 (SAS Institute Inc, Cary, NC, USA).
RESULTS
Proportion of BPH in Male Outpatients
In this study, 14,748 (47%) of 31,371 geriatric male patients visiting an outpatient department had BPH (Table 1).
Table 1.
The proportion of benign prostatic hyperplasia (BPH) in male outpatients in China (n=31,371)

Objective Parameters of the Patients
Among the 2,027 participating outpatients, the mean age, prostate volume, peak flow rate, and quality of life index were 75.7 years, 41.8 mL, 9.6 mL/sec, and 2.6, respectively. For all three IPSS categories the prevalence of urinary symptoms was 28.6% for mild (IPSS, 0 to 7), 70.3% for moderate (IPSS, 8 to 19), and 1.1% for severe (IPSS, 20 to 35) (Table 2).
Table 2.
Objective parameters of the patients (n=2,027)

Values are presented as mean±standard deviation (range) or number (%).
BPH, benign prostatic hyperplasia; IPSS, International Prostate Symptom Score.
Doctors' Preferences for Diagnostic Tests
Among 190 urologists participating in the study, 185 completed the survey, resulting in a response rate of 97.4%. Among the diagnostic tests recommended by the guideline, an overwhelming majority of the doctors used medical history (93.8%), ultrasonography (92.7%), or urinalysis (92.5%) in 2,027 cases. PSA was used at a rate of 88.8%, and uroflowmetry was the least used (31.2%) (Table 3).
Table 3.
Doctors' preferences for diagnostic tests for BPH in China (n=2,027)

Doctors' Preferences for Treatment Options
In this study, drug therapy was the preferred treatment option for the 2,027 participating patients. The rate of drug therapy was 59.4% for mild cases. Both drug therapy and prostatic surgery were used for moderate and severe cases (Table 4).
Table 4.
Doctors' preferences for treatment options of patients (n=2,027) with benign prostatic hyperplasia in China

Drugs Used for BPH
Among 1,293 medical prescriptions, 1,869 drugs and 207 plants were used for treatment of BPH including combination therapy using more than 2 drugs or plant. Finasteride was the most preferred option (48.0%), followed by tamsulosin (22.7%) (Table 5).
Table 5.
Drugs used for the treatment of benign prostatic hyperplasia in China

Total drug or plant prescriptions (n=2,076).
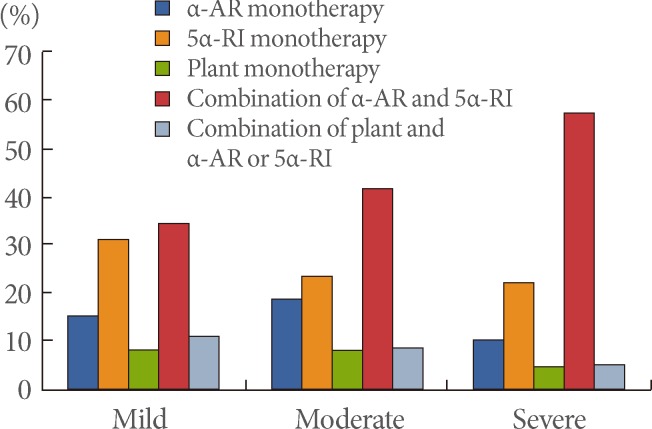
The used rates for combination therapy with α-adrenoceptor (α-AR) antagonist and 5α-reductase inhibitor (5α-RI) increased with the severity of symptoms, from 34.2% for mild cases to 57.5% for severe cases. There was a significant difference in the used rates according to symptom severity (χ2=51.179, P<0.001) (Fig. 1).
Fig. 1.
Rate of use of drug therapies at different severity levels of symptoms. α-AR, α-adrenoceptor; 5α-RI, 5α-reductase inhibitor.
DISCUSSION
A multinational study on community men aged between 40 and 79 years showed that the prevalence of BPH was 14% in France, 18% in Scotland, 38% in the United States, and 56% in Japan [6]. An investigation on community-dwelling men aged 60 years and older in six cities in China in 1997 reported a 46% prevalence of BPH [7]. In our study, approximately 50% of geriatric outpatients aged 60 years and older had BPH. Obviously, BPH is a common disease of elderly men in China. CPGs are believed to improve the quality of clinical decisions by helping and reassuring doctors who may be uncertain about the appropriateness of a clinical choice [8]. Thus, establishing and implementing a CPG for BPH is important in the management of BPH. To date, several CPGs have addressed the optimal treatment of men with BPH. In clinical areas in which there are numerous guidelines, however, there is considerable variations in the recommendations made [9]. In addition, although guidelines provide a framework for evaluation and treatment, they leave a great deal of room for the personal opinions of individual doctors. For example, digital rectal examination and PSA are recommended by most of the guidelines. However, some surveys have shown large differences in the using rates of these tests between countries [10-13]. In our study, digital rectal examination was used at a rate of 67.5%, and PSA was used at a rate of 88.8%. These differences may, in part, result from differences in local health service issues, such as socialized medical systems, manpower issues, availability of extensive technology, the unique perspective of local doctors, or cultural differences in urological practices.
With regard to treatment options, drug therapy was the preferred treatment option in our study. Our results indicate that doctors prefer watchful waiting for less than 50% of mild cases, which could lead to overprescription of medications for patients with mild symptoms, because watchful waiting is the recommended strategy for patients with mild BPH. When prescribing medications for BPH, α-AR antagonists (e.g., tamsulosin) and 5α-RIs (e.g., finasteride) are the medications currently approved by the U.S. Food and Drug Administration for the treatment of BPH [14]. In our study, finasteride was the most preferred option (48.0%), followed by tamsulosin (22.7%). This finding is consistent with recent reports by others in China showing that finasteride held the major share of prescriptions [15]. In our study, finasteride was used more often than α-AR antagonist therapy. This may be because in our study most patients had moderate and severe symptoms. Moreover, convincing evidence exists for the effectiveness of finasteride in the treatment of moderate and severe BPH [16-18]. This may have led the doctors in the present study to prefer finasteride for their patients. Combination therapy with α-AR antagonist and 5α-RI was used more often for patients with severe symptoms, which is consistent with the findings of other studies [19-22].
In conclusion, this is the first multi-center epidemiological study to quantify the extent to which China's BPH CPG is implemented in clinical practice. This study assessed the preferences of urologists in the diagnosis and treatment of BPH, which will serve as an important reference for updating and improving China's current BPH CPG.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Roehrborn CG, McConnell JD. Etiology, pathophysiology, epidemiology and natural history of benign prostatic hyperplasia. In: Walsh PC, Retik AB, Vaughan ED Jr, Wein AJ, Kavoussi LR, Novick AC, et al., editors. Campbell's urology. 8th ed. Philadelphia: WB Saunders; 2002. pp. 1297–1336. [Google Scholar]
- 2.Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132:474–479. doi: 10.1016/s0022-5347(17)49698-4. [DOI] [PubMed] [Google Scholar]
- 3.Gu FL, Xia TL, Kong XT. Preliminary study of the frequency of benign prostatic hyperplasia and prostatic cancer in China. Urology. 1994;44:688–691. doi: 10.1016/s0090-4295(94)80207-6. [DOI] [PubMed] [Google Scholar]
- 4.Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2005;173:1256–1261. doi: 10.1097/01.ju.0000155709.37840.fe. [DOI] [PubMed] [Google Scholar]
- 5.McConnell JD, Barry MJ, Bruskewitz RC, Bueschen AJ, Denton SE, Holtgrewe HL, et al. Benign prostatic hyperplasia: diagnosis and treatment (Clinical practice guideline no. 8; AHCPR publication no. 94-0582) Rockville: U.S.: Department of Health and Human Services, Agency for Healthcare Research and Quality; 1994. [Google Scholar]
- 6.Sagnier PP, Girman CJ, Garraway M, Kumamoto Y, Lieber MM, Richard F, et al. International comparison of the community prevalence of symptoms of prostatism in four countries. Eur Urol. 1996;29:15–20. doi: 10.1159/000473711. [DOI] [PubMed] [Google Scholar]
- 7.Yu P, Zheng H, Su H, Zuo T, Duan C, Gao F, et al. Prevalence of prostatic hyperplasia and its relative factors in six cities of China in 1997. Zhonghua Liu Xing Bing Xue Za Zhi. 2000;21:276–279. [PubMed] [Google Scholar]
- 8.Gravas S, Tzortzis V, Melekos MD. Translation of benign prostatic hyperplasia guidelines into clinical practice. Curr Opin Urol. 2008;18:56–60. doi: 10.1097/MOU.0b013e3282f13bbf. [DOI] [PubMed] [Google Scholar]
- 9.Irani J, Brown CT, van der Meulen J, Emberton M. A review of guidelines on benign prostatic hyperplasia and lower urinary tract symptoms: are all guidelines the same? BJU Int. 2003;92:937–942. doi: 10.1111/j.1464-410x.2003.04529.x. [DOI] [PubMed] [Google Scholar]
- 10.Kim HL, Benson DA, Stern SD, Gerber GS. Practice trends in the management of prostate disease by family practice physicians and general internists: an internet-based survey. Urology. 2002;59:266–271. doi: 10.1016/s0090-4295(01)01504-7. [DOI] [PubMed] [Google Scholar]
- 11.Fukagai T, Maruyama K, Nagata M, Morita M, Naoe M, Yoshida H. Practice patterns regarding prostate cancer and benign prostatic hyperplasia in Japanese primary care practitioners. Int J Urol. 2007;14:412–415. doi: 10.1111/j.1442-2042.2007.01742.x. [DOI] [PubMed] [Google Scholar]
- 12.Hutchison A, Farmer R, Chapple C, Berges R, Pientka L, Teillac P, et al. Characteristics of patients presenting with LUTS/BPH in six European countries. Eur Urol. 2006;50:555–561. doi: 10.1016/j.eururo.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Paick JS, Kim SW, Ku JH. Patterns in the diagnosis and management of benign prostatic hyperplasia in a country that does not have country-specific clinical practice guidelines. Yonsei Med J. 2007;48:281–288. doi: 10.3349/ymj.2007.48.2.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Physicians' desk reference. 61st ed. Montvale: Thomson PDR; 2007. [Google Scholar]
- 15.Lin T. Market analysis of medicines for treatment of benign prostatic hyperplasia in sample hospitals of Shanghai. Pharm Care Res. 2006;6:370–372. [Google Scholar]
- 16.Bruskewitz R, Girman CJ, Fowler J, Rigby OF, Sullivan M, Bracken RB, et al. PLESS Study Group. Proscar Long-term Efficacy and Safety Study. Effect of finasteride on bother and other health-related quality of life aspects associated with benign prostatic hyperplasia. Urology. 1999;54:670–678. doi: 10.1016/s0090-4295(99)00209-5. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan SA, Lee JY, Meehan AG, Kusek JW MTOPS Research Group. Long-term treatment with finasteride improves clinical progression of benign prostatic hyperplasia in men with an enlarged versus a smaller prostate: data from the MTOPS trial. J Urol. 2011;185:1369–1373. doi: 10.1016/j.juro.2010.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vickers AJ, Savage CJ, Lilja H. Finasteride to prevent prostate cancer: should all men or only a high-risk subgroup be treated? J Clin Oncol. 2010;28:1112–1116. doi: 10.1200/JCO.2009.23.5572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Speakman MJ. Integrating patient risk profiles in the treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH) in Clinical Practice. Eur Urol Suppl. 2004;3:18–22. [Google Scholar]
- 20.McConnell JD, Roehrborn CG, Bautista OM, Andriole GL, Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–2398. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan SA, McConnell JD, Roehrborn CG, Meehan AG, Lee MW, Noble WR, et al. Combination therapy with doxazosin and finasteride for benign prostatic hyperplasia in patients with lower urinary tract symptoms and a baseline total prostate volume of 25 ml or greater. J Urol. 2006;175:217–220. doi: 10.1016/S0022-5347(05)00041-8. [DOI] [PubMed] [Google Scholar]
- 22.Lee JY, Lee SH, Kim SJ, Kim CS, Lee HM, Kim CI, et al. Change in International Prostate Symptom storage subscore after long-term medical therapy in BPH patients: finasteride and alpha-blocker combination therapy in men with moderate-to-severe LUTS/BPH in Korea. Urology. 2011;77:171–176. doi: 10.1016/j.urology.2010.05.033. [DOI] [PubMed] [Google Scholar]