Abstract
Objective The current study replicates and extends work with adults that highlights the relationship between trauma exposure and distress in response to subsequent, nontraumatic life stressors. Methods The sample included 213 2–4-year-old children in which 64.3% had a history of potential trauma exposure. Children were categorized into 4 groups based on trauma history and current life stress. Results In a multivariate analysis of variance, trauma-exposed children with current life stressors had elevated internalizing and externalizing problems compared with trauma-exposed children without current stress and nontrauma-exposed children with and without current stressors. The trauma-exposed groups with or without current stressors did not differ on posttraumatic stress disorder symptom severity. Accounting for number of traumatic events did not change these results. Conclusions These findings suggest that early life trauma exposure may sensitize young children and place them at risk for internalizing or externalizing problems when exposed to subsequent, nontraumatic life stressors.
Keywords: posttraumatic stress disorder, stress sensitivity, trauma exposure, young children
Introduction
The prevalence of trauma exposure in young children is concerning and has serious implications for children’s development. A recent examination of the prevalence of trauma exposure using a diverse birth cohort sample in the northeastern United States of 1,152 children aged 1–3 years old indicated that one in six (16.9%) children experienced one or more types of potentially traumatic events (PTEs), including noninterpersonal events, such as a car accident or a dog bite, and interpersonal events, such as family and community violence (Briggs-Gowan, Ford, Fraleigh, McCarthy, & Carter, 2010). Strikingly, when Briggs-Gowan et al. (2010) assessed these children 1 year later, the lifetime prevalence of PTE exposure increased by >50%, implying that a substantial number of children who had not experienced a PTE by the first assessment, were newly exposed within a 12-month period. These findings suggest that one in four infants and toddlers may experience a PTE, which is similar to the estimated prevalance of extreme stress exposure in a community sample of older children from the Great Smoky Mountains Study (Costello, Erklani, Fairbank, & Angold, 2002). Studies of high-risk samples have reported much higher rates of young children’s exposure to PTEs (Farver, Xu, Eppe, Fernandez, & Schwartz, 2005; Linares et al., 2001; U.S. Department of Health and Human Services, 2006). Clearly, in addition to school-age children and adolescents, young children are often exposed to significant adversity. During the lifespan, the prevalence of PTE exposure continues to increase, as it is estimated that 60–90% of adults have experienced at least one PTE (Breslau, Davis, Andreski, Federman, & Anthony, 1998; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995).
Although exposure to a PTE confers risk of negative consequences regardless of the victim’s age, PTE exposure in young children is arguably more detrimental because of the risk of enduring changes in stress-related systems and other brain areas imposed during sensitive periods, when the brain is undergoing rapid development and differentiation (Belsky & de Haan, 2011). Disrupted development could result in a host of functional impairments in emotional, cognitive, behavioral, and interpersonal domains. Indeed, in addition to documented posttraumatic stress disorder (PTSD) in PTE-exposed children (De Young, Kenardy, & Cobham, 2011a; Scheeringa, Zeanah, Myers, & Putnam, 2003), these children also show high rates of other internalizing (Briggs-Gowan et al., 2010; Cicchetti & Toth, 2005) and externalizing behavior problems (Milot, St-Laurent, Ethier, & Provost, 2010; Sroufe, Egeland, Carlson, & Collins, 2005), and social skills deficits and relational problems (Darwish, Esquivel, Houtz, & Alfonso, 2001; Manly, Kim, Rogosch, & Cicchetti, 2001). These may be signs of emergent psychopathology extending beyond PTSD symptoms (Briggs-Gowan et al., 2010).
Two studies of young children have examined mediators of the relationship between PTE-exposure and later emotional and behavioral health problems. Briggs-Gowan, Carter, and Ford (2012) followed up 437 children from 3 years of age to kindergarten and found that PTSD symptoms characterized by arousal and avoidance significantly mediated longitudinal pathways from early violence exposure to emotional problems and lower competence (Briggs-Gowan, Carter, and Ford, 2012). Similarly, a cross-sectional study reported that symptoms of traumatic stress in maltreated and nonmaltreated preschool children statistically mediated the association between early maltreatment and internalizing and externalizing behavior problems (Milot, Ethier, St-Laurent, & Provost, 2010). These studies suggest that trauma-related symptoms interfere with later functioning and contribute to the development of symptoms associated with other internalizing and externalizing disorders.
A possible mechanism by which PTE exposure may lead to internalizing and externalizing behavior problems later in children’s development may be derived from stress-sensitization theory (or “kindling theory”), which has its roots in the adult depression literature. This theory describes a process by which potential trauma affects how an individual responds to subsequent life stressors such that it takes less stress to precipitate a recurrence of depressive symptoms (Antelman, Eichler, Black, & Kocan, 1980; Post & Weiss, 1998). Support for this theory comes from studies showing an association between child abuse and neglect and exaggerated responses to stressful life events in depressed adults (Hammen, Henry, & Daley, 2000). One study found that adolescents with a history of child maltreatment reported a less severe stressful life event before the onset of their first depressive episode compared with adolescents without a maltreatment history (Harkness, Bruce, & Lumley, 2006). In another study, the risk of psychopathology and perceived stress conferred by past-year stressful life events was significantly enhanced in adults with, relative to those without, a history of childhood physical, sexual, or emotional abuse or neglect (McLaughlin, Conron, Koenen, & Gilman, 2010).
Outside of the depression literature, findings from studies focusing on trauma and PTSD are consistent with a stress sensitization model. For example, individuals previously exposed to a PTE have a greater likelihood of developing PTSD after being exposed to a PTE than individuals with no previous exposure (Breslau, Chilcoat, Kessler, & Davis, 1999; Cougle, Resnick, & Kilpatrick, 2009; Kessler, Sonnega, Bromet, & Hughes, 1995; King, King, & Foy, 1996). In addition, studies have reported greater distress after an accident or natural disaster in adults with a history of PTE exposure compared with those without (Bland, O'Leary, Farinaro, & Jossa, 1996; Dougall, Herberman, Delahanty, Inslicht, & Baum, 2000; Smid et al., 2012). A recent study found that perceived stress and emotion-focused coping statistically mediated the relationship between childhood physical or psychological abuse and adult physical health problems, consistent with the view that stress sensitization may be also involved in the long-term association between childhood PTEs and adult health problems (Hager & Runtz, 2012).
The purpose of the current study was to explore whether internalizing and externalizing behavior problems are more pronounced in the presence of concurrent life stress in young children with, relative to without, a history of PTE exposure. A significant relationship between violence exposure and internalizing and externalizing behavior problems in this sample has been previously reported (Briggs-Gowan et al., 2010). Children were categorized into the following four groups based on history of PTE exposure and evidence of current life stressors for the child or family: PTE-exposed with current life stress, PTE-exposed without current life stress, nonexposed with current life stress, and nonexposed without current life stress. In keeping with a stress-sensitization model, it was hypothesized that children with a history of PTE exposure would show greater internalizing and externalizing problems than nonexposed children, and that children with a history of PTE exposure and the presence of a current life stressor would show the most severe internalizing and externalizing problems. A secondary aim was to examine whether PTSD symptoms were greater among PTE-exposed children with, relative to those without, current life stress. A final aim was to examine whether sex would moderate the relationship between PTE-exposure and current life stress. Gender differences have been reported in posttraumatic outcomes among adults (Brand, 2003) and adolescents (Armour et al., 2011), but consistent with other studies (Alisic, Jongmans, van Wesel, & Kleber, 2011), previous work with this infant/toddler sample showed only small gender differences in PTE exposure and sequelae (Briggs-Gowan et al., 2010). Although gender was not expected to moderate trauma-related stress sensitization in this young age group, if gender differences are detected this early in life, they could provide a basis for studying trajectories leading to adult gender effects.
Method
Participants
The sample comprised 213 2–4-year-old children living with a custodial parent, who was able to participate in English or Spanish. A portion of the sample included referred children recruited from seven child psychiatry and developmental and behavioral pediatric clinics and early intervention sites providing assessment and/or treatment services for mental health and developmental delays. Nonreferred children were recruited from the same communities as the referral sites. A total of 264 parents consented and 221 (83.4%) completed the study protocol. Four children were suspected of having or diagnosed with autism spectrum disorders or global cognitive delays, and three children with incomplete data were excluded. Because it was not the focus of the study, one child with a history of sexual abuse was also excluded.
The mean age of child participants was 2.91 years (SD = 0.56), and most of them were boys (n = 152, 71.4%). The sample was ethnically diverse (46% European American, 27% African American, 15% Hispanic, 3% Asian, 7% multiethnic minority, 2% other). Respondents were biological mothers (87%), biological fathers (4%), adoptive/foster parents (5%), and other relatives (4%). Mean parental age was 34.0 years (SD = 7.7). Of parents, 10% had less than a high school/general equivalency degree, and 69.5% had more than a high school/general equivalency degree: 5.2% with a vocational/trade degree, 7.1% with an associates degree, 15.2% with courses towards a bachelor’s degree, 16.7% with a bachelors degree, 14.3% with a masters degree, and 11% with a professional degree (MD, PhD, JD). Most parents (71%) had a spouse/partner. Approximately 45% of families were living in poverty. Forty-eight percent of children were referred; these children were similar to nonreferred children in sociodemographic characteristics, violence exposure, and noninterpersonal exposures (p > .05).
Procedures
Clinic staff introduced the study to referred families. Nonreferred children were recruited in pediatric clinics by research assistants and posted fliers describing a study interview and developmental assessment for young children. Informed consent was obtained by clinic staff or study personnel. All consented families participated except for two that ultimately withdrew for personal reasons. Parents completed questionnaires and a semistructured child psychiatric interview. Research assistants administered a standardized developmental assessment to children. Ethical guidelines for mandated reporting of maltreatment were followed. No reports to child protective services were necessary because each reported incident already had agency-involvement. Visits lasted approximately 2.5 hr and occurred in participant homes or study offices. Parents received $50 to $80 for their time. Compensation varied because of variations in protocol length, because some measures were included in intake procedures at some sites. All procedures were approved by university institutional review boards.
Measures
Demographics
Parents reported about child age and sex, ethnicity, parental education, marital status, income, and receipt of public assistance. Economic disadvantage was defined as poverty-level income following Federal guidelines based on household income and size and/or receipt of public income assistance.
The Preschool Age Psychiatric Assessment
The Preschool Age Psychiatric Assessment (PAPA), a semistructured interview for developmentally appropriate assessment of DSM-IV symptoms and disorders in 2–5-year-old children (Egger et al., 2006), was administered to parents. Computerized diagnostic algorithms require symptom presence at a frequency beyond levels typical for preschool children. The following disorders were analyzed: oppositional defiant disorder, conduct problems (3 + symptoms of conduct disorder), attention-deficit hyperactivity disorder, separation anxiety, specific phobia, and depressive disorders (major depression, dysthymia, and depression-NOS, i.e., three symptoms). Symptoms are abstracted from the algorithm (0 = absent, 1 = present). The disorders and symptom scales analyzed have established acceptable test–retest reliability, with the exception of specific phobia disorder (κ < .40; Egger et al., 2006). The PTSD section was administered whenever any events were reported.
Exposure to PTEs was assessed with the PTSD section of the PAPA, which assesses lifetime exposure to events involving actual or perceived harm or threat to the life or physical integrity of the child or of another individual (APA, 2000). Noninterpersonal events included vehicular accident, poisoning, accidental burning, near drowning, accidental serious fall, animal attack, natural disaster, and fire. Violence exposure included events directed toward the child (physical abuse, physical violence from a nonfamily member, kidnaping or captivity) or witnessed by the child (events causing or having potential to cause death/severe injury). Witnessed family violence was also assessed with the following two items from the Child Life Events Scale (Carter & Briggs-Gowan, 1998): seeing someone hit, push, or kick a family member, and seeing someone use a weapon to threaten or hurt a family member. The Child Life Events Scale has acceptable reliability and validity (Mongillo et al., 2009).
Stressful Life Events
Exposure in the previous 3 months to “stressful” life events (i.e., events that are potentially stressful but not likely traumatic) was assessed with the PAPA. Examples of these events are as follows: new children in home, parental separation/divorce, new parent figure, moving, childcare change, reduction in standard of living, parental hospitalization, and separation from parent for a week or longer.
Data Analyses
All analyses were conducted using IBM SPSS Statistics (Version 19) software. χ2 goodness-of-fit tests, one-way analyses of variance (ANOVAs), and multivariate analyses of variance (MANOVAs) were used. When specific variables in a measure are conceptually interrelated and moderately intercorrelated, a MANOVA is a more conservative test (type 1 errors are minimized) than conducting a series of univariate ANOVAs (Huberty & Morris, 1989). If a MANOVA was significant, subsequent one-way ANOVAs were conducted to evaluate potential group differences on the individual measures. For significant ANOVAs, pairwise post hoc comparisons were conducted using Hochberg’s (1988) modified step-up Bonferroni procedure. Partial  values are reported for effect sizes in the ANOVA models, where .01 represents a small effect, .06 a medium effect, and .14 a large effect (Cohen, 1988).
values are reported for effect sizes in the ANOVA models, where .01 represents a small effect, .06 a medium effect, and .14 a large effect (Cohen, 1988).
Results
Descriptive Statistics
PTE Exposure
Children were classified as having a history of PTE exposure for the following cases: witness to interpersonal partner violence (11.7%), sexual abuse (0.5%), physical abuse (1.9%), victim of nonfamily violence (0.5%), witness to death/violence (2.8%), witness the use of a weapon (1.4%), fire (0.5%), natural disaster (0.5%), animal attack (0.5%), serious fall (4.2%), burned (6.1%), poisoning (1.9%), vehicle accident (2.3%), sudden death of a loved one (5.6%), and hospitalization (17.8%). Most of trauma-exposed children had one identified traumatic event (65.4%), followed by two events (23.1%), three (9%), and four (2.6%).
Recent Stressors
Recent (past 3 months) stressors were identified as presence of new children in the home (4.2%), parental hospitalization (4.2%), parental separation for >1 week (5.6%), divorce (0.5%), new parental figure (1.4%), moving in past 3 months (8.5%), change in school/daycare (9.4%), significant person moving away (3.8%), death of a pet (4.7%), unsafe neighborhood (1.4%), reduced standard of living (8%), and loss of home (0.5%). The number of recent stressors reported by parents ranged from 0 to 6, with 24.9% having one, 10.8% with two, 1.4% with three, and 0.5% with six stressors. Approximately one in three (37.6%) of the parents reported at least one stressor occurring in the past 3 months.
More PTE-exposed children had experienced a recent stressor than nonexposed children (46.1 vs. 32.6%, respectively), χ2 = 3.88, p = .049, and having two or more stressors was nearly five times as common in the PTE-exposed compared with the nonexposed group (25.6 vs. 5.2%, respectively).
Group Differences in Internalizing and Externalizing Symptomatology
A MANOVA examining internalizing and externalizing symptomatology by group type (no PTE/no stress vs. no PTE/stress, vs. PTE/no stress, vs. PTE/stress), and including the covariates sex, age, poverty, and referral status was statistically significant, Pillai’s trace: F(6,410) = 4.80, p < .001. Subsequent one-way ANOVAs revealed that the groups significantly differed on internalizing, F(3,209) = 6.20, p < .001,  = .08, and externalizing behavior problems, F(3,209) = 8.63, p < .001,
= .08, and externalizing behavior problems, F(3,209) = 8.63, p < .001,  = .11, representing medium to large effects. Hochberg post hoc tests indicated that, consistent with hypothesis one, children with histories of PTE exposure and recent stress (M = 5.50, SE = 0.62) had significantly more internalizing symptoms than the no PTE/no stress (M = 2.80, SE = 0.39), no PTE/stress (M = 2.15, SE = 0.56), and PTE/no stress (M = 3.62, SE = 0.57) groups (which did not differ on this outcome). The PTE/stress group (M = 8.37, SE = 0.78) also had more externalizing symptoms than the no PTE/no stress (M = 4.33, SE = 0.49), no PTE/stress (M = 3.37, SE = 0.71), and PTE/no stress (M = 5.60, SE = 0.72) groups (which also did not differ on this outcome).
= .11, representing medium to large effects. Hochberg post hoc tests indicated that, consistent with hypothesis one, children with histories of PTE exposure and recent stress (M = 5.50, SE = 0.62) had significantly more internalizing symptoms than the no PTE/no stress (M = 2.80, SE = 0.39), no PTE/stress (M = 2.15, SE = 0.56), and PTE/no stress (M = 3.62, SE = 0.57) groups (which did not differ on this outcome). The PTE/stress group (M = 8.37, SE = 0.78) also had more externalizing symptoms than the no PTE/no stress (M = 4.33, SE = 0.49), no PTE/stress (M = 3.37, SE = 0.71), and PTE/no stress (M = 5.60, SE = 0.72) groups (which also did not differ on this outcome).
Sex Differences
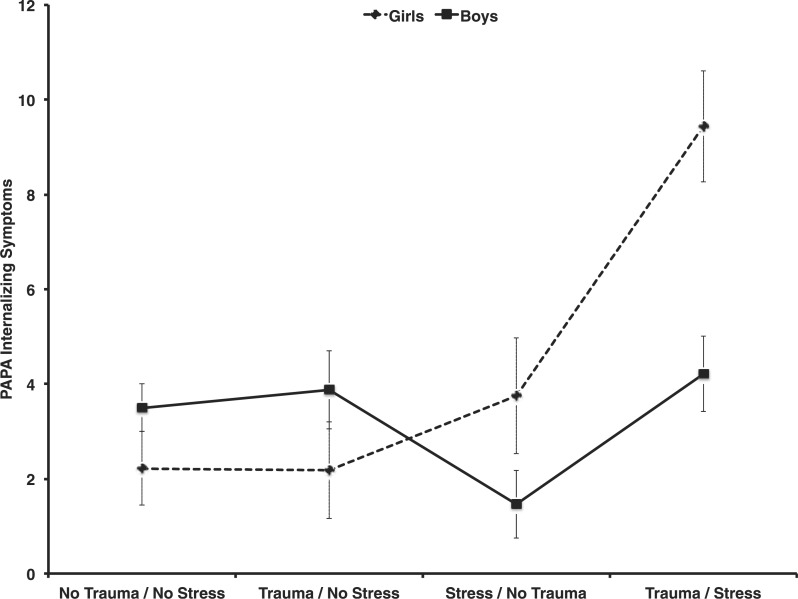
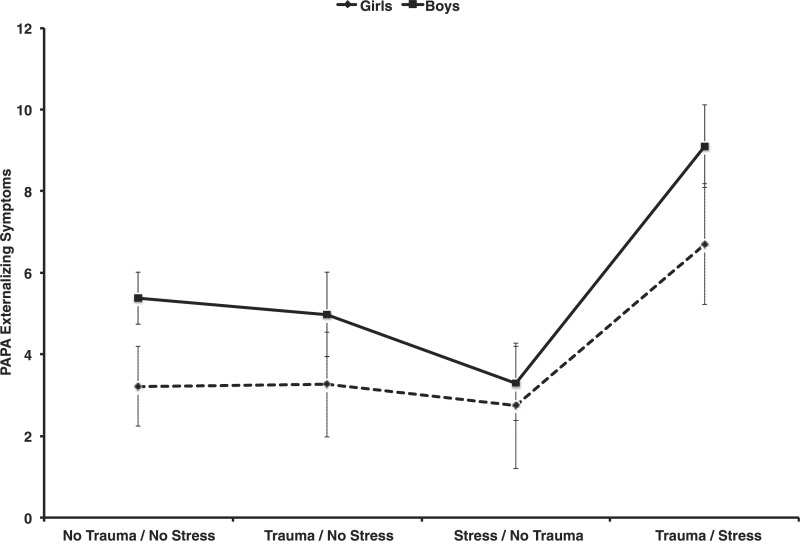
A full factorial MANOVA with internalizing and externalizing symptoms as dependent variables, group type and child sex as independent variables, and including the covariates age, poverty, and referral status was conducted. Results revealed a main effect for group type, Pillai’s trace: F(6,404) = 5.1, p < .001,  = .07, a main effect for child sex, Pillai’s trace: F(2,201) = 8.02, p < .001,
= .07, a main effect for child sex, Pillai’s trace: F(2,201) = 8.02, p < .001,  = .07, and a group type × child sex interaction, Pillai’s trace: F(6,404) = 4.63, p < .001,
= .07, and a group type × child sex interaction, Pillai’s trace: F(6,404) = 4.63, p < .001,  = .06 (see Figures 1 and 2). There was a significant sex main effect for externalizing, F(1,202) = 6.45, p = .012,
= .06 (see Figures 1 and 2). There was a significant sex main effect for externalizing, F(1,202) = 6.45, p = .012,  = .03, but not internalizing symptoms (p > .10), such that male children had greater externalizing symptoms than girls. In addition, a group type × sex interaction was significant for internalizing, F(3,202) = 8.24, p < .001,
= .03, but not internalizing symptoms (p > .10), such that male children had greater externalizing symptoms than girls. In addition, a group type × sex interaction was significant for internalizing, F(3,202) = 8.24, p < .001,  = .11, but not externalizing symptoms (p > .10), such that girls (but not boys) with PTE exposure and current stress had significantly more internalizing symptoms than PTE-exposed girls without a recent stressor and non-trauma-exposed girls with or without a recent stressor. Boys’ internalizing symptoms were unrelated to either PTE exposure or recent stress.
= .11, but not externalizing symptoms (p > .10), such that girls (but not boys) with PTE exposure and current stress had significantly more internalizing symptoms than PTE-exposed girls without a recent stressor and non-trauma-exposed girls with or without a recent stressor. Boys’ internalizing symptoms were unrelated to either PTE exposure or recent stress.
Figure 1.
PAPA internalizing symptoms in girls and boys with and without potential trauma event exposure and recent life stress events.
Figure 2.
PAPA externalizing symptoms in girls and boys with and without potential trauma event exposure and recent life stress events.
Posttraumatic Stress
To examine the possible role of stress sensitivity in PTSD symptoms reported, PTSD symptoms were examined in children with PTE exposure with and without stressors. PTSD symptoms were positively skewed with 54.1% of children with PTE exposure and/or a recent stressor having no symptoms, 31.1% with one, and 14.9% with two or more. A χ2 goodness-of-fit test with group type (PTE/stress vs. PTE/no stress) by number of PTSD symptoms (none vs. one vs. two or more) was nonsignificant, χ2 = 0.83, p = .661, with the proportion of children having one and two or more symptoms in the PTE/stress group (36.1 and 13.9%, respectively) comparable with proportions in the PTE/no stress group (26.3 and 15.8%, respectively).
Discussion
The current study explored a stress sensitization model applied to early life psychopathology in toddlers, with the hypothesis that children with a history of PTE exposure would be at greater risk for internalizing and externalizing problems in the context of current life stress, relative to PTE-exposed children without current life stress and children with no identified PTE history. As hypothesized, children with a history of PTE exposure and current life stress had significantly higher levels of internalizing and externalizing behavior problems (with medium effect sizes) than children in the other groups. In keeping with the stress sensitization model, this pattern suggests that previous PTE exposure may influence young children’s stress response systems, heightening their vulnerability to disruptions in emotional and behavioral regulation when faced with subsequent nontraumatic life stressors. A number of child factors, individually or combined, warrant investigation in future studies as potential contributors to this vulnerability, including greater stress reactivity or differential (e.g., avoidant or emotion-focused) coping skills by the child or the parent(s). Interpersonal factors may play an important role. Transitioning from coregulation to greater self-regulation is a stage-salient task in early childhood. Young children often rely on primary caregivers to help manage emotional, physiological, cognitive, and behavioral responses to stress. Thus, these responses must be considered within the context of the parent–child relationship (De Young, Kenardy, & Cobham, 2011b). Nontraumatic stressors (e.g,. moving, parental hospitalization) may temporarily disrupt the coregulation available from parents and other important caregivers, thus, requiring even better coping skills and self-regulation for adaptation in the face of normative stressors.
PTSD symptoms did not significantly differ among the PTE-exposed or stress-exposed groups, suggesting that the combination of PTE history and current life stress may give rise to internalizing and externalizing problems that are not recognized by parents as characteristic of PTSD. This does not rule out the possibility that posttraumatic stress mediates the pathway from past PTE exposure and children’s responses to nontraumatic stressors. However, longitudinal data are necessary to establish a temporal relationship between PTSD symptoms and later internalizing and externalizing problems that were not available in this study. Previous work from our laboratory suggests that trauma-related symptoms may play an active role, which is underscored by the fact that children with the highest levels of early trauma-related symptoms in a longitudinal birth cohort were nearly seven times more likely to develop later internalizing and externalizing problems (Briggs-Gowan, Carter, and Ford, 2012).
Externalizing behavior problems were greater for boys than girls. This gender discrepancy is often found for children aged ≥5 years (Olson, Sameroff, Kerr, Lopez, & Wellman, 2005) and has been observed in an epidemiologic sample of 1–3-year-olds (Carter, Briggs-Gowan, Jones, & Little, 2003). Notably, despite the mean differences observed in this study, there were substantial elevations in externalizing problems in boys and girls in the PTE/stress group compared with all other groups. Thus, although gender may moderate the development or presentation of children’s externalizing behavior problems, young girls are as susceptible as boys to those problems when they have experienced potentially traumatic events and recent life stressors.
By contrast, a PTE-exposure/current stress interaction effect on internalizing problems was only found for girls, suggesting that current life stressors may not impose the same degree of additional risk for PTE-exposed boys in the internalizing domain as they do for girls. This is consistent with evidence that girls and women are at increased risk for internalizing problems generally, compared with boys and men. There is some, limited, evidence that toddler girls may tend to display more anxiety and fear than boys (Earls, 1980; Carter et al., 2003; Richman et al., 1975). In this study, mean levels of internalizing symptoms were comparable for girls and boys, but their patterns diverged when examined by PTE-stress groupings. Although clearly needing replication and extension with a multimethod, longitudinal design, these findings suggest that trauma-related stress sensitization may contribute to girls’ greater vulnerabilty for internalizing problems (including subsequent PTSD) beginning early in life.
Several clinical implications for clinicians and health professionals working with young children are highlighted by these findings. Firstly, it is critical to inquire about PTE exposure, not only when young children are exhibiting posttraumatic stress symptoms but also when emotional or behavioral problems—which may or may not be readily attributable to PTE exposure—are reported. Although assessing exposure by parent report often yields the most reliable assessment, obtaining information from multiple sources (e.g., child, parent, other caretaker, police report, child protective services) when possible will increase the likelihood of detecting trauma exposure when it exists (Grasso et al., 2009). Although assessing PTE exposure and traumatic stress in young children, many of whom are preverbal, is arguably challenging given the reliance on parent-report and differences in how young children exhibit symptoms (Scheeringa et al., 2003), several psychometrically sound instruments are available (Stover & Berkowitz, 2005). It will be important to make PTE screening standard practice in the pediatric primary care domain, given the high prevalence of PTE exposure in early childhood (Briggs-Gowan et al., 2010) and the frequency with which most young children are seen by pediatric primary care providers. A recent survey of pediatric primary care providers in Connecticut revealed that child abuse and PTSD were among the problems practitioners were least comfortable assessing, diagnosing, or treating (Pidano, Kimmelblatt, & Neace, 2011).
Secondly, consequences of early PTE exposure may not surface until later in a child’s development (including potentially in adolescence and adulthood when gender differences become more apparent). The impact of PTE exposure may take the form of emotional and behavioral problems that may or may not present as symptoms of PTSD. The best approach for addressing these problems given their relationship with past PTE exposure is not fully known. Although a number of evidence-based interventions for treating internalizing and externalizing problems in young children are now available (see reviews by Kaminski, Valle, Filene, & Boyle, 2008; Lieberman & Van Horn, 2009), their effectiveness with trauma-exposed children specifically has not been systematically tested. Future research evaluating enhancements to early childhood psychotherapies addressing trauma-exposure and posttraumatic stress is needed. Study findings suggest that it may be important to structure early childhood therapies to address the combined impact of PTE exposure and current life stressors, rather than focusing separately or exclusively on each domain (Lieberman & Van Horn, 2009).
Thirdly, our findings suggest that PTE-exposed children’s emotional and behavioral problems are associated with co-occurring life stressors (e.g., family financial problems, divorce, relocation). Thus, strengthening these children’s coping skills in the face of life stress may be of particular value. Similarly, helping parents to improve their own coping skills and to facilitate healthy coping in their children may create a home environment in which stress is minimized and more easily managed. Given young children’s reliance on their primary caregivers for help in regulating emotions and arousal, a relational approach focused on promoting children’s feelings of security (e.g., Marvin, Cooper, Hoffman, & Powell, 2002; Dozier et al., 2009) also is likely beneficial. This may be particularly important for PTE-exposed children, many of whom experience dysfunctional interactions with caregivers and more general interpersonal difficulties (Carpenter & Stacks, 2009).
The current study has several limitations. Firstly, all child measures were obtained by parent-report, and as we were unable to covary parents’ own perceived stress and/or psychopathology, we must consider an alternative interpretation of the data—that parents of traumatized children report more internalizing and externalizing behavior problems in the context of identified stressors than do parents of traumatized children without current stress or parents of nontraumatized children with or without current stress. Interestingly, implications for intervention might look similar—in the latter interpretation, families might still benefit from parent support and education programs designed to teach effective strategies for coping with their own stress and their childrens’ stress, which may in turn help to reduce parent perceived burden.
Another study limitation is that trauma-exposure was assessed retrospectively, which may have affected the reliability of parent report and without independent confirmation. Although it is often not feasible to assess trauma exposure prospectively, doing so would contribute to our understanding of current stress as a potential mediator of trauma exposure and later internalizing and externalizing behavior problems in young children. Given these limitations, future research using a longitudinal, multimethod design to examine the effects of exposure to PTEs and stressors on psychopathology, physiological measures of stress response, and coping is warranted.
Conclusion
Young children may be more vulnerable to life stress if they have experienced potentially traumatic events. To maintain an adaptive developmentally trajectory, these children may need enhanced buffering from the effects of stressors that are difficult, but more manageable for other children who do not have the diathesis of PTE exposure. This highlights the need for monitoring of PTE exposures and anticipatory guidance by pediatricians and early childhood interventionists who can identify and help trauma-exposed young children and their parents. Study findings further suggest that girls might be especially vulnerable to developing internalizing symptoms when affected by the combination of PTEs and stressors, and that boys and girls are equally at risk for externalizing problems in the context of this combined adversity. Raising professionals and parents’ awareness of the relationship between PTE exposure and maladaptive responses to life stressors, and assisting parents in using this information in anticipatory guidance, may prove particularly valuable in minimizing or preventing the emergence of internalizing and externalizing behavior problems in young children.
Funding
This work was supported by the National Institute of Mental Health (grant numbers R01MH66645 and R01090301, to M.B.).
Conflicts of interest: None declared.
Acknowledgments
The authors thank study participants for making this work possible. The authors are indepted to collaborators Alice S. Carter, Roseanne Clark, Marilyn Augustyn, Elizabeth Caronna, and Kathleen Hipke for their support, hard work, and commitment to this research.
References
- Alisic E, Jongmans M J, van Wesel F, Kleber R J. Building child trauma theory from longitudinal studies: A meta-analysis. Clinical Psychology Review. 2011;31:736–747. doi: 10.1016/j.cpr.2011.03.001. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders: Text Revision DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Antelman S M, Eichler A J, Black C A, Kocan D. Interchangeability of stress and amphetamine in sensitization. Science. 1980;207:329–331. doi: 10.1126/science.7188649. doi:10.1126/science.7188649. [DOI] [PubMed] [Google Scholar]
- Armour C, Elhai J D, Layne C M, Shevlin M, Durakovic-Belko E, Djapo N, Pynoos R S. Gender differences in the factor structure of posttraumatic stress disorder symptoms in war-exposed adolescents. Journal of Anxiety Disorders. 2011;25:604–611. doi: 10.1016/j.janxdis.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Belsky J, de Haan M. Annual research review: Parenting and children's brain development: The end of the beginning [review] Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2011;52:409–428. doi: 10.1111/j.1469-7610.2010.02281.x. doi:10.1111/j.1469-7610.2010.02281.x. [DOI] [PubMed] [Google Scholar]
- Bland S H, O'Leary E S, Farinaro E, Jossa F. Long-term psychological effects of natural disasters. Psychosomatic Medicine. 1996;58:18–24. doi: 10.1097/00006842-199601000-00004. [DOI] [PubMed] [Google Scholar]
- Brand B. Trauma and women. Psychiatric Clinics of North America. 2003;26:759–779. doi: 10.1016/s0193-953x(03)00034-0. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat H D, Kessler R C, Davis G C. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis G, Andreski P, Federman B, Anthony J C. Epidemiological findings on posttraumatic stress disorder and co-morbid disorders in the general population. In: Dohrenwend B P, editor. Adversity, stress, and psychopathology. New York, NY: Oxford University Press; 1998. pp. 319–328. [Google Scholar]
- Briggs-Gowan M J, Carter A S, Clark R, Augustyn M, McCarthy K J, Ford J D. Exposure to potentially traumatic events in early childhood: Differential links to emergent psychopathology. Journal of Child Psychology and Psychiatry. 2010;51:1132–1140. doi: 10.1111/j.1469-7610.2010.02256.x. doi:10.1111/j.1469-7610.2010.02256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M J, Carter A S, Ford J D. Parsing the effects violence exposure in early childhood: Modeling developmental pathways. [Research Support, N.I.H., Extramural] Journal of Pediatric Psychology. 2012;37:11–22. doi: 10.1093/jpepsy/jsr063. doi:10.1093/jpepsy/jsr063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M J, Ford J D, Fraleigh L, McCarthy K, Carter A S. Prevalence of exposure to potentially traumatic events in a healthy birth cohort of very young children in the northeastern United States. [Research Support, N.I.H., Extramural] Journal of Traumatic Stress. 2010;23:725–733. doi: 10.1002/jts.20593. doi:10.1002/jts.20593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter G L, Stacks A M. Developmental effects of exposure to intimate partner violence in early childhood: A review of the literature. Children and Youth Services Review. 2009;31:831–839. [Google Scholar]
- Carter A S, Briggs-Gowan M J. Child Life Events Screener. Unpublished manuscript; 1998. [Google Scholar]
- Carter A S, Briggs-Gowan M J, Jones S M, Little T D. The Infant-Toddler Social and Emotional Assessment (ITSEA): Factor structure, reliability, and validity. Journal of Abnormal Child Psychology. 2003;31:495–514. doi: 10.1023/a:1025449031360. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth S L. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Costello E J, Erkanli A, Fairbank J A, Angold A. The prevalence of potentially traumatic events in childhood and adolescence. Journal of Traumatic Stress. 2002;15:99–112. doi: 10.1023/A:1014851823163. [DOI] [PubMed] [Google Scholar]
- Cougle J R, Resnick H, Kilpatrick D G. Does prior exposure to interpersonal violence increase risk of PTSD following subsequent exposure? Behaviour Research and Therapy. 2009;47:1012–1017. doi: 10.1016/j.brat.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darwish D, Esquivel G B, Houtz J C, Alfonso V C. Play and social skills in maltreated and non-maltreated preschoolers during peer interactions. Child Abuse & Neglect. 2001;25:13–31. doi: 10.1016/s0145-2134(00)00228-3. doi:10.1016/s0145-2134(00)00228-3. [DOI] [PubMed] [Google Scholar]
- De Young A C, Kenardy J A, Cobham V E. Diagnosis of posttraumatic stress disorder in preschool children. [Research Support, Non-U.S. Gov't] Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division. 2011a;40:375–384. doi: 10.1080/15374416.2011.563474. doi:10.1080/15374416.2011.563474. [DOI] [PubMed] [Google Scholar]
- De Young A C, Kenardy J A, Cobham V E. Trauma in early childhood: A neglected population. Clinical Child and Family Psychology Review. 2011b;14:231–250. doi: 10.1007/s10567-011-0094-3. doi:10.1007/s10567-011-0094-3. [DOI] [PubMed] [Google Scholar]
- Dougall A L, Herberman H B, Delahanty D L, Inslicht S S, Baum A. Similarity of prior trauma exposure as a determinant of chronic stress responding to an airline disaster. Journal of Consulting and Clinical Psychology. 2000;68:290–295. doi: 10.1037//0022-006x.68.2.290. doi:10.1037/0022-006x.68.2.290. [DOI] [PubMed] [Google Scholar]
- Dozier M, Lindhiem O, Lewis E, Bick J, Bernard K, Peloso E. Effects of a foster parent training program on young children’s attachment behaviors: Preliminary evidence from a randomized clinical trial. Child and Adolescent Social Work Journal. 2009;26:321–332. doi: 10.1007/s10560-009-0165-1. doi:10.1007/s10560-009-0165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earls E. Prevalence of behavior problems in 3-year-old children: A cross-national replication. Archives of General Psychiatry. 1980 doi: 10.1001/archpsyc.1980.01780230071010. [DOI] [PubMed] [Google Scholar]
- Egger H L, Erkanli A, Keeler G, Potts E, Walter B K, Angold A. Test–retest reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Farver J A, Xu Y, Eppe S, Fernandez A, Schwartz D. Community violence, family conflict, and preschoolers’ socioemotional functioning. Developmental Psychology. 2005;41:160–170. doi: 10.1037/0012-1649.41.1.160. [DOI] [PubMed] [Google Scholar]
- Grasso D, Boonsiri J, Lipschitz D, Guyer A E, Houshyar S, Douglas-Palumberi H, Massey J, Kaufman J. Posttraumatic stress disorder: The missed diagnosis. Child Welfare. 2009;88:157–176. [PMC free article] [PubMed] [Google Scholar]
- Hager A D, Runtz M G. Physical and psychological maltreatment in childhood and later health problems in women: An exploratory investigation of the roles of perceived stress and coping strategies. Child Abuse and Neglect. 2012;36:393–403. doi: 10.1016/j.chiabu.2012.02.002. [DOI] [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley S E. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;68:782–787. [PubMed] [Google Scholar]
- Harkness K L, Bruce A E, Lumley M N. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of Abnormal Psychology. 2006;115:730–741. doi: 10.1037/0021-843X.115.4.730. [DOI] [PubMed] [Google Scholar]
- Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–802. [Google Scholar]
- Huberty C J, Morris J D. Multivariate analysis versus multiple univariate analyses. Psychological Bulletin. 1989;105:302–308. doi:10.1037/0033-2909 .105.2.302. [Google Scholar]
- Kaminski J W, Valle L A, Filene J H, Boyle C L. A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology. 2008;36:567–589. doi: 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Sonnega A, Bromet E, Hughes M. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- King D W, King L A, Foy D W. Prewar factors in combat-related posttraumatic stress disorder: Structural equation modeling with a national sample of female and male Vietnam veterans. Journal of Consulting and Clinical Psychology. 1996;64:520–531. doi: 10.1037//0022-006x.64.3.520. doi:10.1037/0022-006x.64.3.520. [DOI] [PubMed] [Google Scholar]
- Lieberman A F, Van Horn P. Child-parent psychotherapy: A developmental approach to mental health treatment in infancy and early childhood. In: Zeanah C H Jr., editor. Handbook of infant mental health. New York, NY: Guilford Press; 2009. pp. 439–449. [Google Scholar]
- Linares L O, Heeren T, Bronfman E, Zuckerman B, Augustyn M, Tronick E. A mediational model for the impact of exposure to community violence on early child behavior problems. Child Development. 2001;72:639–652. doi: 10.1111/1467-8624.00302. [DOI] [PubMed] [Google Scholar]
- Manly J T, Kim J E, Rogosch F A, Cicchetti D. Dimensions of child maltreatment and children's adjustment: Contributions of developmental timing and subtype. Development and Psychopathology. 2001;13:759–782. [PubMed] [Google Scholar]
- Marvin R S, Cooper G, Hoffman K, Powell B. The Circle of Security project: Attachment-based intervention with caregiver-pre-school child dyads. Attachment & Human Development. 2002;4:107–124. doi: 10.1080/14616730252982491. [DOI] [PubMed] [Google Scholar]
- McLaughlin K A, Conron K J, Koenen K C, Gilman S E. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] Psychological Medicine. 2010;40:1647–1658. doi: 10.1017/S0033291709992121. doi:10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milot T, Ethier L S, St-Laurent D, Provost M A. The role of trauma symptoms in the development of behavioral problems in maltreated preschoolers. [Research Support, Non-U.S. Gov’t] Child Abuse & Neglect. 2010;34:225–234. doi: 10.1016/j.chiabu.2009.07.006. doi:10.1016/j.chiabu.2009.07.006. [DOI] [PubMed] [Google Scholar]
- Milot T, St-Laurent D, Ethier L S, Provost M A. Trauma-related symptoms in neglected preschoolers and affective quality of mother-child communication. [Comparative Study Research Support, Non-U.S. Gov’t] Child Maltreatment. 2010;15:293–304. doi: 10.1177/1077559510379153. doi:10.1177/1077559510379153. [DOI] [PubMed] [Google Scholar]
- Mongillo E A, Briggs-Gowan M J, Ford J D, Carter A S. Impact of traumatic life events in a community sample of toddlers. Journal of Abnormal Child Psychology. 2009;37:455–468. doi: 10.1007/s10802-008-9283-z. [DOI] [PubMed] [Google Scholar]
- Olson S, Sameroff A J, Kerr D, Lopez N, Wellman H. Developmental foundations of externalizing problems in young children: The role of effortful control. Development and Psychopathology. 2005;17:25–45. doi: 10.1017/s0954579405050029. [DOI] [PubMed] [Google Scholar]
- Pidano A E, Kimmelblatt C A, Neace W P. Behavioral health in the pediatric primary care setting: Needs, barriers, and implications for psychologists. Psychological Services. 2011;8:151–165. doi:10.1037/a0019535. [Google Scholar]
- Post R M, Weiss S R. Sensitization and kindling phenomena in mood, anxiety, and obsessive‚ Äìcompulsive disorders: The role of serotonergic mechanisms in illness progression. Biological Psychiatry. 1998;44:193–206. doi: 10.1016/s0006-3223(98)00144-9. doi:10.1016/s0006-3223(98)00144-9. [DOI] [PubMed] [Google Scholar]
- Scheeringa M S, Zeanah C H, Myers L, Putnam F W. New findings on alternative criteria for PTSD in preschool children. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:561–570. doi: 10.1097/01.CHI.0000046822.95464.14. [DOI] [PubMed] [Google Scholar]
- Smid G E, van der Velden P G, Lensvelt-Mulders G J, Knipscheer J W, Gersons B P, Kleber R J. Stress sensitization following a disaster: A prospective study. Psychological Medicine. 2012;42:1675–1686. doi: 10.1017/S0033291711002765. [DOI] [PubMed] [Google Scholar]
- Sroufe L A, Egeland B, Carlson E A, Collins W A. The Development of the Person: The Minnesota Study of Risk and Adaptation from Birth to Adulthood. New York, NY:: The Guildford Press.; 2005. [Google Scholar]
- Stover C S, Berkowitz S. Assessing violence exposure and trauma symptoms in young children: A critical review of measures. Journal of Traumatic Stress. 2005;18:707–717. doi: 10.1002/jts.20079. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Serices, Administration on Children, Youth, and Families. Child Maltreatment 2005. Washington, DC: U.S. Government Printing Office; 2006. [Google Scholar]