Summary
Two patients with dural sinus stenosis of different causes presenting with refractory benign intracranial hypertension were confirmed by angiogram. Stent-assistant angioplasty was used to dilate the stenosed sinusesand led to prompt clinical improvement. Relative long-term follow-up showed good patency of the stented sinuses.
Key words: cerebral venous stenosis, treatment, stent, angioplasty
Introduction
The use of stent-assisted angioplasty in the coronary circulation, extracranial arteries, or even recently, intracranial arteries has improved clinical outcomes and kept long-term patency. Because of the tortuous anatomy of the jugular bulb and/or venous conflux and the risk of early occlusion, dural sinus stenting remains controversial. We treated two patients with sinus stenosis by successfully implanting the stents within the lesioned sinus; relative long-term follow-up showed good results.
Case 1
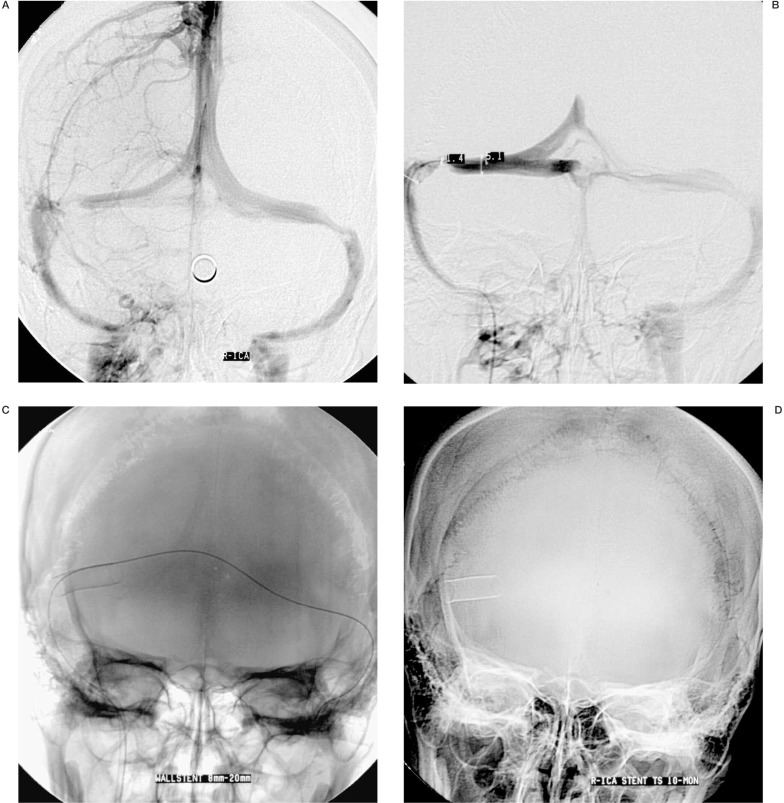
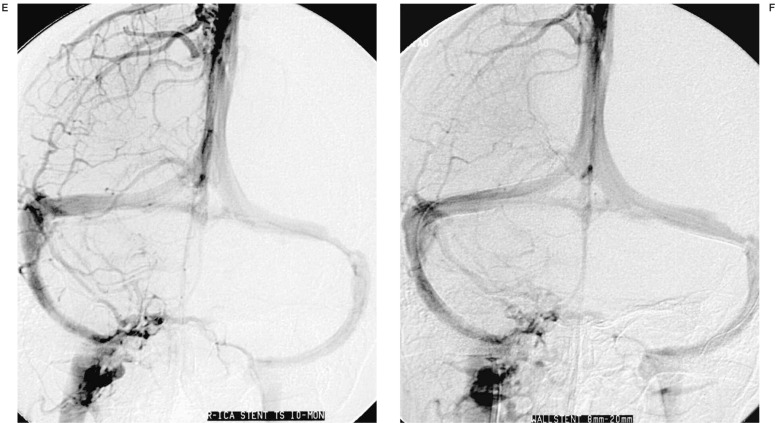
A 32-year-old woman complained of bilateral visual blurring and mild headache, fundus-copy showed bilateral papilloedema, pressure of lumber puncture was more than 350 mmH2O. MRI disclosed mild abnormal high signals in her bilateral transverse sinus. Angiography was performed by transfemoral route 20 days after the symptoms occurred and the patient accepted full heparinization during the procedure. The cerebral artery system was normal but there was mild stagnation of cortical vein drainage at the early venous phase, the obvious lesions confirmed were high stenosis of her bilateral transverse venous sinus, the right side more severe than the left. An arterial thrombolysis was given via the right ICA, a total of 80,0000 IU urokinase were given at a speed of 5,000 IU/min, anticoagulation therapy was given by Warfarin after the procedure. The patient felt mild improvement of symptoms within several days, but reversed to previous conditions later. The pressure of lumber puncture remained unchanged. The patient accepted bilateral puncture via transfemoral route on one side and transfemoral venous route on the other. Selective dural sinus angiography showed the stenosis remained, thrombolysis within the sinus at the site of stenosis was decided, a total of 100,0000 IU urokinase were given, repeat dural sinus angiography showed no change. We decided to implant a stent at the bilateral transverse sinuses after the failure of thrombolysis, pressure gradient between the two sides of the stenosed segment was 40 mmHg, a 9 F guiding catheter was navigated with 0.018 in microwire to the proximal rightjugular bulb, the microwire was passed through the stenosed transverse sinus and navigated to the opposite jugular bulb in order to give strong support of stent delivery. A self-expanded Wallsten stent of 8 × 20 mm was selected after correct calculation using a calibrated stainless steel ball. The stent transferring system was successfully passed through the right jugular bulb but failed to reach the other side because it was difficult to pass the sinus conflux. The stent had to be deployed in the ipisilateral stenosed transverse sinus. Instant angiography via right ICA showed good patency of the stented sinus. The pressure gradient between the two sides of the stented sinus decreased to 4 mmHg. It astonished us that the patient told us her visual blurring improved as soon as the stent was deployed. Anticoagulation was continued using Warfarin for three months. The patient completely recovered three months afterthe procedure; ten months angiography follow-up showed the stent kept in the original site and good patency of the stented sinus.
Figure 1.
Lateral venous phase and venous angiography showed bilateral transverse sinus stenosis (A,B), a 9 F guiding catheter was navigated with a 0.018 in microwire to the proximal right jugular bulb, the microwire was passed through the stenosed transverse sinus and navigated to the opposite jugular bulb, a self-expanded Wallsten stent of 8 × 20 mm was deployed at the stenosis site of right transverse sinus (C), the stenosis segment was completely dilated (D).Ten months angiographic follow-up showed the stent located at the original deployed site and the stented sinus kept good patency (E,F).
Case 2
A 46-year-old man complained of visual blurring and intermittent headache for two months. MRI disclosed a small parafalcial meningioma located near the posterior third of the supersagittal sinus (SSS), MRV showed the SSS was not compressed by the tumor. A craniotomy was performed and the tumor was completely removed. During the procedure, the SSS near the tumor was injured and repaired. However, the symptoms of the patient worsened after the operation. Repeat MRV showed the occlusion of the posterior third of the SSS. Pressure of lumber puncture increased to 350 mmH2O. Cerebral artery angiography showed the occlusion of the posterior third of the SSS, superselective venography showed high stenosis of the posterior third of the SSS, super-selective thrombolysis at the lesion site was given, a total of 80,0000 IU urokinase was infused at the speed of 5,000 IU per minute, repeat angiography showed no change of the stenosed sinus. Angioplasty was decided to dilate the lesion.
A 6F guiding catheter (Envoy, cordis) was navigated with a 0.035 in guiding wire to the the right jugular bulb. A 0.014 in microwire (Luge, Boston Scientific Ltd) was passed through the narrowed sinus, its soft tip reached the anterior sagittal sinus, because the length of stenosed segment was too long there was no single coronary stent long enough, two balloon-expanded coronary stents (BX sonic, 4 × 23 mm, and 4 × 28 mm, Cordis Co.) were deployed. Pressure used to deploy the stent was 8 atm respectively. Pressure was increased slowly to avoid sinus rupture. Instant post-procedure angiography showed the stenosed segment was fully dilated. Artery angiography via bilateral ICA showed the venous reflux changed to normal. Anticoagulation using heparin was administered for three days (the range of APTT is kept within 60-80 seconds), antiplatlet therapy with aspirin (300 mg per day) plus clopidogrel (250 mg per day) were continued for threemonths, angiographic follow-up after three months showed the stented sinus kept open. Clinical follow-up found the patient completely recovered.
Discussion
Dural sinus stenosis may cause intracranial hypertension whose pathogenesis is unclear. The reasons for sinus stenosis of in case 2 was because of injury to the sinus during tumor excision. Case 1 may have had a pseudo tumor mentioned by some authors 5, because she failed not only anticoagulation but transarterial and transvenous thrombolysis. Stents may be useful not only for arterial stenosis but also to treat venous sinus stenosis 1,4. Three reports, by Malek et Al, Vilela et Al and Marks et Al 2,3,5, point to the usefulness of angioplasty and stenting of venous sinuses in helping to reestablish venous patency and function. Recently, Higgins et Al 1 reported treating a patient with refractory benign intracranial hypertension by dilation of one of the transverse venous sinuses with a stent and the results showed striking symptomatic improvement.
One of the challenges is selecting and transferring the stent. The stent must pass through the complex tortuous anatomy of the jugular bulb (transverse sinus lesions) or sinus conflux (superior sagittal sinus lesion), the selected stent must be not only soft enough, but have a large enough diameter because the diameters of dural sinuses are often larger, diameters of the soft flexible balloon-expanded stent are sometimes smaller, our case 2 is a special case in which the narrowed sinus was small enough to use this kind of stent. Usually the relative stiff self-expanded stent system must be used, but this kind of stent is not easy to position.
Another problem with dural sinus stenting is long-term effectiveness. It is usually considered that the stented sinus will occlude because of thrombosis.
However, the outcome of our two cases showed good patency at the follow-up period of three ~ ten months. Clinical follow-up also showed encouraging results and the symptoms of these two patients improved quickly after the procedure. They completely recovered at the follow-up period.
Post procedure medication included anticoagulation therapy and antiplatelet therapy to prevent re-thrombosis within the stent.
References
- 1.Higgins JN, Owler BK, et al. Venous sinus stenting for refractory benign intracranial hypertension. Lancet. 2002;359(9302):228–230. doi: 10.1016/S0140-6736(02)07440-8. [DOI] [PubMed] [Google Scholar]
- 2.Malek AM, Higashida RT, et al. Endovascular recanalization with balloon angioplasty and stenting of an occluded occipital sinus for treatment of intracranial venous hypertension: technical case report. Neurosurgery. 1999;44:896–901. doi: 10.1097/00006123-199904000-00133. [DOI] [PubMed] [Google Scholar]
- 3.Marks MP, Dake MD, et al. Stent placement for arterial and venous cerebrovascular disease: preliminary experience. Radiology. 1994;191:441–446. doi: 10.1148/radiology.191.2.8153318. [DOI] [PubMed] [Google Scholar]
- 4.Murphy KJ, Gailloud P, et al. Endovascular treatment of a Grade IV transverse sinus dural arteriovenous fistula by sinus recanalization, angioplasty, and stent placement: technical case report. Neurosurgery. 2000;46:497–501. doi: 10.1097/00006123-200002000-00048. [DOI] [PubMed] [Google Scholar]
- 5.Vilela P, Willinsky RA, ter Brugge K. Treatment of intracranial venous occlusive disease with sigmoid sinus angioplasty and stent placement in a case of infantile multifocal dural arteriovenous shunts. Interventional Neuroradiology. 2001;7:51–60. doi: 10.1177/159101990100700108. [DOI] [PMC free article] [PubMed] [Google Scholar]