Abstract
Background
Problems persist with surrogate decision making in intensive care units, leading to distress for surrogates and treatment that may not reflect patients’ values.
Objectives
To assess the feasibility, acceptability, and perceived effectiveness of a multifaceted, nurse-led intervention to improve surrogate decision making in intensive care units.
Study Design
A single-center, single-arm, interventional study in which 35 surrogates and 15 physicians received the Four Supports Intervention, which involved incorporating a family support specialist into the intensive care team. That specialist maintained a longitudinal relationship with surrogates and provided emotional support, communication support, decision support, and anticipatory grief support. A mixed-methods approach was used to evaluate the intervention.
Results
The intervention was implemented successfully in all 15 patients, with a high level of completion of each component of the intervention. The family support specialist devoted a mean of 48 (SD 36) minutes per day to each clinician-patient-family triad. All participants reported that they would recommend the intervention to others. At least 90% of physicians and surrogates reported that the intervention (1) improved the quality and timeliness of communication, (2) facilitated discussion of the patient’s values and treatment preferences, and (3) improved the patient-centeredness of care.
Conclusions
The Four Supports Intervention is feasible, acceptable, and was perceived by physicians and surrogates to improve the quality of decision making and the patient-centeredness of care. A randomized trial is warranted to determine whether the intervention improves patient, family, and health system outcomes.
One in 5 Americans die in or shortly after discharge from an intensive care unit (ICU).1 An expanding body of literature documents that communication between clinicians and patients’ family members is often poor in ICUs.2–12 These deficiencies are associated with life-support decisions that may be inconsistent with patients’ goals and preferences,13–15 clinician-family conflict,5 and high rates of adverse psychological outcomes among surrogates.3,16 There is also mounting evidence that clinicians experience negative consequences of conflicts about end-of-life care in ICUs, such as moral distress and burnout.17–19 Although the problems with communication and decision making in ICUs have been recognized for several decades, there remains a lack of evidence-based, generalizable interventions to improve this aspect of care.
Several interventions tested in large, well-funded trials did not improve patients’ or surrogates’ outcomes. The intervention tested in the SUPPORT trial provided physicians with prognostic estimates and information about patients’ previously expressed treatment preferences.20 It did not affect patients’ outcomes or intensity of treatment near the end of life. Curtis and colleagues21 tested a multicomponent quality improvement intervention that centered on educating clinicians and providing performance feedback, as well as implementation of systems-level support to improve palliative care in ICUs. The intervention had no effect on most key palliative care process measures and patients’ outcomes. In separate studies, Daly et al22 and Lilly et al23 tested an intervention involving regular, structured family meetings conducted by the ICU team. Although the intervention was associated with shorter length of stay in a single-center study, a subsequent multicenter study showed no changes in length of stay or treatment limitation decisions. The Critical Care Family Needs Assessment Program (CCFNAP), a quality improvement initiative funded by the CHEST Foundation, sought to improve families’ overall experiences in the ICU by increasing communication with clinicians, providing educational materials, and improving the physical environment of the ICU. In a before-after quasi-experimental study, family ratings of the quality of communication with ICU clinicians were not improved, nor was there evidence of change in ICU length of stay.24,25
Conceptually, these interventions focused largely—but not exclusively—on increasing the frequency of communication between clinicians and patients’ families and the clarity of information provided. Although these are important elements of care, empirical research suggests that decisions by surrogates can also be heavily influenced by emotional, moral, and interpersonal considerations. 26–30 These observations parallel an evolution in the field of decision psychology away from viewing decision makers as simply “rational actors” and toward viewing them as relying on both analytical reasoning and also more intuitive, emotion-based forms of reasoning (eg, dual process reasoning).31,32
No interventions to improve surrogate decision making in ICUs have been explicitly grounded in dual-process theories of decision making. A small but growing body of work suggests that proactive palliative care consultation or ethics consultation—interventions that presumably provide some degree of both cognitive and emotional support to surrogates—may improve outcomes for patients and their families.33,34 Although encouraging, such interventions raise several concerns. First, they may not be feasible in the large numbers of hospitals that do not have well-staffed palliative care consultation services or ethics consultation services. Second, because the interventions generally have not been described in detail (eg, the frequency and content of interaction with families), it is unclear whether such interventions could be implemented at other institutions. Third, many ICU clinicians conceptualize family support as central to their professional role and may be reluctant to cede these responsibilities to consultants.
One approach to overcome these limitations is to add to the ICU team a specially trained family support specialist (FSS) to complement and extend the support provided by the other ICU clinicians. However, such an approach raises questions about feasibility and acceptability. Specifically, given the complexity of ICUs, it is unknown whether it is logistically possible to implement this new role on the care team. It is also unknown whether it will be acceptable to families and clinicians to have some elements of decision counseling and support provided by someone other than patients’ physicians and nurses.
Therefore, we conducted a single-center, single-arm interventional study to test whether a nurse-led, multicomponent family support intervention is feasible, acceptable, and perceived as beneficial by physicians and surrogate decision makers.
Methods
Study Population and Enrollment
This was a single-center, single-arm, interventional study. The surrogate decision makers of incapacitated patients with acute respiratory failure and a high risk of death or severe functional impairment were recruited from August 2010 to December 2010 from a neurological ICU at University of Pittsburgh Medical Center. A research coordinator screened daily for patients who met the following criteria: (1) age greater than 50 years, (2) lacking decision-making capacity, score of at least 25 on the Acute Physiology and Chronic Health Evaluation (APACHE) II or a greater than 50% chance of long-term severe functional impairment (as judged by the patients’ attending physician). Exclusion criteria included (1) lack of a surrogate decision maker who was able to speak English and complete a written questionnaire and (2) patient is awaiting organ transplantation.
Surrogates who met enrollment criteria received a brief introduction to the study by the bedside nurse after the patient’s attending physician gave permission for staff to approach the family. Surrogates willing to hear about the study met with the research staff in a private room. Written informed consent was obtained. Surrogates provided proxy consent for the patients. Physicians also provided written informed consent for their study participation. Surrogates were paid $20 for study participation and physicians were paid $10. The institutional review board approved all study procedures.
Theoretical Grounding of the Intervention
The intervention is grounded in the dual-process theory of decision making, which postulates that decision making involves both cognitive and emotional processes, both of which can lead to poor quality decisions if they are not attended to.31,32 The Cognitive Emotional Decision Making framework, which is rooted in dual-process theory and developed specifically for medical decision making, views medical decisions as influenced by not only the emotional and cognitive issues that arise from the health threat, but also those issues that arise from being required to make difficult, highly consequential decisions.31 Accordingly, interventions to improve decision making should attend not only to the cognitive and emotional considerations in determining the most appropriate treatment plan, but also the difficulties encountered in the role of decision maker.
To successfully implement a multicomponent intervention in the complex ICU environment, we used the Donabedian structure-process-outcome framework to organize potential barriers to high-quality decision making.35–37 Poor quality surrogate decision making may result from the interplay of cognitive and emotional factors within and between clinicians and surrogates, process of care factors, and organizational factors. For example, the acute threat to their loved one and the foreign nature of the ICU may compromise surrogates’ ability to understand and process the medical information needed to make patient-centered decisions. Physicians may be reluctant to talk about prognosis and goals of care and may not have the skills or disposition to attend to all important aspects of these conversations.10,12,38 Structural and process-of-care attributes of ICUs also pose barriers to good surrogate decision making, such as the shift-based nature of work in ICUs, and the very substantial constraints on physicians’ time because of high patient volume and acuity. A more comprehensive overview of the potential barriers to optimal surrogate decision making in ICUs has been published previously.39
Midrange theories and empirical research in ICUs support the theoretical assertion that cognitive and emotional considerations are highly important to effective surrogate decision making27–29 and that organizational and process-of-care factors also pose important barriers to optimal communication and decision making.40,41 Therefore, the intervention is specifically designed to provide to surrogates emotional support, cognitive decisional support, and also to overcome process-of-care barriers to high-quality communication and decision making.
We designed the intervention to be administered by an ICU nurse for both conceptual and pragmatic reasons. Conceptually, the nursing ethic of caring and family-centeredness makes nurses well suited to help families with this aspect of care.42,43 In addition, the clinical nurse’s presence in the ICU creates opportunities to work with families in ways that are not feasible for physicians. Pragmatically, testing the intervention as administered by an ICU nurse selected from within the existing ICU staff creates a potentially more generalizable intervention compared to having the intervention administered by some-one with more advanced skills, but who may not be as available in some ICUs, such as a psychologist, health coach, or palliative care consultant.
Description of Intervention
The Four Supports Intervention is a multifaceted intervention involving the addition of a trained FSS to the usual clinical team. The intervention consists of multiple components that are tailored to the needs of individual families and clinical teams. In broad terms, the intervention delivers 4 kinds of support: emotional support, communication support, decision support, and anticipatory grief support, each of which is summarized in the following paragraphs.
Emotional Support
The central element of emotional support arises from the FSS forming and maintaining a longitudinal, empathic relationship with the family. The FSS provides empathy, a space to focus on the families’ experience and needs, and assists the family to understand the routines of the ICU. In addition, the interventionist provides emotional support to families before, during, and after meetings in which prognosis and goals of care are discussed, as well as during the patient’s dying process.
Communication Support
The FSS arranges and assists in delivering early, frequent, and supportive communication between the family and clinical team. A meeting is arranged within 48 hours of study enrollment and at regular intervals thereafter. The interventionist prepares families for these meetings by assisting them to create a list of their key questions and concerns. During the meetings, the FSS ensures that the families’ main questions are answered and works to prevent misunderstandings about the patient’s values, prognosis, and available treatment pathways.
Decision Support
The decision support provided to families consists of (1) clarification of the role of the surrogate, (2) anticipatory guidance about the types of questions likely to be raised by clinicians, (3) elicitation of families’ understanding of the medical situation and likely outcomes, (4) guidance in clarifying the patient’s values and treatment preferences in the setting of critical illness, and (5) creating early and frequent opportunities for families to consider the patient’s goals. The decision support provided to clinicians consists of written and verbal feedback about the surrogates’ main questions, their understanding of the prognosis, their preferred role in decision making, and the family’s report of the patient’s values and health care preferences (see Appendix). The interventionist also takes steps to ensure that the patient’s prognosis, values, and available treatment options are adequately discussed during clinician-family meetings.
Anticipatory Grief Support
When there is uncertainty about the patient’s outcome, families are encouraged to think about what it would mean to “hope for the best and prepare for the worst,” which is a strategy advocated to help families begin to prepare emotionally for the possibility of death at a time that they are also hoping for recovery.44 If it becomes clear that a patient is going to die, either because they are moribund or because of a decision to withdraw life support, families are offered the opportunity to gather at the bedside for a ceremony to honor the patient’s life and to say good-bye. These encounters are modeled after life review/closure sessions that were originally developed for patients with terminal illnesses and adapted to the needs of surrogates rather than patients.45 The interventionist also offers to stay with the family during the dying process and provides emotional support.
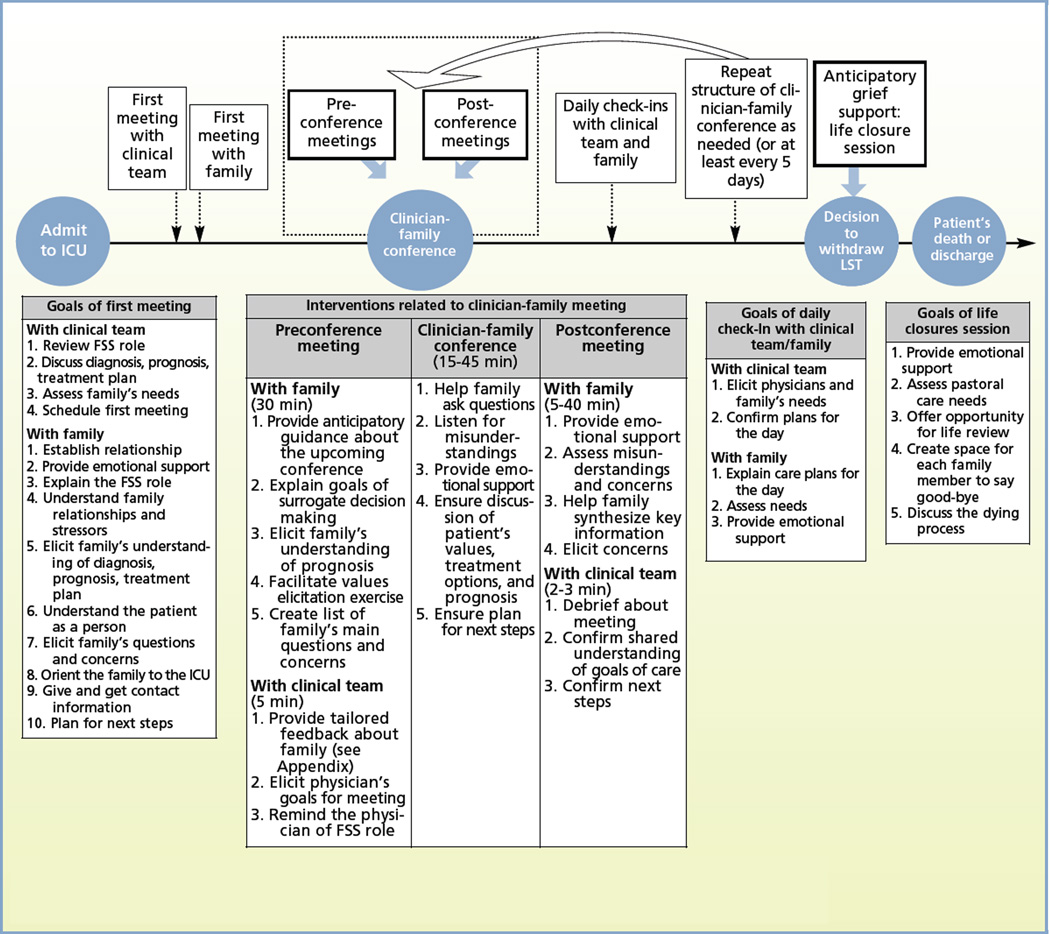
The 4 types of support are implemented in parallel through a series of encounters with the family and the clinical team, including initial individual meetings, preconference meetings with the family and clinicians, unstructured clinician-family meetings in which the FSS participates, postconference meetings, daily check-ins, and anticipatory grief sessions. The temporal flow and content of each of these meetings are summarized in the Figure. To accommodate the needs of participants who were unable to be in the hospital, intervention procedures were occasionally implemented by telephone, but every effort was made to maximize face-to-face encounters.
Figure.
The Four Supports Intervention: timeline of procedures.
Abbreviations: FSS, family support specialist; ICU, intensive care unit; LST, life-sustaining treatment.
Training of Study Interventionist
Before joining the study team, the nurse interventionist had been a clinical nurse for 3 years, all of which were in the study ICU. She had no additional expertise beyond her nursing training and clinical experience in interacting with surrogate decision makers. The study interventionist underwent approximately 40 hours of training in intervention procedures and research procedures. Training techniques included supervised reading and discussion of the intervention manual, role playing, and structured feedback from the investigator team. The interventionist also shadowed experts in nursing, social work, and palliative care medicine during interactions with families in ICUs. Proficiency in study procedures was assessed by investigators (D.B.W. and R.M.A.) through direct observation during a role-playing exercise as well as direct questioning of the interventionist on key aspects of the intervention.
Assessment of Intervention Fidelity
Intervention fidelity was assessed through (1) quarterly assessment of the nurse interventionist’s adherence to intervention principles in simulated family interactions, in which the senior author evaluated the nurse interventionist; (2) measurement of whether the planned study encounters occurred for each enrolled patient (eg, preconference meetings, postconference meetings, and daily check-ins); and (3) semistructured interviews with clinicians and surrogates in which they described their interactions with the FSS. Funding limitations precluded audio recording of the encounters and content analysis.
Measures
Basic demographic information was collected from surrogates, patients, and the attending physician. Clinical details were prospectively collected from the medical record.
Feasibility
Feasibility of the intervention was assessed by measuring the enrollment rate and the degree to which study procedures were successfully implemented. Daily, the study interventionist recorded the type, content, and duration of interactions with clinicians and surrogates. Feasibility of long-term follow-up was assessed by response rates to the 3-month follow-up call.
Acceptability and Perceived Effectiveness
Acceptability was quantitatively measured by assessing the proportion of subjects who dropped out of the study. In addition, a random sample of 30% of subjects (5 physicians and 10 surrogates) completed a semistructured interview and questionnaire about the acceptability and perceived effectiveness of the intervention. This interview was conducted approximately 1 week after enrollment for surrogates and after the patient’s death/discharge for physicians. Acceptability was measured quantitatively by a single item eliciting whether subjects would recommend the intervention to a friend. It was assessed qualitatively by whether surrogates expressed dissatisfaction with any aspect of the intervention during the interview. Perceived effectiveness was assessed with a 10-item questionnaire addressing subjects’ perceptions of whether the intervention increased clarity about the patient’s values, improved communication, and improved the patient-centeredness of care (see Table 3).
Table 3.
Acceptability and perceived effectiveness of the intervention
| Score, mean (SD) |
||
|---|---|---|
| Variable | Physician (n = 5) | Family (n = 10) |
| How well did the intervention facilitate communication? | 4.4 (0.5) | 4.4 (0.9) |
| 1 (lowest) to 5 (highest) Likert scale | ||
| How much did the family support specialist appear to integrate with the clinical team? | 4.2 (0.4) | 4.1 (0.8) |
| 1 (lowest) to 5 (highest) Likert scale | ||
| Did the family support specialist ease the subjects’ experience? | 4.8 (0.4) | 4.6 (0.9) |
| 1 (lowest) to 5 (highest) Likert scale | ||
| Compared to normal communication with families, did the physician spend the same, more, or less time with the family? | 2.8 (0.4) | — |
| 1 (less than normal) to 3 (more than normal) Likert scale | ||
| Did the intervention improve: | Percentage answering yes | |
| - the quality of communication? (yes/no) | 100 | 100 |
| - the timeliness of communication? (yes/no) | 100 | 90 |
| - the family’s ability to articulate the patient’s values/preferences? (yes/no) | 100 | 90 |
| - the hospital experience for the family? (yes/no) | 100 | 90 |
| - the clarity of the patient’s goals of care? (yes/no) | 100 | 100 |
| - the patient-centeredness of care delivered? (yes/no) | 100 | 90 |
| Would you recommend the intervention to a friend if one of their family members were admitted to the intensive care unit and at high risk of death or severe functional dependence? (yes/no) | 100 | 100 |
Patient Outcomes
The main patient outcomes were the patient-centeredness of care, hospital mortality, 3-month mortality, and 3-month functional status. Patient-centeredness of care was measured by adapting the Patient-Perceived Patient Centeredness of Care measure for surrogate decision makers. It is a 14-item instrument used to assess the extent to which care was perceived to reflect the patient’s needs and values. 46 This was measured among surrogates 3 months after discharge. Construct validity for the instrument is supported by a correlation between higher ratings of patient-centered care and better emotional health, less use of diagnostic tests, and fewer referrals to specialists among a cohort of outpatients.46 Ability to perform activities of daily living was assessed by surrogates 3 months after discharge by using the Katz Activities of Daily Living checklist.47 We also assessed length of stay in the ICU and hospital, discharge location, and whether there was any limitation of life-sustaining treatment before patients’ deaths.
Communication and Decision-Making Process Measures
The surrogates’ ratings of the quality of communication with the health care team were assessed with the Quality of Communication (QOC), a previously validated 17-item instrument measuring respondents’ perceptions of how well clinicians performed important communication tasks.48,49 Surrogates’ perceived self-efficacy to make medical decisions for the patient was measured with the Decision Self-Efficacy Scale. It contains 11-items, each of which is scored from 0, indicating “not at all confident,” to 5, indicating “very confident.”50 Decisional conflict was measured by using the Decisional Conflict Scale, developed and validated by O’Connor. This scale consists of 16 items scored on a 5-point Likert scale.50 To assess the degree of conflict between the clinical team and surrogates around decision making, we used a 1-item measure developed by Abbott and colleagues51 and validated by McDonagh and colleagues.52 This item yields a 0 to 10 score, with higher scores indicating more conflict. Both the physician and the surrogate completed this 1-item scale. Each of these instruments was completed after the first clinician-family conference in which the nurse interventionist participated.
Semistructured Interviews
A random sample of 10 surrogates and 5 physicians participated in a semistructured interview about the intervention. The semistructured interview elicited surrogates’ perspectives on the structure, strengths, and weaknesses of the intervention. The interview was conducted by a trained interviewer who adhered to principles of cognitive interviewing. Interviews were audio taped and transcribed for analysis.
Analyses
Quantitative Analyses
We assessed the degree of discordance between physicians and surrogates about patients’ prognoses by using the Wilcoxon-Mann-Whitney test for nonparametric data.
Qualitative
We used constant comparative methods to develop a framework to describe participants’ feedback about the intervention. Constant comparison is a general method for developing theory inductively from data that are systematically gathered and analyzed.53,54 To develop the preliminary coding scheme, 2 investigators (S.M.C., D.B.W.) independently performed open coding in which we read and performed line by line coding of a subset of the transcripts to identify themes and concepts. As concepts accumulated and distinctions between concepts became more refined, similar concepts were grouped into conceptual categories. These categories were developed further by comparing the categories between transcripts. Both coders reviewed this preliminary framework, and through a series of investigator meetings, arrived at consensus on the coding framework.54,55 We modified the framework iteratively over the study period when interviews yielded new themes or ideas. We continued interviews until we attained thematic saturation.
Results
We identified 29 eligible patients during the study period. Surrogates for 16 of the 29 eligible patients consented to study enrollment, for an overall enrollment rate of 55%. Ten patients were not enrolled because their surrogate declined participation; 3 patients were not enrolled because their attending physician declined. Enrolled and unenrolled patients did not differ in age, sex, race, or APACHE II score. One surrogate was not exposed to the intervention because the patient died soon after study enrollment, before the intervention could be implemented; therefore this patient was excluded from further data collection and is not included in the remaining analyses. Thirty-five surrogates and 15 physicians participated in the study. The characteristics of enrolled patients, surrogates, and physicians are summarized in Table 1.
Table 1.
Demographic characteristics of patients, surrogates, and physicians
| Patients (n = 15) | Surrogates (n = 35) | Physicians (n = 15) | |
|---|---|---|---|
| Sex, No. (%) | |||
| Male | 4 (27) | 15 (43) | 13 (87) |
| Female | 11 (73) | 20 (57) | 2 (13) |
| Race/ethnicity, No. (%) | |||
| Non-Hispanic white | 12 (80) | 25 (71) | 7 (47) |
| Non-Hispanic black | 3 (20) | 7 (20) | 0 (0) |
| Hispanic | 0 (0) | 0 (0) | 2 (13) |
| Asian/Pacific Islander | 0 (0) | 3 (9) | 4 (27) |
| Native American | 0 (0) | 0 (0) | 0 (0) |
| Other/undocumented | 0 (0) | 0 (0) | 2 (13) |
| Age, mean (SD), y | 73 (10.9) | 51 (13.9) | 33 (7.0) |
| Admission diagnosis, No. (%) | |||
| Respiratory failure | 15 (100) | — | — |
| Neurological failure | — | — | |
| Central nervous system neoplasm | 1 (7) | ||
| Stroke (hemorrhagic or ischemic) | 10 (67) | — | — |
| Subarachnoid hematoma | 1 (7) | — | — |
| Subdural/epidural hematoma | 2 (13) | — | — |
| Seizures | 1 (7) | — | — |
| APACHE II score at time of enrollment, mean (SD) | 28.2 (2.2) | — | — |
| Physician estimated risk of long-term severe functional impairment at time of enrollment, mean (SD) | 66.7 (10.5) | — | — |
| Relationship to patient, No. (%) | |||
| Spouse/partner | — | 5 (14) | — |
| Child | — | 21 (60) | — |
| Brother/sister | — | 6 (17) | — |
| Other relationship | — | 3 (9) | — |
| Staff position, No. (%) | |||
| Attending physician | — | — | 9 (60) |
| Resident or fellow | — | — | 6 (40) |
| Medical specialty, No. (%) | |||
| Critical care medicine | — | — | 4 (27) |
| Neurology | — | — | 4 (27) |
| Neurosurgery | — | — | 5 (33) |
| General surgery | — | — | 2 (13) |
| Subspecialty, No. (%) | |||
| Critical care | — | — | 2 (13) |
| Pulmonary, critical care | — | — | 2 (13) |
| Medicine | — | — | 1 (7) |
| Stroke | — | — | |
| Vascular neurology | — | — | 1 (7) |
| Years in practice, mean (SD) | — | — | 5 (7.4) |
Abbreviation: APACHE, Acute Physiology and Chronic Health Evaluation.
Feasibility
With the exception of the patient who died immediately after study enrollment, the intervention was successfully implemented in all surrogates. The intervention was implemented with high fidelity, as defined by the proportion of subjects who received each component of the intervention (Table 2). Three-month follow-up data were obtained from 83% of surrogates (29 of 35).
Table 2.
Feasibility of implementing the intervention
| Variable | % of patients for whom this encounter occurred (N = 14)a |
Duration, mean (SD), min |
|---|---|---|
| First conversation with physician | 86 | 6 (3) |
| First interaction with family | 100 | 47 (35) |
| Preconference with physician | 86 | 3 (3) |
| Preconference meeting with family | 100 | 15 (11) |
| Facilitated physician-family conference | 100 | 28 (16) |
| Postconference meeting with family | 86 | 17 (18) |
| Postconference meeting with physician | 50 | 2 (1) |
| Daily check-in with physicianb | 64 | 3 (2) |
| Daily check-in with familyb | 93 | 15 (22) |
| Life closure session for surrogates of the patients who died | 75 | 73 (69) |
| Mean time per day per patient | 48 (36) |
These data were not collected on 1 patient.
Applicable only on days when no first meeting, bedside update, or facilitated family conference occurred.
Acceptability and Perceived Effectiveness
No subjects dropped out of the study. All physicians and surrogates indicated that they would recommend the intervention to a friend. Table 3 shows high levels of perceived effectiveness by physicians and surrogates regarding key elements of communication and decision making. At least 90% of physicians and surrogates reported that the intervention (1) improved the quality and timeliness of communication, (2) facilitated a discussion of the patient’s values and treatment preferences, and (3) improved the patient-centeredness of care.
Patients’ Outcomes
The mean ICU and hospital length of stay were 12 (SD, 7.2) days and 14 (SD, 10.6) days, respectively. Eleven of 15 patients had treatment limitation decisions made a mean of 5 (SD, 4) days after study enrollment. The in-hospital mortality rate was 53% (8 of 15). All 8 deaths were preceded by limitation of life-sustaining treatment. At 3 months, the mortality rate was 73% (11 of 15). The mean Katz ADL inventory was 3.3 out of 6, indicating substantial functional impairment among survivors. Patient-centeredness of care measured at 3 months was high (3.3 [SD, 0.5] on a 4-point scale).
Communication and Decision-Making-Process Measures
The mean time spent by the study interventionist per patient per day on care-related activities was 48 (SD, 36) minutes. The mean Decisional Conflict score was 16.4 (SD, 16.8; on a scale of 0–100 with higher scores indicating more conflict). The mean Decisional Confidence score was 3.4 (SD, 0.6; on a scale of 0–4, with higher scores indicating more confidence). The mean score on the Quality of Communication Scale was 7.6 (SD, 1.8; on a scale of 0–10, with higher scores indicating higher quality).
Before undergoing the intervention, there was significant discordance between physicians’ and surrogates’ estimates of the likelihood that the patient would have severe, long-term functional impairment at 6 months after discharge, with surrogates significantly more optimistic about patients’ being free of severe functional impairment (chance of severe impairment: physicians’ estimate 88% [SD, 11%] vs surrogates’ estimate 66% [SD, 34%]), which decreased significantly after implementation of the intervention (physicians’ estimate 88% [SD, 11%] vs surrogates’ estimate 84% [SD, 27%], P = .01).
Semistructured Interviews
Participants’ responses during the semistructured interview revealed a more detailed view of the ways in which the intervention was perceived to be beneficial. Table 4 contains the main themes from subjects regarding the value of the intervention. No subject expressed discomfort with the intervention, and the feedback was overwhelmingly positive.
Table 4.
Participants’ views of the benefits of the Four Supports Intervention
| Theme | Examples |
|---|---|
| Surrogates (n = 10) | |
| Provides emotional support | “I saw her as a … she was just like my support system.” |
| “She’s kind o’ been our therapist and our … our social worker … a nurse. You know, nurse, therapist, social worker kind of all rolled into one.” | |
| “She was there when I cried.” | |
| Ensures timely communication | “That’s what I found to be the most valuable—what she did on our behalf, to arrange meeting with the doctors.” |
| “I would say it is needed for the patient and families, it is invaluable. I don’t know how the meetings with the team—the medical care—would have been accomplished without the intervention.“ | |
| Provides anticipatory guidance | “The thing I found most, was having a go-to person to … give us a little heads up [about] what [the clinical team] was anticipating doing and how they were feeling about things. It made it a little less, … we weren’t caught off guard, … we had an inkling what was going to be said.” |
| “It’s always easier when she explains things a little bit ahead of time and we kinda know.” | |
| Increases patient-centeredness of care | “It’s been huge. And just also [deep breath] you know, sitting down with us and making sure kinda we were all on the same page about what Mom would want.” |
| “She brought up, a couple times to us, just kinda keep in mind … what would Mom want? What would … what would she not want?” | |
| Maintains availability for families | “But what she has become is … is someone who we can go to, when we can’t go to a doctor, for whatever reason.” |
| Bridges lay and medical knowledge | “Not having a medical background is very concerning; regardless of what you do, There is a certain level of education that you take for granted, it was nice to be able to have someone you could talk to and ask questions, sometimes it’s not the doctor you want to ask, its nice to have someone to ask about what terms mean, what is dialysis, there are different ports, or how people respond…” |
| Physicians (n = 5) | |
| Provides high-level communication skills | “She really acted as a go-between, between the physician and the family, who could … who honestly had more time to devote and probably more focused training along the lines of discussing important issues—that physicians, once again, sometimes neither have the time for nor the best training for. |
| Prepares clinicians for families’ questions/concerns | “I think she did very good job of coordinating, making sure that we were all present… and sort of prepping us for, you know, what types of questions [the family] might have.” |
| Ensures timely communication | “It was a good gentle reminder, on the days when we … we needed to have discussions, she sort of would page me, track me down.” |
| Enables difficult conversations | “I think [she] forced me to address these issues with the family that sometimes can … can get overlooked.” |
| “She could ask the questions that needed to be asked…” | |
| Focuses on the patient’s values | “She helped us stay in the perspective of where the family’s feelings were about overall goals of therapy, before the conversation, which kind of helped facilitate the conversation.” |
| Increases the ease and efficiency of communication | “I think that she definitely facilitated the discussion, made it go much more smoothly, much more efficient.” |
| “She was able to sort of kind of answer a lot of first-line questions, so that we were focused on the crux issues as opposed to sort of belaboring all the first types of questions that are more straightforward issues.” | |
Early in the pilot phase, 1 physician noted that a potential area for improvement was to better integrate the FSS into the clinical team: “I think there is a need to make sure she is just sort of an extension of our current clinical team.” A second theme raised by a neurosurgeon addressed the general difficulty of physicians being available to meet with families because of busy operating schedules: “For busy surgeons, we round when we can. We see families as often and whenever we can fit them in.” Another framed it as: “The logistics of planning times where we could meet with the specialist and the family … would be difficult for a surgeon.” These comments prompted several modifications to improve the integration of the FSS and to increase the ease for clinicians of meeting with families (described in the following section).
Discussion
We describe a novel, multifaceted intervention involving the addition to the ICU team of a specially trained nurse to function as a family support specialist who provides 4 types of support to families of patients with advanced critical illness in a structured, individualized way. The intervention was designed to overcome the cognitive, emotional, psychological, and communication barriers that threaten the quality of surrogate decision making in ICUs. The present study indicates that the intervention is feasible, acceptable, and was perceived by clinicians and surrogates to increase the quality of communication, families’ ability to articulate the patients’ values, and the patient-centeredness of care.
The Four Supports Intervention is innovative in several ways. First, the intervention creates a new role on the ICU team specifically to facilitate intensive support of families and to ensure that the family has a predictable, longitudinal relationship with at least 1 clinician during the hospitalization. Second, the intervention is grounded in empirical insights from the fields of decision psychology and behavioral economics, suggesting that people employ both cognitive and emotional reasoning in judgment and decision making.56 This grounding resulted in an intervention that is substantially different from traditional decision aids and decision-support interventions. Specifically, in addition to addressing the usual cognitive targets of decision aids, the intervention also addresses the emotional aspects of (1) having a loved one who is critically ill and (2) being asked to make end-of-life decisions for the patient. Third, the intervention incorporates Donabedian health systems theory to target organizational barriers to frequent, robust communication between clinicians and families. Fourth, the intervention is structured and guided by a detailed intervention manual, which will aid in dissemination should it be shown to be effective in a large-scale randomized clinical trial.
There are several potential criticisms of the intervention. Some may argue that it is too complex. Although the intervention has multiple components, each are discrete, teachable behaviors. Recent research suggests that some nurses already undertake some of these behaviors.57 Our feasibility testing revealed that the intervention was implemented successfully. Others may argue that a simple “pen and paper” decision aid may achieve the same goal. Although this is theoretically possible, there are several conceptual reasons to doubt whether a standard decision aid will be effective for difficult decisions near the end of life in ICUs. First, empirical research suggests that emotional factors and inadequate clinician-family communication—not just informational deficiencies—contribute substantially to the problems.27,28 Decision aids provide information but do not provide emotional support or overcome the barriers to frequent clinician-family communication in ICUs. Second, decision aids are generally designed for “one-time” decisions, such as whether to undergo radiotherapy or prostatectomy for early stage prostate cancer. However, decisions in ICUs generally require multiple conversations over time in the face of frequently changing information about prognosis and treatment options.
There were 2 main challenges that arose in implementing the intervention, both of which provided an opportunity to refine the intervention. First, a few physicians found it difficult to be available to meet with the family regularly. This challenge is not specific to the Four Supports Intervention, has been noted in several other studies,40,41 and has proven resistant to quality improvement interventions. 21,58 We successfully addressed this problem by giving more advanced notice to these clinicians and arranging meetings at times that were feasible for clinicians, as well as through persistent advocacy for the needs of the family. Another approach to address this—that should be explored in future research—is for the FSS to take on even more responsibility for communication. However, our impression is that communication was most effective when the physician, bedside nurse, and FSS met with families together.
There were also early challenges in integrating the FSS into the care team. This is perhaps not surprising because clinical team structures and role expectations are deeply ingrained in hospital cultures. We overcame this barrier by ongoing education of the clinical team about the FSS role and increasing the amount of direct engagement between the FSS and the other members of the clinical team. In particular, we found it was very helpful for the FSS to participate in daily ICU rounds, during which the FSS gave the team structured feedback about the family and their needs, as well as information about the patient’s goals and values.
This study has several strengths. First, we undertook a detailed assessment of quantitative process and outcome measures, which will aid in realistic power calculations for future studies. We quantified the time expenditure per patient by the FSS, which is crucial to staffing questions that will arise when implementing the intervention more broadly. Second, we conducted semistructured interviews with both physicians and surrogates, which allowed a more detailed qualitative understanding of the participants’ experiences with the intervention. The findings led to changes in the intervention, including changes that improved the degree to which the FSS was integrated into the clinical team.
This study has several limitations. First, because there is no control arm, it does not establish the effectiveness of the intervention. The subjective benefit reported by participants is encouraging, but should be viewed with caution pending the results of a randomized trial in which the intervention is compared with usual care. Second, we did not assess whether the intervention improved bedside nurses’ perceptions of multidisciplinary collaboration, an important topic because of previously documented difficulties in this aspect of care. Third, the study was conducted in a single ICU. Although the intervention was designed to be flexible to accommodate the varied needs and preferences of participants, additional studies in diverse ICUs are needed to understand how to best tailor the intervention to local factors. There may be differences between surrogates who did and did not consent to study enrollment, which could pose a threat to generalizability of the results. We were not permitted by the institutional review board to elicit from surrogates reasons for nonenrollment in order to distinguish between those who did not wish to participate in research and those who felt they did not need more support.
In conclusion, a multifaceted intervention involving the addition of a family support specialist to the standard ICU team is feasible, acceptable, and was perceived by physicians and surrogates to improve the quality of decision making and the patient-centeredness of care. A randomized clinical trial is warranted to assess the effect of the intervention on patient, family, and health system outcomes.
Acknowledgments
FUNDING DISCLOSURES
Dr White was supported by a Paul Beeson Career Development Award from the National Institute of Aging and a Greenwall Foundation Faculty Scholars in Bioethics award.
Appendix
Summary sheet for physicians.
|
Family’s decision making and relationships | |
|
1. Who are the main family members making decisions for the patient? 2. Are there any intrafamily conflicts that may require attention? |
What role do the family members prefer in decision making about goals of care? □ prefer to make final decision □ prefer to make the final decision after seriously considering the doctor’s opinion □ prefer that the doctor and family share equal responsibility □ prefer that the doctor makes the final decision but seriously considers family’s opinion □ prefer that the doctor decides |
|
Family’s understanding of the patient’s prognosis | |
| 1. Likelihood of survival to hospital discharge | |
| 2. Likelihood of severe functional impairment in 6 months | 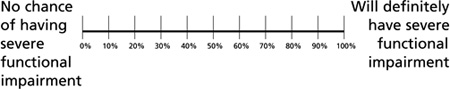 |
|
Patient’s treatment preferences and values | |
|
1. Is there a written advance directive? (If so, summarize key points) 2. What is known about patient’s values and health care preferences? |
3. Patient’s preferences about continuing life support if likely outcome is: - Living in a nursing home or with substantial care-giving burdens? - Being unable to think clearly or interact with others? - Being unable to do valued physical activities? - Being a burden on family (financially or care giving)? - Being attached to machines to be kept alive? |
| Family’s main questions | |
REFERENCES
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32(3):638–643. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 2.Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28(8):3044–3049. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 3.Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of posttraumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 4.Baggs JG, Schmitt MH, Mushlin AI, Eldredge DH, Oakes D, Hutson AD. Nurse-physician collaboration and satisfaction with the decision-making process in three critical care units. Am J Crit Care. 1997;6(5):393–399. [PubMed] [Google Scholar]
- 5.Breen CM, Abernethy AP, Abbott KH, Tulsky JA. Conflict associated with decisions to limit life-sustaining treatment in intensive care units. J Gen Intern Med. 2001;16(5):283–289. doi: 10.1046/j.1525-1497.2001.00419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtis JR, Engelberg RA, Wenrich MD, Shannon SE, Treece PD, Rubenfeld GD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med. 2005;171(8):844–849. doi: 10.1164/rccm.200409-1267OC. [DOI] [PubMed] [Google Scholar]
- 7.Hanson LC, Danis M, Garrett J. What is wrong with end-of-life care? Opinions of bereaved family members. J Am Geriatr Soc. 1997;45(11):1339–1344. doi: 10.1111/j.1532-5415.1997.tb02933.x. [DOI] [PubMed] [Google Scholar]
- 8.Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung. 1990;19(4):401–415. [PubMed] [Google Scholar]
- 9.Rubenfeld GD, Randall Curtis J. End-of-life care in the intensive care unit: a research agenda. Crit Care Med. 2001;29(10):2001–2006. doi: 10.1097/00003246-200110000-00025. [DOI] [PubMed] [Google Scholar]
- 10.White DB, Braddock CH, 3rd, Bereknyei S, Curtis JR. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med. 2007;167(5):461–467. doi: 10.1001/archinte.167.5.461. [DOI] [PubMed] [Google Scholar]
- 11.White DB, Curtis JR. Care near the end-of-life in critically ill patients: a North American perspective. Curr Opin Crit Care. 2005;11(6):610–615. doi: 10.1097/01.ccx.0000184301.76007.70. [DOI] [PubMed] [Google Scholar]
- 12.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med. 2007;35(2):442–448. doi: 10.1097/01.CCM.0000254723.28270.14. [DOI] [PubMed] [Google Scholar]
- 13.Lynn J, Teno JM, Phillips RS, et al. Perceptions by family members of the dying experience of older and seriously ill patients. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97–106. doi: 10.7326/0003-4819-126-2-199701150-00001. [DOI] [PubMed] [Google Scholar]
- 14.Murphy DJ, Burrows D, Santilli S, Kemp AW, Tenner S, Kreling B, Teno J. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330(8):545–549. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]
- 15.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 16.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154(5):336–346. doi: 10.7326/0003-4819-154-5-201103010-00008. [DOI] [PubMed] [Google Scholar]
- 17.Embriaco N, Azoulay E, Barrau K, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175(7):686–692. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 18.Poncet MC, Toullic P, Papazian L. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175(7):698–704. doi: 10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- 19.Rushton CH. Defining and addressing moral distress: tools for critical care nursing leaders. AACN Adv Crit Care. 2006;17(2):161–168. [PubMed] [Google Scholar]
- 20.SUPPORT: a controlled trial to improve care for seriously ill hospitalized patients. JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 21.Curtis JR, Nielsen EL, Treece PD, et al. Effect of a qualityimprovement intervention on end-of-life care in the intensive care unit: a randomized trial. Am J Respir Crit Care Med. 2011;183(3):348–355. doi: 10.1164/rccm.201006-1004OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daly BJ, Douglas SL, O’Toole E, et al. Effectiveness trial of an intensive communication structure for families of longstay ICU patients. Chest. 2010;138(6):1340–1348. doi: 10.1378/chest.10-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lilly CM, De Meo DL, Sonna LA, et al. An intensive communication intervention for the critically ill. Am J Med. 2000;109(6):469–475. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]
- 24.Dowling J, Vender J, Guilianelli S, Wang B. A model of family-centered care and satisfaction predictors: the Critical Care Family Assistance Program. Chest. 2005;128(3 Suppl):81S–92S. doi: 10.1378/chest.128.3_suppl.81S. [DOI] [PubMed] [Google Scholar]
- 25.Dowling J, Wang B. Impact on family satisfaction: the Critical Care Family Assistance Program. Chest. 2005;128(3 Suppl):76S–80S. doi: 10.1378/chest.128.3_suppl.76S. [DOI] [PubMed] [Google Scholar]
- 26.Limerick MH. The process used by surrogate decision makers to withhold and withdraw life-sustaining measures in an intensive care environment. Oncol Nurs Forum. 2007;34(2):331–339. doi: 10.1188/07.ONF.331-339. [DOI] [PubMed] [Google Scholar]
- 27.Swigart V, Lidz C, Butterworth V, Arnold R. Letting go: family willingness to forgo life support. Heart Lung. 1996;25(6):483–494. doi: 10.1016/s0147-9563(96)80051-3. [DOI] [PubMed] [Google Scholar]
- 28.Kirchhoff KT, Walker L, Hutton A, Spuhler V, Cole BV, Clemmer T. The vortex: families’ experiences with death in the intensive care unit. Am J Crit Care. 2002;11(3):200–209. [PubMed] [Google Scholar]
- 29.Tilden VP, Tolle SW, Garland MJ, Nelson CA. Decisions about life-sustaining treatment: impact of physicians’ behaviors on the family. Arch Intern Med. 1995;155(6):633–638. [PubMed] [Google Scholar]
- 30.Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs Res. 2001;50(2):105–115. doi: 10.1097/00006199-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Power TE, Swartzman LC, Robinson JW. Cognitive-emotional decision making (CEDM): a framework of patient medical decision making. Patient Educ Couns. 2011;83(2):163–169. doi: 10.1016/j.pec.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 32.Pham MT. Emotion and rationality: a critical review and interpretation of empirical evidence. Rev Gen Psychol. 1997;11(2):155–178. [Google Scholar]
- 33.Campbell ML, Guzman JA. Impact of a proactive approach to improve end-of-life care in a medical ICU. Chest. 2003;123(1):266–271. doi: 10.1378/chest.123.1.266. [DOI] [PubMed] [Google Scholar]
- 34.Norton SA, Hogan LA, Holloway RG, Temkin-Greener H, Buckley MJ, Quill TE. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med. 2007;35(6):1530–1535. doi: 10.1097/01.CCM.0000266533.06543.0C. [DOI] [PubMed] [Google Scholar]
- 35.Closs SJ, Tierney AJ. The complexities of using a structure, process and outcome framework: the case of an evaluation of discharge planning for elderly patients. J Adv Nurs. 1993;18(8):1279–1287. doi: 10.1046/j.1365-2648.1993.18081279.x. [DOI] [PubMed] [Google Scholar]
- 36.Richie ND. An approach to hospice program evaluation: the use of Donabedian theory to measure success. Am J Hosp Care. 1987;4(5):20–27. doi: 10.1177/104990918700400511. [DOI] [PubMed] [Google Scholar]
- 37.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 38.White DB, Malvar G, Karr J, Lo B, Curtis JR. Expanding the paradigm of the physician’s role in surrogate decision-making: an empirically derived framework. Crit Care Med. 2010;38(3):743–750. doi: 10.1097/CCM.0b013e3181c58842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.White DB. Rethinking interventions to improve surrogate decision making in intensive care units. Am J Crit Care. 2011;20(3):252–257. doi: 10.4037/ajcc2011106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gay EB, Pronovost PJ, Bassett RD, Nelson JE. The intensive care unit family meeting: making it happen. J Crit Care. 2009;24(4):629.e1–629.e12. doi: 10.1016/j.jcrc.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelson JE, Mulkerin CM, Adams LL, Pronovost PJ. Improving comfort and communication in the ICU: a practical new tool for palliative care performance measurement and feedback. Qual Saf Health Care. 2006;15(4):264–271. doi: 10.1136/qshc.2005.017707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rushton CH. Respect in critical care: a foundational ethical principle. AACN Adv Crit Care. 2007;18(2):149–156. doi: 10.1097/01.AACN.0000269258.14418.1e. [DOI] [PubMed] [Google Scholar]
- 43.Spichiger E, Wallhagen MI, Benner P. Nursing as a caring practice from a phenomenological perspective. Scand J Caring Sci. 2005;19(4):303–309. doi: 10.1111/j.1471-6712.2005.00350.x. [DOI] [PubMed] [Google Scholar]
- 44.Back AL, Arnold RM, Quill TE. Hope for the best, and prepare for the worst. Ann Intern Med. 2003;138(5):439–443. doi: 10.7326/0003-4819-138-5-200303040-00028. [DOI] [PubMed] [Google Scholar]
- 45.Chochinov HM. Dying, dignity, and new horizons in palliative end-of-life care. CA Cancer J Clin. 2006;56(2):84–103. doi: 10.3322/canjclin.56.2.84. quiz 104-105. [DOI] [PubMed] [Google Scholar]
- 46.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 47.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the Index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 48.Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit Care Med. 2006;34(6):1679–1685. doi: 10.1097/01.CCM.0000218409.58256.AA. [DOI] [PubMed] [Google Scholar]
- 49.Curtis JR, Engelberg RA, Nielsen EL, Au DH, Patrick DL. Patient-physician communication about end-of-life care for patients with severe COPD. Eur Respir J. 2004;24:200–205. doi: 10.1183/09031936.04.00010104. [DOI] [PubMed] [Google Scholar]
- 50.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 51.Abbott KH, Sago JG, Breen CM, Abernethy AP, Tulsky JA. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med. 2001;29(1):197–201. doi: 10.1097/00003246-200101000-00040. [DOI] [PubMed] [Google Scholar]
- 52.McDonagh JR, Elliott TB, Engelberg RA, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med. 2004;32(7):1484–1488. doi: 10.1097/01.ccm.0000127262.16690.65. [DOI] [PubMed] [Google Scholar]
- 53.Glaser BG, Strauss AL. Discovery of Grounded Theory. Chicago, IL: Adline Publishing Company; 1967. [Google Scholar]
- 54.Strauss AL, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 55.Charmaz KC. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- 56.Sloman SA. Two systems of reasoning. In: Griffin D, Kahneman D, Gilovich T, editors. Heuristics and Biases: The Psychology of Intuitive Judgment. New York, NY: Cambridge University Press; 2002. [Google Scholar]
- 57.Reinke LF, Shannon SE, Engelberg R, Dotolo D, Silvestri GA, Curtis JR. Nurses’ identification of important yet under-utilized end-of-life care skills for patients with life-limiting or terminal illnesses. J Palliat Med. 2010;13(6):753–759. doi: 10.1089/jpm.2009.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Black MD, Levy M, McNicholl L, Cornell M. A multifaceted intervention to improve communication in the ICU [abstract] Am J Respir Crit Care Med. 2011;183:A4121. [Google Scholar]