Abstract
Endoscopy is widely accepted as the first treatment option in the management of bile duct stones. In this review we focus on the alternative endoscopic modalities for the management of difficult common bile duct stones. Most biliary stones can be removed with an extraction balloon, extraction basket or mechanical lithotripsy after endoscopic sphincterotomy. Endoscopic papillary balloon dilation with or without endoscopic sphincterotomy or mechanical lithotripsy has been shown to be effective for management of difficult to remove bile duct stones in selected patients. Ductal clearance can be safely achieved with peroral cholangioscopy guided laser or electrohydraulic lithotripsy in most cases where other endoscopic treatment modalities have failed. Biliary stenting may be an alternative treatment option for frail and elderly patients or those with serious co morbidities.
Keywords: Choledocholithiasis, Mechanical lithotripsy, Laser lithotripsy, Electrohydra-ulic lithotripsy, Difficult to remove biliary stones, Endoscopic large balloon papillary dilation, Peroral cholangioscopy
INTRODUCTION
Common bile duct (CBD) stones are seen in approximately 7%-12% of patients who undergo cholecystectomy for symptomatic cholelithiasis and are a common indication for referral to a biliary endoscopist[1]. They vary in size ranging from rather small (approximately 1-2 mm) to very large (> 3 cm). Endoscopic retrograde cholangiopancreatography (ERCP) with endoscopic sphincterotomy (ES) and basket or balloon extraction are well established therapeutic procedures for the management of CBD stones. It is estimated that nearly 85%-95% of all CBD stones can be managed effectively by these conventional endoscopic methods[2,3]. Failure to clear the bile duct renders the patient vulnerable to biliary obstruction, cholangitis and pancreatitis, thereby increasing the morbidity[4,5]. The occurrence of acute cholangitis is associated with significant mortality, especially in the elderly, underscoring the need for early intervention to clear the bile duct of stones and to relieve the obstruction to achieve adequate biliary drainage. Extraction of CBD stones is one of the most commonly performed procedures by therapeutic endoscopists. With novel advances in extraction techniques and instruments emerging routinely, it is vital to keep abreast of the new developments in order to improve the outcome. This review focuses on the alternative endoscopic management options for the treatment of difficult to remove CBD stones.
REVIEW CRITERIA
In July 2011, we searched MEDLINE from 1982 to the present using the Medical Subject Headings terms common bile duct stone, endoscopic retrograde cholangiopancreatography, difficult stone, endoscopy, and the key word “common bile duct stone”. Full papers and abstracts in English language were considered. Important developments in research, reports from centers of excellence, and our own clinical experience in managing them, form the basis of this review article.
FACTORS ASSOCIATED WITH DIFFICULT TO TREAT BILE DUCT STONES
Multiple factors have been postulated to govern the success or failure of endoscopic extraction of CBD stones. In approximately 10%-15% of patients, managing biliary stones becomes formidable primarily due to difficulties in accessing the bile duct (periampullary diverticulum, sigmoid shaped CBD, post-gastrectomy Billroth type II anatomy, Roux-en-Y-gastrojejunostomy), large number of stones (greater than 10), large size of stones (stones with a diameter > 15 mm which cannot be grasped with a basket), unusually shaped stones (barrel-shaped) or location of the stones (intra hepatic, cystic duct, proximal to strictures)[6]. In addition, endoscopic management becomes challenging in Mirizzi syndrome, in which stones in the cystic duct cause obstruction of the main bile duct[7]. Kim et al[8] prospectively evaluated the factors contributing to technical difficulty during endoscopic clearance of CBD stones. They reported that older age (> 65 years), previous gastrojejunostomy, larger stone size (≥ 15mm), impaction of stones, shorter length of the distal CBD arm (≤ 36mm), and more acute distal CBD angulation (≤ 135 degrees) are all contributors to technical difficulty for endoscopic removal of bile duct stones[8].
MANAGEMENT OF DIFFICULT STONES
In high risk patients, the risks and benefits of alternative techniques for removal of bile duct stones not amenable to conventional endoscopic techniques must be carefully balanced against each other and with surgery. The individual decision concerning the appropriate therapy is also influenced by the local expertise and the availability of the technical equipment.
CBD stones up to 1.5 cm in diameter can be extracted intact after endoscopic sphincterotomy. The rate of successful retrieval progressively declines with increasing size of the stone[9]. Larger stones especially those with a diameter ≥ 2cm may need fragmentation before removal to reduce the risk of stone impaction.
Mechanical lithotripsy
In 1982, Riemann et al[10], first introduced mechanical lithotripsy (ML). ML is currently the most widely used technique for fragmentation of stones. Contemporary lithotripter baskets have a high breaking strengths and have improved the success rate of ML for extraction of large CBD stones (> 2 cm) to well over 90% without serious complications[11]. Broadly speaking, there are two types of baskets for ML. The type of basket used depends on whether lithotripsy is done on an elective (“through the scope”) basis or on an emergent basis (salvage device) for basket impaction[12]. The ‘through the scope’ model is typically a three-layer system with the basket, inner plastic sheath, and an outer metal sheath (Figure 1). The stone is captured with the basket and the outer metal sheath is advanced to the stone which will be crushed against it. Sometimes, unexpectedly, stone and basket impaction can occur even during routine extraction of smaller stones. Under such circumstances, stone fragmentation can be done after removing the handle from the basket and the duodenoscope from the patient. An endotriptor (a spiral metal sheath) is introduced under fluoroscopic guidance, over the basket wires, and the stone is crushed after connecting the bare basket wires to the crank handle (Figure 2). The broken basket and the stone are then removed. The shaft of the endotriptor is generally shorter and thicker than that employed in standard ML[13]. Although basket impaction can occur with through the scope lithotripsy baskets; it is more commonly encountered with extraction baskets, which have thinner wires and weaker handles not suitable for fragmentation of stones.
Figure 1.
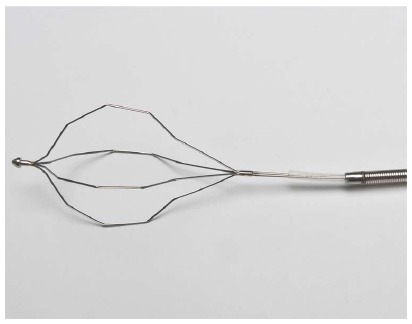
Example of a three-layered mechanical lithotripsy device with the basket, inner plastic sheath and an outer metal sheath. The stone is captured by the basket and crushed against the outer metal sheath.
Figure 2.

Image of a mechanical lithotripter which can be used as a “salvage device” for removal of impacted baskets.
In patients with multiple large stones, lithotripters with a sleeve system can be employed multiple times without withdrawal of the endoscope, facilitating stone fragmentation[14,15].
ML has been widely used as it is a readily available, cost effective, and simple procedure. Unfortunately the failure rate is high especially in patients with stones greater than 2.8 cm in diameter[15]. In a retrospective study the size of the stone was the only factor that significantly affected the success or failure of bile duct clearance. In this study of 162 patients, the cumulative probability of bile duct clearance ranged from > 90% for stones with a diameter less than 10 mm to 68% for those greater than 28 mm in diameter (P < 0.02)[15]. A subsequent prospective study by Garg et al[16] however reported that stone size alone may not be important unless considered together with the diameter of the bile duct. They concluded that the only important predictive factor that compromised the success of mechanical lithotripsy was stone impaction in the bile duct, with either an inability to pass the basket proximal to the stone or a failure of the basket to open fully around the stone to allow it to be grasped properly[16]. Although stone composition was not included in the study by Leung et al[12], some endoscopists believe that stones that are hard and densely calcified (visualized on a plain radiograph) resist mechanical fragmentation, resulting in an extraction failure with standard baskets. Although the stones which are molded to the shape of the bile duct may be softer, they are more difficult to crush because they may not be easily engaged by the lithotripter basket[12].
A multi-center study reported the rate of complications associated with ML to be around 3.6%[13]. Among the spectrum of complications, basket impaction or fracture of the basket wire are uniquely associated with ML. Non-surgical interventions that have been utilized in this setting include extension of sphincterotomy, awaiting spontaneous passage of the impacted basket and stone after successful stent placement, use of a second lithotripter, extracorporeal shock wave lithotripsy (ESWL), laser lithotripsy, electrohydraulic lithotripsy, and transhepatic lithotripsy and stone dislodgement[13-18]. Other complications include broken handle and perforation or injury to the bile duct[13-18].
In about 10% of the patients ML proves to be cumbersome, protracted and ineffective[6] wherein one has to resort to other methods such as electrohydraulic, or laser lithotripsy for stone fragmentation and subsequent removal.
Electrohydraulic lithotripsy
Initially used as an industrial tool for fragmenting rocks in mines, its application was extrapolated to medical use when Koch attempted fragmentation of biliary stones using this technology[19]. Electrohydraulic Lithotripsy (EHL) consists of a bipolar lithotripsy probe which discharges sparks with the aid of a charge generator in an aqueous medium. The sparks generated under water generate high-frequency hydraulic pressure waves, the energy of which is absorbed by nearby stones and results in their fragmentation[20]. The shock waves can cause inadvertent injury or perforation of the bile duct wall if the probe is not deployed close to the stone and away from the ductal wall. EHL can be performed under fluoroscopic guidance by using centering balloons or direct cholangioscopic vision[20]. The disadvantage of using only fluoroscopic guidance is related to the two dimensional imaging and the inability to confirm correct positioning of the probe. Therefore direct visualization is frequently preferred to avoid damage to the ductal wall[21]. A cholangioscope is inserted through the instrument channel of the mother scope. One or two dedicated biliary endoscopists are needed for this procedure. Continuous irrigation with water during the procedure generates a fluid medium for propagation of the shock waves and in addition offers a clear view of the stones by flushing away the debris[20].
The overall complication rate ranges from 7% to 9%[22,23], with most common complications being hemobilia, cholangitis, and less commonly, ductal perforation. Binmoeller et al[6], in one of the earlier large studies reported that EHL was successful in 63 of the 64 patients who had failed previous attempts of ML. Smaller published studies report stone fragmentation rates between 77%-100% for peroral EHL with minimal complications[22,24-28]. Arya et al[23], reported a stone fragmentation rate of 96% and final stone clearance of 90%. In a retrospective study of 94 patients who had failed stone extraction by conventional techniques, Hui et al[29], compared the outcomes of EHL with further endoscopy to stenting alone in a subset of elderly and infirm patients. They demonstrated that EHL and further ERCPs had a higher success rate (80%) with a low complication rate (7.7%) and recommended that elderly and frail patients should be referred to tertiary centers for EHL in order to prolong survival and decrease biliary complications[29].
The EHL equipment is compact, requires no special electricity, and is relatively inexpensive[30]. Other advantages are that the EHL procedure does not require special training or protective gear. In the United States, use of EHL for fragmentation and removal of biliary stones is quite common in centers with special interest in biliary disorders.
Laser lithotripsy
In laser lithotripsy (LL), laser light at a particular wavelength is focused on the surface of the stone to induce a wave-mediated fragmentation. The pulsed laser energy utilized in stone fragmentation is in contrast to the continuous laser energy used in tumor ablation[7]. The first successful use of pulsed laser for shock-wave lithotripsy of bile duct stones was reported in 1986[31]. Since then the technology has evolved and other laser types such as neodymium: yttrium-aluminum-garnet (Nd: YAG), flash lamp-pulsed dye (coumarin), the flash lamp-pulsed dye (rhodamine) with an automatic stone recognition system and the new Frequency Doubled Double Pulse Nd:YAG (FREDDY) system have been introduced[32-35]. LL is typically performed perorally under cholangioscopic or fluoroscopic guidance or by the transhepatic approach. As with EHL, LL under direct visualization using a cholangioscope is often preferred to avoid damage to the ductal wall (Figure 3).
Figure 3.
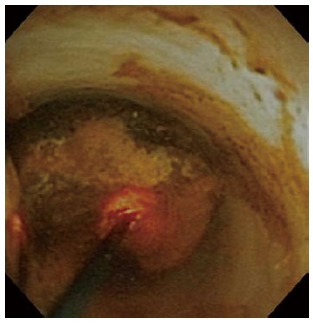
Laser lithotripsy of a bile duct stone under cholangioscopic guidance.
Based on some reports, ductal clearance can be accomplished in 64% to 97% of patients by using[7,36] LL. In the majority of patients ductal clearance could be achieved in one session, although more sessions were required occasionally. LL has been demonstrated to be more effective than ESWL in terms of stone clearance rate and more rapid stone fragmentation with a shorter duration of treatment leading to a significant reduction in cost[37,38]. In some centers where the laser equipment is available, laser lithotripsy has gained popularity and has managed to replace EHL as the primary modality for fragmentation of difficult to remove stones.
A recent innovation worth mentioning is the introduction of a double-lumen basket which allows passage of a laser probe for effective laser lithotripsy after the stone is captured by the basket[39]. For a selected group of patients, this technique was shown to be feasible and effective, and the authors hope that continuous improvements in designs and construction materials would further enhance the success rate of this device.
Extracorporeal shockwave lithotripsy
In ESWL, high-pressure shock waves are generated outside the body (extracorporeal) by underwater spark gap (electrohydraulic) generated by piezoelectric crystals or electromagnetic membrane technology[30]. The shock waves are focused by elliptical transducers to the designated target through a liquid or tissue medium which prevents the energy attenuation. ESWL is performed under ultrasound or fluoroscopic guidance. Since most biliary stones are radiolucent and are not adequately visualized by fluoroscopy alone, placement of a nasobiliary tube for contrast instillation is required if ESWL is performed under fluoroscopy. In case of first generation lithotripters, the patients needed to be immersed in a water bath. Subsequent ESWL lithotripters employ water-filled compressible bags and a gel is applied to the skin surface for interface with the patient. Comparison between the lithotripters at a single center showed no significant difference in fragmentation of CBD stones[40]. General anesthesia is usually needed as the discomfort produced may not be adequately controlled by conscious sedation. The critical determining factor for success of single ESWL session is stone size and microcrystalline structure and architecture of the stone[41,42]. The presence or absence of bile duct stenosis can also influence the success of ESWL[43]. Sauerbruch et al[44], reported the efficacy of ESWL in achieving CBD stone fragmentation in over 90% of patients with minimal side effects.
In most institutions that already have access to ESWL for treatment of renal calculi, no other purchases of equipment needs to be made. For ESWL direct contact with the calculi is not needed, and multiple stones can be managed simultaneously[41]. ESWL can be of particular help in patients with abnormal anatomy such as those who have undergone Billroth-II or Roux-en-Y surgeries in whom endoscopic access to the major papilla is difficult.
Although in general ESWL is tolerated well, it can be associated with adverse events such as transient biliary colic, subcutaneous ecchymosis, cardiac arrhythmia, self limited hemobilia, cholangitis, ileus and pancreatitis[7,45]. Perinephric hematoma, biliary obstruction, bowel perforation, lung injury and splenic rupture are among the rarely reported complications[42]. Multiple ESWL sessions may be required in a subset of patients to achieve ductal clearance, and endoscopic procedures between the ESWL sessions may become necessary to clear the bile duct of debris to assure drainage. The recurrence rate of CBD stones after ESWL clearance during a 1 to 2 year follow up was considerable and was around 14%[45,46]. In a randomized trial comparing fluoroscopic guided ESWL and LL, LL was preferable not only for successful stone free rate (73% vs 97%), but also in terms of the number of sessions needed to clear the duct (3 in ESWL vs 1.2 in LL) and the duration of treatment[30]. Another randomized trial comparing ultrasound guided ESWL and laser lithotripsy in the treatment of CBD stones refractory to conventional treatment clearly showed superior stone clearance rate and cost effectiveness in laser lithotripsy (52.4% vs 82%)[40]. However, a prospective trial comparing EHL vs ESWL showed no difference in success rates for clearing the CBD, duration and cost of hospitalization between the two modalities[24].
In the United States, ESWL is rarely performed for management of biliary stones and most centers prefer cholangioscopy-guided LL or EHL for this purpose.
Cholangioscopy-guided lithotripsy
EHL or LL is ideally performed under direct visual control using a cholangioscope. The traditional cholangioscopy systems consist of a duodenoscope (also called “mother scope”) and a dedicated cholangioscope (also called “baby scope” or “daughter scope”) which is introduced into the bile duct through the accessory channel of the mother scope. The baby scope itself has an instrument channel through which the EHL or laser probe is introduced. Peroral cholangioscopy guided EHL or LL is cumbersome and can be labor intensive requiring an additional endoscopic unit and often participation of two skilled endoscopists, one to handle the duodenoscope and the other to maneuver the cholangioscope. The traditional cholangioscopes are capable of only 2-way steering, which may limit the field of view. These cholangioscopes are also extremely vulnerable to damage, requiring frequent expensive repairs. Furthermore, sharp angulations in the biliary tree may limit access into intrahepatic ducts or the cystic duct[47].
To negate these limitations, the Spyglass Direct Visualization System (Boston Scientific Corp, Natick, Mass) was designed for single operator examination of the bile ducts, 4-way steering, and dedicated irrigation channels[48,49]. In a large international multicenter study conducted at 10 centers in the United States and 5 centers in Europe, ductal clearance was successfully achieved in 71% of the patients using the Spyglass cholangioscopy system[50]. Despite its effectiveness, the spyglass system has been underutilized mainly due to its fiber optic image quality which is inferior to the video image quality offered by the new videocholangioscopes[51].
Direct peroral cholangioscopy
In direct peroral cholangioscopy (DPOC), an ultraslim upper endoscope is maneuvered across the biliary sphincter and into the bile duct for direct observation. With the introduction of high-definition ultraslim endoscopes with narrow band imaging capability, direct peroral cholangioscopy has gained popularity. This is mainly due to the many advantages of this technique. Compared to ductoscopy using a dedicated cholangioscope, direct cholangioscopy has several advantages. It offers a single operator platform, digital image quality and simultaneous irrigation and therapeutic capabilities. The most profound disadvantage of DPOC, however, is the difficulty associated with traversing the biliary sphincter to gain access to the bile duct. This is mainly due to looping of the ultraslim upper endoscope in the stomach or in the duodenum. To enhance the success rate of DPOC, specialized accessories or techniques are needed to advance the ultra slim endoscope into the proximal biliary system.
Larghi and Waxman[52] reported their experience in which the ultraslim upper endoscope was inserted with the aid of a guidewire placed during ERCP to maintain access. Additional use of manual pressure applied on the patient’s abdomen has been shown to ease the passage of the ultraslim endoscope into the hilar area in some patients[53]. The main drawback encountered with passage of an ultraslim upper endoscope over a guidewire for gaining access to the bile duct is the dislodgement of the guidewire from the bile duct and also large loop formation hindering the entrance of the endoscope into the biliary system. Moon et al[54] demonstrated the ropeway technique using an intraductal balloon that can be anchored within an intrahepatic bile duct to advance an ultraslim upper endoscope into the biliary tree for performance of DPOC. However, withdrawal of the balloon may cause technical difficulties in maintaining access which underscores the need for other accessories to maintain the scope’s position within the bile duct. The same group also reported use of an overtube balloon originally designed for double balloon enteroscopy to facilitate the introduction of an ultraslim upper endoscope into the biliary tree[55]. However the large inner diameter of the overtube (10.8 mm) compared to the outer diameter of the ultraslim upper endoscopes (5.2-6 mm), makes it difficult to manipulate both instruments and results in discomfort to the patient, looping of the endoscope in the duodenum, and difficulty in reaching the proximal bile duct[55,56].
In a recent study, we assessed utility of a novel anchoring balloon for performance of DPOC. Use of the anchoring balloon allowed consistent access to the biliary tree for performance of diagnostic and therapeutic DPOC distal to the confluence of the right and left hepatic ducts. More proximal access, however, was challenging owing to looping of the ultraslim endoscope after balloon removal.
Efforts are underway to develop the combined use of an intraductal anchoring balloon and an overtube especially designed for DPOC. Very recently, air embolism was reported following DPOC, resulting in a left sided hemiparesis[57]. Endoscopists must be conscious of the fact that air embolism could remain asymptomatic, as in regional embolism (portal venous gas) or manifest as hypoxia, shock, cardiac arrest or cerebral ischemia as noted in this case[57].
Once the hurdle of introducing an ultraslim upper endoscope into the bile duct has been overcome, a laser or an EHL probe can easily be passed through the working channel of the ultraslim endoscope. Stones can be directly visualized before and during lithotripsy by DPOC (Figure 4). Lithotripsy is performed using this technique until the stones are satisfactorily fragmented to allow removal through the biliary sphincter. In a small study with 18 patients who had failed conventional endoscopic therapy including ML, DPOC guided EHL or LL was successful in approximately 90% of the patients with an average of 1.6 treatment sessions per patient[58].
Figure 4.
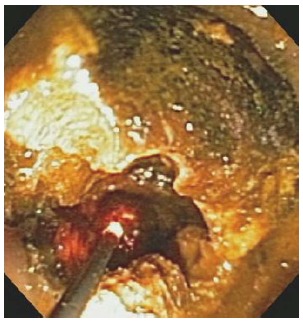
Direct peroral cholangioscopy guided laser lithotripsy of a bile duct stone. The red laser light makes targeting of the stone easier).
Specialized ultraslim upper endoscopes are being designed to facilitate access to the biliary tree for DPOC[59]. Ultraslim upper endoscopes can be passed through the nasal cavity for performance of DPOC. Direct transnasal cholangioscopy has been reported for successful extraction of CBD stones[60].
Endoscopic papillary balloon dilatation
Endoscopic papillary balloon dilation (EPBD) was introduced as an alternative to endoscopic sphincterotomy for removal of bile duct stones in 1980’s[61]. In an initial report involving 10 patients with CBD stones, biliary sphincteroplasty to 15 mm allowed removal of CBD stones in 6 patients[61]. In the other 4 patients, ductal clearance required a combination of biliary sphincterotomy and mechanical lithotripsy. The use of large diameter papillary balloon dilatation (up to 20 mm in diameter) for management of difficult to remove biliary stones was reported by Ersoz et al[62] in 2003. They reported a high success rate for stone removal. However, their complication rate was also high. Several reports have suggested that EPBD is associated with risk of severe pancreatitis which raises safety concern of this procedure[61,63]. In our institution, we use EPBD selectively and try to avoid its use in those with high risk of post ERCP pancreatitis (Figure 5).
Figure 5.

Large diameter papillary balloon dilatation to remove bile duct stone.
Since those initial reports, multiple studies have shown that EPBD alone or in combination with other techniques can be of use for management of difficult to remove biliary stones[62-68]. EPBD is especially attractive in patients who are at risk for bleeding after endoscopic sphincterotomy or in those with altered anatomy in whom a full sphincterotomy cannot be successfully achieved.
Some authors have suggested that the stone recurrence rate may also be higher with EPBD than with endoscopic sphincterotomy and mechanical lithotripsy[69]. However the results of a Japanese multicentric trial with a mean follow up of 6.7 years demonstrated that there is lesser risk of stone recurrence following EPBD when compared with sphincterotomy[70]. Further, a recent meta-analysis which included 15 randomized trials comparing EPBD and endoscopic sphincterotomy showed reduced risk of bleeding and infections and is especially indicated in older patients, those who are at risk for infection and coagulopathy[71]. Despite its effectiveness, EPBD has been associated with serious complications[63]. A higher risk of post ERCP pancreatitis has been observed which has been attributed to the inadequately loosened sphincter of Oddi and the intra mucosal hemorrhage and inflammation/edema around the papilla. This may cause compression of the pancreatic duct and may accentuate the risk of pancreatitis[72]. In this regard, a randomized controlled trial demonstrated that a 5-min dilation time as opposed to the conventional 1-min time resulted in an adequately loosened sphincter of Oddi and consequently reduced the risk of post ERCP pancreatitis and improved its efficacy[73]. The rate of these complications can be reduced by strict patient selection, avoidance of forced procedures, optimal dilation duration and immediate conversion to an alternative procedure if any difficulty is encountered during EPBD.
Endoscopic biliary stenting
In very old patients and those with serious co-morbidities where other endoscopic or surgical procedures may confer unacceptably high risks, endoscopic biliary stenting is a useful alternative[69]. Biliary drainage by stenting is mandatory if ductal clearance cannot be achieved during ERCP or in between procedures in patients who require more than one session for ductal clearance. CBD stones have been reported to reduce in size in 60% of patients within one to two years after biliary stenting[69].
Mechanical irritation of the stent on the stone is postulated to be one of the mechanisms.
In a study involving 28 geriatric patients with CBD stones refractory to conventional endoscopic removal, endoscopic biliary stent placement combined with oral ursodeoxycholic acid and terpene therapy for a mean of six months led to significant reduction in the size of CBD stone[74]. Subsequently, endoscopic stone removal was successfully performed in 26 of 28 patients with a mean of 1.7 ERCP procedures. This combination therapy may be of use for treatment of difficult to remove CBD stones in a subset of patients with significant co-morbidities and intolerance to prolonged endoscopic treatment modalities.
In conclusion, the past several years have witnessed the emergence of new technologies and techniques for management of difficult to remove biliary stones. Treatment of such stones is generally accomplished using a multimodal approach combining conventional techniques such as endoscopic sphincterotomy, use of extraction balloons and baskets and mechanical lithotripsy, with newer techniques such as cholangioscopy guided laser or electrohydraulic lithotripsy. Recent advances in the development of videocholangioscopes, single operator catheter-based cholangioscopes and specially-designed ultrathin upper endoscopes for DPOC have made lithotripsy under direct visual guidance safer, more reliable, and more routine. Future studies will certainly shed more light on the safety of different modalities for stone extraction and will help determine the best management approach for different subgroup of patients with difficult to remove bile duct stones.
Footnotes
P- Reviewer Al Mofleh IA S- Editor Gou SX L- Editor A E- Editor Zhang DN
References
- 1.Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol. 2006;12:3162–3167. doi: 10.3748/wjg.v12.i20.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samardzic J, Latic F, Kraljik D, Pitlovic V, Mrkovic H, Miskic D, Latic A, Delibegovic S. Treatment of common bile duct stones--is the role of ERCP changed in era of minimally invasive surgery? Med Arh. 2010;64:187–188. [PubMed] [Google Scholar]
- 3.Strömberg C, Nilsson M. Nationwide study of the treatment of common bile duct stones in Sweden between 1965 and 2009. Br J Surg. 2011;98:1766–1774. doi: 10.1002/bjs.7690. [DOI] [PubMed] [Google Scholar]
- 4.Cairns SR, Dias L, Cotton PB, Salmon PR, Russell RC. Additional endoscopic procedures instead of urgent surgery for retained common bile duct stones. Gut. 1989;30:535–540. doi: 10.1136/gut.30.4.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parsi MA, Stevens T, Dumot JA, Zuccaro G. Endoscopic therapy of recurrent acute pancreatitis. Cleve Clin J Med. 2009;76:225–233. doi: 10.3949/ccjm.76a.08017. [DOI] [PubMed] [Google Scholar]
- 6.Binmoeller KF, Brückner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy. 1993;25:201–206. doi: 10.1055/s-2007-1010293. [DOI] [PubMed] [Google Scholar]
- 7.McHenry L, Lehman G. Difficult bile duct stones. Curr Treat Options Gastroenterol. 2006;9:123–132. doi: 10.1007/s11938-006-0031-6. [DOI] [PubMed] [Google Scholar]
- 8.Kim HJ, Choi HS, Park JH, Park DI, Cho YK, Sohn CI, Jeon WK, Kim BI, Choi SH. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007;66:1154–1160. doi: 10.1016/j.gie.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 9.Lauri A, Horton RC, Davidson BR, Burroughs AK, Dooley JS. Endoscopic extraction of bile duct stones: management related to stone size. Gut. 1993;34:1718–1721. doi: 10.1136/gut.34.12.1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riemann JF, Seuberth K, Demling L. Clinical application of a new mechanical lithotripter for smashing common bile duct stones. Endoscopy. 1982;14:226–230. doi: 10.1055/s-2007-1021626. [DOI] [PubMed] [Google Scholar]
- 11.Schneider MU, Matek W, Bauer R, Domschke W. Mechanical lithotripsy of bile duct stones in 209 patients--effect of technical advances. Endoscopy. 1988;20:248–253. doi: 10.1055/s-2007-1018186. [DOI] [PubMed] [Google Scholar]
- 12.Leung JW, Tu R. Mechanical lithotripsy for large bile duct stones. Gastrointest Endosc. 2004;59:688–690. doi: 10.1016/S0016-5107(04)00174-9. [DOI] [PubMed] [Google Scholar]
- 13.Thomas M, Howell DA, Carr-Locke D, Mel Wilcox C, Chak A, Raijman I, Watkins JL, Schmalz MJ, Geenen JE, Catalano MF. Mechanical lithotripsy of pancreatic and biliary stones: complications and available treatment options collected from expert centers. Am J Gastroenterol. 2007;102:1896–1902. doi: 10.1111/j.1572-0241.2007.01350.. [DOI] [PubMed] [Google Scholar]
- 14.Chung SC, Leung JW, Leong HT, Li AK. Mechanical lithotripsy of large common bile duct stones using a basket. Br J Surg. 1991;78:1448–1450. doi: 10.1002/bjs.1800781214. [DOI] [PubMed] [Google Scholar]
- 15.Cipolletta L, Costamagna G, Bianco MA, Rotondano G, Piscopo R, Mutignani M, Marmo R. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84:1407–1409. doi: 10.1002/bjs.1800841019. [DOI] [PubMed] [Google Scholar]
- 16.Garg PK, Tandon RK, Ahuja V, Makharia GK, Batra Y. Predictors of unsuccessful mechanical lithotripsy and endoscopic clearance of large bile duct stones. Gastrointest Endosc. 2004;59:601–605. doi: 10.1016/S0016-5107(04)00295-0. [DOI] [PubMed] [Google Scholar]
- 17.Shim CS. How Should Biliary Stones be Managed? Gut Liver. 2010;4:161–172. doi: 10.5009/gnl.2010.4.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shim CS. How Should Biliary Stones be Managed? Gut Liver. 2010;4:161–172. doi: 10.5009/gnl.2010.4.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koch H, Stolte M, Walz V. Endoscopic lithotripsy in the common bile duct. Endoscopy. 1977;9:95–98. doi: 10.1055/s-0028-1098497. [DOI] [PubMed] [Google Scholar]
- 20.Seitz U, Bapaye A, Bohnacker S, Navarrete C, Maydeo A, Soehendra N. Advances in therapeutic endoscopic treatment of common bile duct stones. World J Surg. 1998;22:1133–1144. doi: 10.1007/s002689900532. [DOI] [PubMed] [Google Scholar]
- 21.Yoo KS, Lehman GA. Endoscopic management of biliary ductal stones. Gastroenterol Clin North Am. 2010;39:209–27, viii. doi: 10.1016/j.gtc.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 22.Blind PJ, Lundmark M. Management of bile duct stones: lithotripsy by laser, electrohydraulic, and ultrasonic techniques. Report of a series and clinical review. Eur J Surg. 1998;164:403–409. doi: 10.1080/110241598750004201. [DOI] [PubMed] [Google Scholar]
- 23.Arya N, Nelles SE, Haber GB, Kim YI, Kortan PK. Electrohydraulic lithotripsy in 111 patients: a safe and effective therapy for difficult bile duct stones. Am J Gastroenterol. 2004;99:2330–2334. doi: 10.1111/j.1572-0241.2004.40251.. [DOI] [PubMed] [Google Scholar]
- 24.Adamek HE, Buttmann A, Wessbecher R, Kohler B, Riemann JF. Clinical comparison of extracorporeal piezoelectric lithotripsy (EPL) and intracorporeal electrohydraulic lithotripsy (EHL) in difficult bile duct stones. A prospective randomized trial. Dig Dis Sci. 1995;40:1185–1192. doi: 10.1007/BF02065522. [DOI] [PubMed] [Google Scholar]
- 25.Adamek HE, Maier M, Jakobs R, Wessbecher FR, Neuhauser T, Riemann JF. Management of retained bile duct stones: a prospective open trial comparing extracorporeal and intracorporeal lithotripsy. Gastrointest Endosc. 1996;44:40–47. doi: 10.1016/s0016-5107(96)70227-4. [DOI] [PubMed] [Google Scholar]
- 26.Leung JW, Chung SS. Electrohydraulic lithotripsy with peroral choledochoscopy. BMJ. 1989;299:595–598. doi: 10.1136/bmj.299.6699.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yasuda K, Nakajima M, Cho E, Mukai H, Kawai K. Comparison of peroral and percutaneous cholangioscopy. Endoscopy. 1989;21 Suppl 1:347–350. doi: 10.1055/s-2007-1012988. [DOI] [PubMed] [Google Scholar]
- 28.Moon JH, Cha SW, Ryu CB, Kim YS, Hong SJ, Cheon YK, Cho YD, Kim YS, Lee JS, Lee MS, et al. Endoscopic treatment of retained bile-duct stones by using a balloon catheter for electrohydraulic lithotripsy without cholangioscopy. Gastrointest Endosc. 2004;60:562–566. doi: 10.1016/S0016-5107(04)02012-7. [DOI] [PubMed] [Google Scholar]
- 29.Hui CK, Lai KC, Ng M, Wong WM, Yuen MF, Lam SK, Lai CL, Wong BC. Retained common bile duct stones: a comparison between biliary stenting and complete clearance of stones by electrohydraulic lithotripsy. Aliment Pharmacol Ther. 2003;17:289–296. doi: 10.1046/j.1365-2036.2003.01415.. [DOI] [PubMed] [Google Scholar]
- 30.DiSario J, Chuttani R, Croffie J, Liu J, Mishkin D, Shah R, Somogyi L, Tierney W, Song LM, Petersen BT. Biliary and pancreatic lithotripsy devices. Gastrointest Endosc. 2007;65:750–756. doi: 10.1016/j.gie.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 31.Lux G, Ell C, Hochberger J, Müller D, Demling L. The first successful endoscopic retrograde laser lithotripsy of common bile duct stones in man using a pulsed neodymium-YAG laser. Endoscopy. 1986;18:144–145. doi: 10.1055/s-2007-1018356. [DOI] [PubMed] [Google Scholar]
- 32.Ponchon T, Gagnon P, Valette PJ, Henry L, Chavaillon A, Thieulin F. Pulsed dye laser lithotripsy of bile duct stones. Gastroenterology. 1991;100:1730–1736. doi: 10.1016/0016-5085(91)90676-c. [DOI] [PubMed] [Google Scholar]
- 33.Ell C, Hochberger J, May A, Fleig WE, Bauer R, Mendez L, Hahn EG. Laser lithotripsy of difficult bile duct stones by means of a rhodamine-6G laser and an integrated automatic stone-tissue detection system. Gastrointest Endosc. 1993;39:755–762. doi: 10.1016/S0016-5107(93)70259-X. [DOI] [PubMed] [Google Scholar]
- 34.Kim TH, Oh HJ, Choi CS, Yeom DH, Choi SC. Clinical usefulness of transpapillary removal of common bile duct stones by frequency doubled double pulse Nd: YAG laser. World J Gastroenterol. 2008;14:2863–2866. doi: 10.3748/wjg.14.2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hochberger J, Bayer J, Maiss J, Tex S, Hahn EG. [Clinical results with a new frequency-doubled, double pulse Nd: YAG laser (FREDDY) for lithotripsy in complicated choledocholithiasis] Biomed Tech (Berl) 1998;43 Suppl:172. doi: 10.1515/bmte.1998.43.s1.172. [DOI] [PubMed] [Google Scholar]
- 36.Hochberger J, Bayer J, May A, Mühldorfer S, Maiss J, Hahn EG, Ell C. Laser lithotripsy of difficult bile duct stones: results in 60 patients using a rhodamine 6G dye laser with optical stone tissue detection system. Gut. 1998;43:823–829. doi: 10.1136/gut.43.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neuhaus H, Zillinger C, Born P, Ott R, Allescher H, Rösch T, Classen M. Randomized study of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for difficult bile duct stones. Gastrointest Endosc. 1998;47:327–334. doi: 10.1016/S0016-5107(98)70214-7. [DOI] [PubMed] [Google Scholar]
- 38.Jakobs R, Adamek HE, Maier M, Krömer M, Benz C, Martin WR, Riemann JF. Fluoroscopically guided laser lithotripsy versus extracorporeal shock wave lithotripsy for retained bile duct stones: a prospective randomised study. Gut. 1997;40:678–682. doi: 10.1136/gut.40.5.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee JE, Moon JH, Choi HJ, Song AR, Jung EK, Cheon YK, Cho YD, Lee JS, Lee MS. Endoscopic treatment of difficult bile duct stones by using a double-lumen basket for laser lithotripsy--a case series. Endoscopy. 2010;42:169–172. doi: 10.1055/s-0029-1215353. [DOI] [PubMed] [Google Scholar]
- 40.den Toom R, Nijs HG, van Blankenstein M, Laméris JS, Schröder FH, Terpstra OT. Extracorporeal shock wave treatment of common bile duct stones: experience with two different lithotriptors at a single institution. Br J Surg. 1991;78:809–813. doi: 10.1002/bjs.1800780714. [DOI] [PubMed] [Google Scholar]
- 41.White DM, Correa RJ, Gibbons RP, Ball TJ, Kozarek RJ, Thirlby RC. Extracorporeal shock-wave lithotripsy for bile duct calculi. Am J Surg. 1998;175:10–13. doi: 10.1016/S0002-9610(97)00234-1. [DOI] [PubMed] [Google Scholar]
- 42.Tandan M, Reddy DN, Santosh D, Reddy V, Koppuju V, Lakhtakia S, Gupta R, Ramchandani M, Rao GV. Extracorporeal shock wave lithotripsy of large difficult common bile duct stones: efficacy and analysis of factors that favor stone fragmentation. J Gastroenterol Hepatol. 2009;24:1370–1374. doi: 10.1111/j.1440-1746.2009.05919.x. [DOI] [PubMed] [Google Scholar]
- 43.Amplatz S, Piazzi L, Felder M, Comberlato M, Benvenuti S, Zancanella L, Di Fede F, de’Guelmi A, Bertozzo A, Farris P, et al. Extracorporeal shock wave lithotripsy for clearance of refractory bile duct stones. Dig Liver Dis. 2007;39:267–272. doi: 10.1016/j.dld.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 44.Sauerbruch T, Stern M. Fragmentation of bile duct stones by extracorporeal shock waves. A new approach to biliary calculi after failure of routine endoscopic measures. Gastroenterology. 1989;96:146–152. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 45.Parsi MA, Stevens T, Lopez R, Vargo JJ. Extracorporeal shock wave lithotripsy for prevention of recurrent pancreatitis caused by obstructive pancreatic stones. Pancreas. 2010;39:153–155. doi: 10.1097/MPA.0b013e3181bb1733. [DOI] [PubMed] [Google Scholar]
- 46.Conigliaro R, Camellini L, Zuliani CG, Sassatelli R, Mortilla MG, Bertoni G, Formisano D, Bedogni G. Clearance of irretrievable bile duct and pancreatic duct stones by extracorporeal shockwave lithotripsy, using a transportable device: effectiveness and medium-term results. J Clin Gastroenterol. 2006;40:213–219. doi: 10.1097/00004836-200603000-00008. [DOI] [PubMed] [Google Scholar]
- 47.Chathadi KV, Chen YK. New kid on the block: development of a partially disposable system for cholangioscopy. Gastrointest Endosc Clin N Am. 2009;19:545–555. doi: 10.1016/j.giec.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 48.Chen YK. Preclinical characterization of the Spyglass peroral cholangiopancreatoscopy system for direct access, visualization, and biopsy. Gastrointest Endosc. 2007;65:303–311. doi: 10.1016/j.gie.2006.07.048. [DOI] [PubMed] [Google Scholar]
- 49.Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video) Gastrointest Endosc. 2007;65:832–841. doi: 10.1016/j.gie.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 50.Chen YK, Parsi MA, Binmoeller KF, Hawes RH, Pleskow DK, Slivka A, Haluszka O, Petersen BT, Sherman S, Devière J, et al. Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos) Gastrointest Endosc. 2011;74:805–814. doi: 10.1016/j.gie.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 51.Parsi MA. Peroral cholangioscopy in the new millennium. World J Gastroenterol. 2011;17:1–6. doi: 10.3748/wjg.v17.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853–857. doi: 10.1016/j.gie.2005.07.050. [DOI] [PubMed] [Google Scholar]
- 53.Park do H, Park BW, Lee HS, Park SH, Park JH, Lee SH, Kim HS, Kim SJ. Peroral direct cholangioscopic argon plasma coagulation by using an ultraslim upper endoscope for recurrent hepatoma with intraductal nodular tumor growth (with videos) Gastrointest Endosc. 2007;66:201–203. doi: 10.1016/j.gie.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 54.Moon JH, Ko BM, Choi HJ, Hong SJ, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Intraductal balloon-guided direct peroral cholangioscopy with an ultraslim upper endoscope (with videos) Gastrointest Endosc. 2009;70:297–302. doi: 10.1016/j.gie.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 55.Choi HJ, Moon JH, Ko BM, Hong SJ, Koo HC, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos) Gastrointest Endosc. 2009;69:935–940. doi: 10.1016/j.gie.2008.08.043. [DOI] [PubMed] [Google Scholar]
- 56.Tsou YK, Lin CH, Tang JH, Liu NJ, Cheng CL. Direct peroral cholangioscopy using an ultraslim endoscope and overtube balloon-assisted technique: a case series. Endoscopy. 2010;42:681–684. doi: 10.1055/s-0030-1255616. [DOI] [PubMed] [Google Scholar]
- 57.Efthymiou M, Raftopoulos S, Antonio Chirinos J, May GR. Air embolism complicated by left hemiparesis after direct cholangioscopy with an intraductal balloon anchoring system. Gastrointest Endosc. 2012;75:221–223. doi: 10.1016/j.gie.2011.01.038. [DOI] [PubMed] [Google Scholar]
- 58.Moon JH, Ko BM, Choi HJ, Koo HC, Hong SJ, Cheon YK, Cho YD, Lee MS, Shim CS. Direct peroral cholangioscopy using an ultra-slim upper endoscope for the treatment of retained bile duct stones. Am J Gastroenterol. 2009;104:2729–2733. doi: 10.1038/ajg.2009.435. [DOI] [PubMed] [Google Scholar]
- 59.Itoi T, Moon JH, Waxman I. Current status of direct peroral cholangioscopy. Dig Endosc. 2011;23 Suppl 1:154–157. doi: 10.1111/j.1443-1661.2011.01114.x. [DOI] [PubMed] [Google Scholar]
- 60.Seo MS, Moon JH, Choi HJ, Kim HK, Cheon YK, Cho YD, Lee MS. Bile-Duct Stone Removal under Direct Transnasal Cholangioscopy Using an Ultraslim Upper Endoscope. Gut Liver. 2010;4:428–429. doi: 10.5009/gnl.2010.4.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilatation, a possible alternative to endoscopic papillotomy. Lancet. 1982;1:1306–1307. doi: 10.1016/S0140-6736(82)92873-2. [DOI] [PubMed] [Google Scholar]
- 62.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 63.Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–1299. doi: 10.1053/j.gastro.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 64.Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560–565. doi: 10.1038/ajg.2008.67. [DOI] [PubMed] [Google Scholar]
- 65.Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M, et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278–285. doi: 10.1038/ajg.2010.421. [DOI] [PubMed] [Google Scholar]
- 66.Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–76; quiz 768, 771. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 67.Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, Ajmere N, Ste Marie RW, Bhattacharya K, Gupta K, et al. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67:1046–1052. doi: 10.1016/j.gie.2007.08.047. [DOI] [PubMed] [Google Scholar]
- 68.May GR, Cotton PB, Edmunds SE, Chong W. Removal of stones from the bile duct at ERCP without sphincterotomy. Gastrointest Endosc. 1993;39:749–754. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 69.Lee DK, Jahng JH. Alternative methods in the endoscopic management of difficult common bile duct stones. Dig Endosc. 2010;22 Suppl 1:S79–S84. doi: 10.1111/j.1443-1661.2010.00960.x. [DOI] [PubMed] [Google Scholar]
- 70.Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K, Maeshiro K, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185–1191. doi: 10.1016/j.gie.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 71.Weinberg BM, Shindy W, Lo S. Endoscopic balloon sphincter dilation (sphincteroplasty) versus sphincterotomy for common bile duct stones. Cochrane Database Syst Rev. 2006;(4):CD004890. doi: 10.1002/14651858.CD004890.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455–1460. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 73.Liao WC, Lee CT, Chang CY, Leung JW, Chen JH, Tsai MC, Lin JT, Wu MS, Wang HP. Randomized trial of 1-minute versus 5-minute endoscopic balloon dilation for extraction of bile duct stones. Gastrointest Endosc. 2010;72:1154–1162. doi: 10.1016/j.gie.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 74.Han J, Moon JH, Koo HC, Kang JH, Choi JH, Jeong S, Lee DH, Lee MS, Kim HG. Effect of biliary stenting combined with ursodeoxycholic acid and terpene treatment on retained common bile duct stones in elderly patients: a multicenter study. Am J Gastroenterol. 2009;104:2418–2421. doi: 10.1038/ajg.2009.303. [DOI] [PubMed] [Google Scholar]


