Abstract
A 38-year-old female with a history of alcoholic liver cirrhosis visited our hospital with a massive hematochezia. An esophagogastroduodenoscopy did not demonstrate any bleeding source, and a colonoscopy showed a massive hemorrhage in the ascending colon but without an obvious focus. The source of the bleeding could not be found with a mesenteric artery angiography. We performed an enhanced abdominal computed tomography, which revealed a distal ascending colonic varix, and assumed that the varix was the source of the bleeding. We performed a venous coil embolization and histoacryl injection to obliterate the colon varix. The intervention appeared to be successful because the vital signs and hemoglobin laboratory data remained stable and because the hematochezia was no longer observed. We report here on a rare case of colonic variceal bleeding that was treated with venous coil embolization.
Keywords: Colon ascending, Varicose veins, Liver cirrhosis, Therapeutic embolization
INTRODUCTION
Colonic variceal bleeding is a very rare cause of lower gastrointestinal bleeding. Fewer than 100 cases of colonic variceal bleeding have been reported in English literature and few case reports exist in South Korea. However, most cases in South Korea were caused by different varix locations, etiologies and treatments. A single case in South Korea with ascending colonic variceal bleeding caused by alcoholic liver cirrhosis was treated with a hemicolectomy[1]. We report the first case of an ascending colon variceal bleed caused by alcoholic liver cirrhosis that was treated with venous coil embolization in South Korea.
CASE REPORT
A 38-year-old female was admitted to our hospital with massive hematochezia and hemodynamic instability. She was diagnosed with alcoholic liver cirrhosis (Child-Pugh classification C) 6 years ago and had multiple hospitalizations with complications of esophageal variceal bleeding and hepatic encephalopathy. Upon physical examination, her initial blood pressure was 80/50 mmHg, her heart rate was 110 bpm, her respiration was 28 bpm and her body temperature was 37 °C. No evidence of bleeding was detected with nasogastric tube irrigation. Abnormal laboratory data upon admission included the following: hemoglobin 7.0 g/dL, hematocrit 22.3%, platelets 59 000/mm3, serum creatinine 2.31 mg/dL, international normalized ratio 1.98, and albumin 2.1 g/dL.
An esophagogastroduodenoscopy demonstrated esophageal varices grade III but did not show signs of recent bleeding. The colonoscopy showed fresh blood from the ascending colon to the rectum, but there was no evidence of bleeding in the terminal ileum, which demonstrated that the origin of the bleeding could be assumed to be in the ascending colon (Figure 1). Diagnostic angiographies of the superior and inferior mesenteric arteries were performed, but the source of the bleeding could not be found (Figure 2). Even with 2 units of packed RBCs, the hemoglobin level dropped to 5.6 g/dL the next day, and the vital signs remained unstable.
Figure 1.
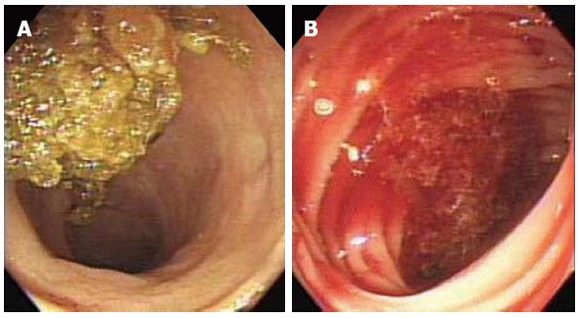
Initial colonoscopy. A: The terminal ileum showing yellowish-colored stool with no evidence of upper gastrointestinal bleeding; B: The ascending colon showing fresh blood without an observable source.
Figure 2.
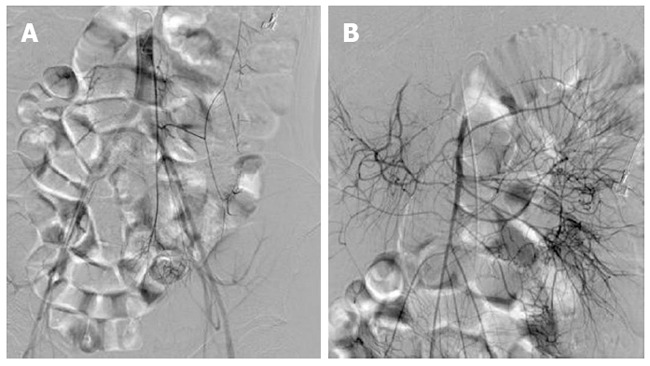
Mesenteric artery angiography. A: The inferior mesenteric artery angiography showing no source of bleeding; B: The superior mesenteric artery angiography showing no source of bleeding.
A second colonoscopy was still unable to visualize the bleeding focus and only detected a massive hemorrhage in the ascending colon (Figure 3). We performed an enhanced abdominal computed tomography (CT), which revealed the formation of a varix surrounding and protruding inside the distal ascending colon by the portacaval shunt (Figure 4). The varix was thought to be the source of the gastrointestinal bleeding. We planned an operation, but a right hemicolectomy could not be performed due to poor vital signs and abnormal coagulopathy. Initially, we tried to perform a Balloon-Occluded Retrograde Transvenous Obliteration (BRTO) but failed due to the selection of the portacaval shunt. Because the patient had unstable vital signs that required immediate intervention, we performed a coil embolization and histoacryl injection to obliterate the varix (Figure 5). After the coil embolization and 4 units of packed red blood cells, the patient’s hemoglobin level rose to 10.0 g/dL, where it stabilized, and the vital signs (blood pressure and heart rate) recovered. There were no further signs of bleeding, such as hematochezia. However, the patient developed complications of pneumonia and renal failure, which led to multiorgan failure. Even with ventilator care and continuous renal replacement therapy, the patient expired 2 wk after the intervention.
Figure 3.
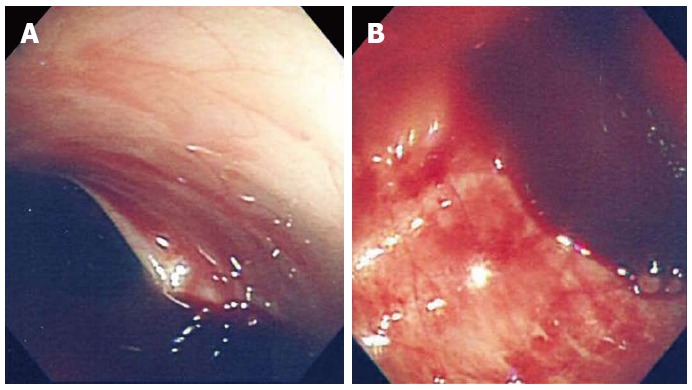
The second colonoscopy. A: Massive hemorrhage within the proximal ascending colon without a definite bleeding focus; B: Fresh blood within the distal ascending colon without a definite bleeding focus.
Figure 4.
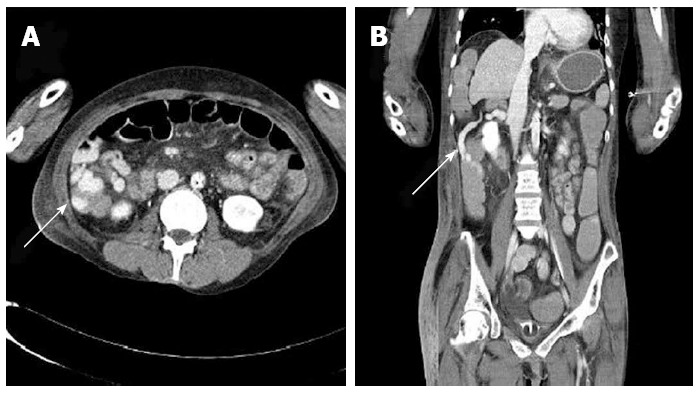
Abdominal computed tomography. A: Portal phase axial view with white arrow showing the varix surrounding and protruding inside the ascending colon formed by portacaval shunt; B: Coronal view with white arrow showing the colon varix.
Figure 5.
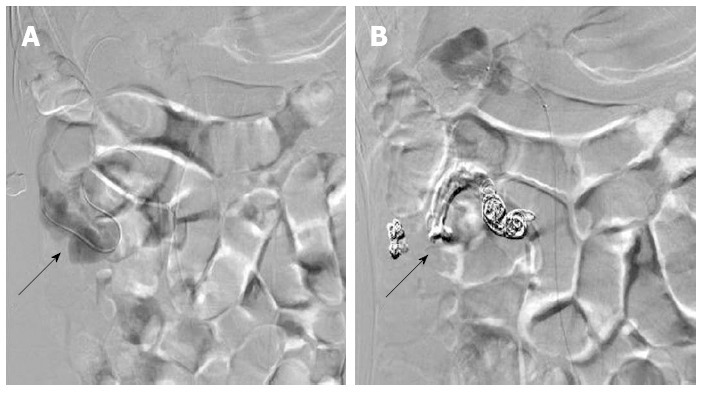
Venous coil embolization. A: Venography showing the varix within the ascending colon (black arrow); B: Coil embolization (black arrow) and histoacryl injection was performed to obliterate the varix.
DISCUSSION
Colon varices are a very rare cause of lower gastrointestinal bleeding, with a reported incidence of 0.07%[2]. Colon varices can be associated with several conditions, such as portal hypertension, portal venous obstruction, postsurgical changes and idiopathic factors, but the vast majority of colonic varices are related to portal hypertension caused by cirrhosis or portal vein obstruction. Embryologically derived anastomoses between the portal and systemic systems exist in the esophagus, terminal ileum, colon, retroperitoneum, and anterior abdominal wall[3]. The most common sites of colonic varices are the rectum and cecum[4]. Colon varices with portal hypertension are hypothesized to arise in patients in whom the colonic portosystemic venous collateral network is highly developed[5]. The rate of colonic variceal bleeding that causes lower gastrointestinal bleeding with liver cirrhosis is approximately 1%-8%[6,7]. Thus, if a patient has a history of liver cirrhosis and has massive gastrointestinal bleeding, the possibility of colon variceal bleeding should also be considered. Other than portal hypertension, mesenteric venous or splenic vein obstruction, which may be due to thrombosis, tumor invasion, extrinsic compression, acute or chronic pancreatitis, mesenteric adhesions, or congenital anatomic variations, may cause a colon varix. With no etiology, colon varix is classified as idiopathic or primary[5].
A colonoscopy is the principal method for the diagnosis of colon varices, but with massive bleeding, the diagnostic rate of a colonoscopy is 69% (range: 48%-90%) because the varices may be obscured by blood[8]. Thus, in case of massive hematochezia, magnetic resonance imaging, mesenteric angiography and abdominal CT are alternative diagnostic tools[9,10].
Management of colonic variceal bleeding has not been standardized. In a report describing a case of massive lower gastrointestinal bleeding with some hemodynamic instability caused by colonic varix, an operation was the optimal choice[11]. However, most cases with colonic variceal bleeding are associated with cirrhotic liver, which makes many cases inoperable due to coagulopathy. Thus, interventional therapies are tested depending on the underlying etiology and the distribution of the varices. These therapies include transhepatic intravenous portosystemic shunt (TIPS), BRTO, endoscopic variceal ligation, somatostatin infusion, argon plasma coagulation, histoacryl injection, and coil embolization[12-15]. Four other cases of colon variceal bleeding have been described in South Korea. Theses cases had different varix locations, etiologies and treatments compared to our case. The first case was a 64-year-old female with liver cirrhosis who had descending colon variceal bleeding that was treated with a left hemicolectomy[16]. The second case was a 24-year-old male who had idiopathic rectal variceal bleeding that was treated with low anterior resection[2]. The third case was a 43-year-old male with ascending colon variceal bleeding due to alcoholic liver cirrhosis. This case was very similar to our case but was treated with a right hemicolectomy[1]. The last case was a 33-year-old woman with a history of systemic lupus erythematosus who developed antiphospholipid syndrome and had ascending colon variceal bleeding that was treated with octreotide, a beta-blocker and warfarin[17]. In our case, the patient was inoperable because of the poor vital signs and coagulopathy caused by the abnormal liver function. We initially tried to perform BRTO to obliterate the portacaval shunt, but the angiographic selection of the portacaval shunt failed. Thus, venous coil embolization along with a histoacryl injection was performed on the ascending colon varix. This technique seemed to be successful because the vital signs (blood pressure and heart rate) along with hemoglobin level remained stable, and no further evidence of gastrointestinal bleeding was observed after the intervention. This result is despite the fact that our patient expired due to complications of multiorgan failure because the patient already had terminal liver cirrhosis and had developed unstable vital signs before arriving in the emergency room. Together, these conditions made the patient susceptible to secondary infection and renal failure. Complications of the varix coil embolization procedure could also be considered after the intervention, such as necrosis, vessel perforation, non-targeting embolization and migration of the coil. However, although rate of complications has not been reported, this rate is thought to be very low because the procedure proceeds through a venous approach, and migration of the coil could be corrected during the procedure, and the patient did not complain of post-interventional symptoms such as abdominal pain, fever, or dyspnea. Thus, acute or delayed complications of the venous coil embolization were eliminated. A similar case in Switzerland included a 43-year-old male patient with ascending colon variceal bleeding due to alcoholic liver cirrhosis. The patient had TIPS initially to reduce the portosystemic pressure gradient, but the bleeding did not stop; the patient then underwent histoacryl injection and venous coil embolization. The patient recovered without further incidents[18]. As noted above, there is no standardized management of colon variceal bleeding, but venous coil embolization could be an effective treatment option for patients with massive hematochezia by the colon varix. Even though our patient could not survive due to multiple organ failure and secondary infection, we believe that the successful venous coil embolization had stopped the bleeding, which prevented a more aggressive progression. Our case is thought to be the first case in South Korea that used venous coil embolization to treat ascending colon variceal bleeding caused by alcoholic liver cirrhosis.
In conclusion, the treatment of colon variceal bleeding has not been well established. However, this case has shown that treatment with venous coil embolization on an ascending colon variceal bleeding caused by alcoholic liver cirrhosis is effective. We report here on the first case of ascending colon variceal bleeding caused by alcoholic liver cirrhosis that was treated with venous coil embolization in South Korea.
Footnotes
P- Reviewer De Nardi P S- Editor Gou SX L- Editor A E- Editor Zhang DN
References
- 1.Kim HU, Her KH, Kim SH, Kim BS, Kang YJ, Lee J, Kim KS. A case of variceal bleeding of the ascending colon associated with alcoholic liver cirrhosis. Korean J Med. 2008;75:215–220. [Google Scholar]
- 2.Han JH, Jeon WJ, Chae HB, Park SM, Youn SJ, Kim SH, Bae IH, Lee SJ. A case of idiopathic colonic varices: a rare cause of hematochezia misconceived as tumor. World J Gastroenterol. 2006;12:2629–2632. doi: 10.3748/wjg.v12.i16.2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards EA. Functional anatomy of the porta-systemic communications. AMA Arch Intern Med. 1951;88:137–154. doi: 10.1001/archinte.1951.03810080005002. [DOI] [PubMed] [Google Scholar]
- 4.Sato T, Akaike J, Toyota J, Karino Y, Ohmura T. Clinicopathological features and treatment of ectopic varices with portal hypertension. Int J Hepatol. 2011;2011:960720. doi: 10.4061/2011/960720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Francois F, Tadros C, Diehl D. Pan-colonic varices and idiopathic portal hypertension. J Gastrointestin Liver Dis. 2007;16:325–328. [PubMed] [Google Scholar]
- 6.Ganguly S, Sarin SK, Bhatia V, Lahoti D. The prevalence and spectrum of colonic lesions in patients with cirrhotic and noncirrhotic portal hypertension. Hepatology. 1995;21:1226–1231. [PubMed] [Google Scholar]
- 7.Hosking SW, Smart HL, Johnson AG, Triger DR. Anorectal varices, haemorrhoids, and portal hypertension. Lancet. 1989;1:349–352. doi: 10.1016/s0140-6736(89)91724-8. [DOI] [PubMed] [Google Scholar]
- 8.Abraham-Igwe C, Patel R. Idiopathic colonic varices: a case report. Endoscopy. 2002;34:680. doi: 10.1055/s-2002-33235. [DOI] [PubMed] [Google Scholar]
- 9.Chevallier P, Motamedi JP, Demuth N, Caroli-Bosc FX, Oddo F, Padovani B. Ascending colonic variceal bleeding: utility of phase-contrast MR portography in diagnosis and follow-up after treatment with TIPS and variceal embolization. Eur Radiol. 2000;10:1280–1283. doi: 10.1007/s003309900308. [DOI] [PubMed] [Google Scholar]
- 10.Choi JW, Lee CH, Kim KA, Park CM, Kim JY. Ectopic varices in colonic stoma: MDCT findings. Korean J Radiol. 2006;7:297–299. doi: 10.3348/kjr.2006.7.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopes LM, Ramada JM, Certo MG, Pereira PR, Soares JM, Ribeiro M, Areias J, Pinho C. Massive lower gastrointestinal bleeding from idiopathic ileocolonic varix: report of a case. Dis Colon Rectum. 2006;49:524–526. doi: 10.1007/s10350-005-0279-2. [DOI] [PubMed] [Google Scholar]
- 12.Allgaier HP, Ochs A, Haag K, Hauenstein KH, Tittor W, Rössle M, Blum HE. [Recurrent bleeding from colonic varices in portal hypertension. The successful prevention of recurrence by the implantation of a transjugular intrahepatic stent-shunt (TIPS)] Dtsch Med Wochenschr. 1995;120:1773–1776. doi: 10.1055/s-2008-1055541. [DOI] [PubMed] [Google Scholar]
- 13.Anan A, Irie M, Watanabe H, Sohda T, Iwata K, Suzuki N, Yoshikane M, Nakane H, Hashiba T, Yokoyama M, et al. Colonic varices treated by balloon-occluded retrograde transvenous obliteration in a cirrhotic patient with encephalopathy: a case report. Gastrointest Endosc. 2006;63:880–884. doi: 10.1016/j.gie.2005.11.038. [DOI] [PubMed] [Google Scholar]
- 14.Misra SP, Dwivedi M. Ligation of a bleeding colonic varix using an upper gastrointestinal endoscope. Endoscopy. 2006;38:657. doi: 10.1055/s-2006-925189. [DOI] [PubMed] [Google Scholar]
- 15.Chen WC, Hou MC, Lin HC, Chang FY, Lee SD. An endoscopic injection with N-butyl-2-cyanoacrylate used for colonic variceal bleeding: a case report and review of the literature. Am J Gastroenterol. 2000;95:540–542. doi: 10.1111/j.1572-0241.2000.01782.x. [DOI] [PubMed] [Google Scholar]
- 16.Song C, Lee Y, Cho H, Kim D, Choi W, Park H. Massive gastrointestinal hemorrhage from the colonic varices. J Korean Surg Soc. 1993;44:923–928. [Google Scholar]
- 17.Sohn W, Lee HL, Lee KN. Variceal hemorrhage of ascending colon. Clin Gastroenterol Hepatol. 2012;10:A24. doi: 10.1016/j.cgh.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 18.Wiegand N, Pfiffner R, Bauerfeind P. Ascending colonic variceal bleeding. Gastrointest Endosc. 2006;63:1073–104; discussion 1074. doi: 10.1016/j.gie.2005.11.021. [DOI] [PubMed] [Google Scholar]


