Abstract
Background
The Critical Access Hospital (CAH) designation was established to provide rural residents local access to emergency and inpatient care. CAHs, however, have poorer short-term outcomes for pneumonia, heart failure, and myocardial infarction compared to other hospitals. We assessed whether 30-day risk-standardized mortality rates (RSMRs) and readmission rates (RSRRs) after ischemic stroke differ between CAHs and non-CAHs.
Methods
The study included all fee-for-service Medicare beneficiaries ≥65 years old with a primary discharge diagnosis of ischemic stroke (ICD-9 433, 434, 436) in 2006. Hierarchical generalized linear models calculated hospital-level RSMRs and RSRRs, adjusting for patient demographics, medical history, and comorbid conditions. Non-CAHs were categorized by hospital volume quartiles and the RSMR and RSRR posterior probabilities in comparison to CAHs were determined using linear regression with Markov chain Monte Carlo simulation.
Results
There were 10,267 ischemic stroke discharges from 1,165 CAHs and 300,114 discharges from 3,381 non-CAHs. The RSMRs of CAHs were higher than non-CAHs (11.9%±1.4% vs. 10.9%±1.7%, p<0.001), but the RSRRs were comparable (13.7%±0.6% vs. 13.7%±1.4%, p=0.3). The RSMRs for the two higher volume quartiles of non-CAHs were lower than CAHs (posterior probability of RSMRs higher than CAHs=0.007 for quartile 3, probability<0.001 for quartile 4), but there were no differences for lower volume hospitals; RSRRs did not vary by annual hospital volume.
Conclusions
Critical Access Hospitals had higher RSMRs compared with non-CAHs, but readmission rates were similar. The observed differences may be partly explained by patient characteristics and annual hospital volume.
Keywords: ischemic stroke, outcomes, critical access hospital, mortality, readmission
INTRODUCTION
The Critical Access Hospital (CAH) designation was established as part of the Medicare Rural Hospital Flexibility Program in the 1997 Balanced Budget Act to support the financial viability of small rural hospitals and provide rural residents local access to emergency and inpatient care.1 CAHs were defined as being >35 miles from the nearest hospital (>15 miles in mountainous terrain or areas with only secondary roads), having <25 inpatient beds (<15 beds if not a swing bed facility), averaging length of stay of ≤96 hours, and providing 24-hour emergency care services 7 days a week.
The number of CAHs has increased since the program's inception from 41 hospitals in January 1999 to 1327 hospitals as of March 2011. CAH conversion has contributed to the financial viability of many rural hospitals,2-4 and it has had a positive effect on some patient safety2 and quality of care metrics.1 Despite these improvements, CAHs lag behind non-CAHs on many performance measures and have poorer short-term outcomes for pneumonia, heart failure, and myocardial infarction.1, 5 Information about outcomes for stroke patients treated at CAHs is limited. Assessing stroke outcomes is important to ensure optimal quality of care in rural areas, as community awareness of stroke, adherence to evidence-based guidelines for stroke treatment, and deficiencies in specialists, diagnostic technologies, and acute stroke teams may influence care in these settings.6-11 To assess the impact of CAH status on stroke outcomes, we determined 30-day hospital-level risk-standardized mortality rates (RSMRs) and risk-standardized readmission rates (RSRRs) for ischemic stroke discharges from all US hospitals in 2006.
METHODS
Study Sample
The study population included all Medicare fee-for-service (FFS) beneficiaries 65 years of age or older hospitalized with a primary discharge diagnosis of ischemic stroke (International Classification of Diseases, ninth revision, Clinical Modification [ICD-9-CM] codes 433, 434, and 436) from January 1–December 31, 2006. Data were obtained from the Medicare Provider Analysis and Review files and included demographic information, primary and secondary discharge diagnosis codes, and procedure codes for each hospitalization. We included patients with 12 months of continuous Medicare FFS enrollment before and 1 month after the hospitalization to obtain complete medical history, mortality, and readmission information. Patients who were younger than 65 years were not included in the analysis because they do not represent typical Medicare patients. Patients discharged from non-acute care facilities, transferred to or from another acute care facility, discharged within 1 day of admission, or who left the hospital against medical advice were also excluded. Hospitals were classified according to their CAH status in 2006.12
Outcomes
Outcome measures were hospital-level 30-day all-cause RSMR and 30-day all-cause RSRR. Mortality information was obtained from the Medicare Enrollment Database and was assessed from the date of hospital admission. The accuracy of vital status is high for this age group using these data resources.13 Readmissions included those for any cause to an acute care hospital treating Medicare patients within 30 days of discharge. We excluded readmissions to any acute care hospital for procedures that may represent planned continuation of treatment after discharge from the index stroke admission, unless ICD-9-CM 433.x1 or 434.x1 (reflecting an acute stroke) was listed as the principal discharge diagnosis for the hospital readmission. Reasons for planned readmissions were determined a priori and included carotid endarterectomy, carotid stenting, percutaneous carotid or vertebral artery stenting, intracranial stenting, patent foramen ovale closure, cardiac ablation procedures, aortic or mitral valve replacement, and cranioplasty.
Patient and Hospital Characteristics
Pre-existing comorbidities were identified using the primary and nine secondary codes from claims submitted in the year before the index hospitalization and from claims from the index admission for conditions that would not represent an acute stroke complication (e.g., hypertension or diabetes) to adjust for differences in case-mix that would not reflect stroke-related quality of care. Potentially preventable complications of acute stroke (e.g., pneumonia or urinary tract infection) that could reflect quality of care and may impact 30-day mortality or readmissions were excluded from the adjustment. Because there are more than 15,000 ICD-9-CM codes, these codes are grouped into clinically coherent categories using the Hierarchical Condition Categories (HCC), a system developed by physician and statistical consultants under a contract to the Centers for Medicare and Medicaid Services (CMS). A total of 29 independent variables were included from inpatient administrative claims data, including 2 demographic variables (age and sex), 7 cardiovascular and stroke history variables (congestive heart failure, acute myocardial infarction, unstable angina, chronic atherosclerosis, cardiopulmonary-respiratory failure, peripheral vascular disease, cerebrovascular disease), and 20 other variables that identify additional coexisting illnesses (e.g., hypertension, chronic obstructive pulmonary disease, renal failure, liver disease, dementia, cancer). These variables have been used in the calculation of RSMRs and RSRRs for prior studies examining hospital-level outcomes after ischemic stroke.14
Hospital characteristics (hospital bed size, teaching status, geographic region, and urban-rural setting) were obtained from the American Hospital Association's 2006 Annual Survey Database. Geographic region was categorized as 9 regions defined by the United States Census. Non-CAHs were further categorized into quartiles by their total Medicare discharge volume in 2006. The mean Medicare expenditure per stroke hospitalization was calculated for CAHs and non-CAHs.
Statistical Analysis
Patient characteristics and outcomes were compared between CAHs and non-CAHs by using chi-square tests for categorical variables and Wilcoxon rank sum tests for continuous variables and by calculating the standardized difference between the two hospital groups.15,16 Consistent with methods described in the development of administrative models,17-20 a hierarchical generalized linear model (HGLM) that includes patient- and hospital-level data was used to relate the log-odds of 30-day mortality to patient risk factors for the study cohort. The model provided data to compute standardized hospital-specific estimates as well as quantitative summaries of between-hospital variation after adjusting for case mix. An RSMR was calculated for each hospital using the regression coefficients from the HGLM. A linear regression model in conjunction with the Markov chain Monte Carlo (MCMC) simulation method was then used to compare RSMRs of CAHs with non-CAHs at the hospital-level. This model used RSMRs as an outcome with CAHs as the referent category and assessed whether the posterior probability of RSMRs is different between non-CAH volume categories (<25th, 25th-50th, 50th-75th, and >75th percentiles) and CAHs. The posterior probability was estimated based on the proportion of total times that a coefficient of each volume-specific dummy variable was greater than 0 (i.e., higher RSMR than CAH) from 10,000 MCMC simulations. The same analytic methods were used to compare RSRRs between CAHs and non-CAHs. All analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC). Statistical testing was 2-sided at a significance level of α=0.05, with hierarchical models estimated using the GLIMMIX procedure.
RESULTS
There were 310,381 ischemic stroke discharges in 2006: 10,267 from 1,165 CAHs and 300,114 from the 3,381 non-CAHs (Table 1). Patients treated at CAHs were older, more often white, and more frequently had a history of dementia and functional disability. They were less likely to have a history of chronic atherosclerosis, respiratory failure, prior cerebrovascular disease, renal failure, or peripheral vascular disease. CAHs had higher unadjusted in-hospital mortality rates (6.4% vs. 4.6%), a shorter mean length of stay (4.0 vs. 4.6 days), and a higher percentage of patients discharged to skilled nursing or intermediate care facilities (26.9% vs. 20.7%) than non-CAHs. CAHs had a smaller median bed size, treated fewer stroke patients annually and were less likely to be Joint Commission-certified Primary Stroke Centers or teaching hospitals than non-CAHs (Table 2). The differences persisted, although they were less marked, for comparisons between CAHs and low volume non-CAHs. Mean Medicare payments per hospitalization tended to be higher in the higher volume hospitals, but the differences were not substantial (Figure 1).
Table 1.
Comparison of Selected Patient Characteristics by Critical Access Hospital Status
| CAH (N=1165) | Non-CAH (N=3381) | p-value | Standardized Difference* | 95% CI | |
|---|---|---|---|---|---|
| No. patients | 10,267 | 300,114 | |||
| Age, mean years (SD) | 81.6 (7.9) | 78.4 (7.8) | <.0001 | 0.41 | (0.39, 0.43) |
| Female | 59.7 | 54.5 | <.0001 | 0.11 | (0.09, 0.12) |
| White | 93.9 | 85.6 | <.0001 | 0.28 | (0.26, 0.30) |
| Medical history / comorbidity | |||||
| Congestive heart failure | 18.0 | 16.8 | 0.001 | 0.03 | (0.01, 0.05) |
| Myocardial Infarction | 1.5 | 1.4 | 0.4 | 0.01 | (-0.01, 0.03) |
| Chronic atherosclerosis | 20.6 | 30.6 | <.0001 | -0.23 | (-0.25, -0.21) |
| Respiratory failure | 1.7 | 3.8 | <.0001 | -0.13 | (-0.15, -0.11) |
| Hypertension | 60.9 | 65.1 | <.0001 | -0.09 | (-0.11, -0.07) |
| Cerebrovascular disease | 13.9 | 36.8 | <.0001 | -0.55 | (-0.57, -0.53) |
| Renal failure | 7.3 | 11.7 | <.0001 | -0.15 | (-0.17, -0.13) |
| COPD | 12.4 | 15.3 | <.0001 | -0.08 | (-0.10, -0.06) |
| Pneumonia | 7.2 | 6.2 | <.0001 | 0.04 | (0.02, 0.06) |
| Dementia | 16.0 | 11.9 | <.0001 | 0.12 | (0.10, 0.14) |
| Functional disability | 35.6 | 26.9 | <.0001 | 0.19 | (0.17, 0.21) |
| Peripheral vascular disease | 5.2 | 10.9 | <.0001 | -0.21 | (-0.23, -0.19) |
| Depression | 6.3 | 5.0 | <.0001 | 0.06 | (0.04, 0.08) |
| Diabetes | 25.4 | 27.8 | <.0001 | -0.05 | (-0.07, -0.03) |
| In-hospital mortality | 6.4 | 4.6 | <.0001 | 0.08 | (0.06, 0.10) |
| Discharge to skilled nursing facility / intermediate care facility | 26.9 | 20.7 | <.0001 | 0.15 | (0.13, 0.17) |
| Length of stay, mean days (SD) | 4.0 (2.3) | 4.6 (4.6) | <.0001 | -0.16 | (-0.18, -0.15) |
CAH, critical access hospital; CI, confidence interval; COPD, chronic obstructive pulmonary disease
Standardized difference = difference in means or proportions between CAH and non-CAH divided by standard error; a standardized difference of greater than 0.1 denotes a meaningful difference.
Table 2.
Comparison of Hospital Characteristics by Critical Access Hospital Status and Hospital Volume Quartiles*
| CAH | Non-CAH According to Hospital Volume Quartile |
Non-CAH | ||||
|---|---|---|---|---|---|---|
| <25th | 25th-50th | 50th-75th | >75th | Overall | ||
| No. of hospitals | 1165 | 840 | 838 | 838 | 838 | 3380 |
| Total admissions, median (IQR) | 679 (400.5-1045.5) | 2130 (1410-3151) | 4442 (3397-6213) | 8800 (6954-11967) | 17849 (13674.5-25139) | 7225 (3368-13819) |
| Medicare discharges, median (IQR) | ||||||
| Overall | 395 (238.5-596.5) | 977 (644-1327) | 2034 (1564-2627) | 4004 (3173-4895) | 7775.5 (6174-10254) | 3117 (1500-5783) |
| Stroke | 7 (3-12) | 14 (7-22) | 36 (26.5-48) | 82 (62-105) | 180 (138.5-247) | 55 (23-120) |
| Medicaid discharges, median (IQR) | 74 (33-139) | 350 (160-624) | 742 (459-1208) | 1423 (881-2271) | 2536.5 (1613-4110) | 1045 (471-2197) |
| Bed size, median (IQR) | 25 (25-55) | 60 (40-111) | 109 (74-159) | 190 (139-258) | 352.5 (266-504) | 161 (85-285) |
| Nurse-to-patient ratio, median (IQR) | 0.04 (0.03-0.06) | 0.03 (0.02-0.04) | 0.03 (0.03-0.04) | 0.03 (0.03-0.04) | 0.03 (0.03-0.04) | 0.03 (0.03-0.04) |
| JC-certified Primary Stroke Center, % | 22.8 | 65.2 | 86 | 94.3 | 96.8 | 85.6 |
| Ownership, % | ||||||
| Public/municipal | 37.3 | 29.9 | 14.1 | 13.3 | 7.9 | 16.2 |
| Private, not-for-profit | 43.3 | 40.9 | 57.9 | 66.5 | 83.7 | 62.1 |
| Private, for-profit | 2.5 | 20.1 | 23.9 | 18.3 | 8.2 | 17.9 |
| Federal/military | 0.1 | 2.4 | 4.2 | 2.0 | 0.2 | 0.6 |
| Not reported | 16.9 | 6.7 | 0 | 0 | 0 | 3.3 |
| Teaching hospital, % | 3.4 | 12.5 | 14.7 | 29.4 | 53.9 | 27.5 |
Figure 1. Distribution of Mean Medicare Payments per Hospitalization by Critical Access Hospital Status and Hospital Volume Quartiles.
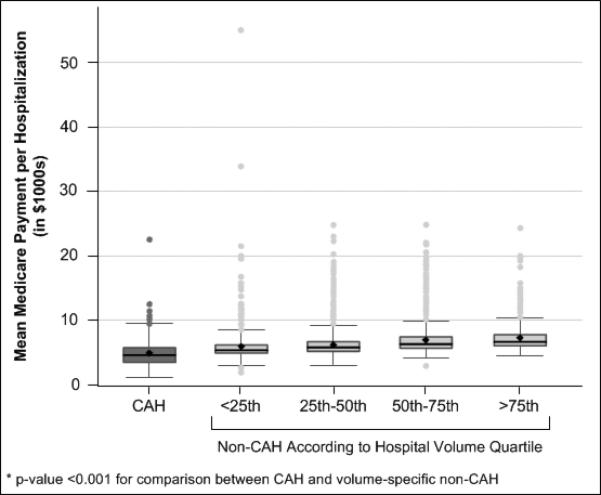
Box and whisker plots of mean Medicare payment per hospitalization in CAH and non-CAH volume categories. The upper boundaries of the boxes represent the seventy-fifth percentile, the lines bisecting the boxes represent the median or fiftieth percentile, and the lower boundaries of the boxes represent the twenty-fifth percentile. The lower and upper boundaries of the whiskers are set at the fifth and ninety-fifth percentiles, with dots representing hospitals beyond these percentiles. Mean (standard deviation) payments for CAHs and non-CAHs in order of increasing quartile are $5,021 (1,956), $6,129 (2,955), $6,691 (2,328), $7,180 (2,231), and $7,425 (1,928). Abbreviations: CAH, Critical Access Hospital.
Patients hospitalized at CAHs had higher 30-day mortality rates than those at non-CAHs (19.9% vs. 10.9%, p<0.001), but lower 30-day all-cause readmission rates (12.4% vs. 13.8%, p<0.001). The hospital-level RSMRs were higher for CAHs than non-CAHs (11.9%±1.4% vs. 10.9%±1.7%, p<0.001), with no difference in 30-day readmissions (13.7%±0.6% vs. 13.7%±1.4%, p=0.3; Figure 2). Compared to CAHs, the RSMRs for non-CAHs decreased with increased hospital volume quartile, but there was no difference for RSRRs (Figures 3 and 4).
Figure 2. Distribution of 30-Day All-Cause Risk-Standardized Mortality Rates and Readmission Rates by Critical Access Hospital (CAH) Status.
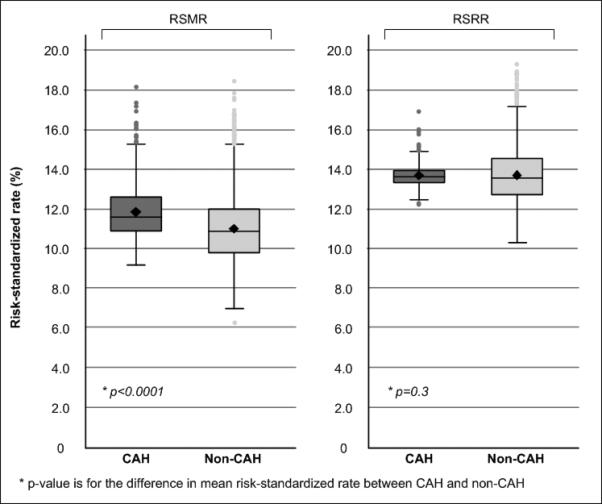
Box and whisker plots of RSMR and RSRR by CAH status. The upper boundaries of the boxes represent the seventy-fifth percentile, the lines bisecting the boxes represent the median or fiftieth percentile, and the lower boundaries of the boxes represent the twenty-fifth percentile. The lower and upper boundaries of the whiskers are set at the fifth and ninety-fifth percentiles, with dots representing hospitals beyond these percentiles. Abbreviations: RSMR, risk-standardized mortality rate; RSRR, risk-standardized readmission rate; CAH, Critical Access Hospital.
Figure 3. Distribution of 30-Day All-Cause Risk-Standardized Mortality Rates and Readmission Rates by Critical Access Hospital Status and Hospital Volume Quartiles.
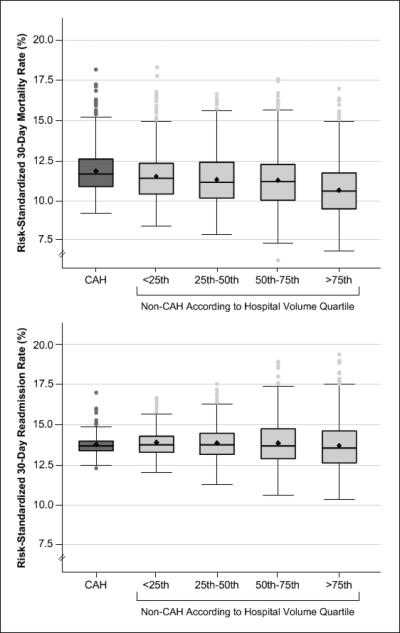
Box and whisker plots of RSMR and RSRR by CAH and non-CAH status. The upper boundaries of the boxes represent the seventy-fifth percentile, the lines bisecting the boxes represent the median or fiftieth percentile, and the lower boundaries of the boxes represent the twenty-fifth percentile. The lower and upper boundaries of the whiskers are set at the fifth and ninety-fifth percentiles, with dots representing hospitals beyond these percentiles. Mean (standard deviation [SD]) RSMR values for CAHs and non-CAHs in order of increasing quartile are 11.9 (1.4), 11.5 (1.5), 11.3 (1.7), 11.2 (1.7), and 10.6 (1.6). Mean (SD) RSRR values are 13.7 (0.6), 13.8 (0.8), 13.8 (1.0), 13.8 (1.4), and 13.7 (1.6). Abbreviations: RSMR, risk-standardized mortality rate; RSRR, risk-standardized readmission rate; CAH, Critical Access Hospital.
Figure 4. Comparison of Risk-Standardized 30-Day All-Cause Mortality Rates and Readmission Rates Between Volume Quartiles of Non-Critical Access Hospitals (CAHs) and CAHs.
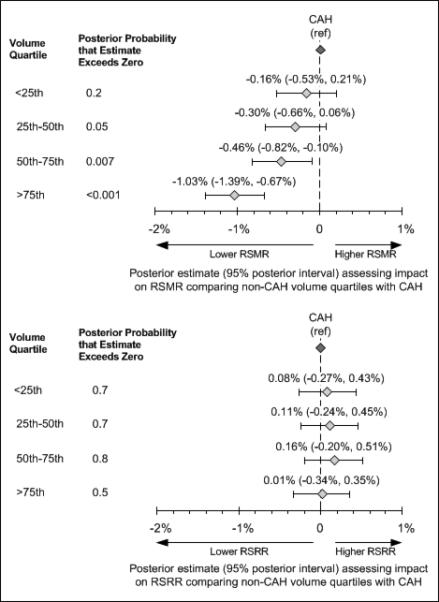
Forest plot displays the posterior estimate for the comparison of RSMR/RSRR between volume quartiles of non-CAHs and all CAHs along with 95% posterior intervals. For example, the estimate of -1.03% comparing the 4th (>75th) quartile of non-CAH to CAH translated to approximately a 1% reduction in RSMR in non-CAHs in the highest quartile of case volume relative to CAHs. Posterior probabilities on the left indicate the probability that the estimate is greater than zero. Abbreviations: RSMR, risk-standardized mortality rate; RSRR, risk-standardized
DISCUSSION
Overall, CAHs had higher mean 30-day RSMRs compared with non-CAHs, but there was no difference in 30-day RSRRs. Higher volume non-CAHs had lower RSMRs than CAHs, but low volume non-CAHs had RSMRs that were similar to CAHs. There was no difference for RSRRs by CAH status or hospital volume quartile.
The Rural Hospital Flexibility Program Tracking Team found that CAHs are involved in a range of quality-related activities (e.g., continuing education, error reporting policies, error prevention, data collection), and that their involvement in these programs remained stable or strengthened after receiving CAH designation.2, 21, 22 Factors thought to enhance quality of care in CAHs include increased staffing, networking with larger acute care hospitals, improvements in case management and discharge planning, and revision of patient safety processes.2, 21, 22 Despite these improvements, CAHs continue to lag behind non-CAHs in resources, clinical capabilities, provision of care consistent with quality metrics, and outcomes.1, 5 Studies comparing CAHs to non-CAHs find higher short-term mortality for several conditions.1, 5 We extend these analyses by showing higher short-term mortality for ischemic stroke at CAHs, but no difference in RSRRs by CAH status. We also noted heterogeneity in RSMRs by hospital volume, with CAHs having RSMRs comparable to non-CAH hospitals of similar size.
Data comparing readmission rates for CAHs and non-CAHs are limited. A prior study using Medicare data from rural and urban hospitals in Iowa, Maine, North Dakota, Oregon, and Utah found that unadjusted readmission rates for rural hospitals were higher than for urban hospitals; however, these differences were attenuated after adjusting for patient age. 23 The rates were higher for urban hospitals compared to rural hospitals after adjustment for disease severity. We found no differences in 30-day readmission rates in risk-standardized hospital-level comparisons.
Several factors may contribute to higher mortality rates for stroke patients treated at CAHs. By definition, CAHs serve rural populations with limited access to emergency care. Given their rural locales, patients cared for at CAHs likely live at greater distances from any hospital, including larger hospitals with more specialized services. With potentially longer travel times, rural patients may arrive at CAHs in worse condition.24, 25 The relative lack of available and readily mobilized Emergency Medical Services may also contribute to longer presentation and transport delays.24, 25 The economic and geographic constraints of CAHs themselves may contribute to acute-care treatment delays.25, 26 We also found that mean payments to CAHs for stroke patients were lower for CAHs than for non-CAHs, especially in comparison to larger volume hospitals, although the differences were small.
Patients treated at CAHs differ systematically from those treated at non-CAHs. Rural residents tend to be older, uninsured, and have more limited access to primary care services.24, 27, 28,29, 30 They also tend to have a higher prevalence of stroke risk factors, yet have less knowledge regarding the warning signs and risk factors for stroke. CAHs often serve as triage centers for stroke patients and transfer patterns may reflect patient characteristics. For example, one study found patients with acute myocardial infarction who remained in community hospitals were older and sicker than those transferring to other facilities.31 Several studies report that rural patients who are younger are more likely to be transferred to urban hospitals than older patients.32-38 Patients may also prefer to be treated at local CAHs and refuse transfer to distant larger, better-equipped and staffed medical centers.29, 30
Higher case volume is generally associated with better care and outcomes.39-41 The low volume of stroke cases treated at CAHs may not be sufficient for the staff to maintain adequate clinical skills. Rural hospitals have limited availability of specialty caregivers, diagnostic technologies, and acute stroke care teams.6-10 Rural-urban gaps have also been noted in adherence to evidence-based guidelines for stroke treatment,6, 11 although compliance with secondary stroke preventive therapies is similar.13 We found that there was no difference in stroke mortality between CAHs and similarly sized non-CAHs, suggesting that lower volume rather than CAH status per se may explain much of the difference.
Our study has limitations. Although the positive predictive values for the selected ischemic stroke ICD-9-CM codes are relatively high, the index ischemic stroke cases were not verified by record review.42, 43 Although we were able to adjust for differences in case mix based on comorbid conditions, Medicare inpatient data do not contain information on stroke severity, which can be an important predictor of outcomes.44 Data were not available to assess stroke process of care measures, but a prior study found that CAHs had lower performance on these types of measures for other conditions including AMI, CHF, and pneumonia, even after adjusting for case mix and other hospital characteristics.5 The study lacked data on the experience of caregivers treating stroke patients, decision making about the receipt of care, time from symptom onset to hospital presentation, and other aspects of outpatient care that my affect outcomes. Although Medicare FFS beneficiaries age 65 years and older represent the majority of ischemic stroke events, the results may not be applicable to those without FFS Medicare coverage or to stroke patients younger than age 65 years. We analyzed outcomes for a single year and did not assess whether patterns have changed since the inception of the CAH program. Finally, our study examined short-term mortality and readmissions and did not consider other important dimensions of patient outcomes such as functional status or quality of life.
Because at least a portion of the difference in stroke mortality rates between CAHs and non-CAHs may be explained by lower volume, procedures such as the adoption of standardized care maps and conduct of “mock stroke codes” may be helpful. The provision of telemedicine services to rural hospitals also extends stroke care expertise to underserved facilities. Additional work is needed to determine the effectiveness of these types of interventions.6
Acknowledgments
Sources of Funding
The Centers for Medicare & Medicaid Services reviewed and approved the use of its data for this work; this approval is based on data use only and does not represent a Centers for Medicare & Medicaid Services endorsement of or comment on the manuscript content. The project described was supported by Grant Number R01NS043322 from the National Institute of Neurological Disorders and Stroke. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health.
Footnotes
Disclosures
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Casey M, Burlew M, Moscovice I. Critical Access Hospital Year 6 Hospital Compare Participation and Quality Measure Results:. Flex Monitoring Team briefing paper No. 28. Rural Health Research Center; Minneapolis, MN: 2011. [October 1, 2011]. Available at: www.flexmonitoring.org. [Google Scholar]
- 2.Li P, Schneider JE, Ward MM. Effect of critical access hospital conversion on patient safety. Health Serv Res. 2007;42:2089–2108. doi: 10.1111/j.1475-6773.2007.00731.x. discussion 2294-2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cameron A, Zelman B, Stewart S. Financial Condition of Critical Access Hospitals: 1996-1999. In: Rural Hospital Flexibility Program Tracking Team, editor. Rural Hospital Flexibility Program Tracking Project Year One Report. WWAMI Rural Health Research Center, University of Washington; Seattle, WA: 2001. [December 1, 2011]. Available at: http://www.rupri.org/. [Google Scholar]
- 4.Stensland J, Davidson G, Moscovice I. The Financial Benefits of Critical Access Hospital Conversion for FY 1999 and FY 2000 Converters. [December 1, 2011];2001 Available at: http://www.sph.umn.edu/hpm/rhrc/pdfs/wpaper/wpaper051.pdf.
- 5.Joynt KE, Harris Y, Orav EJ, Jha AK. Quality of care and patient outcomes in critical access rural hospitals. JAMA. 2011;306:45–52. doi: 10.1001/jama.2011.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okon NJ, Fogle CC, McNamara MJ, Oser CS, Dietrich DW, Gohdes D, et al. Statewide efforts to narrow the rural-urban gap in acute stroke care. Am J Prev Med. 2010;39:329–333. doi: 10.1016/j.amepre.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 7.Camilo O, Goldstein LB. Statewide assessment of hospital-based stroke prevention and treatment services in North Carolina: Changes over the last 5 years. Stroke. 2003;34:2945–2950. doi: 10.1161/01.STR.0000103137.44496.AD. [DOI] [PubMed] [Google Scholar]
- 8.Gropen T, Magdon-Ismail Z, Day D, Melluzzo S, Schwamm LH. Regional implementation of the stroke systems of care model: Recommendations of the Northeast Cerebrovascular Consortium. Stroke. 2009;40:1793–1802. doi: 10.1161/STROKEAHA.108.531053. [DOI] [PubMed] [Google Scholar]
- 9.Leira EC, Hess DC, Torner JC, Adams HP., Jr. Rural-urban differences in acute stroke management practices: A modifiable disparity. Arch Neurol. 2008;65:887–891. doi: 10.1001/archneur.65.7.887. [DOI] [PubMed] [Google Scholar]
- 10.Ruland S, Gorelick PB, Schneck M, Kim D, Moore CG, Leurgans S. Acute stroke care in Illinois: A statewide assessment of diagnostic and treatment capabilities. Stroke. 2002;33:1334–1339. doi: 10.1161/01.str.0000014609.44258.ad. [DOI] [PubMed] [Google Scholar]
- 11.Burgin WS, Staub L, Chan W, Wein TH, Felberg RA, Grotta JC, et al. Acute stroke care in non-urban emergency departments. Neurology. 2001;57:2006–2012. doi: 10.1212/wnl.57.11.2006. [DOI] [PubMed] [Google Scholar]
- 12.Flex Monitoring Team CAH Information. [July 1, 2012]; Available at: www.flexmonitoring.org/cahlistRA.cgi.
- 13.Rodriguez D, Cox M, Zimmer LO, Olson DM, Goldstein LB, Drew L, et al. Similar secondary stroke prevention and medication persistence rates among rural and urban patients. J Rural Health. 2011;27:401–408. doi: 10.1111/j.1748-0361.2010.00352.x. [DOI] [PubMed] [Google Scholar]
- 14.Lichtman JH, Jones SB, Wang Y, Watanabe E, Leifheit-Limson E, Goldstein LB. Outcomes after ischemic stroke for hospitals with and without Joint Commission-certified primary stroke centers. Neurology. 2011;76:1976–1982. doi: 10.1212/WNL.0b013e31821e54f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mamdani M, Sykora K, Li P, Normand SL, Streiner DL, Austin PC, et al. Reader's guide to critical appraisal of cohort studies: 2. Assessing potential for confounding. BMJ. 2005;330:960–962. doi: 10.1136/bmj.330.7497.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Academic Press; Hillsdale, NJ: 1988. [Google Scholar]
- 17.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp MT, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keenan PS, Normand S-LT, Lin Z, Drye EE, Bhat KR, Ross JS, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 19.Krumholz HM, Wang Y, Mattera JA, Wang Y, Han LF, Ingber MJ, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 20.Krumholz HM, Wang Y, Mattera JA, Wang Y, Han LF, Ingber MJ, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113:1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 21.Moscovice I, Gregg W. CAH Quality Assurance (QA) and Quality Improvement (QI) Strategies. In: Rural Hospital Flexibility Program Tracking Team, editor. Rural Hospital Flexibility Program Tracking Project Year Two Report. WWAMI Rural Health Research Center, University of Washington; Seattle, WA: 2001. [December 1, 2011]. Available at: http://www.rupri.org/. [Google Scholar]
- 22.Moscovice I, Gregg W. The Maturation of CAH Quality Assurance (QA) and Quality Improvement (QI) Strategies. In: Rural Hospital Flexibility Program Tracking Team, editor. Rural Hospital Flexibility Program Tracking Project Year Three Report. WWAMI Rural Health Research Center, University of Washington; Seattle, WA: 2002. [December 1, 2011]. Available at: http://www.rupri.org/ [Google Scholar]
- 23.Klug MG, Muus K, Casey M, Moscovice I. Upper Midwest Rural Health Research Center; Aug, 2009. [October 1, 2011]. Policy brief: Potentially preventable readmissions in rural hospitals. Available at: www.uppermidwestrhrc.org. [Google Scholar]
- 24.Callison RC, Leira EC. Strategies to improve acute stroke care of patients in rural and other geographically dispersed areas. Curr Treat Options Neurol. 2008;10:450–454. doi: 10.1007/s11940-008-0047-4. [DOI] [PubMed] [Google Scholar]
- 25.Gebhardt JG, Norris TE. Acute stroke care at rural hospitals in Idaho: challenges in expediting stroke care. J Rural Health. 2006;22:88–91. doi: 10.1111/j.1748-0361.2006.00004.x. [DOI] [PubMed] [Google Scholar]
- 26.Zweifler RM, Mendizabal JE, Cunningham S, Shah AK, Rothrock JF. Hospital presentation after stroke in a community sample: The Mobile stroke project. South Med J. 2002;95:1263–1268. [PubMed] [Google Scholar]
- 27.Eberhardt MS, Pamuk ER. The importance of place of residence: Examining health in rural and nonrural areas. Am J Public Health. 2004;94:1682–1686. doi: 10.2105/ajph.94.10.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pearson TA, Lewis C. Rural epidemiology: Insights from a rural population laboratory. Am J Epidemiol. 1998;148:949–957. doi: 10.1093/oxfordjournals.aje.a009571. [DOI] [PubMed] [Google Scholar]
- 29.Lipsky MS, Glasser M. Critical access hospitals and the challenges to quality care. JAMA. 2011;306:96–97. doi: 10.1001/jama.2011.928. [DOI] [PubMed] [Google Scholar]
- 30.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94:1675–1678. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehta RH, Stalhandske EJ, McCargar PA, Ruane TJ, Eagle KA. Elderly patients at highest risk with acute myocardial infarction are more frequently transferred from community hospitals to tertiary centers: Reality or myth? Am Heart J. 1999;138:688–695. doi: 10.1016/s0002-8703(99)70184-5. [DOI] [PubMed] [Google Scholar]
- 32.Hall MJ, Marsteller J, Owings M. Factors influencing rural residents’ utilization of urban hospitals. Natl Health Stat Report. 2010:1–12. [PubMed] [Google Scholar]
- 33.Buczko W. What affects rural beneficiaries use of urban and rural hospitals? Health Care Financ Rev. 1992;14:107–114. [PMC free article] [PubMed] [Google Scholar]
- 34.Tai WTC, Porell FW, Adams EK. Hospital choice of rural medicare beneficiaries: Patient, hospital attributes, and the patient-physician relationship. Health Serv Res. 2004;39:1903–1922. doi: 10.1111/j.1475-6773.2004.00324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adams EK, Houchens R, Wright GE, Robbins J. Predicting hospital choice for rural medicare beneficiaries: The role of severity of illness. Health Serv Res. 1991;26:583–612. [PMC free article] [PubMed] [Google Scholar]
- 36.Porell FW, Adams EK. Hospital choice models: A review and assessment of their utility for policy impact analysis. Med Care Res Rev. 1995;52:158–195. doi: 10.1177/107755879505200202. [DOI] [PubMed] [Google Scholar]
- 37.Hogan C. Patterns of travel for rural individuals hospitalized in New York State: Relationships between distance, destination, and case mix. J Rural Health. 1988;4:29–41. doi: 10.1111/j.1748-0361.1988.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 38.Basu J, Cooper J. Out-of-area travel from rural and urban counties: A study of ambulatory care sensitive hospitalizations for New York state residents. J Rural Health. 2000;16:129–138. doi: 10.1111/j.1748-0361.2000.tb00446.x. [DOI] [PubMed] [Google Scholar]
- 39.Bateman BT, Schumacher HC, Boden-Albala B, Berman MF, Mohr JP, Sacco RL, et al. Factors associated with in-hospital mortality after administration of thrombolysis in acute ischemic stroke patients: an analysis of the nationwide inpatient sample 1999 to 2002. Stroke. 2006;37:440–446. doi: 10.1161/01.STR.0000199851.24668.f1. [DOI] [PubMed] [Google Scholar]
- 40.Heuschmann PU, Kolominsky-Rabas PL, Misselwitz B, Hermanek P, Leffmann C, Janzen RW, et al. Predictors of in-hospital mortality and attributable risks of death after ischemic stroke: the German Stroke Registers Study Group. Arch Intern Med. 2004;164:1761–1768. doi: 10.1001/archinte.164.16.1761. [DOI] [PubMed] [Google Scholar]
- 41.Saposnik G, Baibergenova A, O'Donnell M, Hill MD, Kapral MK, Hachinski V. Hospital volume and stroke outcome: does it matter? Neurology. 2007;69:1142–1151. doi: 10.1212/01.wnl.0000268485.93349.58. [DOI] [PubMed] [Google Scholar]
- 42.Goldstein LB. Accuracy of ICD-9-CM coding for the identification of patients with acute ischemic stroke : Effect of modifier codes. Stroke. 1998;29:1602–1604. doi: 10.1161/01.str.29.8.1602. [DOI] [PubMed] [Google Scholar]
- 43.Tirschwell DL, Longstreth WT. Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 44.Saposnik G, Hill MD, O'Donnell M, Fang J, Hachinski V, Kapral MK. Variables associated with 7-day, 30-day, and 1-year fatality after ischemic stroke. Stroke. 2008;39:2318–2324. doi: 10.1161/STROKEAHA.107.510362. [DOI] [PubMed] [Google Scholar]


