Poor health amongst commercial truck drivers is a dangerous and costly public health problem. The high rate of obesity in truckers increases their risk for heart disease, stroke, type 2 diabetes and some types of cancer1. Driver health problems, especially obesity and related conditions like sleep apnea, are related to driving errors and increased crash rates,2-4 impacting both driver safety and the safety of the general public. While truck drivers have less than half the crash rate per vehicle mile compared to passenger car drivers,5 large truck crashes are deadly. In 2010 there were 3,413 fatalities in large truck crashes, and 85% of those fatalities were passenger car occupants, pedestrians, or cyclists.6 Annual healthcare costs for overweight and obese drivers are also over $200 higher compared to normal weight drivers.7 Furthermore, the costs to society per fatal large truck crash averaged $7.74 million during 2009 (in 2012 dollars).6,8 While obesity in trucking is a multi-level public health problem involving workers, supervisors, company policies, federal regulations, and built environments,9 effective weight-loss interventions are essential if we are to produce meaningful health and economic improvements for both drivers and society.
The SHIFT intervention is a 6-month weight loss and health promotion program for truck drivers that combines the evidence-based tactics of competition, computer-based training, behavioral self-monitoring, and motivational interviewing. Outcomes of the SHIFT pilot study (n = 29)10 suggest that the SHIFT program is more effective than previous weight loss interventions for truck drivers, including superior engagement, knowledge gains, behavior change, and objectively measured weight loss.11-13 Over a 6-month period pilot participants made significant reductions in the consumption of high calorie foods and drinks, and lost an average of 7.8lbs in objectively measured body weight (roughly 1 BMI unit). Drivers completed an average of 3.9 of 4 possible motivational interviewing sessions, and those who completed computer-based training showed large knowledge gains (d = 2.69).14 Overall, pilot study results showed that the SHIFT intervention was effective for improving body weight and health during a 6-month time period.
Maintenance of initial weight-loss is essential for participants to realize the long-term benefits of a healthier body weight. Data on weight-loss maintenance following worksite interventions are generally lacking,15 but in available studies, participants in worksite weight-loss competitions maintained only 27% of initial weight-loss during the first year post-intervention.16 This level of maintenance is consistent with findings from a meta-analysis of weight-loss interventions in general.15 Given the likelihood of weight regain among participants in weight loss interventions, we set out to conduct a low-cost investigation of weight loss maintenance among participants in the original SHIFT pilot study. Post-intervention support for weight-loss maintenance can prevent weight regain.18-20 Therefore, in addition to evaluating the level of maintenance among pilot participants, we hoped that follow-up data might inform future plans for maintenance support in the SHIFT program, which is currently being evaluated with a randomized controlled trial (NHLBI 1R01HL105495).
All 29 drivers who completed baseline enrollment in the SHIFT pilot study were eligible to participate in the follow-up study. Of those 29 pilot study participants, 15 completed a follow-up phone interview. Three drivers from the pilot study declined participation in the follow-up, and the remaining 11 pilot study participants were not successfully contacted by phone. Most follow-up participants (12 of 15) were still working as truck drivers, although 8 reported reduced driving hours or breaks of two or more months in driving since the end of the SHIFT pilot study. Follow-up participants included one driver who did not complete a post-intervention assessment in the original study, and one who completed the phone interview but did not provide a recent body weight.
The SHIFT pilot study did not include a maintenance phase and participants received no contact from SHIFT during the 30-month period between the post-intervention assessment and follow-up. Verbal consent was obtained over the phone following a description of procedures, and participants received a $20 gift card in the mail after completing a phone interview. Interviews were designed to last 20 minutes and followed a script that was developed and rehearsed through role-play. Participants were also asked to complete and return a paper survey via postal mail.
Self-reported body weight was the primary outcome measure. Participants were also asked to report their current dietary behaviors (daily servings of fruits and vegetables and frequencies of fast food, sugary drinks, and sugary snacks), and exercise levels (days per week of 30+ minutes of exercise). If participants did not know their current body weight during the phone interview, they were asked to obtain a weight measurement and report their results by phone or text message. The paper survey was from the pilot study, and included standardized scales that were analogous to behavioral measures in the phone interview with the exception of exercise (see Olson, et al.10 for a full description).
Descriptive statistics were calculated for all variables collected in phone interviews. For participants who returned the paper survey (n = 8), data from phone interview and surveys were averaged for each variable prior to analyses. The primary analyses were within group repeated measures ANOVAs with pairwise comparisons between pre-intervention (t1), post-intervention (t2), and 30-month follow-up (t3). Effect sizes and percent change statistics were also calculated for each measure.
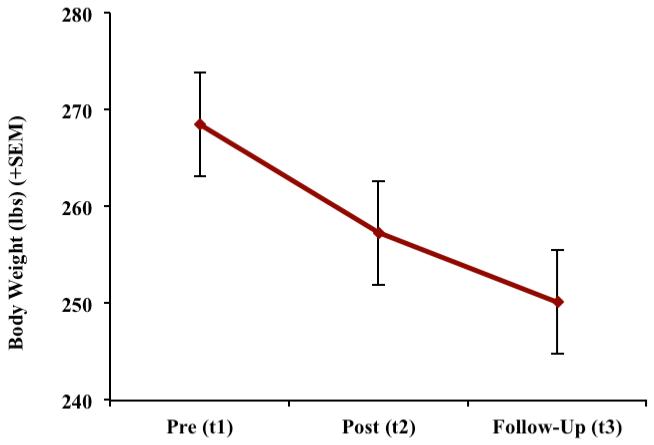
Average body weight at t3 was 250.1lbs (SD = 39.5), and average BMI was 36.3 (SD = 5.1). Participants reported eating 3.0 servings of fruits and vegetables per day (SD = 1.7), and consuming 1.1 fast food meals (SD = 0.9), 3.6 sugary drinks (SD = 5.4), and 1.3 (SD = 1.3) sugary snacks per week. The repeated measures ANOVA for body weight was significant (p < .001), and pairwise contrasts revealed significant differences between t1 and t2, and between t1and t3 time points. Contrasts for the follow-up period (t2-t3) showed moderate effect sizes for weight loss in pounds (d = 0.51) and BMI (d = 0.56) that approached significance (p =.09 and .06, respectively). The average total change in body weight from t1 to t3 was −18.4lbs (SD = 15.9, d = 1.15; see Table 1 and Figure 1). Three drivers reported gaining weight between t1 and t3 (1-7lbs), one maintained, and 9 lost additional weight (3-47lbs). The three participants who gained weight reported experiencing injuries that required time away from work in the time between measurements. The repeated measures ANOVA for BMI was also significant (p < .001), and the average change in BMI between t1 and t3 was −2.7 units (SD = 2.5, d = 1.16). Sugary drink servings per week decreased from 9.6 (SD = 10.4) at t1 to 3.6 (SD = 5.4) at t3 (p < .05). Repeated measures ANOVAs for fruit and vegetable consumption, fast food frequency, and sugary snack frequency were non-significant, with all three variables trending towards improvement or remaining stable between measurements. Exercise contrasts were problematic because we opted not to conduct the same 7-day physical activity recall interview that was conducted in the pilot study, which produces an exercise metric of kcals per kilogram per week. However, from a descriptive standpoint, participants reported an average of 1.5 days per week (SD = 1.8) with 30 minutes or more of exercise in the past month.
Table 1.
Changes in Body Weight, BMI, and Dietary Behaviors over 36 Months
| Measure | t1-t2Δ (SD) | p * | Δ d | t2-t3Δ (SD) | P | Δ d | t1-t3A (SD) | P | Δ d |
|---|---|---|---|---|---|---|---|---|---|
| Body Weight (lbs) |
−11.2(11.6)** | .005 | 0.97 | −7.2 (14.1) | .09 | 0.51 | −18. (15.9) | .001 | 1.15 |
| BMI | −1.6(1.6) | .004 | 1.00 | −1.2 (2.2) | .06 | 0.56 | −2.7 (2.5) | .001 | 1.16 |
| Fruits & Vegetables† |
−0.4 (1.0) | .17 | 0.39 | .3 (1.3) | .41 | 0.23 | −0.1 (1.7) | .82 | 0.06 |
| Sugary Drinks†† |
−5.3 (8.8) | .04 | .61 | −0.8 (9.4) | .77 | .08 | −6.1 (9.9) | .04 | .61 |
| Sugary Snacks†† |
−0.1 (4.0) | .92 | .03 | −0.1 (3.4) | .95 | .01 | −0.2 (2.1) | .78 | .08 |
| Fast Food†† | −1.5 (3.6) | .16 | 0.40 | 0.5 (1.0) | .09 | 0.49 | −1.0 (3.6) | .32 | 0.28 |
Note: p values are from pairwise comparisons between the respective measurements.
average weight loss t1-t2 is greater than the original pilot study results due to the smaller sample of participants who agreed to participate in the follow-up study.
Δ = change.
= servings per day.
= servings per week.
Figure 1.
Participant Body Weight: Pre-Intervention to Follow-Up
The results of the 30-month follow-up study of SHIFT pilot participants should be viewed as encouraging. On average, follow-up participants reported losing additional weight in the absence of any formal maintenance program. If the self-reported weight loss during the follow-up period was accurate, it is not clear what behaviors were most responsible for this favorable result. While there were significant reductions in high-sugar and high fat food consumption in the original pilot study, no significant changes in these behaviors were reported during the follow-up period, and drivers also reported low levels of exercise (only one participant reported 4 or more days/week with 30+ minutes of exercise). However, it may be that drivers maintained original reductions in high-fat and high sugar foods, or that they made changes to unmeasured behaviors. For example, we did not measure changes in portion sizes or general physical activity levels. Anecdotally, during phone interviews several drivers reported eating smaller portion sizes since completing the SHIFT pilot study. For drivers who reported working fewer hours or having gaps in employment, increases in standing time and general physical activity could have contributed to continued weight loss.
Limitations of the current study warrant a degree of skepticism. First, self-reported body weights at the follow-up time point are more likely to be inaccurate than objectively measured body weights collected during the pilot study. However, prior research shows that self-reported body weight is, on average, accurate to within 1-3lbs of actual body weight.21 In addition, attrition (t1 n = 29; t2 n = 22; t3 n = 15) may have resulted in a follow-up sample that was biased toward people who were more successful at losing weight during all time periods. This potential for differential attrition bias at follow-up is supported by the fact that follow-up participants had better initial weight loss results than pilot participants in general (M = −11.2lbs and −7.8lbs, respectively)
Maintenance of initial weight-loss is critical to assessing the long-term potential health impacts of weight-loss interventions. The maintenance period was important to evaluate among SHIFT participants because of the novel combination of intervention components and the difficulty for participants to simulate or continue these components outside of a structured program. Successful weight-loss maintenance has been defined as “losing at least 10% of initial body weight and maintaining the loss for at least 1 year.”22 In the original pilot study only one participant lost 10% or greater of their body weight, and in the follow-up study, three participants met or exceeded the Wing and Hill criterion for successful maintenance.22 However, total weight loss among follow-up participants averaged 18.4 pounds over a 36-month period (6.8% of original body weight), and moderate, sustained weight loss such as this among obese individuals provides clinically significant effects such as normalized blood pressure and reduced cardiovascular risk factors.23-25 These findings should be viewed as good news for the trucking industry, which generally lacks evidence-based methods for helping truck drivers lose and manage body weight.
Acknowledgments
Funding: This project was supported by grant #R01 HL105495 from the National Heart, Lung, and Blood Institute, and by the Center for Research on Occupational and Environmental Toxicology Summer Internship Program at Oregon Health & Science University.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control [Accessed July 2012];Obesity FAQs. 2006 Available at: http://www.cdc.gov/nccdphp/dnpa/obesity/index.htm.
- 2.Cantor DE, Corsi TM, Grimm CM, Özpolat K. A driver focused truck crash prediction model. Transp Res Part E: Logist Transp Rev. 2010;46:683–692. [Google Scholar]
- 3.Stoohs RA, Guilleminault C, Itoi A, Dement WC. Traffic accidents in commercial long haul truck drivers: the influence of sleep disordered breathing and obesity. Sleep. 1994;17:619–623. [PubMed] [Google Scholar]
- 4.Wiegand DM, Hanowski RJ, McDonald SE. Commercial drivers’ health: a naturalistic study of body mass index, fatigue, and involvement in safety-critical events. Traffic Inj Prev. 2009;10:573–579. doi: 10.1080/15389580903295277. [DOI] [PubMed] [Google Scholar]
- 5.Federal Motor Carrier Safety Administration . Large Truck Crash Facts 2002. FMCSA; Washington, DC: 2004. Publication No.FMCSA-RI-04-021. [Google Scholar]
- 6.Insurance Institute for Highway Safety [Accessed July 2012];Fatality facts 2010: Large trucks. Available at: http://www.iihs.org/research/fatality.aspx?topicName=Largetrucks&year=2010.
- 7.Martin BC. The impact of overweight and obesity on the direct medical costs of truck drivers. J Occup Environ Med. 2009;51:180–184. doi: 10.1097/JOM.0b013e3181965d6e. [DOI] [PubMed] [Google Scholar]
- 8.Federal Motor Carrier Safety Administration . Large Truck and Bus Crash Facts 2009: Final Version. FMCSA; Washington, DC: 2011. Publication No. FMCSA-RRA-11-025. [Google Scholar]
- 9.Orleans TC. Promoting the maintenance of health behavior change: recommendations for the next generation of research and practice. Health Psychol. 2000;19(Suppl.):76–83. doi: 10.1037/0278-6133.19.suppl1.76. [DOI] [PubMed] [Google Scholar]
- 10.Olson R, Anger WK, Elliot DL, Wipfli B, Gray M. A new health promotion model for lone workers: results of the Safety & Health Involvement For Truckers (SHIFT) pilot study. J Occup Environ Med. 2009;51:1233–1246. doi: 10.1097/JOM.0b013e3181c1dc7a. [DOI] [PubMed] [Google Scholar]
- 11.Roberts S, York J. Technical Memorandum Number Three: Pilot Test Results and Marketing Plan. Federal Motor Carrier Safety Administration; Washington, DC: 1999. [Google Scholar]
- 12.Holmes SM, Power ML, Walter CK. A motor carrier wellness program: Development and testing. Transp J. 1996;35:33–48. [Google Scholar]
- 13.Sorensen G, Stoddard A, Quintilani L, et al. Tobacco use cessation and weight management among motor freight workers: results of the gear up for health study. Cancer Causes Control. 2010;21:2113–2122. doi: 10.1007/s10552-010-9630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Academic Press; New York: 1969. [Google Scholar]
- 15.Benedict MA, Arterburn D. Worksite-Based weight loss programs: a systematic review of recent literature. Am J Health Promot. 2008;22:408–416. doi: 10.4278/ajhp.22.6.408. [DOI] [PubMed] [Google Scholar]
- 16.Stunkard A, Cohen R. Felix M. Weight loss competitions at the worksite: how they work and how well. Prev Med. 1989;18:460–474. doi: 10.1016/0091-7435(89)90006-6. [DOI] [PubMed] [Google Scholar]
- 17.Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes. 2005;29:1168–1174. doi: 10.1038/sj.ijo.0803015. [DOI] [PubMed] [Google Scholar]
- 18.Abrams DB, Follick MJ. Behavioral weight-loss intervention at the worksite: feasibility and maintenance. J Consult Clin Psychol. 1983;51:226–233. doi: 10.1037//0022-006x.51.2.226. [DOI] [PubMed] [Google Scholar]
- 19.Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obes Rev. 2012;13:509–517. doi: 10.1111/j.1467-789X.2011.00972.x. [DOI] [PubMed] [Google Scholar]
- 20.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. J Am Med Assoc. 2008;299:1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 21.Rowland ML. Self-reported weight and height. Am J Clin Nutr. 1990;52:1125–1133. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 22.Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–341. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- 23.Goldstein DJ. Beneficial health effects of modest weight loss. Int J Obes. 1992;16:397–415. [PubMed] [Google Scholar]
- 24.Mertens IL, Van Gaal LF. Overweight, obesity, and blood pressure: the effects of modest weight reduction. Obes Res. 2000;8:270–278. doi: 10.1038/oby.2000.32. [DOI] [PubMed] [Google Scholar]
- 25.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]