Abstract
Cystic lesions can be occasionally be found in the mediastinum, and typically include bronchogenic cysts, esophageal duplication cysts, and neuroenteric cysts. In 2005, Hattori described the first mediastinal cyst with Mullerian differentiation. Since that time, three other authors have described similar cysts occurring in the posterior mediastinum. Here we present two cases of patients with ciliated cysts with Mullerian differentiation with expression of estrogen receptor, progesterone receptor, PAX8 and Wilm’s tumor 1, occurring in the posterior mediastinum and review the related literature.
KEY WORDS : Mediastinal, mullerian cyst, estrogen receptor
Introduction
Primary congenital mediastinal cysts are relatively rare, accounting for approximately 12-30% of all mediastinal masses (1). The most common cyst is the bronchogenic/foregut cyst, which accounts for approximately half of these cystic lesions and typically occurs in the middle and posterior mediastinum. Recent case reports (2-6) have shown that several of these presumed foregut cysts exhibit Mullerian differentiation. Here we present two cases of posterior mediastinal ciliated cysts with Mullerian differentiation. In each case, the diagnosis was confirmed with immunostains for estrogen receptor, progesterone receptor, PAX8 and Wilm’s tumor 1. We also review the literature on Mullerian cysts and possible pathogenesis.
Case 1 presentation
A 52 year-old female complaining of exertional shortness of breath was found to have a posterior mediastinal cyst that was originally identified on MRI scan for follow-up of a lipoma excision (Figure 1). A CT scan was subsequently performed that confirmed the presence of a 4.1 cm × 3.0 cm × 2.2 cm posterior mediastinal hypodense lesion consistent with a cyst, at the level of the carina, which was suspected to arise from either the right posterior lateral wall of the esophagus or the left main bronchus. The radiologic differential diagnosis included a bronchogenic cyst or esophageal duplication cyst. Surgical removal of the cyst was performed by robotic assisted thoracoscopy. The cyst was opened during the procedure. The removed tissue consisted of a collapsed unilocular cyst with a thin-wall and glistening, pink-tan inner surface. The specimen was submitted in its entirety for histologic examination.
Figure 1.
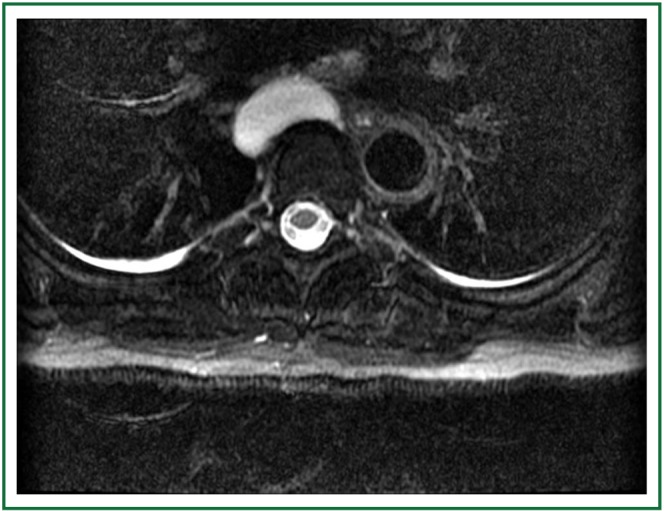
MR scan of posterior paravertebral mediastinal cyst.
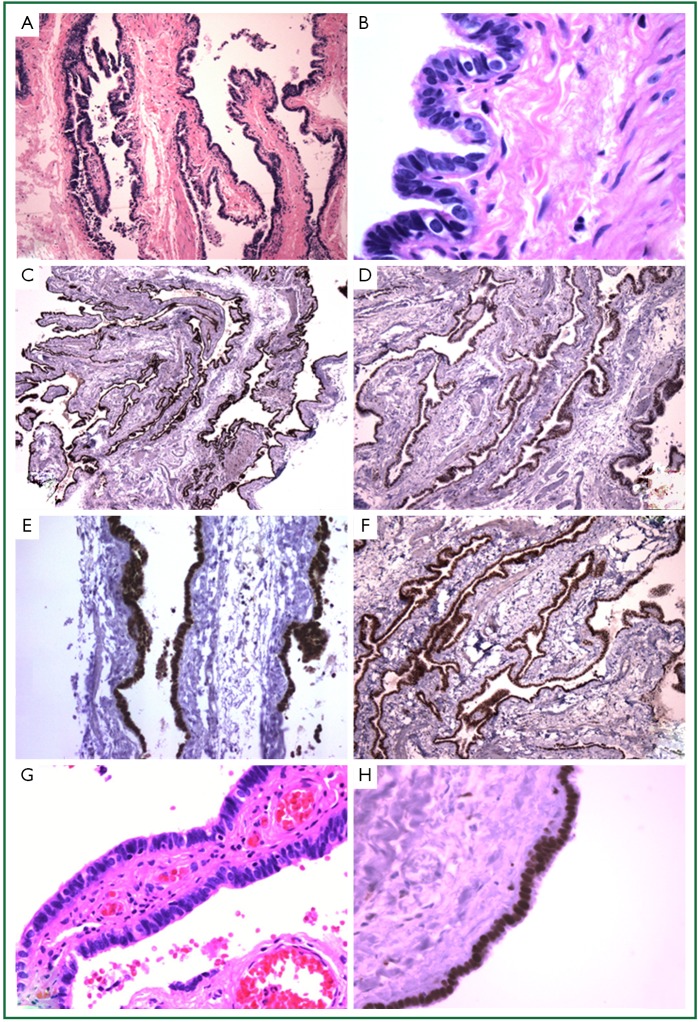
Microscopically, the tissue consisted of a thin-walled cyst lined by cylindrical to cuboidal epithelium (Figure 2A, B, C, D, E, F). Ciliated, secretory, and intercalated cells, consistent with Mullerian epithelium were easily identified. Smooth muscle was found adjacent to the epithelial lining, and capillaries were easily identifiable in the remainder for the loose fibrous stroma. The epithelial cells had nearly 100% nuclear staining for estrogen receptor (ER), progesterone receptor (PR), PAX8, and Wilm’s Tumor 1 (WT1) by immunohistochemistry, supportive of Mullerian differentiation. Ultimately, the case was signed out as a cyst of the posterior mediastinum showing Mullerian differentiation (Hattori’s cyst).
Figure 2.
Histologic appearance of two cases of posterior mediastinal cysts with Mullerian differentiation. (A) Microscopic appearance of cyst from Case 1 showing a thin wall supported by fibrous stroma [hematoxylin and eosin stain (H&E); magnification 4×]; (B) Higher magnification demonstrates the cyst lining is composed of Mullerian-type epithelium with ciliated columnar, secretory, and intercalated cells (H&E, 4×); (C) Immunohistochemistry for ER showing diffuse nuclear positivity in the cyst epithelium (4×); Immunohistochemistry for PR (D), PAX8 (E), and WT-1 (F) also demonstrates diffuse nuclear positivity in the lining epithelium (4×); (G) Microscopic appearance of cyst from Case 2 showing ciliated columnar cells with occasional intercalated cells (H&E, 20×) and also has diffuse nuclear staining for ER (H).
Case 2 presentation
Case 2 was a 47 year-old female who presented with a left posterior mediastinal mass. Excision of the mass revealed a 5.0 cm × 2.0 cm × 1.0 cm cyst lined by a smooth, glistening pink-red surface. Microscopically, the cyst was lined by ciliated columnar-type cells (Figure 2G, H) and was originally diagnosed as an esophageal cyst. However, re-examination of the histology revealed focal areas consisting of Mullerian-type epithelium with secretory and intercalated-type cells. Immunohistochemical stains for ER and WT1 were performed and were diffusely positive, consistent with a Hattori cyst.
Discussion
Review of the literature reveals only five previous reports regarding mediastinal cysts in the posterior mediastinum with Mullerian differentiation (2-6). Hattori (2) was the first to describe such a cyst in 2005 in an 18 year-old female. Hattori later published a review of 19 mediastinal cysts, three of which contained Mullerian differentiation (3). Subsequently, a group in France re-reviewed all mediastinal cysts received in their laboratory, and found that 5.5% of the cysts (nine total cases) had histological features consistent with Mullerian differentiation (4). However, two of these nine cases were negative for estrogen and progesterone receptor by immunohistochemical study, bringing the diagnosis of these two cysts somewhat into question. In 2007, Businger et al. (5) published a case report of a single cyst, and Batt et al. (6) published the first case report of mediastinal cyst with Mullerian differentiation in the United States.
In total, including the present cases, fourteen definitive mediastinal cysts with Mullerian differentiation have been identified. All of the cases have occurred in females 40-60 years old, with the exception of Hattori’s original case report occurring in an 18 year-old female. The patients typically presented with cough or were asymptomatic. All cysts were paravertebral in location, occurring between T3-T8 vertebrae. All of the cysts were positive for either ER or PR. Our report is the first to show expression of PAX8 and WT1, both markers of Mullerian differentiation, in these cysts.
Mullerian cysts in locations outside of the female pelvis are rare. Some reported locations include the skin (7) and retroperitoneum (8). The etiology of Mullerian cysts arising in the mediastinum is unclear. Several authors have proposed various theories as to their origin. Batt (6) suggested that the lesion is derived directly from the primary Mullerian apparatus, similar to that of the postulated pathogenesis for the Mayer-Rokitansky-Kuster-Hauser syndrome. Hattori (2) suggested that the cyst could represent misplaced mesothelium with Mullerian characteristics. It should be noted that Mullerian cysts located in the posterior mediastinum are likely of a different etiology than those in the retroperitoneum, given that the latter often have endocervical differentiation, which typically is not seen in the mediastinal cysts (9).
While only 14 cases of mediastinal cysts with Mullerian differentiation have been described in the literature, it is likely that they are much more common than presumed in older females and often misdiagnosed as either bronchial or esophageal cysts. It is likely that a paravertebral mediastinal ciliated cyst in a middle-aged female should be considered a cyst with Mullerian differentiation until proven otherwise. However, given the limited number of described cases and lack of clinical follow-up, it is uncertain whether these cysts have different clinical outcomes than bronchial or esophageal cysts. It does appear that the cysts behave in a benign fashion.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Takeda S, Miyoshi S, Minami M, et al. Clinical spectrum of mediastinal cysts. Chest 2003;124:125-32 [DOI] [PubMed] [Google Scholar]
- 2.Hattori H.Ciliated cyst of probable mullerian origin arising in the posterior mediastinum. Virchows Arch 2005;446:82-4 [DOI] [PubMed] [Google Scholar]
- 3.Hattori H.High prevalence of estrogen and progesterone receptor expression in mediastinal cysts situated in the posterior mediastinum. Chest 2005;128:3388-90 [DOI] [PubMed] [Google Scholar]
- 4.Thomas-de-Montpréville V, Dulmet E.Cysts of the posterior mediastinum showing müllerian differentiation (Hattori's cysts). Ann Diagn Pathol 2007;11:417-20 [DOI] [PubMed] [Google Scholar]
- 5.Businger AP, Frick H, Sailer M, et al. A ciliated cyst in the posterior mediastinum compatible with a paravertebral Mullerian cyst. Eur J Cardiothorac Surg 2008;33:133-6 [DOI] [PubMed] [Google Scholar]
- 6.Batt RE, Mhawech-Fauceglia P, Odunsi K, et al. Pathogenesis of mediastinal paravertebral müllerian cysts of Hattori: developmental endosalpingiosis-müllerianosis. Int J Gynecol Pathol 2010;29:546-51 [DOI] [PubMed] [Google Scholar]
- 7.Chong SJ, Kim SY, Kim HS, et al. Cutaneous ciliated cyst in a 16-year-old girl. J Am Acad Dermatol 2007;56:159-60 [DOI] [PubMed] [Google Scholar]
- 8.Konishi E, Nakashima Y, Iwasaki T.Immunohistochemical analysis of retroperitoneal Müllerian cyst. Hum Pathol 2003;34:194-8 [DOI] [PubMed] [Google Scholar]
- 9.Kondi-Pafiti A, Kairi-Vassilatoul E, Spanidou-Carvouni H, et al. Extragenital cystic lesions of peritoneum, mesentery and retroperitoneum of the female. Clinicopathological characteristics of 19 cases. Eur J Gynaecol Oncol 2005;26:323-6 [PubMed] [Google Scholar]