Abstract
Fibrosing mediastinitis is a rare but benign disorder characterized by an excessive fibrotic reaction in the mediastinum which can result in compromise of airways, great vessels, and other mediastinal structures. In this paper we presented a patient with fibrosing mediastinitis mimicking bronchogenic carcinoma. The patient was a 32-year-old diabetic male admitting with cough and hemoptysis. There was a right hilar mass and multiple mediastinal conglomerated lymph nodes on chest computed tomography. Positron emission tomography with computed tomography (PET/CT) scan demonstrated increased fluorodeoxyglucose (FDG) uptake at the right hilar mass lesion and mediastinal lymph nodes. Fiberoptic bronchoscopy showed mucosal distortion of right upper lobe. Pathologic examination of the mucosal biopsy revealed inflammation. Endobronchial ultrasound guided transbronchial needle and cervical mediastinoscopic lymph node biopsies were undiagnostic. Diagnostic thoracotomy confirmed the diagnosis fibrosing mediastinitis. Administration of six months of systemic corticosteroid and antituberculous therapy was not beneficial. In conclusion, despite being a rare clinical entity, fibrosing mediastinitis should be kept in mind in the differential diagnosis of mediastinal mass lesions of unknown etiology. The diagnosis is exceptionally difficult in the presence of atypical radiological findings. The treatment is particularly challenging without any proven effective therapy.
KEY WORDS : Fibrosing mediastinitis, tuberculosis, bronchogenic carcinoma
Introduction
Fibrosing mediastinitis is a rare but benign disorder characterized by an excessive fibrotic reaction in the mediastinum which can result in compromise of airways, great vessels, and other mediastinal structures. It is due to an excessive host response to a prior granulomatous infection which has involved the mediastinal lymph nodes. The vast majority of cases are thought to be sequela of histoplasmosis infection in the endemic regions (1). It is also associated with, tuberculosis, mediastinal radiation therapy, idiopathic fibrotic diseases such as sclerosing cholangitis, Reidels thyroiditis, and retroperitoneal fibrosis (2,3). In this paper we present a diabetic patient with fibrosing mediastinitis mimicking bronchogenic carcinoma.
Case
A 32-year-old male patient admitted with one month history of cough and hemoptysis. He denied anorexia, malaise, weight loss, night sweats or chest pain. In past medical history, he had hepatosteatosis diagnosed via liver biopsy performed due to high levels of transaminases. He had diabetes mellitus for the last two years and he was using insulin. He was smoking half packet of cigarettes per day, for the last 15 years. He was working as a cashier. He denied any exposure to occupational or environmental asbest exposure. There was no history of tuberculosis or a prior respiratory disease.
In physical examination, vital signs were normal, general and respiratory examination was unremarkable. Apart from a high fasting glucose level 177 mg/dL, eritrocyte sedimentation rate 48 mm/hr, liver function tests (AST: 73 IU/L, ALT: 92 IU/L), rutine laboratory analysis were normal. Respiratory function tests and oxygenation in room air were normal. The chest radiograph revealed prominence of right hilum and infiltration in the anterior segment of right upper lobe. A computed tomography scan revealed a 4 cm mass lesion in the right hilum and multiple mediastinal conglomerated lymph nodes (Figure 1). A PET/CT scan (Figure 2) demonstrated significantly increased activity (SUVmax: 9.74) at the right hilar mass lesion and right lower paratracheal (SUVmax: 3.57), subcarinal (SUVmax: 4.83), prevascular (SUVmax: 5.76) lymph nodes. Fiberoptic bronchoscopy showed mucosal distortion of right upper lobe. Pathologic examination of the mucosal biopsy revealed inflammation. Endobronchial ultrasound guided transbronchial needle biopsy from the hilar mass, right lower paratracheal and subcarinal lymph nodes revealed CD-45 positive normal lymphoid cells without any evidence of malignancy (Figure 3). Cervical mediastinoscopic biopsies of right lower paratracheal and subcarinal lymph nodes were undiagnostic. Diagnostic thoracotomy confirmed the diagnosis fibrosing mediastinitis. Hilar mass was a conglomerated lymph node showing dense hyalinized fibrous tissue with chronic inflammation (Figure 4). We administered 6 months of systemic corticosteroid and antituberculous therapy (Isoniazid, rifampicin, pirazinamid, ethambutol for two months and isoniazid, rifampicin for four months). A thorax tomography performed after discontinuation of therapy revealed similar findings with the postoperative thorax tomography.
Figure 1.
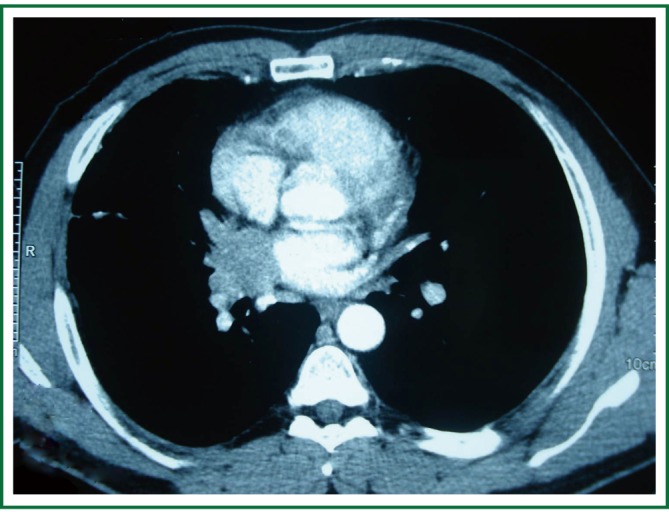
Right hilar mass lesion 4 cm in diameter is seen on computed tomography scan of thorax.
Figure 2.
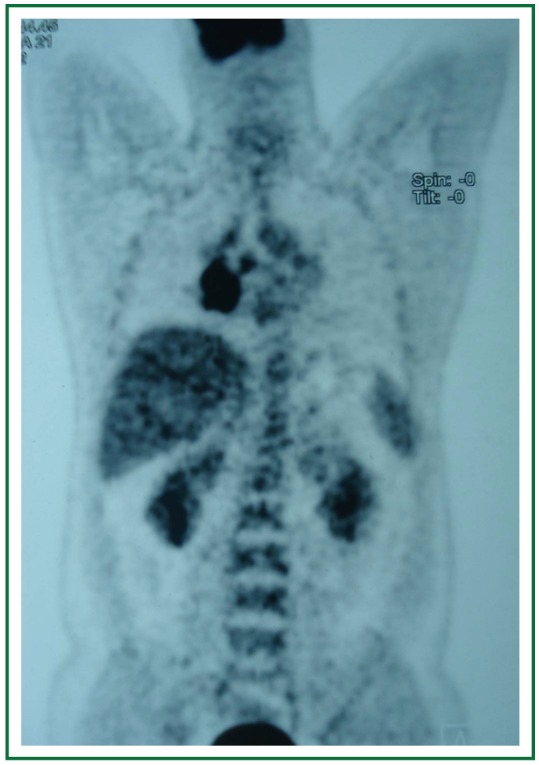
PET/CT scan demonstrating significantly increased activity at the right hilar mass lesion and mediastinal lymph nodes.
Figure 3.
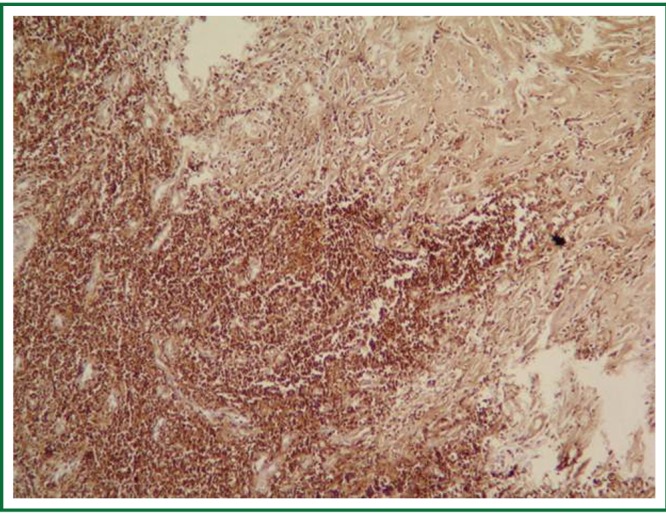
CD45 positivity in the lymphoid tissue obtained by endobronchial ultrasound guided needle biopsy (CD45 ×200).
Figure 4.
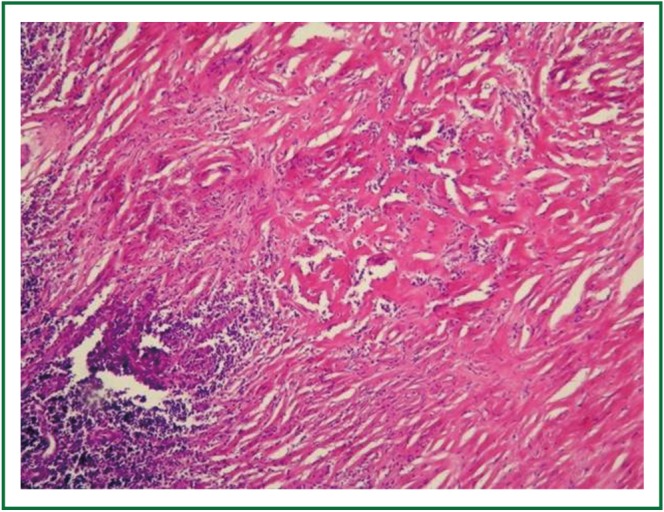
Fibrous tissue with collagen bundle in lymph node and adipose tissue (HE ×100).
Discussion
Fibrosing mediastinitis is a disorder characterized by an excessive fibrotic reaction in the mediastinum. The cause is probably an abnormal fibroproliferative response to an inflammatory stimulus that leads to encasement of mediastinal structures within a dense fibrotic mass. The inflammatory stimulus is commonly the infection with Histoplasma Capsulatum in the endemic regions (southeastern, mid-Atlantic, central United States). Tuberculosis is often included as a potential precipitant of fibrosing mediastinitis, but it rarely stimulates an invasive fibrotic reaction similar to that seen following histoplasmosis (4,5). In this patient, we suggested that fibrosing mediastinitis is a result of untreated, spontaneously healed mediastinal tuberculosis infection and diabetes mellitus might be a facilitator of this infection.
The clinical presentation of fibrosing mediastinitis depends on the structures of the mediastinum which are compressed externally by the fibrotic tissue (1). The airways, heart and great vessels, esophagus are the major organs that can be involved. Tracheobronchial narrowing is a common presentation of fibrosing mediastinitis and is most commonly seen in the right upper lobe as in the presented patient.
In computed tomography, fibrosing mediastinitis is strongly suggested by the obliteration of fat planes of the mediastinum and the presence of discrete masses and/or extensive calcified paratracheal, hilar and subcarinal lymphadenopathy causing circumferential encasement of the mediastinal structures (4,6). Sometimes it is difficult to distinguish a discrete mass from a malignant process despite enhanced imaging modalities. It can mimic a bronchogenic carcinoma in countries outside endemic fungal infection areas (5).
In the endemic areas, the diagnosis is usually based on typical clinical and radiological findings (1). Mediastinoscopy or thoracotomy may be necessary to exclude malignancy and to confirm diagnosis (4). But in the presence of atypical features invasive diagnostic procedures are needed (7). It is usually difficult to make an accurate histopathological diagnosis using minimally invasive methods. Consequently many patients with fibrosing mediastinitis undergo surgical biopsy of the mediastinum to confirm the diagnosis and rule out a neoplasm. In this patient, there was a non-calcified right hilar mass lesion on CT scan. On PET/CT there was a high uptake of fluorodeoxyglucose both on the right hilar mass lesion and mediastinal lymph nodes. Endobronchial ultrasound guided mediastinal lymph node biopsies and mediastinoscopic biopsies were undiagnostic that the patient was sent to thoracotomy.
There is no proven effective medical therapy for fibrosing mediastinitis. Most of the avaliable data are based either on case reports or small case series. There have been no prospective randomized controlled trials conducted so far. Corticosteroids do not appear to be beneficial apart from a few cases proving its benefit for symptomatic relief of dyspnea due to vena cava superior obstruction (8). Another possible exception is autoimmune fibrosing mediastinitis which appears to respond more favorably to steroid therapy. However these cases are difficult to identify prospectively (9). Tamoxifen was also shown to be effective in selected cases (10). In the presented patient, after informing the patient about the outcome, potential beneficial and adverse effects of the therapy, we instituted a therapy regimen including corticosteroids and antituberculosis drugs. Antituberculosis drugs are given to the patient in order to prevent reactivation tuberculosis disease due to long term corticosteroid therapy. After six months we stopped the therapy due to unchanged radiological and clinical findings.
In conclusion, despite being a rare clinical entity, fibrosing mediastinitis should be kept in mind in the differential diagnosis of mediastinal mass lesions of unknown etiology. The diagnosis is exceptionally difficult in the presence of atypical radiological findings. The treatment is particularly challenging without any proven effective therapy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Loyd JE, Tillman BF, Atkinson JB, et al. Mediastinal fibrosis complicating histoplasmosis. Medicine (Baltimore) 1988;67:295-310 [DOI] [PubMed] [Google Scholar]
- 2.Mole TM, Glover J, Sheppard MN. Sclerosing mediastinitis: a report on 18 cases. Thorax 1995;50:280-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dechambre S, Dorzee J, Fastrez J, et al. Bronchial stenosis and sclerosing mediastinitis: an uncommon complication of external thoracic radiotherapy. Eur Respir J 1998;11:1188-90 [DOI] [PubMed] [Google Scholar]
- 4.Goodwin RA, Nickell JA, Des Prez RM. Mediastinal fibrosis complicating healed primary histoplasmosis and tuberculosis. Medicine (Baltimore) 1972;51:227-46 [DOI] [PubMed] [Google Scholar]
- 5.Bateman K, Chauhan AJ, Singh N, et al. Sclerosing mediastinitis in a smoker with suspected lung cancer. Respir Med CME 2010;3:257-9 [Google Scholar]
- 6.Sherrick AD, Brown LR, Harms GF, et al. The radiographic findings of fibrosing mediastinitis. Chest 1994;106:484-9 [DOI] [PubMed] [Google Scholar]
- 7.Dunn EJ, Ulicny KS, Jr, Wright CB, et al. Surgical implications of sclerosing mediastinitis. A report of six cases and review of the literature. Chest 1990;97:338-46 [DOI] [PubMed] [Google Scholar]
- 8.Bays S, Rajakaruna C, Sheffield E, et al. Fibrosing mediastinitis as a cause of superior vena cava syndrome. Eur J Cardiothorac Surg 2004;26:453-5 [DOI] [PubMed] [Google Scholar]
- 9.Ikeda K, Nomori H, Mori T, et al. Successful steroid treatment for fibrosing mediastinitis and sclerosing cervicitis. Ann Thorac Surg 2007;83:1199-201 [DOI] [PubMed] [Google Scholar]
- 10.Clark CP, Vanderpool D, Preskitt JT. The response of retroperitoneal fibrosis to tamoxifen. Surgery 1991;109:502-6 [PubMed] [Google Scholar]


