Negative Affect Shares Genetic and Environmental Influences with Symptoms of Childhood Internalizing and Externalizing Disorders
Epidemiological studies conducted in the United States estimate that the average prevalence rate for childhood (age 9 – 13) and adolescent (age 13 – 18) psychopathology is between 13% and 22% (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Merikangas et al., 2010). Further, of those who have any disorder, 25% – 40% have two or more disorders (Costello et al., 2003). Research examining the latent structure of common mental disorders has supported the conceptualization of two broad, higher-order Internalizing and Externalizing factors. This structure has been found in both child and adolescent samples (Cosgrove et al., 2011; Hewitt et al., 1997; Lahey et al., 2004; Lahey, Rathouz et al., 2008). The Internalizing factor reflects anxiety, fear, and misery and typically includes major depressive disorder (MDD), generalized anxiety disorder (GAD), separation anxiety disorder (SAD), panic disorder (PD), and phobias (Cosgrove et al., 2011; Krueger, 1999). The Externalizing factor reflects acting-out, aggression, and antisocial behavior and usually includes attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and conduct disorder (CD) in children and adolescents (Lahey et al., 2004; Lahey, Rathouz et al., 2008).
Although internalizing and externalizing problems are conceptualized as distinct factors, they are often correlated (Angold, Costello, & Erkanli, 1999; Cosgrove et al., 2011; Kessler, Chiu, Demler, & Walters, 2005; Krueger 1999; Krueger, Caspi, Moffitt, & Silva, 1998; Krueger & Markon, 2006; O’Connor, McGuire, Reiss, Hetherington, & Plomin, 1998; Pesenti-Gritti et al., 2008; Rhee, et al., 2007). The correlation between Internalizing and Externalizing factors is estimated to be between .66 and .72 in children (Cosgrove et al., 2011; Lahey et al., 2004), suggesting substantial co-occurrence of disorders across factors. Children and adolescents with co-occurring psychopathology are at increased risk for later alcohol and substance use problems (Miller-Johnson, Lochman, Coie, Terry, & Hyman, 1998; Pardini, White, & Stouthamer-Loeber, 2007), increased antisocial behavior (Polier, Vloet, Herpertz-Dahlmann, Laurens, & Hodgins, 2012), arrests, sexual promiscuity (Dishion, 2000), suicidal ideation (Capaldi, 1992), repeat admission to inpatient services (Fite, Stoppelbein, Greening, & Dhossche, 2008), and adult psychopathology (Dalsgaard, Mortensen, Frydenberg, & Thomsen, 2002; Fischer, Barkley, Smallish, & Fletcher, 2002; Fombonne, Wostear, Cooper, Harrington, & Rutter, 2001).
Genetic and Environmental Influences on Co-occurring Internalizing and Externalizing Behaviors
Despite the high prevalence and negative outcomes, relatively little is known about the development of co-occurring disorders. One possible route to co-occurrence is through common genetic and environmental influences. The twin study method allows for an estimation of the contribution of genetic, shared environmental, and nonshared environmental influences on a behavior or set of behaviors. Genetic influences, and more specifically additive genetic influences, refer to the sum of effects across multiple gene alleles which are directly inherited from one’s parents. Shared environmental influences are aspects of the environment that affect both twins and make them more similar, and nonshared environmental influences are those that are unique to each twin (as well as measurement error) and contribute to differences between twins. Twin studies have been used to examine the overlap of genetic and environmental influences between internalizing and externalizing behaviors and results have been mixed. For instance, in a community sample of 10- to 18-year-old twins, O’Connor et al. (1998) examined checklists of depression and antisocial symptoms and found that 45% of their co-occurrence was attributed to genetics, 30% to shared environment, and 25% to nonshared environment. However, Gjone and Stevenson (1997a) found that shared environment primarily accounted for the co-occurrence between Child Behavior Checklist (CBCL; Achenbach, 1991) internalizing and externalizing scores for children between the ages of 5 and 15, although genetic influences contributed as well, especially in older children. Differences between these studies are expected, though, due to different conceptualizations of internalizing and externalizing behaviors (i.e., symptoms of a single disorder vs. a broad measure). However, others examining the CBCL in a slightly older sample found that both shared environment and genetic factors contributed about equally to the co-occurrence of internalizing and externalizing behaviors, with negligible influence of non-shared environmental factors (Pesenti-Gritti et al., 2008). Although the CBCL provides a broad measure of externalizing, it does not tap into all symptoms of disorders on the externalizing spectrum. For example, the externalizing scale of the CBCL does not include symptoms of ADHD. Perhaps a more comprehensive way to examine the covariation between internalizing and externalizing problems is to conceptualize each as the latent factor underlying internalizing and externalizing disorders.
A recent study by Cosgrove and colleagues (2011) examined the genetic and environmental effects of the covariance between an Internalizing factor (including MDD, GAD, and SAD) and an Externalizing factor (including ADHD, ODD, and CD) with manifest variables assessed using a clinical interview in a large community sample of 12- to 18-year-old adolescent twins. Using a bivariate common factor model, they concluded that the co-occurrence between these Internalizing and Externalizing factors was due to common genetic influences (62%) as well as nonshared environmental influences (38%), with no shared environmental influences. Another recent study (Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011) examined a slightly younger sample of twins (i.e., ages 9–17 years) and assessed a wider range of psychopathology, including agoraphobia, obsessive-compulsive disorder (OCD), social phobia (SP), and specific phobia on the Internalizing factor. They tested several models of the structure of genetic and environmental effects of these disorders and similarly concluded that co-occurrence among the disorders can be explained primarily by genetics, with very little influences of shared and nonshared environment. Overall, the majority of the research suggests that genetic influences contribute, at least to some degree, to the co-occurrence between internalizing and externalizing disorders. Conclusions about environmental influences are more difficult to establish. Studies measuring the dimensions of internalizing and externalizing with the CBCL tend to find more shared environmental effects, whereas studies assessing the individual disorders that make up the Internalizing and Externalizing factors tend to find smaller or nonsignificant shared environmental effects contributing to the co-occurrence.
The Role of Negative Affect
Another route to co-occurrence of internalizing and externalizing disorders may be through common underlying dispositions, such as temperament or personality factors (Clark, 2005; Bijttebier & Roeyers, 2009; Lilienfeld, 2003; Muris & Ollendick, 2005; Nigg, 2006; Saudino, 2005; Tackett, 2006). Although several dispositions may interact to influence the development of specific psychopathology, it has been proposed that negative affect may play a causal role in the development of both internalizing and externalizing disorders (Lilienfeld, 2003). Negative affect (sometimes referred to as negative emotionality) is defined as the stable and pervasive propensity to experience aversive emotions, such as nervousness, anger, guilt, rejection, and sadness (Watson & Clark, 1984). Research has shown that negative affect is moderately positively correlated with both internalizing and externalizing disorders in children (Anthony, Lonigan, Hooe, & Phillips, 2002; Gjone & Stevenson, 1997b; Guerin, Gottfried, & Thomas, 1997; Lengua, West, & Sandler, 1998; Muris, Meesters & Blijlevens, 2007; Rhee et al., 2007; Singh & Waldman, 2010) and has been conceptualized as a predisposition for both (Clark, Watson, & Mineka, 1994; Lonigan, Phillips, Wilson, & Allan, 2011; Muris & Ollendick, 2005; Schmitz et al., 1999; Tackett, 2006), whereas other dispositions are often conceptualized as specifically related to either internalizing (i.e., positive affect; Watson & Naragon-Gainey, 2010) or externalizing (i.e. constraint; Krueger et al., 2002) disorders. Given the idea that negative affect may underlie both internalizing and externalizing disorders, examining their common genetic and environmental influences may provide a greater understanding of vulnerability to childhood psychopathology, and may inform the development of effective interventions.
Genetic and Environmental Influences on Covariation of Negative Affect and Internalizing Behaviors
Only one study to date examined the common genetic and environmental influences of negative affect and internalizing disorders in children or adolescents. Goldsmith and Lemery (2000) examined the longitudinal bivariate relationships between fear (negative affect as a result of anticipated threat) and overanxious and separation anxiety symptoms in twins ages 3 to 9 years. They found that fear and overanxious symptoms had common genetic influences, and fear and separation anxiety had common shared environmental influences. Although there is limited research examining young samples, several studies have examined the common genetic and environmental influences of neuroticism (a personality construct similar to negative affect) and internalizing disorders in adults (Hettema, Neale, Myers, Prescott, & Kendler, 2006; Hettema, Prescott, & Kendler, 2004; Jardine, Martin, & Henderson, 1984). In these studies, the relationship between neuroticism and internalizing disorders was largely due to common genetic influences.
Genetic and Environmental Influences on Covariation of Negative Affect and Externalizing Behaviors
Others have examined the common genetic and environmental influences on negative affect and externalizing disorders (Singh & Waldman, 2010; Waldman et al., 2011) and found that the relationship between them is due largely to common genetic influences and, to a lesser degree, nonshared environmental influences. In the most comprehensive study thus far, Singh and Waldman (2010) examined the genetic and environmental influences on the covariation between the manifest variables of negative affect, ODD, CD, inattention, and hyperactivity/impulsivity in a sample of 838 four- to seventeen-year-old twins. They first fit bivariate models to negative affect and each externalizing disorder separately. They then fit a multivariate model to negative affect and all the externalizing disorders together. Their results suggested that negative affect and externalizing disorders have common genetic variance (25–67%), nonshared environment variance (5–23%), but not shared environment variance. Further, CD, inattention, and hyperactivity/impulsivity shared all of their additive genetic influences with negative affect.
Genetic and Environmental Influences on Covariation of Negative Affect, Internalizing, and Externalizing Behaviors
The first reported twin study of the covariation of negative affect, internalizing, and externalizing behavior was conducted by Gjone and Stevenson (1997b). This study used the EAS Temperament Survey (Buss & Plomin, 1984) to assess emotionality (the tendency to cry and get upset easily, and react intensely when upset) which is similar to negative affect. The authors conducted a series of bivariate analyses examining the longitudinal relation between emotionality and behavioral problems, including anxious/depressed behavior, attention problems, delinquent behavior, and aggressive behavior (assessed with the CBCL), in 7- to 17-year-old twins. Their results suggested that there were no common genetic or environmental factors between emotionality and anxious/depressed behavior or between emotionality and delinquent behavior. Further, only common genetic factors (not environmental factors) accounted for the relations between emotionality and aggressive behavior and between emotionality and attention problems.
Using a younger twin sample, Schmitz et al. (1999) reported findings on bivariate relationships between infant emotionality (as measured by the Colorado Childhood Temperament Inventory; CCTI; Rowe & Plomin, 1984) and internalizing and externalizing scores from the CBCL at age 4 years. Consistent with Gjone and Stevenson (1997b), they concluded that common genetic factors accounted for the relation between emotionality and externalizing behaviors, although they also found a similar relation with internalizing behaviors. Rhee and colleagues (2007) intended to extend the findings from the Schmitz et al. (1999) study by examining the relation between emotionality in infancy (assessed with the CCTI) and internalizing and externalizing behaviors assessed (with the CBCL) between ages 4 and 12 years. This was the first study to explore emotionality, internalizing behaviors, and externalizing behaviors together in a single multivariate model. Because the researchers were interested in disentangling the effects of gender, they explored these relations in males and females separately. They reported that, for males, emotionality did not share genetic or shared environmental influences with internalizing or externalizing, though nonshared environmental influences had a small but significant inverse influence on externalizing. For females, emotionality, internalizing, and externalizing only had shared environmental influences in common. However, Rhee et al. were concerned that their mulitivariate analyses were underpowered and therefore reinterpreted the data by dividing phenotypic correlations between emotionality and internalizing behaviors and emotionality and externalizing behaviors into phenotypic correlations attributable to common genetic, shared environmental, and nonshared environmental effects. Results from those analyses suggested that, in males, the covariation between emotionality and internalizing behaviors and between emotionality and externalizing behaviors was explained by common genetic influences and shared environmental influences. In females, the covariation between emotionality and internalizing behaviors and emotionality and externalizing behaviors was explained mostly by common shared environmental influences.
Finally, a recent study by Tacket, Waldman, Van Hulle, and Lahey (2011) examined whether the genetic influences on negative emotionality (as assessed by the Child and Adolescent Dispositions Scale; CADS; Lahey, Applegate et al., 2008) were shared with the genetic influences contributing to the co-occurrence between MDD and CD. Using data from over 2,000 twin pairs between the ages of 6 and 18 years, Tackett et al. examined multivariate models on manifest variables separately for males and females. They found common genetic (for males only), shared environmental, and nonshared environmental influences on negative emotionality, internalizing (MDD), and externalizing (CD).
Overall, research examining the common genetic and environmental influences on negative affect, internalizing behavior, and externalizing behavior suggests that primarily genetic influences contribute to their covariation; however, the evidence for the contribution of shared and nonshared environmental influences is mixed, suggesting the need for additional research to clarify the influences of these factors. Further, only two previous studies have examined negative affect, internalizing problems, and externalizing problems in the same model (Rhee et al., 2007; Tackett et al., 2011). To date, no studies have examined the genetic and environmental influences on the covariation between negative affect, internalizing, and externalizing, while conceptualizing internalizing and externalizing as factors that capture the shared variance among the disorders that make up those dimensions. The current study addresses this gap in the literature with a sample of child and adolescent twins. Examining the common genetic and environmental influences may aid in understanding vulnerability to the development of co-occurring internalizing and externalizing psychopathology. For instance, if the data show that common genetic influences are associated with negative affect, internalizing, and externalizing, then this would suggest that genes are conferring risk for a child to experience negative affect as well as conferring risk for developing a range of psychological disorders. If shared environmental influences are associated with negative affect, internalizing, and externalizing, then this would indicate that perhaps aspects of the rearing environment (e.g., low parental warmth, chaotic home environment, low economic resources, etc.) promote the development of negative affect and a range of psychological disorders in children. Further, using a factor model will allow for including the full spectrum of internalizing and externalizing problems while also decreasing the influence of error in the model. Based on previous findings, it was hypothesized that the covariation between the three factors (Negative Affect, Internalizing, and Externalizing) would be mostly explained by common underlying genetic influences. It was expected that shared and nonshared environmental influences would also contribute to the covariation, though to a lesser degree than genetic influences.
Method
Participants
Twins for this study were originally recruited through the Twin Registry via the Project on Reading (e.g.,). Twins were identified through a statewide database of student academic test scores and parent-provided school registration information. Recruitment packets for inclusion in the Twin Registry were given to parents of children in this database who had the same last name, birth date, and school and were in grades K through 5. These packets contained a letter about the study, a consent form for the parents, and a five-question form assessing zygosity that has been used in other twin studies and has demonstrated a high accuracy rate (Lykken, Bouchard, McGue, & Tellegen, 1990). As part of a larger study concerning the behavior and environment of twins, parents whose families were part of the Twin Registry were mailed consent and assent forms, questionnaires, and a cover letter explaining the project. One parent (or guardian) was asked to complete the questionnaire. Given the young age of the twins, it was expected that a parent would provide the most valid and accurate report of the twins’ symptomatology. Parents received a $30 gift card to the retailer of their choice for their participation.
Through the Twin Registry, 1,624 same-sex twin families were sent packets requesting their participation. Of the packets sent out, 150 (9%) were returned by the post office as undeliverable. Of the packets delivered, 718 families (49%) replied, and 693 families (47%) agreed to participate and returned a completed packet. Two families were not included because the zygosity of the twins could not be determined. The final sample for this study included 691 same-sex 7- to 13-year-old (M = 10.08, SD = 1.73) twin pairs and their parents (350 families with female twins; 341 families with male twins). Racial composition of the present sample as reported by parents was 70% White, 12% African American, 9% mixed race, 2% Asian, and 5% other with 2% failing to provide information about race. Parent reported ethnic composition was 24% Hispanic and 70% non-Hispanic with 6% not reporting ethnicity. Parents reported household income on a scale ranging from 1 “less than $10,000” to 6 “$90,000 or more”. The mean response was 3.98 (SD = 1.67), indicating an average household income of $50,000 to $69,000. The modal reported income was $90,000 or more. Income was not reported by 3.5% of the sample. There were no significant differences between MZ and DZ twins on parent reported race (χ2 (4, N = 675) = 4.60, p =.33), ethnicity (χ2 (1, N = 652) = 1.46, p = .23) or income (χ2 (6, N = 667) = 8.14, p =.23). Potential sampling biases were examined by comparing participants and non-participants on demographic variables available from 2000 census data by zip code in which the twins’ family lived (detailed data on income were not available from the 2010 census). Participants did not differ from non-participants in terms of housing value (t = 1.28, p = .20) and number of households (t = 1.46, p = .14). Participants lived in areas with significantly higher median family income than non-participants (t = 2.18, p = .03), but the effect size was small (d = .12). There was also a significantly higher number of households receiving public assistance in the areas where non-participants lived (t = 4.44, p < .001) and again the effect was small (d =.24). It should be noted that no multiple-comparison correction was used, allowing for a less conservative view of differences between groups.
Measures
Externalizing behaviors
The Disruptive Behavior Disorder scale (DBD; Pelham, Gnagy, Greenslade, & Milich, 1992) was used to measure parent reported externalizing disorder symptoms. Previous studies provide support for the reliability and validity of the DBD (Pelham, Fabiano, & Massetti, 2005). Further, research suggests that parent report of child disruptive behavior disorders may be more valid than child report (Loeber, Green, Lahey, & Stouthamer-Loeber, 1989; Smith, 2007). The DBD contains 45 items closely aligned with the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV; American Psychiatric Association, 2000) criteria for ODD, CD, and the inattention and hyperactive/impulsive dimensions of ADHD. Parents rate their children on a 4-point Likert-like scale, with response options of 0 “Not at all” to 3 “Very much.” Scores for inattention, hyperactivity/impulsivity, ODD, and CD scales were obtained by calculating the mean of the summed responses to each scale. Scales were created allowing for up to 10% missing data by respondent. Oppositional defiant disorder was measured by eight items and provided adequate reliability in this sample (α = .86). Conduct disorder was measured by 15 items and provided adequate reliability (α = .71). The inattention and hyperactivity dimensions of ADHD were measured by nine items each and provided adequate reliability (α = .90 and α = .85 respectively).
Internalizing behaviors
The Revised Child Anxiety and Depression Scale (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) is a 47-item measure originally designed to assess child self-report symptoms of the DSM-IV internalizing disorders of MDD, SP, SAD, PD, GAD, and OCD. The parent version used in this study is identical to the child version except that the items have been altered so as to apply to the parent’s perspective (Ebesutani, Chorpita et al., 2011; Muris, Meesters, & Spinder, 2003). The parent version of the RCADS has demonstrated good convergent and discriminant validity and reliability (Ebesutani, Chorpita et al., 2011). Items are assessed using a 4-point Likert-like scale, with response options of 1 “Never” to 4 “Always.” Scores for each scale were obtained by calculating the mean of the summed responses to each scale. Scales were created allowing for up to 10% missing data by respondent. Major depressive disorder was measured by 10 items and provided adequate reliability in this sample (α = .75). Social phobia was measured by nine items and provided adequate reliability (α = .82). Panic disorder was measured by nine items also and provided marginal reliability (α = .69). Separation anxiety disorder was measured by seven items and provided marginal reliability (α = .68). Generalized anxiety disorder was measured by six items and provided adequate reliability (α = .81). Obsessive-compulsive disorder was measured by six items and provided marginal reliability (α = .63).
Negative affect
Negative emotionality
The Child and Adolescent Dispositions Scale (CADS; Lahey, Applegate et al., 2008) is a 57-item measure designed to assess the dispositions of prosociality, negative emotionality, and daring. Previous studies provide support for the reliability, internal validity, and external validity of caretaker ratings of the CADS scales (Lahey, Applegate et al., 2008). Parents rate how often children’s behavior occurred over the last 12 months using a 4-point Likert-like scale with response options 1 “Not at all” to 4 “Very much.” Scores for each scale were obtained by calculating the mean of the summed responses to each scale. Only the negative emotionality scale was used in this study. Negative emotionality was measured by seven items and provided adequate reliability in this sample (α = .78).
Negative affect
The PANAS (Watson, Clark, & Tellegen, 1988) was used to measure positive and negative affect. The PANAS contains 20 one-word adjective items reflecting relatively pure positive and negative emotions. Research supports the use of parent rated measures of positive and negative affect (Ebesutani, Okamura, Higa-McMillan, & Chorpita, 2011). Parents rate the degree children feel each emotion using a 5-point Likert-like scale with response options 1 “Very slightly or not at all” to 5 “Extremely.” Scores for each scale were obtained by calculating the mean of the summed responses to each scale. Scales were created allowing for up to 10% missing data by respondent. Only the negative affect scale was used in this study. Negative affect was measured by 10 items and provided adequate reliability (α = .86).
Data Analysis
Twin analyses take into account that identical or monozygotic (MZ) twins share 100% of their genes, and fraternal or dizygotic (DZ) twins share approximately 50% of their segregating alleles. This allows for an estimation of additive genetic (A), shared environmental (C), and nonshared environmental (E) influences on traits and behaviors. First, twin intraclass correlations were calculated and compared across zygosity for all measured variables. Intraclass correlations suggest genetic influences when MZ correlations are higher than DZ correlations, shared environmental influences when MZ correlations are less than twice the magnitude of DZ correlations, and nonshared environmental influences (and measurement error) when MZ correlations are less than 1.00. Next, univariate biometrical models were used to estimate A, C, and E for each measured variable.
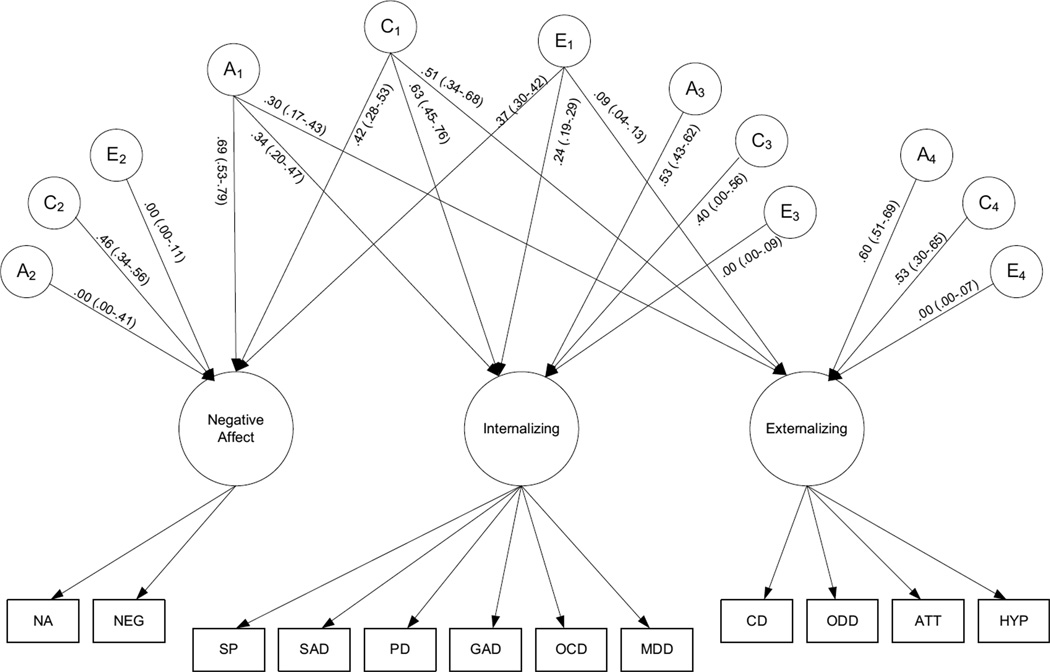
Finally, a multifactorial independent pathway model (Neale & Cardon, 1992) was used to examine the genetic and environmental influences underlying the covariation of negative affect, internalizing disorder symptoms, and externalizing disorder symptoms (see Figure 1). As a first step within the larger model, three factors representing the three constructs were created. The use of factors allows for a test of construct validity, as well as provides random-error-free estimates for further analyses (see Gayan & Olson, 2003). Therefore, the Negative Affect factor was comprised of the negative emotionality scale from the CADS and the negative affect scale from the PANAS. The Internalizing factor was comprised of the SP, SAD, PD, GAD, OCD, and MDD scales from the RCADS. The Externalizing factor was comprised of the CD, ODD, inattention, and hyperactivity/impulsivity scales of the DBD.
Figure 1.
Independent pathway model representing Negative Affect, Internalizing, and Externalizing as separate factors. Standardized path coefficients and residuals (and 95% confidence intervals) are provided. A = additive genetic influences; C = shared environmental influences; E = nonshared environmental influences; NA = Negative Affect scale from the PANAS; NEG = Negative Emotionality scale from the CADS; SP = social phobia; SAD = separation anxiety disorder; PD = panic disorder; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; MDD = major depressive disorder; CD = conduct disorder; ODD = oppositional defiant disorder; ATT = attention-deficit hyperactivity disorder inattention; HYP = attention-deficit hyperactivity disorder hyperactivity/impulsivity.
An independent pathway model was simultaneously applied to the factors, allowing for four sets of biometric factors to be estimated. The first set (A1, C1, and E1) is particularly relevant for the current hypotheses, as it represents the genetic and environmental influences that contribute to the covariance among the three factors (Negative Affect, Internalizing and Externalizing). The other three sets of biometric factors represent the genetic and environmental influences that are unique to each factor after accounting for the first set of biometric factors.
Results
Means, standard deviations, and ranges for all raw variables are presented in Table 1. The distributions of measured variables were examined for normality and found to be positively skewed. Therefore, data were transformed using an inverse transformation as recommended by Tabachnick and Fidell (2007). Because age and gender effects can bias twin analyses, and age and gender differences were not a focus of the current hypotheses, data were corrected by residualizing on age, age-squared, gender, and an age-by-gender interaction prior to analyses (McGue & Bouchard, 1984). However, it should be noted that non-transformed and non-residualized data produced similar results. Pearson correlations between variables (post transforming and residualizing) are presented in Table 2, and intraclass correlations by zygosity are presented in Table 3. Intraclass correlations were consistently higher among MZ twins, suggesting genetic influences. Given that the MZ correlations were not twice the magnitude of DZ correlations and less than 1.00, there was also evidence for shared and nonshared environmental influences.
Table 1.
Descriptive Statistics for Negative Affect, Internalizing and Externalizing Scales.
| Variable | Mean | SD | Range | Skewness | |
|---|---|---|---|---|---|
| Minimum | Maximum | ||||
| Negative Affect | |||||
| Negative Affect | 18.23 | 6.94 | 6.00 | 47.00 | −0.13 |
| Negative Emotionality | 18.55 | 4.60 | 9.00 | 36.00 | 0.21 |
| Internalizing | |||||
| Social Phobia | 16.46 | 4.30 | 9.00 | 35.00 | 0.16 |
| Separation Anxiety | 10.75 | 3.16 | 7.00 | 24.00 | −0.37 |
| Panic | 10.51 | 1.94 | 8.00 | 32.00 | −1.59 |
| Generalized Anxiety | 9.30 | 2.80 | 6.00 | 24.00 | −0.51 |
| Obsessive−Compulsive | 7.13 | 1.73 | 6.00 | 20.00 | −1.39 |
| Depression | 12.49 | 2.88 | 9.00 | 32.00 | −1.08 |
| Externalizing | |||||
| Conduct | 0.79 | 1.72 | 0.00 | 19.00 | −2.48 |
| Oppositional Defiant | 3.10 | 3.57 | 0.00 | 23.00 | −0.38 |
| Inattention | 4.67 | 4.74 | 0.00 | 25.00 | −0.14 |
| Hyperactivity | 4.43 | 4.36 | 0.00 | 27.00 | −0.19 |
Note: Skewness values are provided for variables used in analyses (after residualizing and transforming data).
Table 2.
Pearson Correlations among Negative Affect, Internalizing and Externalizing Scales.
| Negative Affect | Internalizing | Externalizing | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| 1. Negative Affect | 1.00 | |||||||||||
| 2. Negative Emotionality | .52* | 1.00 | ||||||||||
| 3. Social Phobia | .35* | .38* | 1.00 | |||||||||
| 4. Separation Anxiety | .33* | .26* | .42* | 1.00 | ||||||||
| 5. Panic | .38* | .30* | .50* | .41* | 1.00 | |||||||
| 6. Generalized Anxiety | .47* | .35* | .56* | .51* | .55* | 1.00 | ||||||
| 7. Obsessive Compulsive | .37* | .24* | .38* | .41* | .49* | .53* | 1.00 | |||||
| 8. Depression | .50* | .46* | .47* | .41* | .51* | .52* | .50* | 1.00 | ||||
| 9. Conduct | .28* | .38* | .13* | .07* | .12* | .17* | .15* | .31* | 1.00 | |||
| 10. Oppositional Defiant | .44* | .64* | .25* | .16* | .20* | .26* | .19* | .46* | .62* | 1.00 | ||
| 11. Inattention | .31* | .47* | .21* | .14* | .22* | .20* | .19* | .43* | .47* | .63* | 1.00 | |
| 12. Hyperactivity | .31* | .53* | .17* | .13* | .22* | .23* | .22* | .38* | .48* | .66* | .69* | 1.00 |
| Standardized Loadings | .99* | .52* | .66* | .62* | .70* | .78* | .68* | .73* | .66* | .85* | .79* | .79* |
| Standardized Residuals | .01 | .73* | .57* | .61* | .51* | .39* | .54* | .47* | .57* | .28* | .38* | .38* |
Note. The Negative Affect factor is comprised of the negative affect and negative emotionality scales. The Internalizing factor is comprised of the social phobia, separation anxiety, panic, generalized anxiety, obsessive compulsive, and depression scales. The Externalizing factor is comprised of conduct, oppositional defiant, inattention, and hyperactivity scales.
p < .01.
Table 3.
Intraclass Correlations by Zygosity and Univariate Estimates for Measured Variables [with 95% confidence intervals].
| Variable | MZ | DZ | h2 | c2 | e2 |
|---|---|---|---|---|---|
| Negative Affect | |||||
| Negative Affect | .86* | .64* | .47 [.35–.60] | .36 [.22–.50] | .14 [.12–.16] |
| Negative Emotionality | .81* | .54* | .54 [.40–.70] | .28 [.12–.43] | .19 [.16–.22] |
| Internalizing | |||||
| Social Phobia | .75* | .49* | .56 [.39–.74] | .18 [.02–.34] | .26 [.23–.31] |
| Separation Anxiety | .87* | .65* | .55 [.42–.69] | .32 [.17–.46] | .15 [.13–.18] |
| Panic | .80* | .55* | .51 [.37–.67] | .27 [.11–.41] | .22 [.19–.25] |
| Generalized Anxiety | .79* | .63* | .33 [.20–.47] | .44 [.30–.58] | .22 [.19–.26] |
| Obsessive–Compulsive | .84* | .67* | .42 [.30–.56] | .42 [.27–.55] | .18 [.15–.21] |
| Depression | .83* | .70* | .41 [.29–.54] | .44 [.31–.57] | .17 [.14–.19] |
| Externalizing | |||||
| Conduct | .93* | .56* | .73 [.60–.89] | .15 [.00–.29] | .12 [.10–.14] |
| Oppositional Defiant | .87* | .52* | .59 [.46–.74] | .24 [.09–.38] | .16 [.13–.18] |
| Inattention | .85* | .59* | .56 [.44–.71] | .28 [.13–.42] | .16 [.13–.18] |
| Hyperactivity | .89* | .57* | .69 [.55–.85] | .18 [.02–.32] | .13 [.12–.16] |
Note. MZ = monozygotic; DZ = dizygotic; h2 = genetic; c2 = shared environment; e2 = nonshared environment.
p < .01.
Biometric models were fit to transformed scores using Mx; 95% confidence intervals were used to test for significance (Neale, Boker, Xie, & Maes, 2003). Data were missing for some scale scores for between six and 56 participants due to items left unanswered by participants, and this was handled by using the Full Information Maximum Likelihood (FIML) approach. Univarite genetic (or heritability, h2), shared environmental (c2), and nonshared environmental (e2) estimates, presented in Table 3, were consistent with intraclass correlations. Each variable was found to have significant genetic, shared environmental, and nonshared environmental influences. The only exception was CD, which had a nonsignificant estimate of shared environmental effects. Univariate estimates of each factor are presented in Table 4. Results for Negative Affect, Internalizing, and Externalizing factors suggested moderate genetic and shared environmental effects. For all factors, nonshared environmental effects were low.
Table 4.
Univariate Estimates for Negative Affect, Internalizing, and Externalizing Factors [with 95% confidence intervals].
| h2 | c2 | e2 | |
|---|---|---|---|
| Negative Affect | .48 [.36–.63] | .38 [.24–.50] | .13 [.09–.17] |
| Internalizing | .39 [.26–.46] | .55 [.41–.67] | .06 [.04–.09] |
| Externalizing | .45 [.34–.49] | .54 [.41–.64] | .01 [.00–.02] |
Note. h2 = univariate genetic; c2 = univariate shared environment; e2 = univariate nonshared environment.
The main purpose of the current study was to examine the genetic and environmental influences underlying the covariation of negative affect, internalizing disorder symptoms, and externalizing disorder symptoms. This was done using a multifactorial independent pathway model, shown in Figure 1. The model fit statistics were as follows: -2 times log-likelihood = 37,931.08, df = 16159; Akaike’s Information Criterion = 5,613.08; Bayesian Information Criterion = −33,800.69. Factor loadings of the indicators on the Negative Affect, Internalizing and Externalizing factors (presented in Table 2) were moderate to high, ranging from .52 to .99 for the Negative Affect factor, .62 to .78 for the Internalizing factor, and .66 to .85 for the Externalizing factor, suggesting that the measured variables formed cohesive factors. The first set of biometric factors estimated (A1, C1, and E1; see Figure 1) in the independent pathway model represents the general genetic and environmental influences that contribute to the covariance among the Negative Affect, Internalizing and Externalizing factors. The general genetic biometric factor (A1) suggested significant (i.e., confidence interval did not include zero) shared genetic effects underlying the Negative Affect, Internalizing, and Externalizing factors (pathways .69, .34, and .30). The general shared environmental biometric factor (C1) suggested significant shared environmental effects underlying the three factors as well (pathways .42, .63, and .51). Finally, the general nonshared environmental biometric factor (E1) also suggested common nonshared environmental factors among three factors (pathways .37, .24, and .09). Results support the hypothesis that the Negative Affect, Internalizing, and Externalizing factors have common genetic, shared environmental, and nonshared environmental effects. However, the results suggest higher than expected shared environmental influences on the covariation among factors.
The second set of biometric factors (A2, C2, and E2) represent the genetic and environmental influences unique to the Negative Affect factor beyond the variance accounted for by the general biometric factors (A1, C1, and E1). As can be seen in Figure 1, the only significant pathway in the second set of biometric factors was C2 suggesting independent shared environmental effects accounting for 21% of variance (.462) in Negative Affect. The third set of biometric factors (A3, C3, and E3) represent the genetic and environmental influences unique to the Internalizing factor. Pathway A3 suggests significant independent genetic influences on the Internalizing factor, accounting for 28% of variance (.532). The fourth set of biometric factors (A4, C4, and E4) represent the genetic and environmental influences unique to the Externalizing factor. Pathways A4 and C4 were both significant, suggesting independent genetic effects accounting for 36% of the variance (.602) and independent shared environmental effects accounting for 28% of the variance (.532) in the Externalizing factor.
Discussion
Understanding the genetic and environmental influences underlying the co-occurrence of disorders may help us to understand vulnerability to psychopathology and may also shed light on developmental trajectories of psychopathology. Previous research clearly shows that internalizing and externalizing disorders covary (Angold et al., 1999; Cosgrove et al., 2011; Kessler et al., 2005; Krueger, 1999; Krueger & Markon, 2006; Krueger et al., 1998; O’Connor et al., 1998; Pesenti- Gritti et al., 2008; Rhee et al., 2007), and many have suggested that negative affect may partially account for the covariance between internalizing and externalizing disorders (Lilienfeld, 2003; Rhee et al., 2007; Tackett et al., 2011). The present study is the first to provide an examination of negative affect in relation to a wide spectrum of childhood internalizing and externalizing problems using a biometric model. This study extends prior findings of more narrowly focused associations by using a factor approach including multiple disorders and provides a comprehensive perspective of these relations. Results of the current study suggest that negative affect shares genetic and environmental influences with both internalizing and externalizing disorders in childhood. These common influences may partially explain their co-occurrence.
Several previous studies have examined the bivariate relationships between negative affect and either internalizing or externalizing behaviors (Gjone & Stevenson, 1997b; Rhee et al., 2007; Schmitz et al., 1999). Though results of these studies are not entirely consistent, jointly they demonstrate that genetic and/or shared environmental influences contribute to the covariation between negative affect and psychopathology. Results of the current study are consistent with the literature to the extent that both genetic and shared environmental influences were found to be significant contributors to the covariation between the Negative Affect, Internalizing, and Externalizing factors. The results of a study by Tackett et al. (2011) are perhaps more comparable to this study, as they include negative emotionality, an internalizing disorder, and an externalizing disorder in the same model. The results of the Tackett et al. (2011) study suggest significant genetic (for males), shared environmental, and nonshared environmental influences contributing to the covariation among negative emotionality and disorder dimensions, which is similar to the pattern of results of the current study (although the current study likely lacked power to decisively examine gender differences). Results of the current study are somewhat inconsistent with the literature in that the estimates of non-shared environmental influences are lower than those found in prior work (Rhee et al., 2007; Tackett et al., 2011). This is likely due to the use of a factor approach in the current study. An advantage of using a factor independent pathway model is that the measurement error is not included in the non-shared environmental estimates, but rather is contained in the residual variance of each manifest variable. Thus, the effects of measurement error in the biometric results are decreased, providing a better estimate of true non-shared environmental effects, which may have been overestimated in previous work.
Results of the present study were generally in line with the hypotheses, although the results suggest higher than expected shared environmental influences on the covariation between the Negative Affect, Internalizing, and Externalizing factors. As previously mentioned, the results of prior studies are mixed in terms of the significance and magnitude of shared environmental effects on childhood psychopathology. A meta-analysis by Burt (2009) offers some potential explanations. Burt’s findings suggested that different assessment methods and informants may lead to differences in estimates of genetic and environmental influences. Studies that rely on parent report rather than child report and studies that use questionnaires instead of diagnostic interviews tended to have higher shared environment estimates (Burt, 2009). Considering that the present study relied on questionnaires completed by parents it is possible that estimates of shared environmental influence in this study are inflated. Another possibility is that the magnitude of shared environmental influence is, in part, determined by the type of environment. Studies have shown higher shared environment estimates in high-risk, disadvantaged environments (Cleveland, 2003; Tuvblad, Grann & Lichtenstein, 2005). Although the present study did not specifically target families living in disadvantaged environments, the sample did include families with wide ranging incomes.
Prior studies have provided support for a ‘failure model’ in which the occurrence of an externalizing disorder (namely conduct disorder) leads to the development of an internalizing disorder, such as depression (Capaldi 1991, 1992). Results from the current study are consistent with this model such that common genetic and environmental influences, as well as negative affect, may contribute to the development of both disorders. The data from the current study were collected at one time point and, thus, could not provide information about the temporal relationship between externalizing and internalizing disorders. However, it would be useful for future studies with multiple waves of data on twins to examine the failure model more explicitly and test for genetic and environmental influences on the associations between negative affect, internalizing, and externalizing over time.
Weiss, Susser, and Catron (1998) proposed a model for characterizing common and specific features of childhood psychopathology. In this model, “common features” are those that distinguish psychopathology from normality, “broadband-specific features” are those that differentiate internalizing disorders from externalizing disorders, and “narrowband-specific features” are those that differentiate specific disorders from one another. From this framework, the present study suggests that negative affect is a “common feature,” partially accounting for the covariation between childhood internalizing and externalizing disorders (see also Lilienfeld, 2003). Future research should seek to discover other “common features” contributing to this covariation, which may include other dispositions, temperament, or personality factors. Also, in the present study the Internalizing factor had unique genetic influences and the Externalizing factor had unique genetic and shared environmental influences (after accounting for the genetic and environmental influences contributing to the covariance among the Negative Affect, Internalizing and Externalizing factors). These unique influences can be conceptualized as “broadband-specific features,” which serve to differentiate internalizing and externalizing disorders. Future research should aim to identify specifically what these unique influences are, especially for the shared environmental influences on the Externalizing factor, as identifying these influences may lead to the development of interventions.
It should be noted that although dispositions are often thought to underlie or predispose to psychopathology, the relationship is not necessarily unidirectional. Multiple models have been proposed to explain the relationship between dispositions and psychopathology (Tackett, 2006). The “vulnerability” model suggests that dispositions increase the risk for developing a particular disorder. The “complication” model suggests that the development of a disorder changes an individual’s disposition. The “exacerbation” model suggests that dispositional traits may influence the course, severity, or presentation of a disorder. Finally, the “spectrum” model suggests that dispositions and psychopathology are on a dimensional continuum. These models are not necessarily mutually exclusive (Tackett, 2006; Lonigan et al., 2011), and the results of the current study fit with both the “vulnerability” model and the “spectrum” model. However, the present study was not designed or intended to evaluate these models. It is important for future research to utilize etiologically informative, longitudinal designs to gain a better understanding of the developmental course of psychopathology.
The present study included ODD as an indicator of the Externalizing factor and did not examine the unique relationship between ODD and negative affect. However, recent research suggests that the symptoms of ODD can be divided into three dimensions, including a dimension that may have construct overlap with negative affect (Burke, Hipwell & Loeber, 2010; Stringaris & Goodman, 2009a; Stringaris & Goodman, 2009b). Specifically, Stringaris & Goodman found that ODD was comprised of Irritable, Headstrong, and Hurtful dimensions. The Irritable dimension, thought to overlap with negative affect, was predictive of internalizing disorders (Stringaris & Goodman, 2009b). Given that ODD loaded the highest on the Externalizing factor in this study, it is possible that the relationship between the Externalizing factor and the Negative Affect factor was driven by ODD (perhaps via the Irritable dimension). Although the current work focused on common variance among externalizing disorders, future work should continue to examine personality traits like Negative Affect in relation to individual externalizing disorders and their dimensional components.
As with all studies, there are important limitations that should be considered when interpreting these results. First, only parent reported data were available for the current study. Given the young age of many of the twins in this study, it is likely that parents would provide a more accurate and valid rating of negative affect and psychopathological symptoms than the twins could provide. However, as previously mentioned, the use of parent report tends to increase estimates of shared environmental influences (Burt, 2009; Hewitt, Silberg, Neale, Eaves, & Erickson, 1992). It is possible that examining teacher report or child report could result in differences in estimates of genetic and environmental influences, and thus should be investigated in future research. Second, although diagnostic interviews are typically considered the “gold standard” for the assessment of psychopathology, the present study relied on questionnaires to assess symptoms. Given that the factor structures of internalizing and externalizing disorders in the present study were similar to studies that have used interviews (Krueger et al., 1998), it suggests that the method of assessment had little effect on the results. Finally, some previous studies that have examined the effects of gender have found differences between girls and boys in terms of the genetic and environmental influences contributing to the relationship between negative affect, internalizing disorders, and externalizing disorders (Rhee et al., 2007; Tackett et al., 2011). However, analyses examining these differences in a decisive way would likely have been underpowered in the present sample, given that the investigation that was able to investigate gender differences adequately (Tackett et al., 2011) had over twice the sample size of the current study. Future research should aim to further investigate gender differences, as well as differences across other characteristics such as socioeconomic status and age. It is possible that there may be developmental changes in the relative contribution of etiological influences. For example, shared environmental influences may contribute to the covariation of negative affect, internalizing, and externalizing behaviors more at an early age, while genetic influences on the covariation may increase throughout development.
Results of the present study suggest that a child’s level of negative affect is intertwined with their risk for various disorders, including internalizing disorders like separation anxiety and depression, as well as externalizing disorders like conduct disorder and oppositional defiant disorder. Understanding that negative affect is at least one contributor to the covariation among these disorders may highlight avenues for early risk assessment, intervention, and perhaps prevention. Future research should determine the extent to which negative affect in children is malleable, and if reduced negative affect decreases the risk for developing comorbid disorders. Also, it would be beneficial to identify protective factors that might prevent children high in negative affect from developing psychopathology. It is likely that negative affect interacts with other dispositions or temperament traits, and those different combinations of traits serve as different vulnerabilities. The use of prospective research designs examining temperament traits as well as environmental factors would aid in understanding the developmental course of comorbid psychopathology in children. Finally, results of the present study suggest common genetic and environmental influences underlying negative affect, internalizing and externalizing disorders. Future research should seek to identify these underlying specific genes as well as specific environmental factors, and attempt to discover how they interact.
Acknowledgments
This research was supported, in part, by grants from the National Institute of Child Health and Human Development (P50 HD052120) and the Institute of Education Sciences, U.S. Department of Education (R305B04074). Views expressed herein are those of the authors and have neither been reviewed nor approved by the granting agencies.
Contributor Information
Amy J. Mikolajewski, Department of Psychology, Florida State University
Nicholas P. Allan, Department of Psychology, Florida State University
Sara A. Hart, Florida Center for Reading Research and Department of Psychology, Florida State University
Christopher J. Lonigan, Florida Center for Reading Research and Department of Psychology, Florida State University
Jeanette Taylor, Department of Psychology, Florida State University.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders. 4th ed text revised. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Anthony JL, Lonigan CJ, Hooe ES, Phillips BM. An affect-based, hierarchical model of temperament and its relations with internalizing symptomatology. Journal of Clinical Child and Adolescent Psychology. 2002;31:480–490. doi: 10.1207/S15374424JCCP3104_7. [DOI] [PubMed] [Google Scholar]
- Bijttebier P, Roeyers H. Temperament and vulnerability to psychopathology: Introduction to the special section. Journal of Abnormal Child Psychology. 2009;37:305–308. doi: 10.1007/s10802-009-9308-2. [DOI] [PubMed] [Google Scholar]
- Burke JD, Hipwell AE, Loeber R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:484–492. doi: 10.1097/00004583-201005000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt SA. Rethinking environmental contributions to child and adolescent psychopathology: A metaanalysis of shared environmental influences. Psychological Bulletin. 2009;135(4):608–637. doi: 10.1037/a0015702. [DOI] [PubMed] [Google Scholar]
- Buss AH, Plomin R. Temperament: Early developing personality traits. Hillsdale, NJ: Erlbaum; 1984. [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: I. Familial factors and general adjustment at grade 6. Development and Psychopathology. 1991;3:277–300. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. A 2-year follow-up at grade 8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114(4):505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Cleveland HH. Disadvantaged neighborhoods and adolescent aggression: Behavioral genetic evidence of contextual effects. Journal of Research on Adolescence. 2003;13:211–238. [Google Scholar]
- Cosgrove VE, Rhee SH, Gelhorn HL, Boeldt D, Corley RC, Ehringer MA, Hewitt JK. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescence. Journal of Abnormal Child Psychology. 2011;39(1):109–123. doi: 10.1007/s10802-010-9444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. Conduct problems, gender, and adult psychiatric outcome of children with attention-deficit hyperactivity disorder. British Journal of Psychiatry. 2002;181:416–421. doi: 10.1192/bjp.181.5.416. [DOI] [PubMed] [Google Scholar]
- Dishion TJ. Cross-setting consistency in early adolescent psychopathology: Deviant friendships and problem behavior sequelae. Journal of Personality. 2000;68:1109–1126. doi: 10.1111/1467-6494.00128. [DOI] [PubMed] [Google Scholar]
- Ebesutani C, Chorpita BF, Higa-McMillan CK, Nakamura BJ, Regan J, Lynch RE. A psychometric analysis of the revised child anxiety and depression scales – parent version in a school sample. Journal of Abnormal Psychology. 2011;39:173–185. doi: 10.1007/s10802-010-9460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C, Okamura K, Higa-McMillan C, Chorpita BF. A psychometric analysis of the positive and negative affect schedule for children-parent version in a school sample. Psychological Assessment. 2011;23:406–416. doi: 10.1037/a0022057. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. Journal of Abnormal Child Psychology. 2002;30:463–475. doi: 10.1023/a:1019864813776. [DOI] [PubMed] [Google Scholar]
- Fite PJ, Stoppelbein L, Greening L, Dhossche D. Child internalizing and externalizing behavior as predictors of age at first admission and risk for repeat admission to a child inpatient facility. American Journal of Orthopsychiatry. 2008;78:63–69. doi: 10.1037/0002-9432.78.1.63. [DOI] [PubMed] [Google Scholar]
- Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M. The Maudsley long-term follow-up of child and adolescent depression. British Journal of Psychiatry. 2001;179:210–217. doi: 10.1192/bjp.179.3.210. [DOI] [PubMed] [Google Scholar]
- Gayan J, Olson RK. Genetic and environmental influences on individual differences in printed word recognition. Journal of Experimental Child Psychology. 2003;84:97–123. doi: 10.1016/s0022-0965(02)00181-9. [DOI] [PubMed] [Google Scholar]
- Gjone H, Stevenson J. The association between internalizing and externalizing behavior in childhood and early adolescence: Genetic or environmental common influences? Journal of Abnormal Child Psycholgy. 1997a;25(4):277–286. doi: 10.1023/a:1025708318528. [DOI] [PubMed] [Google Scholar]
- Gjone H, Stevenson J. A longitudinal twin study of temperament and behavior problems: Common genetic or environmental influences? Journal of the American Academy of Child and Adolescent Psychiatry. 1997b;36(10):1448–1456. doi: 10.1097/00004583-199710000-00028. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Lemery KS. Linking temperamental fearfulness and anxiety symptoms: A behavioralgenetic perspective. Biological Psychiatry. 2000;48:1199–1209. doi: 10.1016/s0006-3223(00)01003-9. [DOI] [PubMed] [Google Scholar]
- Guerin DW, Gottfried AW, Thomas CW. Difficult temperament and behaviour problems: A longitudinal study from 1.5 to 12 years. International Journal of Behavioral Development. 1997;21(1):71–90. [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry. 2006;163(5):857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Kendler KS. Genetic and environmental sources of covariation between generalized anxiety disorder, and neuroticism. American Journal of Psychiatry. 2004;161(9):1581–1587. doi: 10.1176/appi.ajp.161.9.1581. [DOI] [PubMed] [Google Scholar]
- Hewitt JK, Silberg JL, Neale MC, Eaves LJ, Erickson M. The analysis of parental ratings of children’s behavior using LISREL. Behavior Genetics. 1992;22:293–317. doi: 10.1007/BF01066663. [DOI] [PubMed] [Google Scholar]
- Hewitt JK, Silberg JL, Rutter M, Siminoff E, Meyer JM, Maes H, Eaves LJ. Genetics and developmental psychopathology: 1. Phenotypic assessment in the Virginia twin study of adolescent behavioral development. Journal of Child Psychology and Psychiatry. 1997;38(8):943–963. doi: 10.1111/j.1469-7610.1997.tb01613.x. [DOI] [PubMed] [Google Scholar]
- Jardine R, Martin NG, Henderson AS. Genetic covariation between neuroticism and the symptoms of anxiety and depression. Genetic Epidemiology. 1984;1:89–107. doi: 10.1002/gepi.1370010202. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107(2):216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Chronis AM, Jones HA, Williams SH, Loney J, Waldman ID. Psychometric characteristics of a measure of emotional dispositions developed to test a developmental propensity model of conduct disorder. Journal of Clinical Child & Adolescent Psychology. 2008;37:794–807. doi: 10.1080/15374410802359635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Applegate B, Waldman ID. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68(2):181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ, West SG, Sandler IN. Temperament as a predictor of symptomatology in children: Addressing contamination of measures. Child Development. 1998;69(1):164–181. [PubMed] [Google Scholar]
- Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: Reflections and directions. Journal of Abnormal Child Psychology. 2003;31(3):285–291. doi: 10.1023/a:1023229529866. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Stouthamer-Loeber M. Optimal informants on childhood disruptive behaviors. Development and Psychopathology. 1989;1:317–337. [Google Scholar]
- Lonigan CJ, Phillips BM, Wilson SB, Allan NP. Temperament and anxiety in children and adolescents. In: Silverman WK, Field A, editors. Anxiety Disorders in Children and Adolescents. 2nd edition. New York, NY: Cambridge University Press; 2011. pp. 198–224. [Google Scholar]
- Lykken DT, Bouchard TJ, Jr, McGue M, Tellegen A. The Minnesota twin registry: Some initial finders. Acta Geneticae Medicate at Gemellologiae: Twin Research. 1990;39:35–70. doi: 10.1017/s0001566000005572. [DOI] [PubMed] [Google Scholar]
- McGue M, Bouchard TJ. Adjustment of twin data for the effects of age and sex. Behavior Genetics. 1984;14:325–343. doi: 10.1007/BF01080045. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication – Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidty of conduct and depressive problems at sixth grade: Substance use outcomes across adolescence. Journal of Abnormal Child Psychology. 1998;26:221–232. doi: 10.1023/a:1022676302865. [DOI] [PubMed] [Google Scholar]
- Muris P, Meesters C, Blijlevens P. Self-reported reactive and regulative temperament in early adolescence: Relations to internalizing and externalizing problem behavior and “Big Three” personality factors. Journal of Adolescence. 2007;30:1035–1049. doi: 10.1016/j.adolescence.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Muris P, Meesters C, Spinder M. Relationships between child- and parent-reported behavioural inhibition and symptoms of anxiety and depression in normal adolescents. Personality and Individual Differences. 2003;34:759–771. [Google Scholar]
- Muris P, Ollendick TH. The role of temperament in the etiology of child psychopathology. Clinical Child and Family Psychology Review. 2005;8(4):271–289. doi: 10.1007/s10567-005-8809-y. [DOI] [PubMed] [Google Scholar]
- Neale MC, Boker SM, Xie G, Maes HH. Mx: Statistical modeling. 6th ed. Richmond: Department of Psychiatry, Virginia Commonwealth University; 2003. [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Dordrecht, The Netherlands: Kluwer Academic Publishers; 1992. [Google Scholar]
- Nigg JT. Temperament and developmental psychology. Journal of Child Psychology and Psychiatry. 2006;47(3/4):395–422. doi: 10.1111/j.1469-7610.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, McGuire S, Reiss D, Hetherington EM, Plomin R. Co-occurrence of depressive symptoms and antisocial behavior in adolescence: A common genetic liability. Journal of Abnormal Psychology. 1998;107(1):27–37. doi: 10.1037//0021-843x.107.1.27. [DOI] [PubMed] [Google Scholar]
- Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug and Alcohol Dependence. 2007;88:S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Capaldi DM. A mediational model for boys’ depressed mood. In: Rolf J, Masten AS, Cicchetti D, Nuechterlein KH, Weintraub S, editors. Risk and protective factors in the development of psychopathology. New York, NY: Cambridge University Press; 1990. pp. 141–163. [Google Scholar]
- Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pesenti-Gritti P, Spatola CAM, Fagnani C, Ogliari A, Patriarca V, Stazi MA, Battaglia M. The co-occurrence between internalizing and externalizing behaviors. European Child & Adolescent Psychiatry. 2008;17:82–92. doi: 10.1007/s00787-007-0639-7. [DOI] [PubMed] [Google Scholar]
- Polier GG, Vloet TD, Herpertz-Dahlmann B, Laurens KR, Hodgins S. Comorbidity of conduct disorder symptoms and internalising problems in children: investigating a community and a clinical sample. European Child & Adolescent Psychiatry. 2012;21:31–38. doi: 10.1007/s00787-011-0229-6. [DOI] [PubMed] [Google Scholar]
- Rhee SH, Cosgrove VE, Schmitz S, Haberstick BC, Corley RC, Hewitt JK. Early childhood temperament and the covariation between internalizing and externalizing behavior in school-aged children. Twin Research and Human Genetics. 2007;10(1):33–44. doi: 10.1375/twin.10.1.33. [DOI] [PubMed] [Google Scholar]
- Rowe DC, Plomin R. Temperament in early childhood. Journal of Personality Assessment. 1977;41:150–156. doi: 10.1207/s15327752jpa4102_5. [DOI] [PubMed] [Google Scholar]
- Saudino KJ. Behavioral genetics and child temperament. Journal of Developmental and Behavioral Pediatrics. 2005;26(3):214–223. doi: 10.1097/00004703-200506000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz S, Fulker DW, Plomin R, Zahn-Waxler C, Emde RN, DeFries JC. Temperament and problem behaviour during early childhood. International Journal of Behavioral Development. 1999;23(2):333–355. [Google Scholar]
- Singh AL, Waldman ID. The etiology of associations between negative emotionality and childhood externalizing disorders. Journal of Abnormal Psychology. 2010;199(2):376–388. doi: 10.1037/a0019342. [DOI] [PubMed] [Google Scholar]
- Smith SR. Making sense of multiple informants in child and adolescent psychopathology: A guide for clinicians. Journal of Psychoeducational Assessment. 2007;25:139–149. [Google Scholar]
- Stringaris A, Goodman R. Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry. 2009a;50:216–223. doi: 10.1111/j.1469-7610.2008.01989.x. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the Academy of Child and Adolescent Psychiatry. 2009b;48:404–412. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using miltivariate statistics. 5th edn. Boston: Pearson Education; 2007. [Google Scholar]
- Tackett JL. Evaluating models of the personality-psychopathology relationship in children and adolescents. Clinical Psychology Review. 2006;26:584–599. doi: 10.1016/j.cpr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Waldman ID, Van Hulle CA, Lahey BB. Shared genetic influences on negative emotionality and major depression/conduct disorder comorbidty. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:818–827. doi: 10.1016/j.jaac.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuvblad C, Grann M, Lichtenstein P. Heritability for adolescent antisocial behavior differs with socioeconomic status: Gene-environment interaction. Journal of Child Psychology and Psychiatry. 2005;47:734–743. doi: 10.1111/j.1469-7610.2005.01552.x. [DOI] [PubMed] [Google Scholar]
- Waldman ID, Tackett JL, Van Hulle CA, Applegate B, Pardini D, Frick PJ, Lahey BB. Child and adolescent conduct disorder substantially shares genetic influences with three socioemotional dispositions. Journal of Abnormal Psychology. 2011;120(1):57–70. doi: 10.1037/a0021351. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin. 1984;96(3):465–490. [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Naragon-Gainey K. On the specificity of positive emotional dysfunction in psychopathology: Evidence from the mood and anxiety disorders and schizophrenia/schizotypy. Clinical Psychology Review. 2010;30:839–848. doi: 10.1016/j.cpr.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss B, Susser K, Catron T. Common and specific features of childhood psychopathology. Journal of Abnormal Psychology. 1998;107(1):118–127. doi: 10.1037//0021-843x.107.1.118. [DOI] [PubMed] [Google Scholar]