Abstract
Objective
To evaluate the effect of hysterosalpingo-contrast sonography (HyCoSy) on natural conception in the infertile patient.
Methods
We conducted a prospective observational study recruiting 180 patients admitted to Infertility Center of Ferrara University from January 2010 to February 2012. The essential inclusion criteria was the couple's desire to perform only diagnostic evaluation on infertility causes and to wait for natural conception before proceeding with further management. Couples were investigated with hormonal profile, semen analysis and HyCoSy. Expected time for spontaneous pregnancy was 180 days from HyCoSy. First datation sonography of pregnancy was used calculating time elapsed from HyCoSy at conception.
Results
Forty patients (22.2%) obtained spontaneous pregnancy within 6 months after HyCoSy. The mean of "conception time" was 75 days. The pregnancy rate was significantly higher in the first 30 days (45%) compared to other the months of observation (p<0.0005). Multiple linear regression analysis showed that maternal age and sterility duration proved independent variables in detecting the "conception time" after HyCoSy (t=3.742, p=0.001, t=2.371, p=0.02, respectively).
Conclusion
A possible beneficial effect of HyCoSy is feasible especially in the days following its execution. This temporal correlation supports its therapeutic use.
Keywords: Fallopian tubes, Hysterosalpingography, Sterility, Sonography, Human
Introduction
Infertility is a common reproductive health problem defined as the failure to achieve a clinical pregnancy after one year or more of unprotected, regular sexual intercourses (according to World Health Organization [WHO]). It affects approximately over 15% of couples of reproductive age [1]. Infertility etiology is multifactorial, but in one-third of the cases it is caused by a female factor. Tubal pathology is a common cause of female infertility (14% of couples who require specialist treatment) [2]. Fallopian tubes are important for fertility because they transport gametes and embryos, allow the timely passage of the embryo to the uterus and have an essential role in its early development. For this reason, tubal examination plays a primary role in the study of infertile couples and it is indispensable before starting assisted reproductive techniques (ART) like intrauterine insemination and IVF [3]. The tests now available for the evaluation of the morphology of the uterus and fallopian tubes patency are hysterosalpingography (HSG), laparoscopy and hysterosalpingo-contrast sonography (HyCoSy).
In the past, over 50 years ago, many doctors noticed an increased incidence of spontaneous pregnancies soon after diagnostic tests of tubal patency (HSG and laparoscopy) [4-6]. This positive effect of tubal examinations is probably due to a mechanical action of the fluid. The passage of liquid through tubal lumen removes the buildup of material inside the tubes after inflammatory processes, like microadhesions and flushes inspissated mucus plug that can hamper fecundation. For some years, HyCoSy is the first-line diagnostic test for determining tubal patency and evaluating the uterine cavity by transvaginal ultrasound and the introduction of saline solution mixed with air into the uterine cavity and the Fallopian tubes. This investigation is safe for absence of radiation, well tolerated, quick, simple and economic [7].
The objective of this study was to describe the effect of HyCoSy on the pregnancy rate (PR) correlated to the time elapsed between the examination and the conception.
Methods
1. Patients selection
We conducted a prospective observational study on the possible therapeutic effect of HyCoSy in the study of infertile couples from January 2010 to February 2012. Patients were recruited by the Infertility Center of the Obstetric and Gynecological Clinic, Ferrara University, Italy. The inclusion criteria were: unexplained sterility, age between 25 and 40 years, infertility by at least 1 year, couple's desire to perform only diagnostic evaluation on infertility causes and to wait for natural conception before proceeding with further management. The exclusion criteria were serious semen abnormalities, bilateral tubal occlusion, recurrent spontaneous abortion, FSH>15 mIU/mL and suspected anovulation (menstrual period>35 days). The risk factors considered were: previous pelvic surgery, endometriosis, smoking and endocrine diseases.
A complete medical history was obtained and clinical examination made on both partners. Couples were investigated with hormonal profile at third day of the menstrual cycle, semen analysis performed using the WHO 2010 guidelines [8] and HyCoSy. Patients were given with appropriate information on the objectives and implications of the tests to establish a particular cause of infertility. Written informed consent was obtained from all study subjects. The Ethic Committee of Ferrara University approved our study. Expected time for spontaneous pregnancy was 180 days from HyCoSy. First datation sonography of pregnancy was used calculating time elapsed from HyCoSy at conception ("conception time"). Then, patients were subdivided in two groups: group A, patients with natural conception; group B, non-pregnant patients.
2. Hysterosalpingo-contrast sonography
HyCoSy was performed in the preovulatory phase (between days 5 and 10) of the menstrual cycle. Firstly a transvaginal scan of the ovaries, tubes and uterus was performed using a 7 MHz probe (Aloka Prosound Ssd3500sx, Tokyo, Japan) for excluding hydrosalpix and other contraindications to the use of ultrasound contrast medium.
The vulva and cervix were prepared with disinfecting solution for work in aseptic conditions for preventing ascending infections. A small transcervical catheter was inserted into the endocervical canal and fixed by balloon to secure its position. About ten-milliliter saline solution with air was injected through the catheter into the uterine cavity and the tubes during transvaginal ultrasound scanning. Tubes were considered patent when there was the visualization of continuous flow of contrast medium in the fallopian tube for many seconds and/or it spilled from the fimbrial into peritoneal cavity.
3. Statistical analysis
All data obtained from the cases were analyzed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) for Windows program. A t-test was used for continuous variables and chi-square for categorical variables, Pearson test for assessing the correlation of the factors with the "conception time". Linear regression analysis was used for identifying independent variables while logistic regression analysis for identifying the variables correlated with spontaneous pregnancy. A value of p<0.05 was regarded as statistically significant.
Results
The whole study population was composed of 180 patients of whom 40 with natural conception (group A) and 140 non-pregnant women (group B). The PR was 22.2% within 6 months after HyCoSy; among the 40 pregnancies of group A three (7.5%) ended in early spontaneous abortions (within the 6th week of gestation) and one (2.5%) had an ectopic implantation.
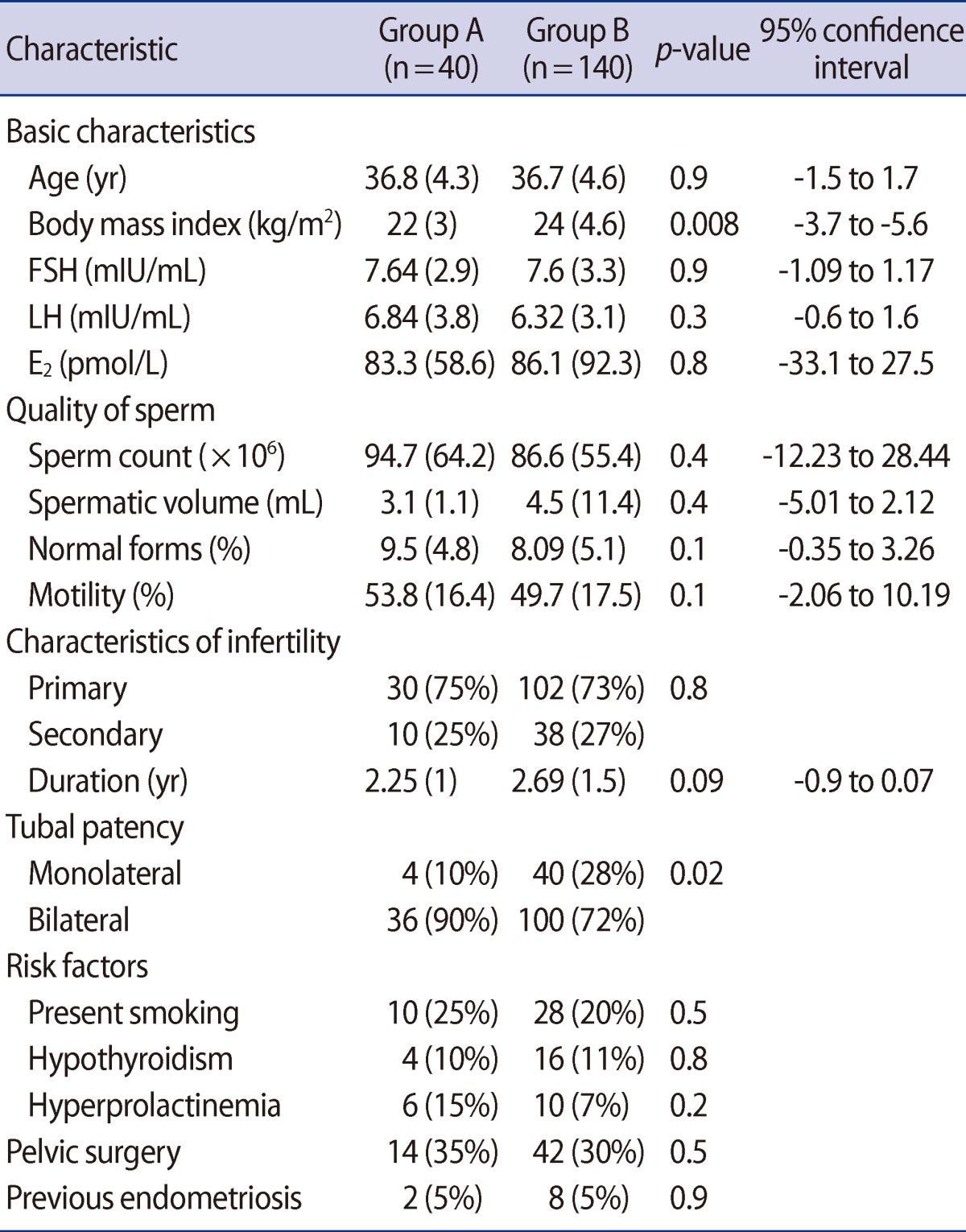
The basal characteristics of the patients were homogenous between the two groups. Mean age was 36.8 years in group A and 36.7 years in group B (p<0.9; 95% confidence interval [CI], -1.5 to 1.7). The sterility duration was 2.25 and 2.69 respectively in group A and B (p=0.09; 95% CI, -0.9 to 0.07); even if absolute value was different, it wasn't statistical significant. Primary infertility was present in 30 patients in group A (75%) and in 102 patients in group B (73%) therefore the difference was not significant (p=0.8). The hormonal profile in the women and the quality of semen did not show any difference (Table 1). Only body mass index (BMI) (p<0.008; 95% CI, -3.7 to -5.6) was significantly different between the two groups. All considered risk factors were comparable between two groups (Table 1). HyCoSy showed a bilateral tubal patency in 36 patients in group A (90%) and in 100 patients in group B (72%) with a statistically significant difference (p<0.02) (Table 1).
Table 1.
General characteristics between the two groups
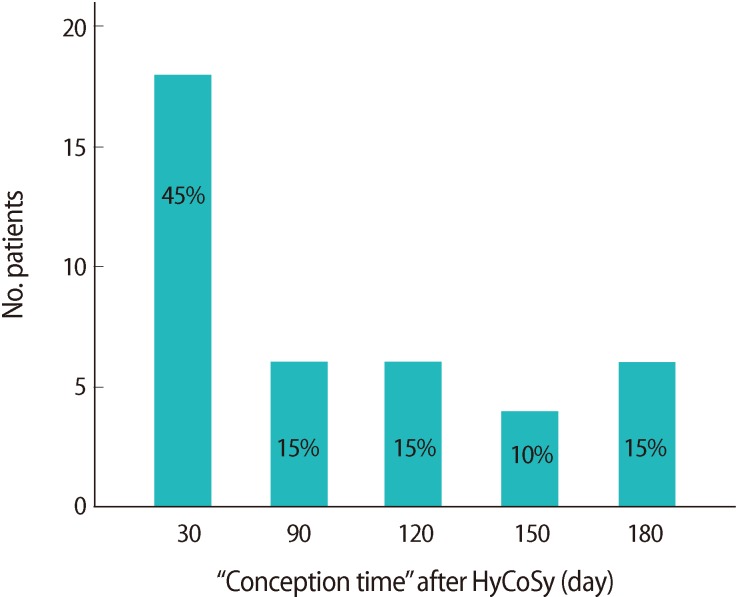
The mean of "conception time" was 75 days. The PR was significantly higher in the first 30 days (45%) compared to other the months of observation (p<0.0005) (Figure 1).
Figure 1.
"Time conception" in the study population. HyCoSy, hysterosalpingo-contrast sonography.
The Pearson test assessing the correlation between the "conception time" and the variables considered, showed a:
Moderate, significant positive correlation with women's age (r, 0.427; p<0.006);
Moderate, significant positive correlation with the value of FSH (r, 0.450; p<0.004);
Moderate, significant positive correlation with the duration of sterility (r, 0.442; p<0.004).
It is interesting to note the significant negative correlation between the sperm counts and the duration of sterility (r, -0.548; p=0.000).
Multiple linear regression analysis showed that age and duration of sterility proved independent variables in detecting the "conception time" after HyCoSy (t=3.742, p=0.001, t=2.371, p=0.02, respectively), while the FSH value was not statistically significant (t=1.898, p=0.06).
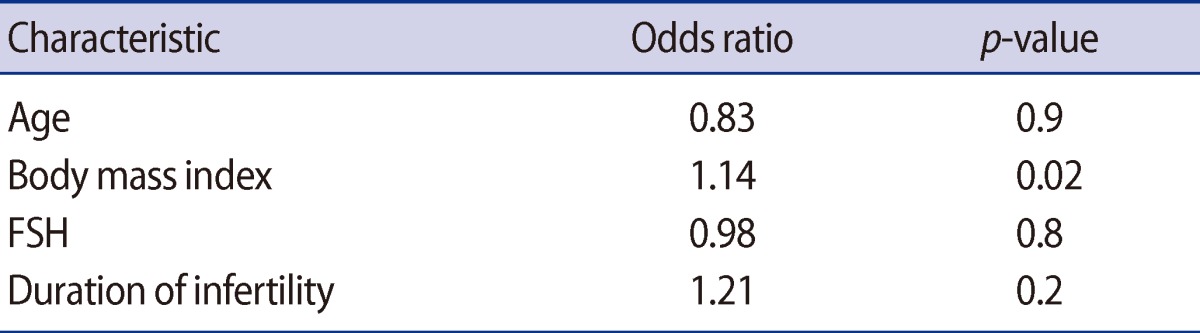
Finally, logistic regression analysis showed that the BMI was the only independent variable able to influence the pregnancy rate between the two groups (odds ratio [OR], 1.14; p=0.02) (Table 2).
Table 2.
Results of logistic regression analysis in determining the variables influencing the pregnancy rate
Discussion
The possible therapeutic effect of tubal patency test has been debated for about half century; nevertheless we are not able to quantify its efficacy yet. Several reports have been published throughout the years showing an increased PR after HSG. In 1966, Wahby et al. [4] reported an 25% to 40% incidence of pregnancy after HSG in couples with unexplained infertility. Recently Nugent et al. [5] have compared couples undergoing examination by instillation of oil-soluble contrast media with untreated couples. In the first group, over the 20% of clinical spontaneous pregnancy was observed, and no pregnancy was reported in the untreated women after six months from examination. Finally, Cochrane review of several randomized trials confirmed that tubal flushing versus no intervention was in relation to significant increase in the odds of pregnancy and live birth [9]. In the past, for increasing the therapeutic effectiveness of the passage of the liquid into the tubes, many gynecologists injected, besides saline solution and air, drugs (like corticosteroids and antibiotics), through a catheter inserted inside the uterine cavity. This technique is called medicated-hydrotubation [10].
Nowadays, these techniques are less used because ART obtains higher PRs. However, the tubal patency test is essential in the evaluation of the infertile couple. In this view, several studies showed that the efficacy of HyCoSy is comparable to HSG [11]. Moreover HSG has several side effects as exposure to radiation, potential severe adverse contrast reaction [12,13]. In consideration of this, HyCoSy is the first level tubal patency test available today [14].
From these considerations derived our desire to describe the possible therapeutic action of a diagnostic test that is essential in the evaluation of couples that are admitted to our center for the study of infertility.
The first data to analyze is the PR (22.2%) in the whole study population. This result is evident because such a high percentage of spontaneous pregnancy cannot be considered accidental; also the highest number of patients with bilateral tubal patency in group A supports this hypothesis (90% in group A vs. 72% in group B, p=0.02) pointing to importance of tubal factor.
Possible confounders may be excluded because the characteristics of the patients in the two groups (age, hormonal profile, quality of semen, duration of sterility, risk factors) were homogenous. The only significantly different factor between two groups was the BMI (p<0.008); however it was still less than 24 (Table 1). For quantifying the therapeutic effect of HyCoSy it is necessary to correlate the PR with the "conception time". This correlation is very interesting because 18 pregnancies began within the first 30 days (45%) after HyCoSy with a highly significant difference (p<0.005) compared to the remaining 22 pregnancies that had a homogeneous distribution in the following months (Figure 1). This result confirmed the role of HyCoSy favoring spontaneous pregnancy during the same menstrual cycle in which it has been carried out.
The factor "Conception Time" had a positive correlation with age, FSH values and duration of sterility. In particular age and duration of sterility were independent variables representing the better variables to determine a good response to HyCoSy.
These results confirm the importance of ovarian reserve to predict spontaneous pregnancy. Nevertheless, the male factor is equally important, indeed we should remember the negative correlation between the sperm counts and the duration of infertility.
However after logistic regression analysis the only variable able to determine the PR in the whole study population was BMI (p=0.01; OR, 1.14) (Table 2).
The impact of obesity on female fertility is well known [15] even though the question has always been discussed referring to the different fertility among women with high and normal BMI considering 25 as threshold value.
On the contrary, in our study BMI was determinant even if it was normal (<25) in both groups.
Therefore, also small changes in BMI may be crucial to improve PR and then it could not be sufficient to consider 24 as the threshold of BMI in infertile women but a narrower range should be defined.
The hypothesis of a beneficial action of HyCoSy on the natural conception seems strong especially in the days following its execution. This temporal correlation raises interesting questions: is right limit the effect of HyCoSy to one mechanical factor? Is there some sophisticated physiological mechanism at the base of this?
For instance, it could be to hypothesize a role of HyCoSy in inducing ovulation? If these assumptions were verified, HyCoSy could become a real therapeutic tool to be used in the best menstrual period for each patient thus improving the success rate. This could be particularly helpful when couples prefer a natural conception and ART are excessive and expensive. These questions deserve to be solved and should lead us to improve research.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–1524. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Das S, Nardo LG, Seif MW. Proximal tubal disease: the place for tubal cannulation. Reprod Biomed Online. 2007;15:383–388. doi: 10.1016/s1472-6483(10)60362-8. [DOI] [PubMed] [Google Scholar]
- 3.ESHRE Capri Workshop Group. Diagnosis and management of the infertile couple: missing information. Hum Reprod Update. 2004;10:295–307. doi: 10.1093/humupd/dmh024. [DOI] [PubMed] [Google Scholar]
- 4.Wahby O, Sobrero AJ, Epstein JA. Hysterosalpingography in relation to pregnancy and its outcome in infertile women. Fertil Steril. 1966;17:520–530. doi: 10.1016/s0015-0282(16)36010-1. [DOI] [PubMed] [Google Scholar]
- 5.Nugent D, Watson AJ, Killick SR, Balen AH, Rutherford AJ. A randomized controlled trial of tubal flushing with lipiodol for unexplained infertility. Fertil Steril. 2002;77:173–175. doi: 10.1016/s0015-0282(01)02925-9. [DOI] [PubMed] [Google Scholar]
- 6.Lindborg L, Thorburn J, Bergh C, Strandell A. Influence of HyCoSy on spontaneous pregnancy: a randomized controlled trial. Hum Reprod. 2009;24:1075–1079. doi: 10.1093/humrep/den485. [DOI] [PubMed] [Google Scholar]
- 7.Luciano DE, Exacoustos C, Johns DA, Luciano AA. Can hysterosalpingo-contrast sonography replace hysterosalpingography in confirming tubal blockage after hysteroscopic sterilization and in the evaluation of the uterus and tubes in infertile patients? Am J Obstet Gynecol. 2011;204:79.e1–79.e5. doi: 10.1016/j.ajog.2010.08.065. [DOI] [PubMed] [Google Scholar]
- 8.Cao XW, Lin K, Li CY, Yuan CW. A review of WHO laboratory manual for the examination and processing of human semen (5th edition) Zhonghua Nan Ke Xue. 2011;17:1059–1063. [PubMed] [Google Scholar]
- 9.Luttjeboer F, Harada T, Hughes E, Johnson N, Lilford R, Mol BW. Tubal flushing for subfertility. Cochrane Database Syst Rev. 2007;(3):CD003718. doi: 10.1002/14651858.CD003718.pub3. [DOI] [PubMed] [Google Scholar]
- 10.Chenia F, Hofmeyr GJ, Moolla S, Oratis P. Sonographic hydrotubation using agitated saline: a new technique for improving fallopian tube visualization. Br J Radiol. 1997;70:833–836. doi: 10.1259/bjr.70.836.9486049. [DOI] [PubMed] [Google Scholar]
- 11.Hamed HO, Shahin AY, Elsamman AM. Hysterosalpingo-contrast sonography versus radiographic hysterosalpingography in the evaluation of tubal patency. Int J Gynaecol Obstet. 2009;105:215–217. doi: 10.1016/j.ijgo.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Simpson WL, Jr, Beitia LG, Mester J. Hysterosalpingography: a reemerging study. Radiographics. 2006;26:419–431. doi: 10.1148/rg.262055109. [DOI] [PubMed] [Google Scholar]
- 13.Noorhasan D, Heard MJ. Gadolinium radiologic contrast is a useful alternative for hysterosalpingography in patients with iodine allergy. Fertil Steril. 2005;84:1744. doi: 10.1016/j.fertnstert.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 14.Saunders RD, Shwayder JM, Nakajima ST. Current methods of tubal patency assessment. Fertil Steril. 2011;95:2171–2179. doi: 10.1016/j.fertnstert.2011.02.054. [DOI] [PubMed] [Google Scholar]
- 15.Zain MM, Norman RJ. Impact of obesity on female fertility and fertility treatment. Womens Health (Lond Engl) 2008;4:183–194. doi: 10.2217/17455057.4.2.183. [DOI] [PubMed] [Google Scholar]