Abstract
Heterotopic pregnancy is rare event and the risk is increased with assisted reproductive technology procedures. Heterotopic cervical pregnancy is even more unusual. We report a rare case of heterotopic cervical pregnancy that was managed successfully. A 36-year-old women who conceived by IVF-ICSI was diagnosed with heterotopic cervical pregnancy. She visited the emergency room with vaginal bleeding at 5 weeks of gestation and underwent careful intracervical gestational sac reduction with forceps under abdominal guidance the next day. The postoperative course was uneventful and with regular check-ups, the intrauterine pregnancy (IUP) progressed unremarkably through 41 weeks with delivery of a healthy newborn. We reviewed a total of 37 cases of heterotopic pregnancy that have been reported in the English language literature. There have been many attempts to eliminate the cervical embryo while preserving the IUP, and complete cervical evacuation is important in order to avoid infection, bleeding, and premature birth.
Keywords: Cervical pregnancy, Heterotopic pregnancy, Selective fetal reduction
Introduction
Heterotopic pregnancy is a very rare condition. Whereas the incidence has increased from 1 in 10,000-50,000 spontaneous pregnancies, with assisted reproductive technology procedures, the incidence is up to 1%, a 70-fold increased risk [1,2]. Heterotopic cervical pregnancy is even more unusual. There are several approaches for heterotopic cervical pregnancy management, and generally the purpose of conservative management is fertility preservation: surgical treatments including uterine artery ligation and embolization, Foley catheter insertion, and cervical curettage with or without cerclage, while medical treatments include transvaginal potassium chloride (KCl) or methotrexate (MTX) injection. In 1994, Frates et al. [3] reported the first live birth of a heterotopic cervical pregnancy, which was managed with transvaginal ultrasound-guided selective reduction with KCl. Since then, a few more live births from heterotopic cervical pregnancy have been reported.
We present the case of a rare event of a heterotopic pregnancy in which it was possible to maintain the intrauterine pregnancy (IUP) to term without complications and reviewed the literature to suggest the best treatment for a successful pregnancy outcome.
Case report
A 36-year-old woman visited our medical center to seek treatment for primary infertility. At her first visit, transvaginal sonography revealed multiple uterine fibroids. Dilatation and curettage was performed due to a missed abortion that was conceived by the first cycle of IVF-ET. In this cycle, a total of seven oocytes were retrieved, five oocytes were fertilized by intracytoplasmic sperm injection, and two embryos were transferred. The initial serum b-hCG level was 191.44 mIU/mL 11 days after embryo transfer, and follow-up levels were 1,540 mIU/mL and 7,970 mIU/mL at 15 days and 18 days after ET, respectively. At 4 weeks and 5 days of gestation, an 8 mm gestational sac with a yolk sac was seen in the intrauterine cavity and a 3 mm gestational sac-like shadow was seen in the cervical canal in the first TVS (Figure 1A). Two days later, she visited the emergency room with vaginal bleeding. The patient was hemodynamically stable at the time of presentation (hemoglobin 11.5 g/dL). At 5 weeks+2 days of gestation, follow-up sonography confirmed a heterotopic cervical pregnancy (Figure 1B-D).
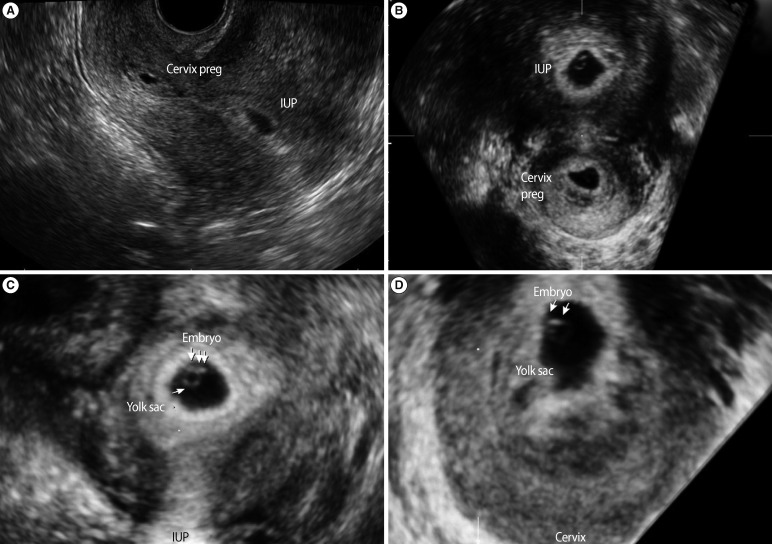
Figure 1.
(A) Transvaginal ultrasonography showed a cervical and intrauterine pregnancy simultaneously at 4 weeks+5 days of gestation. (B) Preoperative follow-up imaging at 5 weeks+2 days of gestation. Two gestational sacs were confirmed. (C) One sac in the uterine cavity, measuring 13.5 mm with a live fetus (crown-rump length measuring 3 mm with fetal heartbeat). (D) Another sac in the uterine cervix, measuring 9.6 mm with yolk sac and fetal pole and equivocal fetal heart tones. IUP, intrauterine pregnancy; cervix preg, cervical pregnancy.
After explaining the treatment options to the patient, she wanted to try to conserve the IUP. She decided on transvaginal pregnancy reduction of the cervical pregnancy, accepting the risk of severe bleeding and a potential need for emergency hysterectomy.
Selective reduction of the cervically located gestational sac was planned, with readiness for hysterectomy. Careful intracervical gestational sac reduction without harming the endometrial area was carried out with ovum forceps under abdominal ultrasound guidance. Massive uterine bleeding did not occur. Microscopic findings demonstrated trophoblast and chorionic villi in the evacuated tissue. The postoperative course was uneventful with a postoperative hemoglobin level of 11.3 g/dL. The patient was discharged on the seventh postoperative day in good health, with an intact IUP (Figure 2).
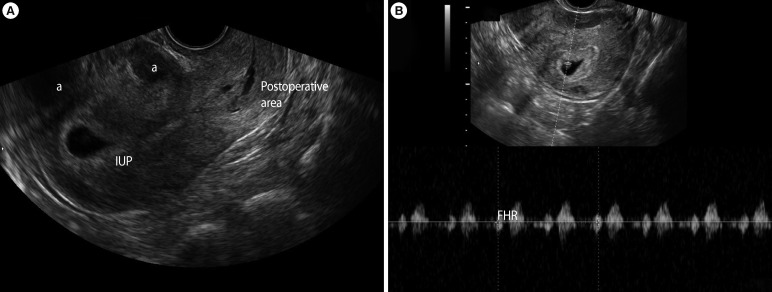
Figure 2.
Postoperative vaginal ultrasonography on the seventh postoperative day (6 weeks+1 days of gestation). (A) A hypervascular echogenic change was shown in the cervical area, whereas the intrauterine pregnancy continued. (B) The heartbeat was positive and biometrics were consistent with the gestational age. IUP, intrauterine pregnancy; FHR, fetal heart rate. aUterine fibroid.
With regular check-ups, the IUP followed without any complications, and an emergency Cesarean section was performed at 40 weeks+5 days of gestation due to failure to progress. An uncomplicated birth of a live newborn weighing 3,360 g occurred; the Apgar scores were 8 and 9 at 1 and 5 minutes, respectively. Written informed consent was obtained from the patient for publication of this case report and the accompanying images, and this report was approved by the Institutional Review Board of CHA Gangnam Medical Center.
Discussion
Heterotopic cervical pregnancy is extremely rare and most cases are associated with assisted reproductive technology. This condition is usually diagnosed by bleeding and transvaginal ultrasound. Early diagnosis of heterotopic cervical pregnancy can provide the opportunity for successful conservative management. In general, the aims of a conservative approach are the protection of a coexisting IUP, the minimization of blood loss, and fertility preservation. However, there are no specific recommendations for the best treatment of heterotopic cervical pregnancy, and there is no universally accepted treatment modality. Therefore, we reviewed the literature to identify the best treatment of heterotopic cervical pregnancy for a successful pregnancy outcome.
Up to the present, a total of 37 cases of heterotopic cervical pregnancy, including the one described here, have been reported in the English language literature. Only four cases of heterotopic cervical pregnancy had been conceived spontaneously and naturally [4-7]: the other patients had received infertility treatment. In the 30 cases in which preserving the IUP was attempted, the attempt was successful in 25 cases: 24 were live births, but one case was followed up to 12 weeks of gestational age and in 5 cases, intrauterine fetal demise occurred. Among the 24 live births, the cases are classified according to the absence or presence of major obstetric complications in Tables 1 and 2, respectively. In 16 cases, the IUP was preserved and followed up until birth without any complications (Table 1). On the other hand, the IUP was preserved with major obstetric complications including placenta accreta, severe bleeding, and subsequent hysterectomy in eight cases (Table 2). Different techniques were attempted to eliminate the cervical embryo. Among them, the following factors should be considered.
Table 1.
An overview of the 16 cases with complication-free live births
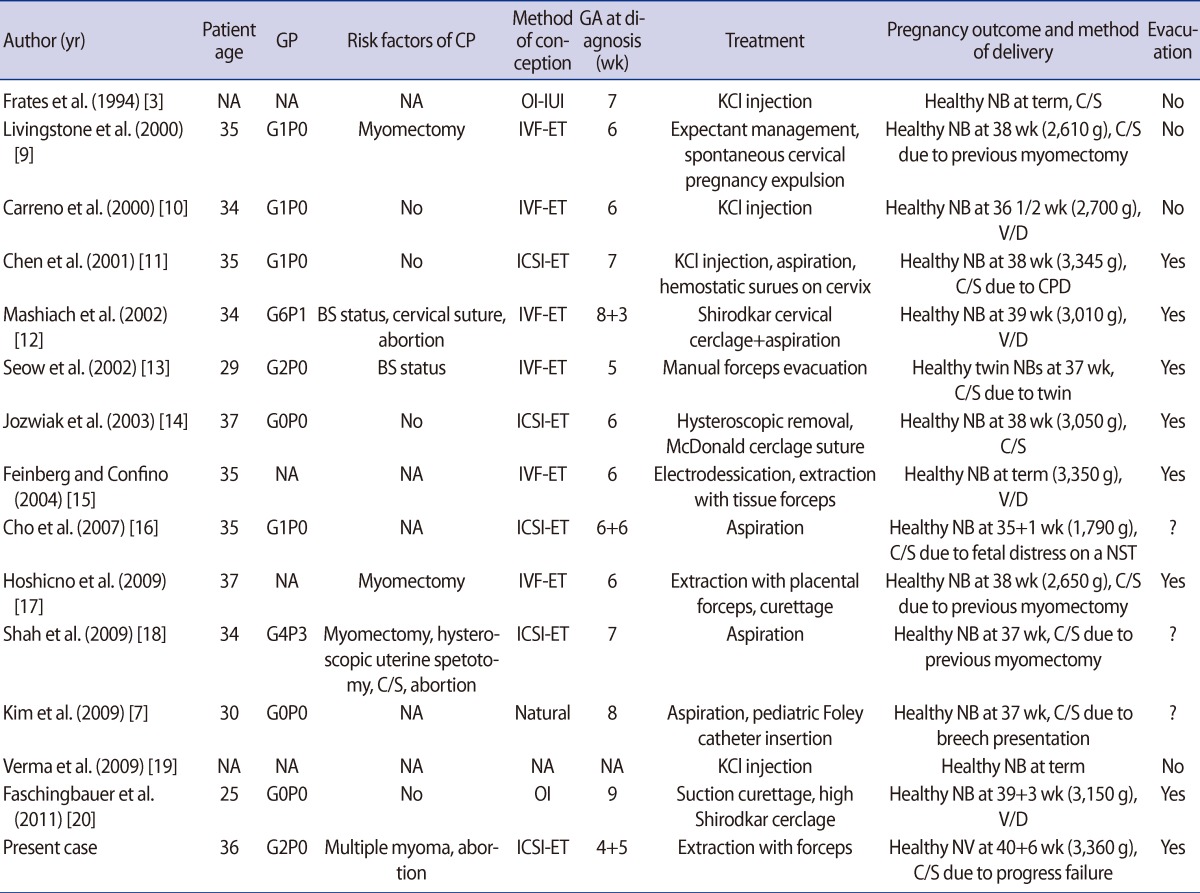
GP, gravid and parity; CP, cervical pregnancy; GA, gestational age; NA, not available; OI, ovulation induction; IUI, intrauterine insemination; KCl, potassium chloride; NB, newborn; C/S, Cesarean section; MTX, methotrexate; PROM, premature rupture of membrane; V/D, vaginal delivery; CPD, cephalopelvic disproportion; BS; bilateral salpingectomy; NST, nonstress test.
Table 2.
An overview of the eight cases with complicated live births
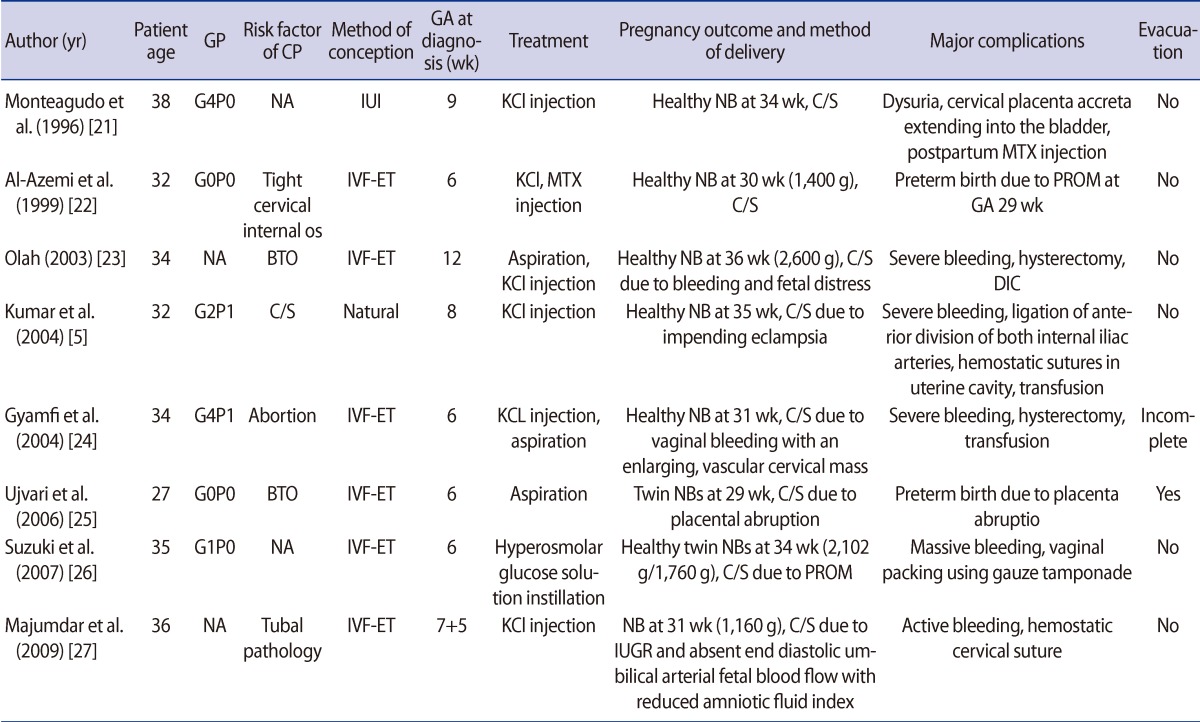
GP, gravid and parity; CP, cervical pregnancy; GA, gestational age; NA, not available; IUI, intrauterine insemination; KCl, potassium chloride; NB, newborn; C/S, Cesarean section; MTX, methotrexate; PROM, premature rupture of membrane; BTO, bilateral tubal obstruction; DIC, disseminated intravascular coagulopathy; IUGR, intrauterine growth retardation.
MTX is an agonist of folic acid that participates in DNA synthesis and has the capacity to stop proliferative cell activity. Transvaginal ultrasound-guided intra-amniotic injection of MTX can be successfully used for cervical pregnancy treatment, but the risk of systemic adverse effects, such as thrombocytopenia, leukopenia, elevated serum liver enzymes, and especially the teratogenic effect, should be taken into consideration. Angiographic arterial embolization has also been used. However, this technique may result in the radiation of the viable IUP, and influence on endometrial receptivity, which could decrease future fertility [8]. Although several cases have been managed by KCl injection, there is a possibility of major bleeding because of the remaining products of conception.
If chorionic tissue remains in the cervix, bleeding, cervical mass infection that could cause intrauterine infection, premature rupture of the membrane, and postpartum bleeding can sometimes occur, and placenta accreta remains a risk because of the possibility of chorionic infiltration to the cervix. In this literature review, 58.3% (7 out of 12) of the cases developed serious complications when evacuation was not performed, regardless of the initial procedure, while 91.7% (11 out of 12) whose treatment included complete evacuation of the cervical pregnancy had no major complications. In fact, the complication of the other one case was placenta abruption, which might not have been associated with remnant chorionic tissue in the cervix. Therefore, careful complete cervical evacuation is important to management of heterotopic cervical pregnancy.
We described a case of heterotopic cervical pregnancy that was successfully treated and reviewed the literature. Although a general treatment strategy cannot be suggested because of the small number of cases, complete removal of the cervical conception should be considered for a successful pregnancy outcome.
Footnotes
This study was supported by a grant (A084923) of the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea.
References
- 1.Molloy D, Deambrosis W, Keeping D, Hynes J, Harrison K, Hennessey J. Multiple-sited (heterotopic) pregnancy after in vitro fertilization and gamete intrafallopian transfer. Fertil Steril. 1990;53:1068–1071. doi: 10.1016/s0015-0282(16)53587-0. [DOI] [PubMed] [Google Scholar]
- 2.Lemus JF. Ectopic pregnancy: an update. Curr Opin Obstet Gynecol. 2000;12:369–375. doi: 10.1097/00001703-200010000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Frates MC, Benson CB, Doubilet PM, Di Salvo DN, Brown DL, Laing FC, et al. Cervical ectopic pregnancy: results of conservative treatment. Radiology. 1994;191:773–775. doi: 10.1148/radiology.191.3.8184062. [DOI] [PubMed] [Google Scholar]
- 4.Porpora MG, D'Elia C, Bellavia M, Pultrone DC, Cosmi EV. Heterotopic cervical pregnancy: a case report. Acta Obstet Gynecol Scand. 2003;82:1058–1059. doi: 10.1034/j.1600-0412.2003.00069.x. [DOI] [PubMed] [Google Scholar]
- 5.Kumar S, Vimala N, Dadhwal V, Mittal S. Heterotopic cervical and intrauterine pregnancy in a spontaneous cycle. Eur J Obstet Gynecol Reprod Biol. 2004;112:217–220. doi: 10.1016/s0301-2115(03)00337-3. [DOI] [PubMed] [Google Scholar]
- 6.Matteo M, Nappi L, Rosenberg P, Greco P. Combined medical-hysteroscopic conservative treatment of a viable cervical pregnancy: a case report. J Minim Invasive Gynecol. 2006;13:345–347. doi: 10.1016/j.jmig.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Kim MG, Shim JY, Won HS, Lee PR, Kim A. Conservative management of spontaneous heterotopic cervical pregnancy using an aspiration cannula and pediatric Foley catheter. Ultrasound Obstet Gynecol. 2009;33:733–734. doi: 10.1002/uog.6363. [DOI] [PubMed] [Google Scholar]
- 8.Tan G, Guo W, Zhang B, Xiang X, Chen W, Yang J. Temporary reduction and slow recovery of integrin alphanubeta3 in endometrium after uterine arterial embolization. Eur J Obstet Gynecol Reprod Biol. 2012;160:66–70. doi: 10.1016/j.ejogrb.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 9.Livingstone M, Jansen RP, Anderson JC. Spontaneous miscarriage of a cervical pregnancy and continuation of intra-uterine pregnancy following in vitro fertilisation and embryo transfer. Aust N Z J Obstet Gynaecol. 2000;40:464–465. doi: 10.1111/j.1479-828x.2000.tb01184.x. [DOI] [PubMed] [Google Scholar]
- 10.Carreno CA, King M, Johnson MP, Yaron Y, Diamond MP, Bush D, et al. Treatment of heterotopic cervical and intrauterine pregnancy. Fetal Diagn Ther. 2000;15:1–3. doi: 10.1159/000020967. [DOI] [PubMed] [Google Scholar]
- 11.Chen D, Kligman I, Rosenwaks Z. Heterotopic cervical pregnancy successfully treated with transvaginal ultrasound-guided aspiration and cervical-stay sutures. Fertil Steril. 2001;75:1030–1033. doi: 10.1016/s0015-0282(01)01746-0. [DOI] [PubMed] [Google Scholar]
- 12.Mashiach S, Admon D, Oelsner G, Paz B, Achiron R, Zalel Y. Cervical Shirodkar cerclage may be the treatment modality of choice for cervical pregnancy. Hum Reprod. 2002;17:493–496. doi: 10.1093/humrep/17.2.493. [DOI] [PubMed] [Google Scholar]
- 13.Seow KM, Hwang JL, Tsai YL, Lin YH, Hsieh BC, Huang SC. Transvaginal colour Doppler diagnosis and assessment of a heterotopic cervical pregnancy terminated by forceps evacuation following in vitro fertilisation and embryo transfer. BJOG. 2002;109:1072–1073. doi: 10.1111/j.1471-0528.2002.01080.x. [DOI] [PubMed] [Google Scholar]
- 14.Jozwiak EA, Ulug U, Akman MA, Bahceci M. Successful resection of a heterotopic cervical pregnancy resulting from intracytoplasmic sperm injection. Fertil Steril. 2003;79:428–430. doi: 10.1016/s0015-0282(02)04662-9. [DOI] [PubMed] [Google Scholar]
- 15.Feinberg E, Confino E. Electrodessication of a cervical heterotopic pregnancy. Fertil Steril. 2004;82:448–449. doi: 10.1016/j.fertnstert.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 16.Cho JH, Kwon H, Lee KW, Han WB. Cervical heterotopic pregnancy after assisted reproductive technology successfully treated with only simple embryo aspiration: a case report. J Reprod Med. 2007;52:250–252. [PubMed] [Google Scholar]
- 17.Hoshino T, Kita M, Imai Y, Kokeguchi S, Shiotani M. Successful pregnancy outcome in a case of heterotopic intrauterine and cervical pregnancy and a literature review. J Obstet Gynaecol Res. 2009;35:1115–1120. doi: 10.1111/j.1447-0756.2009.01071.x. [DOI] [PubMed] [Google Scholar]
- 18.Shah AA, Grotegut CA, Likes CE, 3rd, Miller MJ, Walmer DK. Heterotopic cervical pregnancy treated with transvaginal ultrasound-guided aspiration resulting in cervical site varices within the myometrium. Fertil Steril. 2009;91:934.e19–934.e22. doi: 10.1016/j.fertnstert.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Verma U, Goharkhay N. Conservative management of cervical ectopic pregnancy. Fertil Steril. 2009;91:671–674. doi: 10.1016/j.fertnstert.2007.12.054. [DOI] [PubMed] [Google Scholar]
- 20.Faschingbauer F, Mueller A, Voigt F, Beckmann MW, Goecke TW. Treatment of heterotopic cervical pregnancies. Fertil Steril. 2011;95:1787.e9–1787.e13. doi: 10.1016/j.fertnstert.2010.10.043. [DOI] [PubMed] [Google Scholar]
- 21.Monteagudo A, Tarricone NJ, Timor-Tritsch IE, Lerner JP. Successful transvaginal ultrasound-guided puncture and injection of a cervical pregnancy in a patient with simultaneous intrauterine pregnancy and a history of a previous cervical pregnancy. Ultrasound Obstet Gynecol. 1996;8:381–386. doi: 10.1046/j.1469-0705.1997.08060381.x. [DOI] [PubMed] [Google Scholar]
- 22.Al-Azemi M, Ledger WL, Lockwood GM, Barlow DH. Successful transvaginal ultrasound-guided ablation of a cervical pregnancy in a patient with simultaneous intrauterine pregnancy after in vitro fertilization and embryo transfer. Hum Fertil (Camb) 1999;2:67–69. doi: 10.1080/1464727992000198341. [DOI] [PubMed] [Google Scholar]
- 23.Oláh KS. Massive obstetric haemorrhage resulting from a conservatively managed cervical pregnancy at delivery of its twin. BJOG. 2003;110:956–957. doi: 10.1111/j.1471-0528.2003.03063.x. [DOI] [PubMed] [Google Scholar]
- 24.Gyamfi C, Cohen S, Stone JL. Maternal complication of cervical heterotopic pregnancy after successful potassium chloride fetal reduction. Fertil Steril. 2004;82:940–943. doi: 10.1016/j.fertnstert.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 25.Ujvari E, Krizsa F, Sebestyen A, Varbiro S, Paulin F. Successful management of intrauterine twin and concomitant cervical pregnancy: a case report. Fetal Diagn Ther. 2006;21:181–184. doi: 10.1159/000089300. [DOI] [PubMed] [Google Scholar]
- 26.Suzuki M, Itakura A, Fukui R, Kikkawa F. Successful treatment of a heterotopic cervical pregnancy and twin gestation by sonographically guided instillation of hyperosmolar glucose. Acta Obstet Gynecol Scand. 2007;86:381–383. doi: 10.1080/00016340600617486. [DOI] [PubMed] [Google Scholar]
- 27.Majumdar A, Gupta SM, Chawla D. Successful management of post-in-vitro fertilization cervical heterotropic pregnancy. J Hum Reprod Sci. 2009;2:45–46. doi: 10.4103/0974-1208.51357. [DOI] [PMC free article] [PubMed] [Google Scholar]