Abstract
Dental pulp has the ability of repair/regeneration. Indirect pulp therapy (IPT) is recommended for pulp preservation in asymptomatic teeth with extremely deep caries as well as teeth with clinical symptoms of reversible pulpitis. In this case study, we performed IPT with calcium enriched mixture (CEM) cement on a symptomatic permanent molar. After clinical/radiographic examinations the tooth was diagnosed with irreversible pulpitis and associated apical periodontitis. IPT involved partial caries removal, the placement of CEM cement pulp cap and overlying adhesive permanent restoration. At the 1 week follow-up, patient's spontaneous symptoms had resolved. One-year follow-up demonstrated pulp vitality, clinical function, as well as the absence of pain/tenderness to percussion/palpation/cold sensitivity tests; periapical radiograph showed a healing periradicular lesion with newly formed bone, that is normal pulp with normal periodontium. These favorable results indicate that IPT/CEM may be a good treatment option in comparison to endodontic treatment in young patients. IPT of deep-caries lesion is an easier, more practical and valuable treatment plan than complete caries removal.
Keywords: Apical periodontitis, calcium enriched mixture cement, endodontic, pulp cap, pulpitis, stepwise excavation
INTRODUCTION
Symptomatic irreversible pulpitis is a pulpal state characterized by mild/severe pain that lingers after removal of a stimulus. In such cases, pulpectomy/extraction is required to alleviate the symptoms and prevent apical periodontitis.[1] However, as the severity of pulpal inflammation cannot be measured quantitatively, it must be based on clinical findings rather than histological diagnosis; moreover, there is poor correlation between the two.[2] In addition, pulps of teeth clinically diagnosed with irreversible pulpitis were shown to have the potential to heal after pulpotomy with appropriate biomaterials such as mineral trioxide aggregate (MTA) and calcium enriched mixture (CEM) cement.[3–7]
A systematic review revealed that to reduce the risk of carious pulp exposure, partial caries removal (indirect pulp therapy [IPT]) can result in long-term success compared with complete caries removal in the deep lesion.[8] A clinical trial demonstrated high survival rate of permanent teeth when deep carious lesions were managed without exposing the pulp by placing an indirect pulp cap.[9] These results demonstrated that the teeth pulps remained symptomless and maintained their healing potential and defensive capacity after treatment. Elimination of the bulk of the infected dentin and sealing the remaining carious lesion from oral fluids with appropriate materials is an accepted treatment for badly decayed teeth.[10] In addition, performance of IPT is simpler/more economical than RCT.
CEM cement has been introduced as a water-based and tooth-colored endodontic biomaterial. After mixing with liquid, the pH of CEM increases to >10.[11] It is assumed that in a high pH environment the calcium ions that are released from CEM react with endogenous phosphates to form hydroxyapatite; this would explain the favorable sealing ability/biocompatibility of the cement.[12] An in vitro study revealed that the anti-bacterial properties of CEM are similar to calcium hydroxide.[13] CEM has been employed as a root-end filling material,[14] as well as direct pulp capping agent,[15] pulpotomy agent,[5,6,16,17] apical plug,[18] in the repair of furcal perforations,[19] management of root resorption,[20] and regenerative endodontics.[21] Recently, an interesting report demonstrated favorable treatment outcomes of direct pulp capping with CEM for management of a permanent mature molar with irreversible pulpitis and associated apical periodontitis.[22]
The following report discusses the first case of successful management of a symptomatic permanent tooth with irreversible pulpitis and associated apical periodontitis using IPT with CEM, followed by a sandwich glass-ionomer composite restoration.
CASE REPORT
A 12-year-old female with a symptomatic first left lower molar was observed at a private clinic. She complained of severe lingering pain to cold lasting for few minutes. She also complained of spontaneous pain during the day and at night time. Review of the patient's medical history revealed no significant findings.
Extraoral evaluation revealed normal soft tissue structures with no apparent pathosis. Intraoral examination showed a first left lower molar with a large carious lesion. Diagnostic tests were performed; the involved tooth responded with mild pain to percussion and severe lingering pain to Endo-Frost cold spray (Roeko; Coltene Whaledent, Langenau, Germany).
Radiographic examination showed a large carious lesion associated with apical periodontitis [Figure 1]. The adjacent/opposing teeth were asymptomatic and responded normally to all diagnostic tests. Based on the clinical and radiographic examinations, the diagnosis of irreversible pulpitis with apical periodontitis was made. Thereafter, IPT of the tooth was decided; an informed consent was obtained from the patient's legal guardian.
Figure 1.
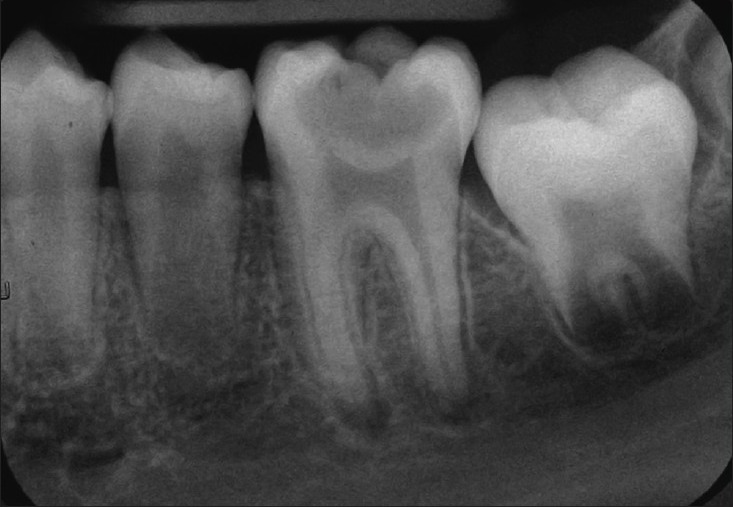
Intraoral pre-operative radiograph showing well-defined radiolucency of mesial and distal roots of symptomatic first lower left molar
The patient was instructed to rinse her mouth with 0.2% chlorhexidine. The tooth was anesthetized with 2% lidocaine with 1:80,000 epinephrine (DarouPakhsh, Tehran, Iran) and then isolated with rubber dam. Subsequently the dentin-enamel junction was completely excavated. The bulk of soft carious dentin was carefully removed by tungsten-carbide round burs (Komet, Lemgo, Germany) at low speed; medium and large spoon excavators (Ash, London, UK) were also used. Excavation was terminated once the remaining carious dentin showed increased resistance to manual instrumentation. After that, the remaining carious dentin in pulpal floor was covered by ≈1.5 mm layer of CEM cement (BioniqueDent, Tehran, Iran). The remaining tooth cavity was then restored/sealed with glass-ionomer cement and composite resin sandwich technique [Figure 2].
Figure 2.

Post-operative Orthopantomogram (OPG) showing threelayers ofrestorationconsistofindirectpulptherapy/calcium enriched mixture, glass ionomer and composite resin. Left: Higher magnification of treated first lower left molar revealing well defined periapical radiolucency of both roots
The patient was re-examined clinically after 1 and 7 days. At the 1-day follow-up the patient complained of sensitivity to cold which had significantly decreased 1 week post-operatively. Tenderness to percussion was not reported in both follow-ups. Patient was recalled at 1 year for clinical/radiographic follow-up. Clinical examination with cold test showed a vital tooth which was functional, asymptomatic, with normal physiologic mobility, normal probing depths, and a satisfactory coronal restoration. Radiographic examinations showed normal periodontium, and evidence of periapical healing [Figures 3 and 4]. The final diagnosis was normal pulp with normal PDL.
Figure 3.

Six-month follow-up radiograph showing healing process of apical pathology
Figure 4.

One-year follow-up radiograph showing complete periapical healing
DISCUSSION
This study conducted IPT with CEM cement for a pulp with sign/symptoms of irreversible pulpits along with apical periodontitis. Though, apical periodontitis seemed evident on the radiograph, the pulp was still vital. The general consensus in cases where irreversibly inflamed pulp has been diagnosed, is that the pulp no longer has the potential to heal and will not survive with any form of treatment. However, it should be considered that irreversible pulpitis is a clinical term for the classification of pulpal diseases; when treating the deep carious lesion clinicians have to diagnose irreversible pulpitis on the basis of indirect diagnostic methods. There is little evidence to correlate the clinical signs/symptoms with histological feature of the diseased pulp.[2] Therefore, dentists are trained to diagnose irreversible pulpitis when patient complains of pain lasting for a few minutes to several hours, pain exacerbating with hot/cold fluids, and radiating pain;[23] as well as tender to percussion. However, there is no information to indicate which symptom is an indication that the pulp no longer can repair itself. Conversely, recent reports have demonstrated that teeth with irreversible pulpitis showed favorable treatment outcomes with pulpotomy using CEM/MTA as pulp cappings.[3–5,7] Though the diseased pulps in these cases were inflamed, they were still vital; that is they still maintained a blood supply and therefore the most important factor for healing. In the light of recent high-level evidences,[7] the inflammatory process should be re-examined to recognize its possible or probable positive effect on pulpal healing.[23] Our clinical/radiographic follow-ups also showed favorable treatment outcomes for IPT/CEM. These results reveal that severe local inflammation in pulpal tissue may heal and be repaired if the irritant is removed and the pulp is well protected from further irritants. If further studies support this, there may be a need for reclassification of dental pulp diseases.
The concept of complete caries removal is currently being challenged for permanent teeth.[24] A growing body of evidence has demonstrated that IPT is successful for the management of deep caries lesion in primary molars as well as two-stage technique in immature permanent teeth; however, some recent studies have shown similar results in mature permanent teeth. IPT reduces the risk of carious pulp exposure, diminishes the substrate for microorganisms, prevents lesion development and promotes a physiological reaction in the pulp-dentin complex.[25] Several studies have demonstrated that once cariogenic bacteria are isolated from their nutritional supply by an adequate coronal seal, they either perish or become inactive.[24] Furthermore, once a seal is applied to carious dentin, it becomes dry/hard, arresting the carious process after IPT with a one-visit method. Accordingly, the second appointment may not be needed, if the coronal restoration preserves the seal of cavity. Our 1-year clinical follow-up showed that the one-visit IPT coronal filling was satisfactory, and therefore a second appointment was not scheduled.
Several dental materials have been suggested for capping the remaining carious lesion in IPT, that is calcium hydroxide, polycarboxylate cement combined with tannin-fluoride preparation, zinc-oxide eugenol cements, resin-bonded composite, glass ionomer cements and copper phosphate cement.[24] The ideal capping material should be anti-bacterial, non-toxic, dimensionally stable, biocompatible, and create a hermetic seal as well as be able to induce regeneration of the pulp. CEM cement as a new endodontic biomaterial demonstrated reasonable characteristics. Considerable data has shown favorable properties of CEM cement namely; anti-bacterial properties, sealing ability, dimensional stability and biocompatibility when compared with other gold standard materials such as calcium hydroxide or MTA.[6,11,13,15,16]
The favorable results in this case study may be partly attributed to the patient's age. A young patient's tooth may have slightly open apices and the dental pulp may respond more positively to pulp capping than a mature pulp.
CONCLUSIONS
Based on our clinical and radiographic observations, we can conclude that despite apparent pulpal and periradicular inflammation from the deep caries lesion, a conservative IPT can generate pulpal repair and periradicular healing in a mature permanent molar tooth. In addition, IPT/CEM of deep caries lesion in young patients is an easier, more practical and valuable treatment plan than complete caries removal which may result in pulp exposure and root canal treatment. However, well-conducted clinical trials on this proposed technique will be required for more grounding clinical evidence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Levin LG, Law AS, Holland GR, Abbott PV, Roda RS. Identify and define all diagnostic terms for pulpal health and disease states. J Endod. 2009;35:1645–57. doi: 10.1016/j.joen.2009.09.032. [DOI] [PubMed] [Google Scholar]
- 2.Seltzer S, Bender IB, Ziontz M. The dynamics of pulp inflammation: Correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol. 1963;16:846–71. doi: 10.1016/0030-4220(63)90323-2. [DOI] [PubMed] [Google Scholar]
- 3.Eghbal MJ, Asgary S, Baglue RA, Parirokh M, Ghoddusi J. MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J. 2009;35:4–8. doi: 10.1111/j.1747-4477.2009.00166.x. [DOI] [PubMed] [Google Scholar]
- 4.Asgary S, Ehsani S. Permanent molar pulpotomy with a new endodontic cement: A case series. J Conserv Dent. 2009;12:31–6. doi: 10.4103/0972-0707.53340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asgary S. Calcium-enriched mixture pulpotomy of a human permanent molar with irreversible pulpitis and condensing apical periodontitis. J Conserv Dent. 2011;14:90–3. doi: 10.4103/0972-0707.80733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nosrat A, Seifi A, Asgary S. Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: A randomized clinical trial. Int J Paediatr Dent. 2012 doi: 10.1111/j.1365-263X.2012.01224.x. [DOI] [PubMed] [Google Scholar]
- 7.Asgary S, Eghbal MJ. Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: A multi-center randomized controlled trial. Acta Odontol Scand. 2012 doi: 10.3109/00016357.2011.654251. [DOI] [PubMed] [Google Scholar]
- 8.Ricketts DN, Kidd EA, Innes N, Clarkson J. Complete or ultraconservative removal of decayed tissue in unfilled teeth. Cochrane Database Syst Rev. 2006;3:CD003808. doi: 10.1002/14651858.CD003808.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Bjørndal L, Thylstrup A. A practice-based study on stepwise excavation of deep carious lesions in permanent teeth: A 1-year follow-up study. Community Dent Oral Epidemiol. 1998;26:122–8. doi: 10.1111/j.1600-0528.1998.tb01938.x. [DOI] [PubMed] [Google Scholar]
- 10.Stark MM, Nicholson RJ, Soelberg KB. Direct and indirect pulp capping. Dent Clin North Am. 1976;20:341–9. [PubMed] [Google Scholar]
- 11.Asgary S, Shahabi S, Jafarzadeh T, Amini S, Kheirieh S. The properties of a new endodontic material. J Endod. 2008;34:990–3. doi: 10.1016/j.joen.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J. Effect of two storage solutions on surface topography of two root-end fillings. Aust Endod J. 2009;35:147–52. doi: 10.1111/j.1747-4477.2008.00137.x. [DOI] [PubMed] [Google Scholar]
- 13.Asgary S, Kamrani FA. Antibacterial effects of five different root canal sealing materials. J Oral Sci. 2008;50:469–74. doi: 10.2334/josnusd.50.469. [DOI] [PubMed] [Google Scholar]
- 14.Asgary S, Eghbal MJ, Ehsani S. Periradicular regeneration after endodontic surgery with calcium-enriched mixture cement in dogs. J Endod. 2010;36:837–41. doi: 10.1016/j.joen.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Asgary S, Eghbal MJ, Parirokh M, Ghanavati F, Rahimi H. A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:609–14. doi: 10.1016/j.tripleo.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Malekafzali B, Shekarchi F, Asgary S. Treatment outcomes of pulpotomy in primary molars using two endodontic biomaterials. A 2-year randomised clinical trial. Eur J Paediatr Dent. 2011;12:189–93. [PubMed] [Google Scholar]
- 17.Nosrat A, Asgary S. Apexogenesis treatment with a new endodontic cement: A case report. J Endod. 2010;36:912–4. doi: 10.1016/j.joen.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 18.Nosrat A, Asgary S, Eghbal MJ, Ghoddusi J, Bayat-Movahed S. Calcium-enriched mixture cement as artificial apical barrier: A case series. J Conserv Dent. 2011;14:427–31. doi: 10.4103/0972-0707.87218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samiee M, Eghbal MJ, Parirokh M, Abbas FM, Asgary S. Repair of furcal perforation using a new endodontic cement. Clin Oral Investig. 2010;14:653–8. doi: 10.1007/s00784-009-0351-8. [DOI] [PubMed] [Google Scholar]
- 20.Asgary S, Nosrat A, Seifi A. Management of inflammatory external root resorption by using calcium-enriched mixture cement: A case report. J Endod. 2011;37:411–3. doi: 10.1016/j.joen.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Nosrat A, Seifi A, Asgary S. Regenerative endodontic treatment (revascularization) for necrotic immature permanent molars: A review and report of two cases with a new biomaterial. J Endod. 2011;37:562–7. doi: 10.1016/j.joen.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Asgary S, Nosrat A, Homayounfar N. Periapical Healing After Direct Pulp Capping With Calcium-Enriched Mixture Cement: A Case Report. Oper Dent. 2012;37:571–5. doi: 10.2341/11-417-S. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg M, Farges JC, Lacerda-Pinheiro S, Six N, Jegat N, Decup F, et al. Inflammatory and immunological aspects of dental pulp repair. Pharmacol Res. 2008;58:137–47. doi: 10.1016/j.phrs.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson V, Craig RG, Curro FA, Green WS, Ship JA. Treatment of deep carious lesions by complete excavation or partial removal: A critical review. J Am Dent Assoc. 2008;139:705–12. doi: 10.14219/jada.archive.2008.0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maltz M, de Oliveira EF, Fontanella V, Bianchi R. A clinical, microbiologic, and radiographic study of deep caries lesions after incomplete caries removal. Quintessence Int. 2002;33:151–9. [PubMed] [Google Scholar]


