Abstract
A 32 year old Asian female on 300 mg per day of phenytoin following meningioma excision developed a fever with a diffuse maculopapular rash, lymphadenopathy and splenomegaly after12 days. A diagnosis of DRESS (Drug Rash Eosinophilia and Systemic Symptoms) syndrome was made. Patient was started on prednisolone at a dose of 1 mg/kg but since there was further deterioration in her condition, intravenous immunoglobulin was started. Clinical and blood parameters began to improve by the next day with liver functions returning to normal by the third week. DRESS syndrome is a drug hypersensitivity syndrome which can be fatal and therefore needs to be recognized early for the appropriate treatment to be started. The use of Intravenous immunoglobulins is anecdotal and the dramatic improvement noted in this case indicates that it is another treatment choice. The case and a brief review of the literature are discussed.
Keywords: Drug rash eosinophilia systemic symptoms, intravenous immunoglobulins, phenytoin
Introduction
Neurologists are familiar with the cutaneous adverse effects of anticonvulsant drugs which range from the mild itchy skin rash to the life threatening reactions like toxic epidermal necrolysis (TEN) and Steven Johnson syndrome (SJS). However, another serious adverse reaction which is rare with an incidence ranging from 1 in 5000 to 10000 after exposure to anticonvulsants but still with a risk of 10% for mortality is DRESS (Drug Rash Eosinophilia Systemic symptoms) syndrome.[1] Here we describe a patient who developed this reaction after exposure to phenytoin and responded well to intravenous Immunoglobulins (IVIG).
Case Report
A 32 year old Asian lady underwent excision surgery of a left frontal meningioma under Neurosurgery and was started on phenytoin at a dose of dose of 300 mg / day along with dexamethasone in the perioperative period. Dexamethasone was discontinued after 2 days and she was discharged from hospital with normal blood parameters including liver function tests 6 days after the surgery. While at home she developed fever and skin rash 12 days from the date of surgery. Phenytoin was promptly discontinued and it was replaced with Leviteracetam by the neurosurgeon but this was also discontinued 2 days later because of the rash becoming more widespread. She was then referred to the Neurology department 3 weeks after the onset of rash for further management.
On examination she had extensive maculopapular rash all over the body involving the face, trunk, upper and lower limbs. She had cervical and posterior auricular lymphadenopathy, jaundice, and splenomegaly. She denied any history of exposure to any other drug, recreational drug abuse, alcohol or blood transfusion.
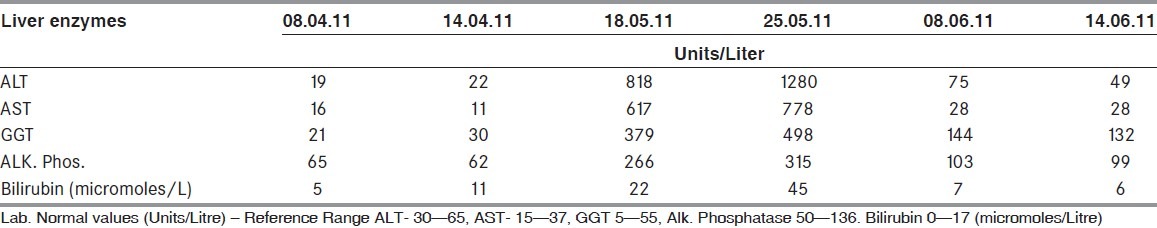
Lab investigation including complete blood count showed absolute eosinophilia 14.9% (Normal-0 to 7%), marked impairment of liver function [Table 1]. Investigations for other causes of hepatic disease including Serum copper, serum ceruloplasmin, screening for collagen disease, viral markers for hepatitis were all negative (HAV, HBV, HCV).
Table 1.
Blood investigations
Epstein Barr virus IgM and IgG antibodies were both positive. Cytomegalovirus Ab-IgG positive and IgM- negative
Serum ammonia, serum amylase, D Dimers were negative.
Urine R/M –no cells, Protein -1. Urine, throat, blood cultures were negative.
Drug hypersensitivity due to phenytoin was diagnosed and she was started on oral prednisolone 1 mg /Kg. However there was no improvement and the rashes were becoming more florid and liver function tests deteriorated further. Investigations 7 days after admission showed persistent increase of liver enzymes. Despite stopping phenytoin and treatment with prednisolone (1 mg /Kg) the rash was becoming more diffuse and serial LFT revealed increasing enzyme levels. Dermatology consultation confirmed the case as DRESS syndrome (Drug rash, Eosinophilia, Systemic symptoms) syndrome based on fever (39 to 40°c) drug rash, facial edema, eosinophilia, systemic manifestations of lymphadenopathy, splenomegaly, liver and renal impairment.
IVIG (0.4 Gm/ Kg) was added to prednisolone as there was no improvement even after 7 days of steroid treatment. After 5 days of I.V. Immunoglobulin (0.4 Gram/Kg) clinical improvement was evident, the rash subsided and a rapid decline of liver enzymes was observed [Table 1 and Figure 1]. Blood parameters returned to normal 3 weeks after starting IVIG and 6 weeks after the onset of the rash. In the meantime she was started on Topiramate which she tolerated well and was discharged from the hospital with tapering dose of prednisolone. On follow up till 2 months she was asymptomatic and well.
Figure 1.
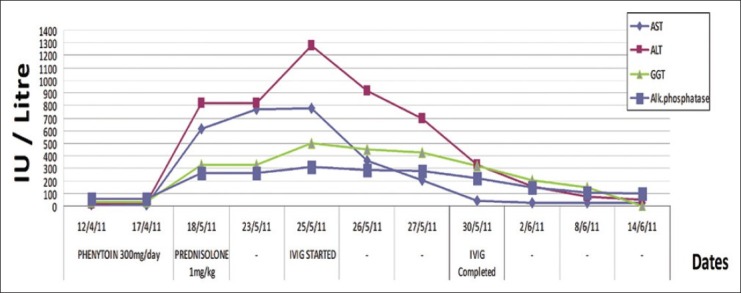
LFT with Steroid/IVIG Treatment Graph The graph is created by us and there is no cross citation
Discussion
DRESS Syndrome is an idiosyncratic reaction denoting Drug rash, Eosinophilia, and Systemic Symptoms occurring with a long latency period after exposure to the offending drug. Drug hypersensitivity to phenytoin was first described in 1940[2] and since then several names like drug hypersensitivity syndrome, anticonvulsant syndrome and phenytoin hypersensitivity syndrome, drug induced hypersensitivity syndrome (DIHS), drug induced pseudolymphoma were used to describe the syndrome. In 1996 Bocquet et al. introduced the term DRESS Syndrome to include all the above terms.[3] It is most frequently caused by aromatic anticonvulsants (Phenytoin, Phenobarbital, and Carbamazepine) however, later on other drugs such as sulphonamides, metronidazole, minocycline, allopurinol, and antivirals like nevirapine and abacavir have been implicated.
The latency occurs at a mean of 35 days (range 2 to 6 weeks) after starting the offending drug and the constellation of systemic manifestations distinguishes this from other severe cutaneous adverse reactions (SCAR) which include Steven Johnson syndrome (SJS) and Toxic epidermal necrolysis (TEN).[2] High fever up to 41°C. is a common presenting finding. The skin rash is usually maculopapular rash and or erythrodermic and facial edema is common.
Our patient developed rash 12 days after the exposure to phenytoin, had high fever (40°C.), maculopapular rash and facial edema. Hence, along with the lymphadenopathy, organomegaly, eosinophilia and elevated liver enzymes she fulfills the European Registry of Severe Cutaneous Adverse Reaction (RegiSCAR) criteria for the diagnosis of DRESS.[4]
The exact pathogenesis of DRESS Syndrome is not known and may be multifactorial which includes immunological mechanisms and failure of drug detoxification due to genetic deficiency in enzyme pathways.[5] The association of slow acetylation with increased risk of DRESS syndrome highlights the importance of drug metabolism in causation. Genetic polymorphism in the cytochrome enzymes that metabolize phenytoin may be responsible for variable rates of metabolism and thus susceptibility to toxicity even in individuals taking appropriate doses.[6] A recent retrospective study of 154 patients in Taiwan with AED induced SCARs revealed that phenytoin is the most common cause for DRESS syndrome and the liver was the most frequently involved internal organ as compared to AED induced SJS/TEN.[7]
The internal organ involvement is due to accumulation of eosinophils,that plays a role in the management and dramatic improvement noticed with steroids.
A study of Han Chinese population found that HLA-B5801 is a genetic marker for both TEN/SJS and HSS/DRESS caused by allopurinol.[8]
Early reactivation of Human herpes virus 6, Epstein Barr virus, Human Herpes virus 7 and cytomegalovirus have all been implicated in the development of DRESS.[9] Interestingly our patient too had elevated titres of both IgG and IgM of Epstein Barr virus and IgG of CMV. The long latency period for the evolution of the syndrome has been explained by the time delay for viral reactivation.[10]
It is recommended to start systemic steroids when involvement of internal organs is manifest.[11] However, our patient did not respond to the first line management of steroids but improvement occurred only after instituting IVIG. This is clearly evident in the graph that while on steroids the liver enzymes was increasing steadily to a peak and abrupt decrease of enzymes and rapid descent of the curve immediately after the IVIG. The use of IVIG in drug induced hypersensitivity syndrome (DIHS) including Toxic epidermal necrolysis (TEN) and Steven Johnson syndrome (SJS) has been reported earlier.[12] However, the use of IVIG in DRESS syndrome has been only anecdotal.[13] The management of SCAR patients which included supportive care, IVIG, corticosteroids and IVIG with or without corticosteroids in a large study of 281 patients did not show any significant benefit between the treatment arms.[14]
The exact mechanism of the therapeutic effect of IVIG in DRESS syndrome is not clear. The antiviral effect of IVIG to the viruses mentioned earlier which have been detected in some of the cases has been postulated as a mechanism. Another possible mechanism is the in vitro demonstration that IVIG can inhibit Fas-Fas ligand mediated apoptosis of keratinocytes derived from Toxic epidermal necrolysis patients. In addition IVIG produces effective Blockade of CD95 in Toxic epidermal necrolysis which is included in the spectrum of SCAR.[12]
In conclusion we have reported a case of DRESS syndrome related to phenytoin that developed a rash in 3 weeks. Despite the rarity of this syndrome a high index of suspicion with the appropriate clinical examination and investigations helps to clinch the diagnosis early, to initiate appropriate therapy. Corticosteroids are the first line of therapy, however if the response is not observed early enough initiation of second line therapy with Intravenous immunoglobulins can achieve the desired response and may be life saving.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Tennis P, Stem RS. Risk of serious cutaneous disorders after initiation of use of phenytoin, carbamazepine, sodium valproate: Record linkage study. Neurology. 1997;49:542–6. doi: 10.1212/wnl.49.2.542. [DOI] [PubMed] [Google Scholar]
- 2.Cooper R, Burrows RG. Treatment of epilepsy with sodium diphenyl hydantoin. Lancet. 1940;1:490–2. [Google Scholar]
- 3.Bocquet H, Bagot M, Roujeau JC. Drug induced pseudolymphoma and drug hypersensitivity syndrome. (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS) Semin Cutan Med Surg. 1996;15:250–7. doi: 10.1016/s1085-5629(96)80038-1. [DOI] [PubMed] [Google Scholar]
- 4.Kardaun SH, Sidoroff A, Valeyrie-Allonare L, Halevy S, Davidovici BB, Mockenhaupt M, et al. Variability in clinical pattern of cutaneous side effects of drugs with systemic symptoms: Does a DRESS syndrome really exist? Response Br J Dermatol. 2007;156:609–11. doi: 10.1111/j.1365-2133.2006.07704.x. [DOI] [PubMed] [Google Scholar]
- 5.Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): A clinical update and review of current thinking (Review) Clin Exp Dermatol. 2011;36:6–11. doi: 10.1111/j.1365-2230.2010.03967.x. [DOI] [PubMed] [Google Scholar]
- 6.Mc Cluggage LK, Voils SA, Bullock MR. Phenytoin toxicity due to genetic polymorphism. Neurocrit Care. 2009;10:222–4. doi: 10.1007/s12028-008-9165-9. [DOI] [PubMed] [Google Scholar]
- 7.Yang C-Y, Dao R-L, Lee T-J, Lu CW, Yang CH, Hung SI, et al. Severe cutaneous adverse drug reactions to antiepileptic drugs in Asians. Neurology. 2011;77:2025–33. doi: 10.1212/WNL.0b013e31823b478c. [DOI] [PubMed] [Google Scholar]
- 8.Hung SI, Chung WH, Liou LB, Chu CC, Lin M, Huang HP, et al. HLA B 5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc Natl Acad Sci U S A. 2005;102:4134–9. doi: 10.1073/pnas.0409500102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shiohara T, Inaoka M, Kano Y. Drug induced hypersensitivity syndrome (DIHS) A reaction induced by a complex interplay among herpes viruses and antiviral and antidrug immune responses. Allergol Int. 2006;55:1–8. doi: 10.2332/allergolint.55.1. [DOI] [PubMed] [Google Scholar]
- 10.Kano Y, Hiraharas K, Sakuma K, Shiohara Several herpes viruses can reactivate a severe drug induced multiorgan reaction in the same sequential order as graft versus–host disease. Br J Dermatol. 2006;155:301–6. doi: 10.1111/j.1365-2133.2006.07238.x. [DOI] [PubMed] [Google Scholar]
- 11.Tas S, Simonart T. Management of drug rash with eosinophilia and systemic symptoms (DRESS SYNDROME): An update. Dermatology. 2003;206:353–6. doi: 10.1159/000069956. [DOI] [PubMed] [Google Scholar]
- 12.Viard L, Wehrli P, Bullani R, Schneider P, Holler N, Salomon D, et al. Inhibition of toxic epidermal necrolysis by blockade of CD95 with intravenous immunoglobulin. Science. 1998;282:490–3. doi: 10.1126/science.282.5388.490. [DOI] [PubMed] [Google Scholar]
- 13.Tristani –Firouzi P. Nevirapine associated dress syndrome with intravenous immunoglobulin (IVIG) J Drugs Dermatol. 2005;4:510–3. [PubMed] [Google Scholar]
- 14.Schneck J, Fagot JP, Sekula P, Sassolas B, Roujeau JC, Mockenhaupt M. Effects of treatments of the mortality of Steven Johnson syndrome and toxic epidermal necrolysis; a retrospective study on patients included in the prospective EuroSCAR study. J Am Acad Dermatol. 2008;58:33–40. doi: 10.1016/j.jaad.2007.08.039. [DOI] [PubMed] [Google Scholar]


