Abstract
Purpose
To evaluate the trends in corneal refractive procedure selection for the correction of myopia, focusing on the relative proportions of laser in situ keratomileusis (LASIK) and surface ablation procedures.
Methods
Only eyes that underwent LASIK or surface ablation for the correction of myopia between 2008–2011 were included in this retrospective study. Additional recorded parameters included patient age, preoperative manifest refraction, corneal thickness, and calculated residual corneal bed thickness. A risk score was given to each eye, based on these parameters, according to the Ectasia Risk Factor Score System (ERFSS), without the preoperative corneal topography.
Results
This study included 16,163 eyes, of which 38.4% underwent LASIK and 61.6% underwent surface ablation. The risk score correlated with procedure selection, with LASIK being preferred in eyes with a score of 0 and surface ablation in eyes with a score of 2 or higher. When controlling for age, preoperative manifest refraction, corneal thickness, and all parameters, the relative proportion of surface ablation compared with LASIK was found to have grown significantly during the study period.
Conclusions
Our results indicate that with time, surface ablation tended to be performed more often than LASIK for the correction of myopia in our cohort. Increased awareness of risk factors and preoperative risk assessment tools, such as the ERFSS, have shifted the current practice of refractive surgery from LASIK towards surface ablation despite the former’s advantages, especially in cases in which the risk for ectasia is more than minimal (risk score 2 and higher).
Keywords: surface ablation, LASIK, PRK, myopia correction, ectasia
Introduction
Refractive surgery has evolved dramatically over the past two decades and is currently one of the most rapidly advancing fields of ophthalmology. The first technique for laser refractive correction was photorefractive keratectomy (PRK),1 which later evolved into laser epithelial keratomileusis (LASEK)2,3 and epi-LASEK. These techniques have been continuously improved and are grouped together as “surface ablation” techniques.4
Laser in situ keratomileusis (LASIK) is an alternative technique for refractive correction, in which the laser ablation is not performed at the anterior surface but within the stroma, after a stromal flap has been created.5,6 LASIK has several advantages over surface ablation techniques, such as faster visual recovery, lower rates of regression and infection, and less postoperative pain.7–9 These advantages have led to LASIK’s increasing popularity, and this is currently the most commonly performed corneal refractive procedure worldwide.9 Several recent studies focused on refractive surgery procedure trends attest to LASIK’s popularity, finding that it was performed in as many as 71%–92% of all patients who underwent corneal refractive procedures.9–13
Corneal ectasia is a potential complication of laser corneal refractive procedures that occurs mostly after LASIK for the correction of myopia.8,9 Although relatively rare, postoperative corneal ectasia is of great significance and has both medical and legal consequences.14 It is important to identify patients at risk for this complication and more prudent to consider surface ablation procedures in these cases. In 2008, Randleman et al15 comprehensively reviewed all reported cases of postoperative corneal ectasia and presented the Ectasia Risk Factor Score System (ERFSS). This score takes into account several risk factors associated with corneal ectasia, including abnormal preoperative topography, residual stromal bed thickness (RSB), patient age, preoperative central corneal thickness (CT), and degree of myopia. Although other factors may be associated with an increased risk of corneal ectasia, this score has proven to be relatively accurate,15–17 and we consider it a simple and effective screening tool.
The purpose of this study was to evaluate the trends in corneal refractive procedure selection between 2008 and 2011 at a single high-volume center. An additional goal was to evaluate the effect that awareness to the ERFSS had on the proportion of surface ablation procedures versus LASIK, over time.
Methods
The study was approved by the institutional review board of the Tel-Aviv Medical Center. Data was retrieved from the electronic medical records of a refractive surgery facility (Care Vision, Tel Aviv, Israel). The data was routinely collected and entered into the electronic medical record database by the refractive surgery facility employees. The records of all patients who underwent corneal refractive surgery between January 1, 2008 and December 31, 2011 were retrospectively scanned.
Patients who underwent surgery for the correction of any degree of myopia were included in this study (range −0.5 to −11.75 diopters [D]). Only previously untreated eyes were included in the study, and eyes that underwent any additional intervention after the refractive surgery were excluded. Patients who underwent refractive surgery for the correction of hyperopia were excluded, as were those who underwent enhancement corneal laser procedures or any other type of refractive surgery (eg, conductive keratoplasty, refractive lens exchange, or phakic intraocular lens implantation).
Additional recorded parameters included patient age, preoperative manifest refraction, simulated keratometry obtained from a corneal topographer (Orbscan® IIz; Bausch and Lomb, Rochester, NY, USA or Sirius; Costruzioni Strumenti Oftalmici, Scandicci, Italy), CT (obtained from the same instruments), and RSB. This last value was calculated based on CT, planned treatment, and an estimated 120 micron thickness of the LASIK flap. Only patients over 18 years of age were included in this study. Included in the study were eyes in which the keratometry readings were between 35–49 D and CT was between 400–600 μm. Eyes with preoperative astigmatism over 6.5 D were also excluded. Patients whose records were incomplete for the relevant parameters were excluded.
According to the recorded parameters, an ectasia risk score was calculated for each eye. Since topography data was not available in a numerical form, this was not part of the risk score. The score was therefore an underestimation of the ERFSS reported by Randleman et al.15 Scores were assigned according to the values reported in that study (Table 1).
Table 1.
The ectasia risk score system used in this study, which was the ERFSS reported by Randleman et al,15 without the corneal topography
| Parameter | Points | ||||
|---|---|---|---|---|---|
|
|
|||||
| 4 | 3 | 2 | 1 | 0 | |
| RSB (μm) | <240 | 240–259 | 260–279 | 280–299 | >300 |
| Age (years) | 18–21 | 22–25 | 26–29 | >30 | |
| CT (μm) | <450 | 451–480 | 481–510 | >510 | |
| MRSE (D) | >−14 | −12 to −14 | −10 to −12 | −8 to −10 | −8 or less |
Abbreviations: RSB, residual stromal bed thickness; CT, corneal thickness; MRSE, manifest refraction spherical equivalent; D, diopters.
The selected procedure for correction of myopia was categorized either as LASIK or as surface ablation (ie, PRK and LASEK). The relative proportions of LASIK and surface ablation procedures were calculated for each month, quarter, and year, over a 4-year period. These proportions were compared independently for each parameter and for the ectasia risk score of each eye.
All procedures were performed by the facility’s eight surgeons using the Allegretto 200 Hz Excimer Laser (Wave-Light GmbH, Erlangen, Germany). LASIK procedures were performed using the Moria M2 Single Use microkeratome and Moria One Use Plus SBK microkeratome (Moria, Antony, France). The cost of all procedures was not significantly different, and the profit for the surgeon was the same regardless of the selected procedure. We therefore assume that financial considerations did not affect the choice of procedures and that the surgeons’ decisions were made in the patients’ best interest.
Statistical analysis was performed using the SPSS statistics version 20.0 software (IBM, Armonk, New York). Descriptive statistics were employed. Logistic regression was employed to examine the effect of the year of surgery on the selection of surgical procedure, controlling for differences in age, refraction, corneal thickness, and RSB. Student t-test (2 tailed) was used to compare selection of the surgical procedure for parametric variables and Pearson chi-square test was used for nonparametric variables. Statistical significance was declared when P < 0.05.
Results
The study included 16,163 eyes that fulfilled the inclusion criteria. Of these eyes, 50.1% were right eyes and 49.9% were left eyes; 46% belonged to female patients and 54% to male patients. LASIK was performed on 6214 (38.4%) eyes, and surface ablation was performed on the remaining 9949 (61.6%) eyes.
Mean patient age was 27.68 ± 8.00 years (median 25, range 18–59 years). Patient age was distributed between all age groups without statistical significance (Table 2). The mean CT was 534 ± 33 μm, and 75.4% of the eyes had preoperative CT over 510 μm and were scored as 0 in the risk for ectasia depending on this parameter. The mean manifest refraction spherical equivalent (MRSE) was −3.98 ± 2.08 D, and 95.1% of the eyes were treated for MRSE of less than −8 D and were scored as 0 in the risk for ectasia depending on this parameter. The mean planned RSB was 348 ± 43 μm, and 86.6% of the eyes had planned RSB thicker than 300 μm and were scored as 0 in the risk for ectasia depending on this parameter. The distribution of eyes between the risk groups is provided in Table 2.
Table 2.
The distribution of eyes between the risk factor score groups for each parameter
| Parameter | Risk score group (%) | ||||
|---|---|---|---|---|---|
|
|
|||||
| 4 | 3 | 2 | 1 | 0 | |
| RSB (μm) | 0.6 | 1.8 | 3.9 | 7.1 | 86.6 |
| Age (years) | 24.7 | 26.4 | 15.2 | 33.7 | |
| CT (μm) | 0.8 | 5.5 | 18.3 | 75.4 | |
| MRSE (D) | 0 | 0 | 1.0 | 3.9 | 95.1 |
Abbreviations: RSB, residual stromal bed thickness; CT, corneal thickness; MRSE, manifest refraction spherical equivalent; D, diopters.
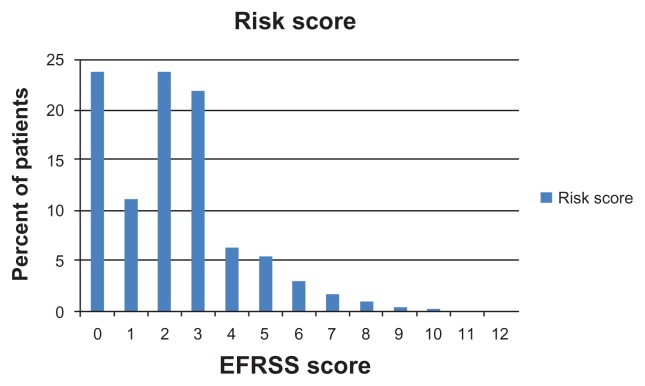
The mean ectasia risk score based on these parameters was 2.25 ± 1.9, with a range between 0–12 of 15 possible points, and 81.5% of eyes included in the study had a risk score of 3 or lower. The distribution of the risk scores is presented in Figure 1.
Figure 1.
The distribution of the risk score in the eyes included in the study.
Note: Values are presented in percentages.
Abbreviation: EFRSS, Ectasia Risk Factor Score System.
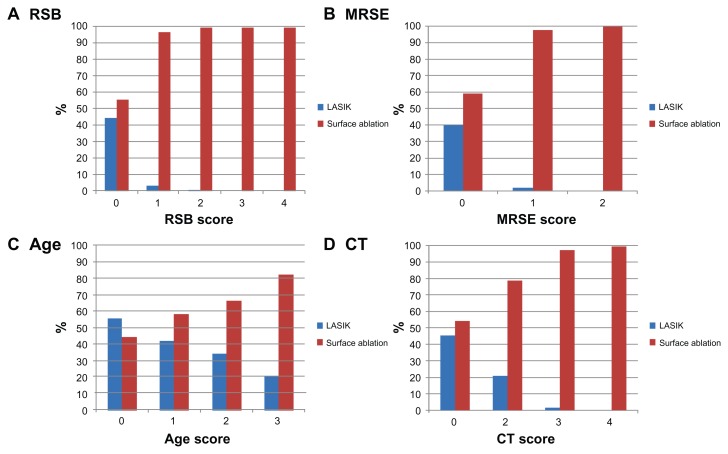
Analysis by risk factors
Planned RSB was significantly higher in eyes that underwent LASIK than in those that underwent surface ablation (371 μm vs 333 μm; t-test P < 0.001). The RSB score had a considerable effect on procedure selection. While eyes with a risk of 0 were distributed equally between LASIK and surface ablation, surface ablation was performed in 98.1% of eyes with a score of 1 or higher, representing a significant effect on procedure selection (Pearson chi-square P < 0.001). The effect of RSB score on procedure selection is presented in Figure 2A.
Figure 2.
The distribution of LASIK and surface ablation procedures according to the risk score of (A) RSB; (B) MRSE; (C) age; and (D) CT.
Note: The relative proportion of the procedures for each risk score is presented in percentages.
Abbreviations: LASIK, laser in situ keratomileusis; RSB, residual stromal bed thickness; MRSE, manifest refraction spherical equivalent; CT, corneal thickness.
Preoperative refractive error (calculated as MRSE) was significantly more myopic in eyes that underwent surface ablation than in those that had LASIK (−4.4 D vs −3.3 D, respectively; t-test P < 0.001). MRSE score had a considerable effect on procedure selection, as surface ablation was performed in 98.4% of eyes with a score of 1 or higher, representing a significant effect on procedure selection (Pearson chi-square P < 0.001). The effect of MRSE score on procedure selection is presented in Figure 2B.
Patient age was significantly higher in eyes that underwent LASIK than in those that underwent surface ablation (30.7 vs 25.8 years; t-test P < 0.001). Age score had an effect on procedure selection. While eyes with a risk score of 0–1 distributed equally between LASIK and surface ablation, LASIK was performed in 64.8% of eyes with a score of 2 or higher (Pearson chi-square P < 0.001). The effect of age score on procedure selection is presented in Figure 2C.
CT was statistically significantly higher in eyes that underwent LASIK than in those that underwent surface ablation (546 μm vs 527 μm; t-test P < 0.001). CT score had a considerable effect on procedure selection. While eyes with a risk of 0 distributed equally between LASIK and surface ablation, surface ablation was performed in 80.8% of eyes with a score of 1 or higher, representing a significant effect on procedure selection (Pearson chi-square P < 0.001). The effect of CT score on procedure selection is presented in Figure 2D.
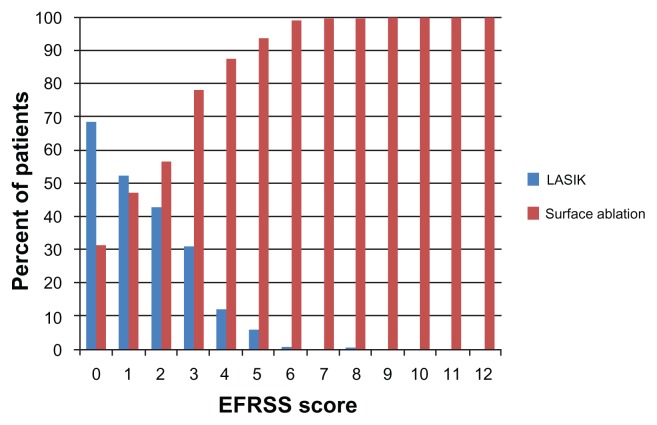
Analysis by risk score
The ectasia risk score had a significant effect on procedure selection (Pearson chi-square P < 0.001). As presented in Figure 3, LASIK was preferred in eyes with a risk score of 0 (3896 eyes), eyes with a risk score of 1 (1852 eyes) distributed equally between the two procedures, and surface ablation was preferred in eyes with a risk score of 2 or higher (10,415 eyes). Virtually all eyes with a risk score of 6 or higher underwent surface ablation.
Figure 3.
The distribution of LASIK and surface ablation procedures according to the overall risk score.
Note: The relative proportion of the procedures for each score is presented in percentages.
Abbreviations: EFRSS, Ectasia Risk Factor Score System; LASIK, laser in situ keratomileusis.
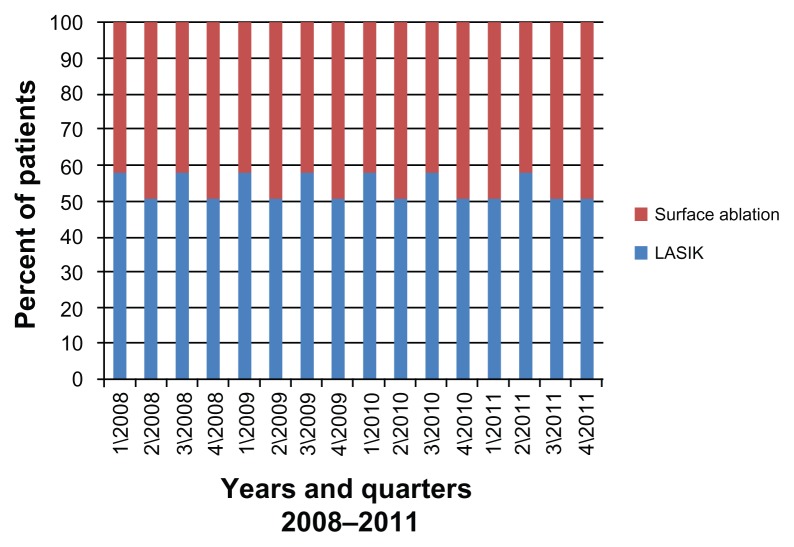
Analysis by time
The annual distribution of LASIK and surface ablation between the years 2008 and 2011 is presented in Table 3. The differences in procedure selection between years were statistically significant (Pearson chi-square P < 0.001). The difference in the relative proportions of LASIK and surface ablation was statistically significant when analyzed by quarters and separate months as well (P < 0.001 for both). The trend of the decline in LASIK’s relative proportion is depicted in Figure 4.
Table 3.
Distribution of procedures between 2008–2011
| Year | Total eyes | LASIK (%) | Surface ablation (%) |
|---|---|---|---|
| 2008 | 3521 | 53.90 | 48.10 |
| 2009 | 4154 | 46.84 | 53.16 |
| 2010 | 4138 | 27.81 | 72.19 |
| 2011 | 4350 | 28.02 | 71.98 |
Abbreviation: LASIK, laser in situ keratomileusis.
Figure 4.
The relative proportions of LASIK and surface ablation procedures by quarters, from 2008 to 2011.
Note: values are presented in percentages.
Abbreviation: LASIK, laser in situ keratomileusis.
Controlling for the above mentioned parameters (RSB, MRSE, age, and CT), the odds, calculated using logistic regression, for choosing surface ablation over LASIK during 2009 compared to 2008 were 1.329 (95% confidence interval [CI] 1.194–1.480). The odds for choosing surface ablation over LASIK during 2010 compared to 2008 were 3.639 (95% CI 3.246–4.079). The odds for choosing surface ablation over LASIK during 2011 compared to 2008 were 2.685 (95% CI 2.399–3.006).
Discussion
Our results indicate that surface ablation procedures were performed more commonly than LASIK during 2008–2011 at our clinic. During this 4-year period, LASIK was only performed in 38.4% of eyes included in this study. This finding stands in contrast to recent studies in which LASIK was reported to be the predominantly performed refractive procedure.9–13
Procedure selection was shown to be significantly influenced by patient age, preoperative MRSE, RSB, and CT. Younger age, increased myopia, and lower RSB and CT are known risk factors for postoperative corneal ectasia, and all were found in this study to be significantly associated with the preference of surface ablation procedures over LASIK (Figure 2). The risk score calculated in this study was also significantly correlated with the preference of surface ablation in higher-risk eyes. LASIK was more commonly performed in eyes with a risk score of 0, but in eyes with a score of 2 or higher, surface ablation was consistently preferred. Of special interest is the fact that the relative proportion of LASIK gradually decreased over the study period, regardless of the risk factors and score (Table 3 and Figure 4).
The risk score used in this study is an underestimation of the ERFSS reported by Randleman et al,15 and we believe our results reflect the accumulating influence of this preoperative risk-assessment tool on refractive surgeons. Corneal ectasia is a dreaded complication, and both surgeons and patients have a keen interest to avoid this as much as possible. Our results demonstrate that despite LASIK’s innate advantages,7–9 surface ablation procedures are preferred when the risk for ectasia is more than minimal. The Randleman et al studies of the ERFSS were published in 2008, and were subsequently assimilated in the practice of corneal refractive surgery. We believe they influenced the consideration of LASIK by refractive surgeons and the way they advised their patients, and shifted the trend toward selection of surface ablation procedures, which increased in 2009 compared with 2008, and even more so in 2010–2011.
Limitations of this study include its retrospective nature and its basis on data from one center only. We believe these limitations are more than compensated for by the large series size, completeness of data, and the fact that surgeries were performed by numerous independent physicians. Another limitation is the absence of corneal topography measurements, which led to an underestimation of the ERFSS. This may have exaggerated the significance of its other parameters. However, these correlations are still statistically valid, and the increased preference of surface ablation over LASIK has also been demonstrated by a comparison controlled for these parameters.
We note that the risk assigned to patient age may contribute significantly to the choice of procedure. Many patients seeking surgery for the correction of myopia are young adults, and anyone 25 years or younger would receive an ERFSS of at least 2, which according to our results, would significantly increase his/her chance of undergoing surface ablation over LASIK. It is also important to note that this study does not corroborate the accuracy of the ERFSS in predicting ectasia, as the occurrence of ectasia was not recorded and was not part of the study design.
In conclusion, our results indicate a shift in recent years towards surface ablation procedures and the preference for these over LASIK, both in general and specifically in eyes at risk for ectasia. Despite greater early discomfort and a longer visual recovery period, it seems that both surgeons and patients are currently more inclined to choose surface ablation procedures in order to minimize the risk of ectasia. This trend reflects recent advances in the understanding of the risk factors for this complication and the development of tools, such as the ERFSS, that aid in preoperative risk assessment and procedure selection. It is possible that with increased awareness of risk factors for ectasia, advanced surface ablation procedures have regained popularity and become more common than LASIK for the correction of myopia.
Footnotes
Disclosure
The authors report no conflicts of interest with the submission of this work. No financial support was received for the submission. No author has any proprietary interest in the publication of this report.
References
- 1.Munnerlyn CR, Koons SJ, Marshall J. Photorefractive keratectomy: a technique for laser refractive surgery. J Cataract Refract Surg. 1988;14(1):46–52. doi: 10.1016/s0886-3350(88)80063-4. [DOI] [PubMed] [Google Scholar]
- 2.Azar DT, Ang RT, Lee JB, et al. Laser subepithelial keratomileusis: electron microscopy and visual outcomes of flap photorefractive keratectomy. Curr Opin Ophthalmol. 2001;12(4):323–328. doi: 10.1097/00055735-200108000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Camellin M. Laser epithelial keratomileusis for myopia. J Refract Surg. 2003;19(6):666–670. doi: 10.3928/1081-597X-20031101-09. [DOI] [PubMed] [Google Scholar]
- 4.Trattler WB, Barnes SD. Current trends in advanced surface ablation. Curr Opin Ophthalmol. 2008;19(4):330–334. doi: 10.1097/ICU.0b013e3283034210. [DOI] [PubMed] [Google Scholar]
- 5.Steinert RF, Shamik B. Surgical correction of moderate myopia: which method should you choose? II. PRK and LASIK are the treatments of choice. Surv Ophthalmol. 1998;43(2):157–179. doi: 10.1016/s0039-6257(98)00027-7. [DOI] [PubMed] [Google Scholar]
- 6.Rashad KM. Laser in situ keratomileusis for myopic astigmatism. J Refract Surg. 1999;15(6):653–660. doi: 10.3928/1081-597X-19991101-09. [DOI] [PubMed] [Google Scholar]
- 7.Sugar A, Rapuano CJ, Culbertson WW, et al. Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American Academy of Ophthalmology. Ophthalmology. 2002;109(1):175–187. doi: 10.1016/s0161-6420(01)00966-6. [DOI] [PubMed] [Google Scholar]
- 8.Ambrósio R, Jr, Wilson S. LASIK vs LASEK vs PRK: advantages and indications. Semin Ophthalmol. 2003;18(1):2–10. doi: 10.1076/soph.18.1.2.14074. [DOI] [PubMed] [Google Scholar]
- 9.Sutton GL, Kim P. Laser in situ keratomileusis in 2010 – a review. Clin Experiment Ophthalmol. 2010;38(2):192–210. doi: 10.1111/j.1442-9071.2010.02227.x. [DOI] [PubMed] [Google Scholar]
- 10.O’Keefe M, Kirwan C. Laser epithelial keratomileusis in 2010 – a review. Clin Experiment Ophthalmol. 2010;38(2):183–191. doi: 10.1111/j.1442-9071.2010.02198.x. [DOI] [PubMed] [Google Scholar]
- 11.Kuo IC. Trends in refractive surgery at an academic center: 2007–2009. BMC Ophthalmology. 2011;11:11. doi: 10.1186/1471-2415-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmack I, Auffarth GU, Epstein D, Holzer MP. Refractive surgery trends and practice style changes in Germany over a 3-year period. J Refract Surg. 2010;26(3):202–208. doi: 10.3928/1081597X-20090515-05. [DOI] [PubMed] [Google Scholar]
- 13.Waring GO, Durrie DS. Emerging trends for procedure selection in contemporary refractive surgery: consecutive review of 200 cases from a single center. J Refract Surg. 2008;24(4):S419–S423. doi: 10.3928/1081597X-20080401-19. [DOI] [PubMed] [Google Scholar]
- 14.Binder PS, Lindstrom RL, Stulting RD, et al. Keratoconus and corneal ectasia after LASIK. J Cataract Refract Surg. 2005;31(11):2035–2038. doi: 10.1016/j.jcrs.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115(1):37–50. doi: 10.1016/j.ophtha.2007.03.073. [DOI] [PubMed] [Google Scholar]
- 16.Randleman JB, Trattler WB, Stulting RD. Validation of the Ectasia Risk Score System for preoperative laser in situ keratomileusis screening. Am J Ophthalmol. 2008;145(5):813–818. doi: 10.1016/j.ajo.2007.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan CC, Hodge C, Sutton G. External analysis of the Randleman Ectasia Risk Factor Score System: a review of 36 cases of post LASIK ectasia. Clin Experiment Ophthalmol. 2010;38(4):335–340. doi: 10.1111/j.1442-9071.2010.02251.x. [DOI] [PubMed] [Google Scholar]