Abstract
This article examined the effects of maternal depression during the postpartum period (Time 1) on the later behavior problems of toddlers (Time 3) and tested if this relationship was moderated by paternal psychopathology during toddlers’ lives and/or or mediated by maternal parenting behavior observed during mother–child interaction (Time 2). Of the 101 mothers who participated in this longitudinal study with their toddlers, 51 had never experienced an episode of Major Depressive Disorder (MDD) and 50 had experienced an episode of MDD during the first 18 months of their toddlers’ lives. Maternal depression at Time 1 was significantly associated with toddlers’ externalizing and internalizing behavior problems only when paternal psychopathology was present. As predicted, maternal negativity at Time 2 was found to mediate the relationship between maternal depression at Time 1 and toddlers’ externalizing behavior problems at Time 3.
Despite a large body of empirical studies illustrating maternal depression as a risk factor for negative developmental outcomes in older children and adolescents, less consistent findings have been demonstrated in studies of the effects of maternal depression on infant and toddler outcomes. Indeed, several studies of early childhood have failed to find differences in markers of socioemotional competence and adaptation in young children based upon exposure to maternal depression. In their study of maternal depression and toddler attachment, Radke-Yarrow and colleagues did not find differences in rates of infant attachment insecurity between depressed and nondepressed mothers, although higher rates of insecure attachment were evident in the children of mothers with bipolar disorder (Radke-Yarrow, Cummings, Kuczynski, & Chapman, 1985). Likewise, Cohen and Campbell (1992) found that maternal depression, in the absence of other risk factors, did not predict poor infant responsiveness or insecure attachment in infants. Toddlers with depressed mothers did not differ from controls in their attachment security and social competence (Seifer et al., 1996) and in attachment security in preschool children with depressed and nondepressed mothers (Frankel & Harmon, 1996). A more recent meta-analysis of studies on the effects of early maternal depression on infant attachment highlighted the heterogeneity in the attachment security of young children exposed to early maternal depression (Martins & Gaffan, 2000). Taken together, these findings suggest that maternal depression, as a single risk factor, may not always predict child maladjustment early in development.
Studies that do not find main effects for the impact of maternal depression on child outcomes may be related to the limited examination of family risk factors that co-occur with maternal depression and increase prediction of which children exposed to maternal depression are most at-risk. Specifically, maternal depression may be more likely to be associated with young children’s maladjustment in the presence of paternal psychopathology and negative maternal interaction styles. Recent conceptual publications have proposed examining multiple contextual risk factors when investigating the relationship between maternal depression and young children’s maladjustment and have presented models for understanding the more complex relationships between maternal depression, family risk factors, and children’s maladjustment (e.g., Goodman & Gotlib, 1999). However, empirical tests of the role of these family risk factors have lagged behind theoretical advances in conceptualizing the nature of multivariate interplay between maternal depression and family risk factors.
Existing studies on the effects of maternal depression on children’s outcomes also often do not examine different indices of maternal depression. Early exposure to maternal depression has been hypothesized to interfere with children’s normative developmental processes and several studies indicate that early exposure to maternal depression has lingering detrimental effects on children’s functioning (Hay, Pawlby, Angold, Harold, & Sharp, 2003; Hay et al., 2001) and mother–child interactions (Stein et al., 1991), even after mothers’ depression remit. Other studies suggest that chronic exposure to maternal depression is more strongly associated with increased maternal parenting stress (Cornish et al., 2006) and negative child outcomes (McMahon, Barnett, Kowalenko, & Tennant, 2006; Trapolini, McMahon, & Ungerer, 2007). At the same time, a growing body of evidence also suggests that a reduction in mother’s depressive symptoms is associated with an improvement in children’s functioning (Cicchetti & Schneider-Rosen, 1986; Field, 1992; Pianta, Erickson, Wagner, Kruetzer, & Egeland, 1990) and in the quality of mother–child interactions (Campbell & Cohn, 1997). Hence, the examination of various indices of maternal depression (e.g., history, chronicity, and recency of maternal depression) may provide answers regarding what types of maternal depression confer the greatest risk to children.
The goal of this empirical study was to advance the social development literature related to maternal depression by testing two alternative multivariate formulations (e.g., mediation, moderation) of the effects of maternal depression, paternal psychopathology, and negative maternal feedback on toddlers’ behavior problems. This study, involving a multimethod battery, clinically identified sample of mothers and prospective diagnostic assessment of maternal depression, attempts to improve methodological characteristics highly representative of the maternal depression literature to date that typically rely on monomethod designs, community samples of mothers, and single assessments of maternal depression (e.g., lifetime history or current depression).
PATERNAL PSYCHOPATHOLOGY
Epidemiological studies have consistently outlined a higher likelihood for cooccurring psychopathology in spouses (Dierker, Merikangas & Szatmari, 1999; Merikangas, 1984). Because depressed women are more likely to choose spouses with depression, substance use disorders, or antisocial personality disorder (Gotlib & Hammen, 1992), young children of depressed mothers are more likely to have fathers with a psychological disturbance. Paternal psychopathology has been associated with high levels of behavior problems and maladjustment in children and adolescents (see Kane & Garber, 2004). The presence or absence of mental disorders in fathers may modify the degree of risk these children experience. Involvement with healthy fathers may promote resilience in children with depressed mothers and may buffer children from negative effects of maternal depression (Field, Hossain, & Malphurs, 1999; Tannenbaum & Forehand, 1994). However, involvement with impaired fathers may increase the likelihood for negative outcomes in young children with depressed mothers (Jaffee, Moffitt, Caspi, & Taylor, 2003). Paternal psychopathology increases children’s genetic vulnerability for developing psychiatric disorders, exacerbates stress between family members, and reduces cohesion in the family environments in which these children are socialized (Dierker et al., 1999). Hence, the combined risk of both maternal depression and paternal psychopathology may pose a “double whammy” for children already at risk for maladjustment (Jaffee et al., 2003).
Goodman and Gotlib (1999) outlined a conceptual model whereby the presence of paternal psychopathology moderates the effect of maternal depression on children’s risk for psychopathology. They proposed that fathers may increase the risk for psychopathology in children of depressed mothers if they too have psychopathology. The rationale for exploring paternal psychopathology as a moderator, rather than mediator, is supported by a handful of empirical studies indicating that school-aged children with two depressed parents are at significantly greater risk for disorder than are school-aged children with one depressed parent (Weissman, Leckman, Merikangas, Gammon, & Prusoff, 1984) and, conversely, that the presence of a healthy father in the home is associated with low rates of disorder among school-aged children with depressed mothers (Conrad & Hammen, 1989). Connell and Goodman (2002) also presented preliminary evidence in their meta-analysis that paternal psychopathology moderates the association between maternal psychopathology and school age children’s maladjustment.
The role of paternal psychopathology to moderate young children’s maladjustment when maternal depression is present is a promising area of investigation. However, the few studies that have examined paternal psychopathology in relation to maternal depression in young children have not found a moderating effect (Goodman, Brogan, Lynch, & Fielding, 1993) or have found this effect in community samples of mothers who did not meet diagnostic criteria for depression. For example, Eiden and Leonard (1996) found that paternal psychopathology moderated the association between maternal depression and toddlers’ attachment security, as those mothers with elevated symptoms of depression who had alcohol dependent husbands were more likely to have insecurely attached toddlers. Similarly, Carro and colleagues found that paternal depressive symptoms moderated the relationship between maternal postpartum depressive symptoms and toddlers’ behavior problems in situations where maternal depressive symptoms were low (Carro, Grant, Gotlib, & Compras, 1993). These findings, therefore, need to be replicated in a clinical sample of depressed mothers with young children.
MOTHER–CHILD INTERACTION
Mothers’ verbal and nonverbal communication with children in social interactions represents a primary vehicle for young children’s developing social competence (Maccoby, 1992). Positive communication styles and maternal warmth observed in mother–child interactions have been associated with prosocial behavior and positive self-concept development in children (Kochanska, 1997). On the other hand, negative affectivity and communication styles observed in mothers have been associated with negative self-concept (Goodman, Adamson, Riniti, & Cole, 1994; Hammen, Burge, & Stansbury, 1990), low perceived competence (Jacquez, Cole, & Searle, 2004), and high levels of externalizing and internalizing behavior in children (Caspi et al., 2004; Nelson, Hammen, Brennan, & Ulman, 2003; Vostanis, Nicholls, & Harrington, 1994). Similar research on the construct of expressed emotion also indicates that mothers of children with behavioral disorders express more critical comments, fewer positive comments, and less warmth toward their children than do control parents when asked to provide a 5-min speech sample about their children (McCarty, Lau, Valeri, & Weisz, 2004; Nelson et al., 2003; Peris & Baker, 2000). Indeed, a high level of parental criticism in the 5-min speech sample is strongly associated with problematic parent–child interactions (McCarty et al., 2004).
Because depression negatively affects interpersonal relationships, several studies have found that depressed mothers demonstrate high levels of negative affect and critical feedback and low levels of sensitivity and warmth in interactions with their young children (Campbell, Cohn, & Meyers, 1996; Cicchetti & Toth, 1995; Cohn, Matias, Tronick, Connell, & Lyons-Ruth, 1986; Field, 1995; Shaw & Bell, 1993; Zahn-Waxler, Iannotti, Cummings, & Dedham, 1990). As a part of their conceptual model for the intergenerational transmission of depression, Goodman and Gotlib (1999) proposed that parenting interactions mediate the effects of maternal depression on children’s social and emotional development. Maternal negativity, low levels of maternal warmth, and negative communication styles may be mechanisms through which parenting interactions of depressed mothers increase their children’s risk for behavior and emotional problems. However, only a few empirical studies have demonstrated negative maternal parenting mediating the relationship between maternal depression and maladjustment in young children (Campbell et al., 1996; Cicchetti, Rogosch, & Toth, 1998).
RATIONALE OF PROPOSED STUDY
This study examined the associations among maternal depression, paternal psychopathology, and three indices of maternal parenting in the context of mother–child interactions (negativity, warmth, negative feedback) on toddlers’ externalizing and internalizing behavior problems. A large clinical sample of mothers who had experienced an episode of Major Depressive Disorder (MDD) in the first 18 months of their toddlers’ lives and a matched control group were recruited to examine the effects of maternal depression on various aspects of toddlers’ social and emotional development. The sample was relatively homogeneous, composed of mostly intact, middle-class families, which allowed for isolating the influence of maternal depression from other high-risk factors associated with poor child outcomes (e.g., low socioeconomic status [SES], divorce).
The longitudinal design of the study allowed for examining the effects of maternal depression on toddler behavior problems, and the potential of maternal parenting behavior to mediate this relationship, over a 16-month period. Because newer conceptions of mediation and moderation require a temporal precedent (see Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001), maternal depression status when toddlers were approximately 18 months of age (Time 1) was used as our primary index of maternal depression. Retrospective and current assessment of maternal depression at Time 1 allowed for the construction of a single index that captured both history of maternal depression during the first 18 months of toddlers’ lives and mothers’ current depressive symptoms. A measure of toddler adjustment was administered when toddlers were approximately 33 months of age (Time 3). The potential mediators of maternal negativity and warmth reflected data coded from videotaped mother–child interactions conducted when toddlers were approximately 25 months of age (Time 2). The third potential mediator examined, maternal negative feedback, was coded from videotaped mother–child interactions collected at Time 3. Although this potential mediator is concurrent with the outcome variables, maternal negative feedback was not coded from mother–child interactions collected at Time 2. Finally, paternal psychopathology status was collected via maternal retrospective report at Time 3 and reflected the presence or absence of any psychiatric illness in fathers during toddlers’ lives.
Two primary hypotheses were tested: (a) Paternal psychopathology was expected to moderate the relationship between maternal depression and toddlers’ behavior problems, and (b) negative maternal parenting (negativity, low warmth, and negative feedback) was predicted to mediate associations between maternal depression and toddlers’ behavior problems. In the course of testing these hypotheses, the univariate relationships among maternal depression, paternal psychopathology, and maternal parenting variables were also examined, as well as the relationships between these predictors and toddlers’ adjustment.
METHOD
Participants
One hundred and one mother–toddler dyads participated in a longitudinal study of the effects of maternal depression on toddlers’ self-efficacy. This research project was conducted with approval from the University of Pittsburgh’s Institutional Review Board and in accordance with ethical standards in the treatment of human participants as outlined by the American Psychological Association. Of the 101 mothers, 51 had experienced a clinical depression during their toddlers’ lives and 50 had never been depressed. The majority of mothers composing the depressed group were recruited from a large regional psychiatric hospital and its satellite outpatient clinics. The majority of mothers in the nondepressed control group were recruited from a large urban obstetrics hospital. All mothers in the depressed group met Diagnostic and Statistical Manual of Mental Disorders (4th ed. [DSM–IV]; American Psychiatric Association, 1994) criteria for a depressive disorder within the first 18 months of their toddlers’ lives that interfered with their functioning to the point they all sought outpatient psychiatric treatment for depression (therapy, medication, or a combination of both). Of these mothers, 75.5% experienced the onset of their depressive episode within the first 6 months of their infants’ lives. Relatively fewer mothers experienced depression when their infants were 7 to 12 months of age (11.8%) and 13 to 18 months of age (13.7%). Of mothers who experienced depression, 13% received psychotherapy only, 11% chose to take antide-pressant medication only, and 76% opted for combination treatment (therapy and medication). A small percentage of mothers in the depressed group experienced an episode of depression so severe that they were admitted to an inpatient psychiatric hospital for treatment (14%, n= 7).
Mothers were excluded from the nondepressed control group if they met criteria for MDD since the birth of their child or at any time in their lives, or met criteria for any other Axis I disorder in the past 5 years. Mothers were excluded from both depressed and nondepressed groups if they met diagnostic criteria for schizophrenia, bipolar disorder, or any substance use disorder.
Mothers in both the depressed and nondepressed control groups were matched on SES (Hollingshead, 1975), minority status (ethnicity), parity (number of pregnancies), and marital status. Mothers participating in the study were predominantly middle class (mean Hollingshead score = 1.96, SD = 1.04). However, the full range of SES levels (1–5) was represented, with lower scores representing higher SES. Families in both the depressed and nondepressed groups were predominantly of nonminority ethnicity (96% Caucasian, 3% African American, and 1% Latin American), and from intact families (94% of fathers living with toddlers), with one or two children in the home (78%). Eighty-three percent of parents had attained an educational level beyond high school (partial college or specialized training, college, or graduate degrees). Toddlers in the sample consisted of 44 girls and 57 boys, all from healthy, singleton births. None of the toddlers had known disabilities, significant developmental delays or major medical illnesses at the time of recruitment. Table 1 outlines additional demographic characteristics of the sample based on maternal depression status upon entry to the study (Time 1).
TABLE 1.
Demographic Characteristics of Maternal Depression Groups at Time 1
| Control a | Past MDDb | Current MDDc | Statistic | |
|---|---|---|---|---|
| Maternal Age | 33.7 (4.6) | 34.0 (6.7) | 34.1 (4.0) | F(2, 98) = 0.06 |
| Paternal Age | 34.8 (4.6) | 35.1 (5.5) | 35.6 (7.7) | F(2, 91) = 0.14 |
| Maternal Education | 15.8 (1.8) | 15.3 (1.8) | 15.0 (1.9) | F(2, 98) = 1.60 |
| Paternal Education | 15.2 (2.1) | 15.9 (2.1) | 14.6 (2.0) | F(2, 97) = 2.28 |
| No. of Children | 1.72 (0.8) | 1.67 (0.7) | 2.0 (0.8) | F(2, 98) = 1.80 |
| Birth Order, % First-Born | 50.0% | 48.0% | 25.0% | χ2(6, N = 101) = 6.03 |
| Maternal Employment, Time 1 | 62.0% | 44.4% | 50.0% | χ2(2, N = 101) = 2.43 |
| Nonmaternal Care, % Center Care | 41.9% | 41.7% | 16.7% | χ2(2, N = 55) = 2.57 |
| Marital Status, % Married | 84.0% | 88.9% | 81.2% | χ2(4, N = 101) = 4.69 |
| Paternal Psychopathology in Toddlers’ Lives | 16.0% | 33.3% | 41.7% | χ2(2, N = 101) = 6.27* |
| Maternal BDI score, Time 1 | 4.0 (3.5)b | 6.4 (5.1)b | 19.7 (8.9)a | F(2, 96) = 63.79** |
| Months in Therapy, Time 1 | 0.00a | 5.8 (5.9)b | 7.5 (6.4)b | F(2, 98) = 30.25** |
| Months on Medication, Time 1 | 0.00a | 9.5 (7.3)b | 8.00 (6.5)b | F(2,98) = 41.33** |
Note. Values are M (SD) or % unless noted. Means with different subscripts are significantly different (Least Significant Difference). MDD =Major Depressive Disorder; BDI = Beck Depression Inventory (A. T. Beck, Ward, Mendelson, Mock, & Erbaugh, 1961).
n =50.
n =27.
n =24.
p < .05.
p < .01.
Procedure
All mothers provided informed consent prior to participating in this longitudinal study. Data for the longitudinal study were collected at three time points (Time 1–3), when toddlers were approximately 18, 25, and 34 months of age. At Time 1, master’s-level interviewers administered the Structured Clinical Interview for DSM–IV Axis 1 Disorders (SCID-IV; First, Gibbon, Spitzer, & Williams, 1995) to assess mothers’ lifetime psychiatric history, episode(s) of major depression since the birth of the study child, and current depressive symptoms. After this interview, mothers engaged in a 5-min teaching task with their toddlers that were videotaped for later observational coding. A laboratory playroom visit was also conducted during which mothers and their toddlers participated in a battery of observational measures of attachment, joint-attention, persistence, and mastery motivation were videotaped for later behavioral coding and analyses and have been described in other publications (Dietz, Jennings, & Abrew, 2005; Henderson & Jennings, 2003; Jennings, 2004; Jennings & Abrew, 2004; Kelley & Jennings, 2003).
For both follow-up assessments (Times 2–3), the affective disorder module from the SCID-IV was repeated to determine whether mothers experienced any episodes of depression in the previous data collection visit and to index current maternal depressive symptoms. After these interviews, mothers again were videotaped interacting with their toddlers in a 5-min teaching task with their toddlers. At Time 3, mothers were also administered a semistructured diagnostic interviews about psychiatric disorders in toddlers’ biological fathers and a laboratory playroom visit was completed during which toddlers’ mental development was assessed and mothers completed rating of toddlers’ behavior problems.
Measures
Maternal depression status
Maternal psychiatric history was assessed using the SCID-IV (First et al., 1995). Although the reliability and validity of the SCID-IV has not been reported, an earlier version of this instrument, the SCID-III-R, produced reliability coefficients of 0.61 and 0.68 for current and lifetime Axis I diagnoses (Williams et al., 1992). The SCID-IV yields a categorical diagnostic status of (a) absent, (b) subthreshold, and (c) threshold for mood disorders, anxiety disorders, psychotic disorders, substance abuse disorders, eating disorders, and adjustment disorders. Interrater reliability for diagnosing depression in mothers was excellent (κ = .98).
At Time 1, three diagnostic groups were defined: (a) never depressed group, mothers with no history of MDD and no current depressive symptoms (n = 50); (b) past MDD group, mothers who experienced a depressive episode in the first 18 months of their toddlers’ lives but were not currently depressed (n = 27); and (c) current MDD group, mothers who experienced an episode of depression in the first 18 months of their toddlers’ lives and were currently experiencing a sub-threshold or threshold depression (n = 24).
Paternal psychopathology
The Family Informant Schedule and Criteria for DSM–IV (Schleyer & Mannuzza, 1995), an interview derived from the Family History-Research Diagnostic Criteria (Endicott, Andreasen, & Spitzer, 1978), was used to assess fathers’ psychiatric history at Time 3. These semistructured diagnostic interviews have been used extensively in epidemiological and family studies of psychopathology (e.g., Klein, Lewinsohn, Seeley, & Rohde, 2001; Kovacs, Devlin, Pollack, Richards, & Mukerji, 1997; Williamson et al., 1995), with good reliability of diagnostic modules (κ =0.46–0.98) and validity (percent agreement of 87% as compared to interviewing family members directly; Andreasen, Endicott, Spitzer, & Winokur, 1977). Mothers reported on fathers’ symptoms of mood, anxiety, and substance disorders, as well as antisocial personality disorder. Clinical interviewers determined individual symptom ratings for each disorder and established paternal diagnosis for each disorder on a 4-point scale, ranging 1 (absent), 2 (possible diagnosis), 3 (probable diagnosis), and 4 (definite diagnosis). Using videotaped interviews, satisfactory interrater reliability was obtained (average κ = .81).
Twenty-seven percent (27%; n =27) of toddlers’ fathers met diagnostic criteria for at least one psychiatric disorder during toddlers’ lives based on maternal report of fathers’ symptoms on the Family Informant Schedule and Criteria for DSM–IV. The majority of fathers met diagnostic criteria for an internalizing disorder, with 67% (n = 18) meeting criteria for a mood and/or anxiety disorder during toddlers’ lives. Only one third of fathers (n = 9) met criteria for an externalizing disorder, mostly consisting of substance use disorders with comorbid conduct or antisocial personality disorders. A dichotomous measure of paternal psychopathology was established because the low number of fathers meeting criteria for an externalizing disorder prohibited a comparison of paternal psychopathology by type of disorder. However, removing the nine fathers who did not have any internalizing psychopathology from subsequent analyses did not change the results presented in this article.
Mother–child interactions
Maternal parenting behavior was assessed during a videotaped interaction with their toddlers conducted in dyads’ homes at Times 1 to 3. Mothers and toddlers were presented with an attractive but challenging toy. Mothers were prompted to “help toddlers complete the task.” Mothers interacted with their toddlers for 5 min. Indices of Maternal Negativity and Maternal Warmth were coded from mother–child interactions at all three data collection periods using a coding system developed for this project (see Kelley & Jennings, 2003). Maternal Negativity was defined as any behaviors displaying maternal hostility, rejection, and/or unresponsiveness (e.g., negative tone of voice, anger, annoyance, frustration, aggressive touches, and withdrawal from interaction). Maternal Warmth was defined as behaviors that imply acceptance and sensitivity toward toddlers (e.g., praise and encouragement, smiles, and affectionate touches) and that evidence involvement in toddlers’ actions. Maternal Negativity and Maternal Warmth were coded on separate 4-point scales, with higher scores indicating higher levels of negativity or warmth. Ratings of Maternal Negativity and Maternal Warmth were made every 30 sec and were averaged across the number of intervals in which mothers and toddlers interacted with the toy. Coders blinded to maternal depression status achieved satisfactory interrater reliability for both indices of maternal behavior on 20% of the sample at Times 1 to 3 (average κ = 0.71, Maternal Negativity; average κ = .75, Maternal Warmth).
In addition, the frequency of Maternal Negative Feedback toward toddlers’ efforts to master the challenging task was coded for interactions at T1 and T3 to assess maternal evaluative feedback and helpless behaviors in toddlers using a coding system developed for this study (Kelley & Jennings, 2003). Maternal Negative Feedback was operationalized as any verbalization indicating that the toddlers were incorrect in their actions, or statements that were negative about toddlers’ efforts in mastering the task (e.g., “No,” “That’s not where the piece goes,” “That’s the wrong key,” “You can’t get it that way,” and “It doesn’t go in there”). Although all mothers were expected to use some negative feedback to guide their toddlers’ efforts to master the teaching task, it was predicted that our sample of middle-class mothers would rely on more positive strategies and esteem-enhancing feedback to encourage toddlers’ persistence (Hart & Risley, 1995). Hence, higher rates of maternal negative feedback were posited to represent an aspect of criticism in mother–child interactions.
The frequency of Maternal Negative Feedback was also coded in 30-sec intervals for the length of the 5-min interaction by trained coders who were unaware of mothers’ psychiatric history. A single score for Maternal Negative Feedback was calculated by dividing the total frequency by the number of 30-sec intervals coded (≤10). Satisfactory interrater reliability was established on 20% of the sample (percentage agreement = 75; Spearman correlation of .95).
Toddlers’ adjustment
The Externalizing and Internalizing Problems subscales of the Child Behavior Checklist for Ages 2–3 (CBCL; Achenbach, 1992) were used to measure toddlers’ adjustment, based on a strong empirical precedent of using these subscales to index early behavior problems (C. T. Beck, 1999; Campbell, Shaw, & Gilliom, 2000). The CBCL 2–3 has good test–retest reliability (r = .87), and has demonstrated discriminant validity (i.e., children referred for mental health services scored higher than nonreferred children on all scales) and predictive validity for t scores greater than 70 to correspond with the presence of externalizing or internalizing disorders (Achenbach, 1992; Achenbach, Edelbrock, & Howell, 1987).
At Time 3, mothers completed this 99-item questionnaire by rating their toddlers’ behavior during the past 2 months on a 3-point scale, ranging from not at all true to very true or often. The t scores from the CBCL Externalizing and Internalizing Problems subscales were derived from a computer coding program and used in subsequent analyses. Although strongly correlated (r =.71), both indices of toddlers’ behavior problems were examined as separate outcomes to determine whether maternal depression was more likely to be associated with Externalizing or Internalizing behavior problems in this sample of young toddlers.
Statistical Analyses
Prior to analyses, all variables were examined for normality, missing values, and outliers. Outliers were examined using measures of influence (DFFITS and DFBETAS; Cohen, Cohen, West, & Aiken, 2003, pp. 402–405), and 3 participants were missing data on Time 2 indices of maternal negativity and warm, thus sample sizes varied from 98 to 101 depending on the analysis/model. Because there was a strong positive skewness in the Maternal Negativity data that could not be corrected with log or square-root transformations, we dichotomized codes into No Maternal Negativity (87% of sample) and Some Maternal Negativity (13% of sample). Because the pattern of findings was similar when using this dichotomized variable, we opted to use the original codes for Maternal Negativity for ease of interpretation. A square-root transformation was used to successfully correct for positive skewness in the frequency data for Maternal Negative Feedback.
Three sets of multiple regression analyses were conducted to examine Maternal Negativity, Maternal Warmth, and Maternal Negative Feedback as mediators of the relationship between mothers’ depression at Time 1 and toddlers’ Externalizing behavior problems at Time 3. Another set of three multiple regression analyses tested each of these proposed mediators on the relationship between maternal depression at Time 1 and toddlers’ Internalizing behavior problems at Time 3. Because there were significant associations between Time 1 and Time 2 indices of Maternal Negativity (r =.42, p < .05) and Maternal Warmth (r =.57, p < .05), and between Time 1 and Time 3 indices of Maternal Negative Feedback (r =.19, p ≤.06), Time 1 indices of mother–child interaction variables were included as covariates in these multiple regression analyses. Separate multiple regression analyses examined paternal psychopathology as a moderator of mother’s depression on toddlers’ Externalizing and Internalizing behavior problems. In all regression analyses two dummy coded variables (see Cohen et al., 2003, p. 303) were used to compare the effects of maternal depression, specifically in mothers with either (a) a past MDD diagnosis or (b) a current MDD diagnosis at Time 1, with never depressed mothers.
RESULTS
Preliminary Analyses
Analyses were conducted to determine whether demographic or child-specific variables would be significant covariates in subsequent analyses. Demographic covariates, including SES, minority status, toddler sex, number of children in the home, birth order, maternal employment status, and nonmaternal care, were not significantly associated with maternal depression group, paternal psychopathology status, or the CBCL Externalizing or Internalizing subscales. However, SES (r =.46, p < .000) was significantly associated with Maternal Negativity, suggesting mothers with lower SES demonstrated higher negativity toward their toddlers. Similarly, SES (r = −.22, p < .05) and minority status (r =−.22, p < .05) were significantly related to Maternal Warmth, indicating that mothers of higher SES exhibited higher warmth and ethnic/racial minority mothers demonstrated lower levels of warmth toward their toddlers. These covariates were controlled for in subsequent mediator analyses. In addition, the number of children in the home and toddlers’ birth order were significantly associated with higher levels of Maternal Negativity and Maternal Negative Feedback and associated with lower levels of Maternal Warmth. Because these variables were collinear (r =.98, p < .000), only the number of children in the home was controlled for in mediation subsequent analyses. No significant associations were found between the two indices of toddlers’ behavior problems and SES, toddler sex, minority status, number of children in the home, birth order, maternal employment status, nonmaternal care, and the Mental Development Index from Bayley Scales of Infant Development (Bayley, 1993).
Descriptive Statistics
Descriptive statistics for the three maternal parenting variables and toddlers’ Externalizing and Internalizing behavior problems are provided in Table 2. Table 2 also provides the mean and standard deviations by maternal depression group and indicates significant group differences in these variables as determined by analysis of variance. A significant relationship between maternal depression status and paternal psychopathology status during toddlers’ lives was found, χ2(2, N =101) =6.27, p < .05. Specifically, 41% of mothers who experienced current depression at Time 1 reported that toddlers’ fathers also experienced at least one clinically significant psychiatric disorder during toddlers’ lives, compared with only 16% of the spouses of never depressed mothers.
TABLE 2.
Descriptive Statistics (M, SD) for Potential Mediator and Outcome Variables
| Controla | Past MDDb | Current MDDc | Statistic | |
|---|---|---|---|---|
| Maternal Negativity | 1.01 (0.01)b | 1.02 (0.01)b | 1.06 (0.01) a | F(2, 94)=5.14** |
| Maternal Warmth | 2.93 (0.57) | 2.89 (0.60) | 2.70 (0.72) | F(2, 93)=0.06 |
| Maternal Negative Feedback | 1.66 (0.52) | 1.55 (0.49) | 1.75 (0.55) | F(2, 97)=0.50 |
| CBCL Externalizing Behavior Problems | 46.54 (6.67) | 48.81 (9.23) | 50.67 (11.84) | F(2, 100)=1.89 |
| CBCL Internalizing Behavior Problems | 44.52 (7.62)b | 44.19 (9.38)b | 49.46 (10.54)a | F(2, 100)=2.99† |
Note. Means with different subscripts are significantly different (Least Significant Difference). MDD = Major Depressive Disorder; CBCL = Child Behavior Checklist 2–3 (Achenbach, 1992; Achenbach et al., 1987).
n =50.
n =27.
n =24.
p < .10.
p < .05.
p < .01.
Tests of Moderation
Two multiple regression analyses were conducted to test the hypothesis that paternal psychopathology would moderate the effects of current or past maternal depression at Time 1 on toddler’s Externalizing or Internalizing behavior problems at Time 3. Two interaction terms, the products of paternal psychopathology and each of the dummy-coded variables representing current or past maternal depression status at Time 1, were entered into Step 2 of each regression model. Paternal psychopathology was centered (−0.27 = no, 0.73 = yes) to reduce nonessential multicollinearity introduced by the interaction terms (see Aiken & West, 1991).
For toddlers’ Externalizing behavior problems, results yielded a significant interaction between paternal psychopathology and mothers’ past MDD diagnosis (B =13.08, SE =4.89), t(100) =2.68, p < .01, but not between paternal psychopathology and mothers’ current MDD diagnosis. The significant interaction was probed to test the simple slopes and determine the nature of the interaction (see Table 3 for mean CBCL scores by cell). Simple slopes were estimated and tested using methods described by Aiken and West (1991) for probing interactions in regression that contain dichotomous variables (see pp. 130–131). In short, the beta coefficient (simple slope) for the effect of maternal depression on toddler’s Externalizing behavior was reestimated in two new regression equations. In these equations each of the paternal psychopathology groups was recoded to 0 (the opposing group was recoded to 1) and a new interaction term was calculated and included in the corresponding model. Results showed that in the presence of paternal psychopathology, mother’s history of depression was significantly associated with toddlers’ externalizing behavior problems (B = 11.49, SE = 4.16), t(100) =2.76, p < .01, whereas in the absence of paternal psychopathology, mothers’ history of depression was not significantly associated with toddlers’ externalizing behavior problems (B =−1.62, SE =2.41), t(100) = −0.67, ns. Hence, there were significant effects of maternal depression at Time 1 on toddlers’ externalizing behavior problems at Time 3 only when fathers also have a psychiatric diagnosis (see Figure 1).
TABLE 3.
Mean (SD) Toddlers’ Externalizing and Internalizing Behavior Problems Score by Maternal Depression at Time 1 and Paternal Psychopathology
| Paternal Psychopathology Absent | Paternal Psychopathology Present | |
|---|---|---|
| No Maternal Depression | 46.95 (6.5) | 44.38 (7.7) |
| 45.29 (7.4) | 40.50 (7.9) | |
| Past Maternal Depression | 45.33 (6.7) | 55.78 (10.0) |
| 42.00 (7.3) | 48.56 (11.9) | |
| Current Maternal Depression | 49.57 (13.5) | 52.20 (9.6) |
| 47.14 (11.9) | 52.70 (7.7) |
Note. Nonitalicized values represent toddlers’ Externalizing behavior problems scores; italicized values represent toddlers’ Internalizing Child Behavior Checklist (Achenbach, 1992; Achenbach et al., 1987).
FIGURE 1.
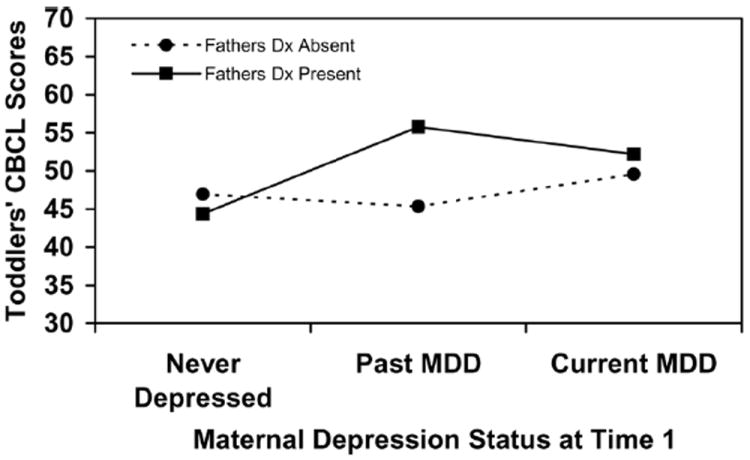
Paternal psychopathology moderates the association between past maternal depression at Time 1 and toddlers’ externalizing behavior problems at Time 3. CBCL = Child Behavior Checklist for Ages 2–3; Dx =diagnosis; MDD = Major Depressive Disorder.
Significant interactions between paternal psychopathology and mothers’ current (B = 9.56, SE =4.86), t(100) = 1.96, p =.05, and past depression (B =10.73, SE =4.85), t(100) =2.21, p < .05, were found to predict toddlers’ Internalizing behavior problems (see Figure 2). Examination of the simple slopes for both interactions yielded a similar pattern of results: Current and past indices of maternal depression at Time 1 were only significantly associated with toddlers’ Internalizing behavior problems at Time 3 when fathers’ also had a psychiatric diagnosis (current maternal depression B =12.54, SE =4.03), t(100) =3.117, p < .01; past maternal depression (B =7.61, SE = 4.14), t(100) = 1.84, p < .07. Maternal depression status at Time 1 was not significantly related to toddlers’ Internalizing behavior problems at Time 3 when fathers did not have a psychiatric diagnosis (current maternal depression, B = 2.84, SE = 2.67), t(100) = 1.07, ns; past maternal depression (B = −3.27, SE = 2.39), t(100)=−1.37, ns.
FIGURE 2.
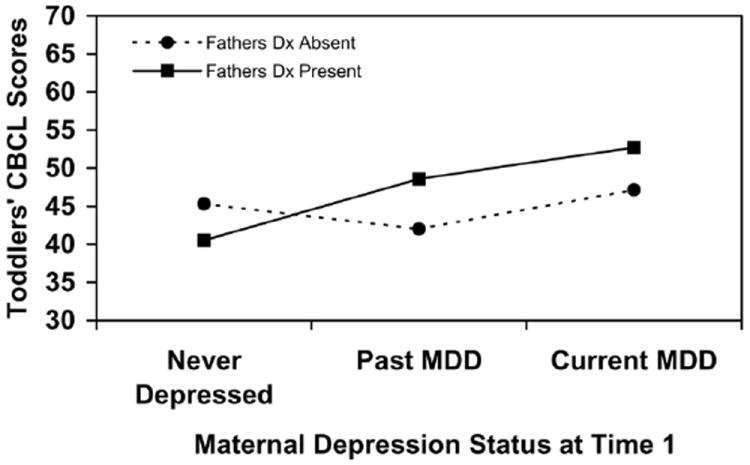
Paternal psychopathology moderates the association between current maternal depression at Time 1 and toddlers’ internalizing behavior problems at Time 3. CBCL = Child Behavior Checklist for Ages 2–3; Dx = diagnosis; MDD = Major Depressive Disorder.
Tests of Mediation
Mediation was tested based on the recommendations of MacKinnon and colleagues (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002), such that (a) there is a significant relationship between the predictor variable and the proposed mediator (path a), (b) there is a significant relationship between the proposed mediator and outcome variable (path b), and (c) the indirect effect or product of these two pathways (a × (b) is also significant. The “product of coefficients” method used to test the significance of the mediated effect (originally proposed by Sobel, 1982) was recommended in lieu of traditional Baron and Kenny (1986) procedures which have been shown to have low power to test mediating effects (see MacKinnon et al., 2002). The product of coefficients method was tested by approximating a Z score, representing the product of the unstandardized betas divided by its standard error (MacKinnon et al., 2002).
Three sets of regression analyses were conducted to test whether each of the proposed mediators (e.g., Maternal Negativity, Maternal Warmth, Maternal Negative Feedback) significantly accounted for any relationship between maternal depression at Time 1 and toddlers’ Externalizing or Internalizing Behavior Problems at Time 3. First, the a paths in each of the models were estimated by regressing each of the proposed mediators on the dummy-coded variables representing mothers’ current and past MDD at Time 1. Next, the b paths were tested by regressing each of the Time 3 outcome variables (e.g., toddlers’ Externalizing and Internalizing Behavior Problems) on the two dummy-coded variables representing mothers’ current and past MDD at Time 1 and each of the proposed mediators (e.g., Maternal Negativity, Maternal Warmth, Maternal Negative Feedback). For analyses involving maternal negativity, the total number of children in the home and SES at Time 1 were included as covariates. Total number of children in the home, SES, and minority status were controlled for in analyses with maternal warmth. Last, total number of children in the home was included as a covariate in analyses involving maternal negative feedback.
Mothers’ current depression at Time 1 was significantly associated with Maternal Negativity at Time 2 (path a; B =0.05, SE =0.16), t(97) =3.40, p <.001. Maternal Negativity at Time 2 was significantly associated with toddlers’ Externalizing behavior problems (path b), above and beyond maternal depression status at Time 1 and other covariates in the model (see Table 4). Thus, results indicated that paths a and b were significant for mothers’ current depression at Time 1. The mediated effect was estimated by calculating the product of the unstandardized beta coefficients that represent path a and path b (a × b). Approximate Z scores for the mediated effect was estimated by dividing the product by its standard error (SE (ab)), where SE (ab)2 =SE (a)2 × (b)2 + SE (b)2 × (a)2 (see MacKinnon et al., 2002). Results showed that the z score was significant (z =2.34, p < .05) supporting the hypothesis that Maternal Negativity at Time 2 was a significant mediator of the relationship between mothers’ depression at Time 1 and toddlers’ Externalizing behavior problems at Time 3. Maternal Negativity at Time 2 was not significantly associated with toddlers’ Internalizing behavior problems (path b) and could not be tested as a mediator of the relationship between maternal depression status at Time 1 and toddlers’ Internalizing problems at Time 3.
TABLE 4.
Regression of Toddlers’ Externalizing Behavior Problems (Time 3) on Maternal Depression Status (Time 1) and Maternal Negativity (Time 2)
| Unstandardized B | SE B | t Value (df =97) | p | |
|---|---|---|---|---|
| Step 1 | ||||
| Past Maternal Depressiona | 2.18 | 2.16 | 1.01 | ns |
| Current Maternal Depressiona | 3.68 | 2.37 | 1.55 | ns |
| Maternal Negativity (Time 1) | 22.62 | 14.05 | 1.61 | ns |
| Socioeconomic Status | −0.03 | 0.99 | −0.03 | ns |
| No. of Children in Home | −0.28 | 1.21 | −0.23 | ns |
| Step 2 | ||||
| Maternal Negativity (Time 2) (Path b) | 48.92 | 15.04 | 3.25 | .002 |
For the effects shown categorical predictor variables were coded based on recommendations by Cohen et al. (2002) such that past maternal depression: 0 =no depression, 0 =current Major Depressive Disorder (MDD), 1 =past MDD; Current maternal depression: 0 =no depression, 1 =current MDD, 0 =past MDD.
Neither current nor past maternal depression at Time 1 was significantly associated with Maternal Warmth at Time 2 (path a). Similarly, Maternal Warmth at Time 2 did not predict toddlers’ Externalizing or Internalizing behavior problems at Time 3 (path b). Hence, the conditions were not satisfied to consider Maternal Warmth as a mediator of the relationship between maternal depression status at Time 1 and toddlers’ behavior problems at Time 3.
No significant relationship emerged between current maternal depression at Time 1 and Maternal Negative Feedback at Time 3 (path a). However, Maternal Negative Feedback was significantly associated with toddlers’ Externalizing behavior problems (path b), above and beyond maternal depression status at Time 1 and other covariates included in the model (R =.40, R2 =.16, Δ in R2 =.08, p < .01). Similarly, Maternal Negative Feedback was also significantly associated with toddlers’ Internalizing behavior problems at Time 3 (R =.43, R2 =.19, Δ in R2 =.05, p < .05). Still, Maternal Negative Feedback did not mediate the relationship between maternal depression status at Time 1 and toddlers’ behavior problems at Time 3.
DISCUSSION
These results are consistent with the hypothesis that adverse outcomes in children exposed to maternal depression are also dependent upon the presence or absence of paternal psychopathology (Goodman & Golib, 1999). Mothers who experienced depression in their toddlers’ lives were more likely to have spouses/partners who also experienced psychopathology in their toddlers’ lives, a finding that is consistent with numerous epidemiological studies that suggest the reciprocal influence of psychiatric illness on spouses (Dierker et al., 1999; Merikangas, 1984). As predicted, paternal psychopathology moderated the effects of maternal depression on toddlers’ behavior problems: Toddlers were more likely to have higher rates of behavior problems in the case where fathers have met criteria for a psychiatric illness and mothers have a history of depression at some point since the toddlers’ birth. However, it is important to note that these mean scores on the CBCL were within the normal range and not indicative of a psychiatric disorder. The absence of paternal psychopathology, however, was related to lower scores of behavior problems in toddlers whose mothers had experienced a past episode of depression but were not currently depressed.
Although similar findings have been reported in samples of older children and adolescents (Brennan, Hammen, Katz, & Le Brocque, 1999; Goodman et al., 1993), this study adds to the developmental psychopathology literature by demonstrating the importance of fathers’ mental health history in assessing the effects of maternal depression on young children. These findings point to the presence of psychopathology in fathers as a risk factor for toddlers’ externalizing behavior problems when mothers have been previously depressed, and for toddlers internalizing problems when mothers have either a history of or current depressive symptoms. In addition, this study is among the few that have investigated paternal internalizing disorders as a moderator of the relationship between maternal depression and young children’s behavior problems. Although paternal substance use disorder and antisocial personality disorder have been studied more extensively (see Phares, Fields, Kamboukos, & Lopez, 2005), parental depression and/or anxiety may also present risk for toddlers’ behavior problems when mothers have a history of MDD. Paternal psychopathology may increase the likelihood of behavior problems in at-risk toddlers directly, as depressed and/or anxious fathers may provide inconsistent and permissive parenting, or indirectly, if they are less involved with caring for their children and leave depressed mothers sole responsibility for the daily behavioral management of toddlers.
Furthermore, maternal negativity was identified as a significant mediating pathway by which maternal depression predicted toddlers’ externalizing behavior problems. Higher levels of maternal negativity were significantly related to mothers’ current depressive symptoms, suggesting that maternal depression may manifest in high levels of irritability, which may be communicated to young children through mother–child interactions. High levels of negativity in the context of mother–child interactions may exacerbate young children’s non-compliance and poor emotion regulation and may negatively affect children’s emotional adjustment and behavioral problems in a manner similar to high levels of maternal criticism (Asarnow, Tompson, Hamilton, Goldstein, & Guthrie, 1994; Goodman et al., 1994; Hirshfeld, Biederman, Brody, Faraone, & Rosenbaum, 1997). Maternal warmth did not differ between never depressed, past depressed, and current depressed mothers at Time 1 and did not mediate the relationship between maternal depression and later toddler behavior problems. This finding may suggest that positive aspects of maternal parenting are less influenced by maternal depression status and that maternal warmth may not be a strong pathway through which maternal depression negatively influences behavior problems in toddlers. Although maternal negative feedback at Time 3 did not mediate the relationship between maternal depression status at Time 1 and toddlers’ behavior problems at Time 3, it remained a significant, concurrent predictor of toddlers’ externalizing and internalizing problems. This suggests that high levels of concurrent maternal negative feedback are associated with toddlers’ behavior problems, above and beyond early exposure to maternal depression.
Findings from our study support the use of various indices of maternal depression for examining relationships between parental risk factors and toddlers’ maladjustment. Residual maternal depressive symptoms at Time 1, rather than a past episode of MDD, predicted more maternal negativity in mother–child interactions 7 months later (Time 2), suggesting that maternal negativity toward toddlers are more influenced by residual, more continuous symptoms of depression. Maternal negativity may be significantly reduced when mothers’ depressive symptoms remit, as evidenced by the comparable levels of negativity observed in mothers who experienced past episodes of MDD but were not currently depressed at Time 1 and mothers with no history of MDD. Similarly, there was a significant interaction between paternal psychopathology and residual maternal depression at Time 1 in predicting toddlers’ Internalizing behavior problems at Time 3.
In contrast, two significant interactions emerged between paternal psychopathology and past episodes of maternal depression in predicting toddlers’ externalizing and internalizing behavior problems. One interpretation of these findings suggest that maternal history of depression remains a salient risk factor for negative outcomes in young children, particularly in situations where there is an increased family loading for psychopathology, regardless of whether mothers experience residual depressive symptoms. However, this finding may be spurious and better accounted for by other correlates of paternal psychopathology, such as marital conflict (see Davies, Harold, Goeke-Morey, & Cummings, 2002).
Limitations of This Study
The primary limitation of our study is that maternal report was used to obtain indices of maternal depression at Time 1 and paternal psychopathology status at Time 3, as well as the outcome measures of toddler behavior problems at Time 3. Data from multiple informants are necessary to reduce the likelihood of single reporter bias, particularly with depressed mothers (Chilcoat & Breslau, 1997). However, there was no evidence of a pervasive negative bias in depressed mothers’ reports of paternal psychopathology and toddlers’ behavior problems. This may be related to the fact that the majority of mothers with a previous history of MDD were not currently depressed at the time these data were collected (67%). Although recently depressed mothers (and mothers with a history of MDD) reported higher rates of paternal psychopathology, recently depressed mothers did not rate their children as having higher rates of behavior problems than never depressed mothers. In addition, a significant correlation in the predicted direction between the observational measure of maternal negativity and maternal negative feedback during mother–child interaction and CBCL ratings suggest that mothers’ ratings of toddlers’ behavior problems were not simply a result of a negative reporting bias. Furthermore, regression analyses controlling for maternal depression status at Time 1 continued to yield significant relationships between paternal psychopathology, maternal behavior during mother–child interactions, and toddlers’ behavior problems.
Depressed mothers may still provide researchers valid information about children and family environments (Biederman, Mick, & Faraone, 1997; Ingersoll & Eist, 1998). For example, the validity of maternal reports of paternal psychopathology is supported and is a frequently used methodology in family studies of psychopathology (Caspi et al., 2001). Despite the concern that maternal of report of fathers’ psychiatric history may inflate effects, maternal report have been found to provide more conservative estimates of paternal psychopathology than fathers’ self-report (Connell & Goodman, 2002). Thus, the findings presented in our study may underestimate, rather than overestimate, the effects of paternal psychopathology on toddlers’ behavior problems.
An additional limitation of our study is its generalizability to community samples of depressed mothers. The majority of mothers described in this article evidenced depressive symptoms so severe that they sought psychiatric treatment in the first 6 months of their infants’ lives and opted for a combination of psychotherapy and antidepressant medication to reduce their emotional distress and functional impairment. As the larger population of depressed mothers typically does not seek psychiatric treatment, one possibility is that the results presented in our study overestimate the negative affects of maternal depression on later toddlers’ externalizing and internalizing problems. However, depressed mothers who do not seek psychiatric treatment may have formidable psychosocial barriers that prevent them from receiving help and may still evidence severe symptoms that interfere with sensitive and effective parenting. Indeed, the clinical sample of mothers in this study had high education levels and consisted of predominantly middle to high socioeconomic status, which may have facilitated their receipt of treatment for depression.
Implications for Research, Policy, and Practice
Maternal depression and co-occurring family risk factors contribute to increased behavior problems in young children. In our study, negative maternal feedback mediated the effects of current maternal depression on toddlers’ behavior problems. Toddlers who experienced both maternal depression and paternal psychopathology in their lives had the highest scores of behavior problems. These findings suggest the importance of investigating other risks associated with maternal depression, particularly those in the family context. These results also argue for examining maternal negativity in the context of mother–child interactions and paternal psychopathology as respective mediators and moderators of maladjustment of young children who have experienced maternal depression.
Findings from this study also support the use of early psychosocial clinical interventions that target negative interaction styles in mothers who have experienced a postpartum depression to decrease toddlers’ risk for later behavioral problems. Existing parent training programs, such as Parent-Child Interaction Therapy (Eyberg, Boggs, & Algina, 1995), Incredible Years Program (Webster-Stratton & Hammond, 1997), and the Home Visiting Family Support Program (Lyons-Ruth & Melnick, 2004), are examples of empirically-supported therapies for preschool children experiencing emotional and behavior problems. Although they do not address maternal depression or paternal psychopathology specifically, each are flexible enough to accommodate some discussion of how parental mood may affect negativity toward toddlers and increased negative feedback. Cicchetti and colleagues’ Toddler–Parent Psychotherapy (Cicchetti, Rogosch, & Toth, 2000; Toth, Rogosch, Manly, & Cicchetti, 2006) is another example of a psychosocial treatment for improving the attachment security of toddlers with depressed mothers. Future directions for intervention include an integrated psychosocial treatment that addresses and reduces both maternal depression and behavior problems in toddlers.
Acknowledgments
This research was supported in part by a grant from the National Institute of Mental Health (MH49419). We thank the mothers and toddlers who participated in the study and David Brent for feedback on the manuscript.
Contributor Information
Laura J. Dietz, Department of Psychiatry, University of Pittsburgh School of Medicine
Kay Donahue Jennings, Department of Psychology, University of Pittsburgh.
Sue A. Kelley, Department of Psychology, Lycoming College
Michael Marshal, Department of Psychiatry, University of Pittsburgh School of Medicine.
References
- Achenbach TM. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington: University of Vermont; 1992. [Google Scholar]
- Achenbach TM, Edelbrock C, Howell CT. Empirically based assessment of the behavioral/emotional problems of 2- and 3-year-old children. Journal of Abnormal Child Psychology. 1987;15(4):629–650. doi: 10.1007/BF00917246. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method of using diagnostic criteria: Reliability and validity. Archives of General Psychiatry. 1977;34:1229–1232. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Tompson M, Hamilton EB, Goldstein MJ, Guthrie D. Family-expressed emotion, childhood-onset depression, and childhood-onset schizophrenia spectrum disorders: Is expressed emotion a nonspecific correlate of child psychopath-ology or a specific risk factor for depression? Journal for Abnormal Child Psychology. 1994;22:129–146. doi: 10.1007/BF02167896. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bayley N. Bayley Scales of Infant Development. Second Edition. San Antonio, TX: The Psychological Corporation; 1993. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck CT. Maternal depression and child behaviour problems: A meta-analysis. Journal of Advanced Nursing. 1999;29:623–629. doi: 10.1046/j.1365-2648.1999.00943.x. [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick E, Faraone SV. Biased maternal reporting of child psychopathology? Journal of the American Academy of Child and Adolescent Psychiatry. 1997;37(1):10–12. doi: 10.1097/00004583-199801000-00005. [DOI] [PubMed] [Google Scholar]
- Brennan PA, Hammen C, Katz AR, Le Brocque RM. Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Counseling Psychology. 2002;70:1075–1085. doi: 10.1037//0022-006x.70.5.1075. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF. The timing and chronicity of postpartum depression: Implications for infant development. In: Murray P, editor. Postpartum depression and child development. New York: Guilford; 1997. pp. 165–197. [Google Scholar]
- Campbell SB, Cohn JF, Meyers T. Depression in first-time mothers: Mother-infant interaction and depression chronicity. Developmental Psychology. 1996;31:349–357. [Google Scholar]
- Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Development and Psychopathology. 2000;12(3):467–488. doi: 10.1017/s0954579400003114. [DOI] [PubMed] [Google Scholar]
- Carro MG, Grant KE, Gotlib IH, Compras BE. Postpartum depression and child development: An investigation of mothers and fathers as sources of risk and resilience. Development and Psychopathology. 1993;5:567–579. [Google Scholar]
- Caspi A, Moffitt TE, Morgan J, Rutter M, Taylor A, Arseneault L, et al. Maternal expressed emotion predicts children’s antisocial behavior problems: Using monozygotic-twin differences to identify environmental effects on behavioral development. Developmental Psychology. 2004;40:149–161. doi: 10.1037/0012-1649.40.2.149. [DOI] [PubMed] [Google Scholar]
- Caspi A, Taylor A, Smart M, Jackson J, Tagami S, Moffitt TE. Can women provide reliable information about their children’s fathers? Cross-informant agreement about men’s lifetime antisocial behaviour. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2001;42(7):915–920. doi: 10.1111/1469-7610.00787. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Does psychiatric history bias mothers’ reports? An application of a new analytic approach. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(7):971–979. doi: 10.1097/00004583-199707000-00020. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: Contributions to the development of attachment insecurity and behavioral problems in toddlerhood. Developmental Psychopathology. 1998;10:283–300. doi: 10.1017/s0954579498001618. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. The efficacy of toddler-parent psychotherapy for fostering cognitive development in offspring of depressed mothers. Journal of Abnormal Child Psychology. 2000;28:135–148. doi: 10.1023/a:1005118713814. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Schneider-Rosen K. An organizational approach to childhood depression. In: Rutter M, Izard CE, Read PB, editors. Depression in young people: Developmental and clinical perspectives. New York: Guilford; 1986. pp. 71–134. [Google Scholar]
- Cicchetti D, Toth SL. Developmental psychopathology and disorders of affect. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol 2 Risk, disorder and adaptation. New York: Wiley; 1995. pp. 317–349. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Cohn JF, Campbell SB. Influence of maternal depression on infant affect regulation. In: Cicchetti D, Toth S, editors. Rochester Symposium in Developmental Psychopathology: Developmental perspectives on depression. Vol. 4. Rochester, NY: University of Rochester Press; 1992. pp. 103–130. [Google Scholar]
- Cohn JF, Matias R, Tronick EZ, Connell D, Lyons-Ruth K. Face-to-face interactions of depressed mothers and their infants. In: Tronick EZ, Field T, editors. Maternal depression and child development (New Directions for Child Development. 34. San Francisco: Jossey-Bass; 1986. pp. 31–45. [DOI] [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior: A meta-analysis. Psychological Bulletin. 2002;128(5):746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Conrad M, Hammen C. Role of maternal depression in perceptions of child maladjustment. Journal of Consulting and Clinical Psychology. 1989;57:663–667. doi: 10.1037//0022-006x.57.5.663. [DOI] [PubMed] [Google Scholar]
- Cornish AM, McMahon CA, Ungerer JA, Barnett B, Kiwalenko N, Tennent C. Maternal depression and the experience of parenting in the second postnatal year. Journal of Reproductive and Infant Psychology. 2006;24:121–132. [Google Scholar]
- Davies PT, Harold GT, Goeke-Morey MC, Cummings EM. Child emotional security and interparental conflict. Monographs of the Society for Research in Child Development. 2002;67(3):vii–viii. Serial No. 270. [PubMed] [Google Scholar]
- Dierker LC, Merikangas KR, Szatmari P. Influence of parental concordance for psychiatric disorders on psychopathology in offspring. American Academy of Child and Adolescent Psychiatry. 1999;38:280–288. doi: 10.1097/00004583-199903000-00015. [DOI] [PubMed] [Google Scholar]
- Dietz LJ, Jennings KD, Abrew AJ. Social skill in self-assertive strategies of toddlers with depressed and nondepressed mothers. Journal of Genetic Psychology. 2005;166:94–116. doi: 10.3200/GNTP.166.1.94-116. [DOI] [PubMed] [Google Scholar]
- Eiden R, Leonard KE. Paternal alcohol use and the mother-infant relationship. Development and Psychopathology. 1996;8:307–323. [Google Scholar]
- Endicott J, Andreasen NC, Spitzer RL. Family history-research diagnostic criteria. 3. New York: Biometrics Research, New York State Psychiatric Institute; 1978. [Google Scholar]
- Eyberg SM, Boggs SR, Algina J. Parent–child interaction therapy: A psychosocial model for the treatment of young children with conduct problems and their families. Psychopharmacology Bulletin. 1995;31:83–91. [PubMed] [Google Scholar]
- Field T. Infants of depressed mothers. Development and Psychopathology. 1992;4:49–66. doi: 10.1017/s0954579497001260. [DOI] [PubMed] [Google Scholar]
- Field T. Psychologically depressed parents. In: Bornstein M, editor. Handbook of parenting. Vol. 4. Mahwah, NJ: Erlbaum; 1995. pp. 85–99. [Google Scholar]
- Field TM, Hossain Z, Malphurs J. “Depressed” fathers’ interactions with their infants. Infant Mental Health Journal. 1999;20:322–332. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. User’s guide for the Structured Clinical Interview for DSM–IV Axis I Disorders. New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. Oct, [Google Scholar]
- Frankel KA, Harmon RJ. Depressed mothers: They don’t always look as bad as they feel. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:289–298. doi: 10.1097/00004583-199603000-00009. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Adamson LB, Riniti J, Cole S. Mothers’ expressed attitudes: Associations with maternal depression and children’s self-esteem and psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:1265–1274. doi: 10.1097/00004583-199411000-00007. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Brogan D, Lynch ME, Fielding B. Social and emotional competence in children of depressed mothers. Child Development. 1993;64:516–531. doi: 10.1111/j.1467-8624.1993.tb02925.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Hammen CL. Psychological aspects of depression: Towards a cognitive-interpersonal integration. Chichester, England: Wiley; 1992. [Google Scholar]
- Hammen C, Burge D, Stansbury K. Relationship of mother and child variables to child outcomes in a high risk sample: A casual modeling analysis. Developmental Psychopathology. 1990;26:24–30. [Google Scholar]
- Hart B, Risley TR. Meaningful differences in the everyday experiences of young American children. Baltimore: Paul H Brookes Publishing; 1995. [Google Scholar]
- Hay DF, Pawlby S, Angold A, Harold GT, Sharp D. Pathways to violence in the children of mothers who were depressed postpartum. Developmental Psychology. 2003;39:1083–1094. doi: 10.1037/0012-1649.39.6.1083. [DOI] [PubMed] [Google Scholar]
- Hay DF, Pawlby S, Sharp D, Asten P, Mills A, Kumar R. Intellectual problems shown by 11-year-old children whose mothers had postpartum depression. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2001;42:871–889. doi: 10.1111/1469-7610.00784. [DOI] [PubMed] [Google Scholar]
- Henderson EN, Jennings KD. Maternal depression and the ability to facilitate joint attention with 18-month-olds. Infancy. 2003;4:27–46. [Google Scholar]
- Hirshfeld DR, Biederman J, Brody L, Faraone SV, Rosenbaum JF. Associations between expressed emotion and child behavioral inhibition and psychopathology: A pilot study. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:205–213. doi: 10.1097/00004583-199702000-00011. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven, CT: Department of Sociology, Yale University; 1975. [Google Scholar]
- Ingersoll BD, Eist HI. Are depressed mothers biased reporters? Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(7):681. doi: 10.1097/00004583-199807000-00001. [DOI] [PubMed] [Google Scholar]
- Jacquez F, Cole DA, Searle B. Self-perceived competence as a mediator between maternal feedback and depressive symptoms in adolescents. Journal of Abnormal Child Psychology. 2004;32:355–367. doi: 10.1023/b:jacp.0000030290.68929.ef. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Taylor A. Life with (or without) father: The benefits of living with two biological parents depends on the father’s antisocial behavior. Child Development. 2003;74(1):109–126. doi: 10.1111/1467-8624.t01-1-00524. [DOI] [PubMed] [Google Scholar]
- Jennings KD. Development of goal-directed behaviour and related self-processes in toddlers. International Journal of Behavioural Development. 2004;28:319–327. [Google Scholar]
- Jennings KD, Abrew AJ. Self-efficacy in 18-month-old toddlers of depressed and nondepressed mothers. Journal of Applied Developmental Psychology. 2004;25:133–147. [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kelley SA, Jennings KD. Putting the pieces together: Maternal depression, maternal behavior, and toddler helplessness. Infant Mental Health Journal. 2003;24:74–90. [Google Scholar]
- Klein DN, Lewinsohn PM, Seeley JR, Rohde P. A family study of major depressive disorder in a community sample of adolescents. Archives of General Psychiatry. 2001;58:13–20. doi: 10.1001/archpsyc.58.1.13. [DOI] [PubMed] [Google Scholar]
- Kochanska G. Mutually responsive orientation between mothers and their young children: Implications for early socialization. Child Development. 1997;68:94–112. [PubMed] [Google Scholar]
- Kovacs M, Devlin B, Pollack M, Richards C, Mukerji P. A controlled family history study of childhood-onset depressive disorder. Archives of General Psychiatry. 1997;54:613–623. doi: 10.1001/archpsyc.1997.01830190033004. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Melnick S. Dose-response effect of mother-infant clinical home visiting on aggressive behavior problems in kindergarten. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:699–707. doi: 10.1097/01.chi.0000122730.72597.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maccoby EE. The role of parents in socialization of children: An historical overview. Developmental Psychology. 1992;28:1006–1017. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and ‘other intervening variables effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins C, Gaffan EA. Effects of early maternal depression on patterns of infant-mother attachment: A meta-analytic investigation. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2000;41:737–746. [PubMed] [Google Scholar]
- McCarty CA, Lau AS, Valeri SM, Weisz JR. Parent-child interactions in relation to critical and emotionally overinvolved expressed emotion (EE): Is EE a proxy for behavior? Journal of Abnormal Child Psychology. 2004;32:83–93. doi: 10.1023/b:jacp.0000007582.61879.6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon CA, Barnett B, Kowalenko NM, Tennent CC. Maternal attachment state of mind moderates the impact of postnatal depression on infant attachment. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2006;47:660–669. doi: 10.1111/j.1469-7610.2005.01547.x. [DOI] [PubMed] [Google Scholar]
- Merikangas KR. Divorce and assortative mating among depressed patients. American Journal of Psychiatry. 1984;141:74–76. doi: 10.1176/ajp.141.1.74. [DOI] [PubMed] [Google Scholar]
- Nelson DR, Hammen C, Brennan PA, Ulman JB. The impact of maternal depression on adolescent adjustment: The role of expressed emotion. Journal of Consulting and Clinical Psychology. 2003;71:935–944. doi: 10.1037/0022-006X.71.5.935. [DOI] [PubMed] [Google Scholar]
- Pianta R, Erikson MF, Wagner N, Kreutzer T, Egeland B. Early predictors of referral for special services: Child-based measures versus mother–child interaction. School Psychology Review. 1990;19:240–250. [Google Scholar]
- Peris TS, Baker BL. Applications of the expressed emotion construct to young children with externalizing behavior: Stability and prediction over time. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41:457–462. [PubMed] [Google Scholar]
- Phares V, Fields S, Kamboukos D, Lopez L. Still looking for Poppa. American Psychologist. 2005;60:735–736. doi: 10.1037/0003-066X.60.7.735. [DOI] [PubMed] [Google Scholar]
- Radke-Yarrow M, Cummings EM, Kuczynski L, Chapman M. Patterns of attachment in two- and three-year-olds in normal families and families with parental depression. Child Development. 1985;56:884–893. [PubMed] [Google Scholar]
- Schleyer BL, Mannuzza S. Family Informant Schedule and Criteria. New York: Anxiety Disorders Clinic, New York State Psychiatric Institute; 1995. Jan, revised for DSM–IV. [Google Scholar]
- Seifer R, Sameroff AJ, Dickstein S, Keitner G, Miller I, Rasmussen S, et al. Parental psychopathology, multiple contextual risks and one-year outcomes in children. Journal of Clinical Child Psychology. 1996;25:423–435. [Google Scholar]
- Shaw DS, Bell RQ. Developmental theories of parental contributors to antisocial behavior. Journal of Abnormal Child Psychology. 1993;21:493–518. doi: 10.1007/BF00916316. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological methodology 1982. Washington, DC: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- Stein A, Gath D, Bucker J, Bond A, Day A, Cooper P. The relationship between postnatal depression and mother-child interaction. British Journal of Psychiatry. 1991;158:46–52. doi: 10.1192/bjp.158.1.46. [DOI] [PubMed] [Google Scholar]
- Tannenbaum L, Forehand R. Maternal depressive mood: The role of the father in preventing adolescent problem behaviors. Behavior Research & Therapy. 1994;32:321–325. doi: 10.1016/0005-7967(94)90129-5. [DOI] [PubMed] [Google Scholar]
- Toth SL, Rogosch FA, Manly JT, Cicchetti D. The efficacy of toddler-parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: A randomized preventive trial. Journal of Consulting and Clinical Psychology. 2006;74:1006–1016. doi: 10.1037/0022-006X.74.6.1006. [DOI] [PubMed] [Google Scholar]
- Trapolini T, McMahon CA, Ungerer JA. The effect of maternal depression and marital adjustment on young children’s internalizing and externalizing behaviour problems. Child: Care, Health, & Development. 2007;33:794–803. doi: 10.1111/j.1365-2214.2007.00739.x. [DOI] [PubMed] [Google Scholar]
- Vostanis P, Nicholls J, Harrington R. Maternal expressed emotion in conduct and emotional disorders of childhood. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1994;35:365–376. doi: 10.1111/j.1469-7610.1994.tb01168.x. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology. 1997;65:93–109. doi: 10.1037//0022-006x.65.1.93. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Leckman JF, Merikangas KR, Gammon GD, Prusoff BA. Depression and anxiety disorders in parents and children. Results from the Yale family study. Archives of General Psychiatry. 1984;41:845–852. doi: 10.1001/archpsyc.1984.01790200027004. [DOI] [PubMed] [Google Scholar]
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, et al. The Structured Clinical Interview for DSM-III-R (SCID) II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- Williamson DE, Ryan ND, Birmaher B, Dahl RE, Kaufman J, Rao U, et al. A case-control family history study of depression in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1596–1607. doi: 10.1097/00004583-199512000-00010. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Iannotti RJ, Cummings EM, Dedham S. Antecedents of problem behaviors in children of depressed mothers. Developmental and Psychopathology. 1990;2:271–291. [Google Scholar]


