Abstract
With over one-third of pregnancies in the United States being delivered by cesarean and the growing knowledge of morbidities associated with repeat cesarean deliveries, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the Society for Maternal-Fetal Medicine, and the American College of Obstetricians and Gynecologists convened a workshop to address the concept of preventing the first cesarean. The available information on maternal and fetal factors, labor management and induction, and non-medical factors leading to the first cesarean were reviewed as well as the implications of the first cesarean on future reproductive health. Key points were identified to assist with reduction in cesarean rates including that labor induction should be performed primarily for medical indication; if done for non-medical indications, the gestational age should be at least 39 weeks or more and the cervix should be favorable, especially in the nulliparous patient. Review of the current literature demonstrates the importance of adhering to appropriate definitions for failed induction and arrest of labor progress. The diagnosis of “failed induction” should only be made after an adequate attempt. Adequate time for normal latent and active phases of the first stage, and for the second stage, should be allowed, as long as the maternal and fetal conditions permit. The adequate time for each of these stages appears to be longer than traditionally estimated. Operative vaginal delivery is an acceptable birth method when indicated, and can safely prevent cesarean delivery. Given the progressively declining use, it is critical that training and experience in operative vaginal delivery is facilitated and encouraged. When discussing the first cesarean with a patient, counseling should include its effect on future reproductive health.
Cesarean delivery is the most commonly performed major surgery in the United States. Approximately one in three pregnancies are delivered by cesarean, accounting for over one million surgeries each year (1). In 2007, 26.5% of low risk women giving birth for the first time had a cesarean delivery (2). The Healthy People target for 2020 is a cesarean delivery rate of 23.9% in low-risk full term women with a singleton, vertex presentation. This is much higher than the never achieved target cesarean rate of 15% for Healthy People 2010 (3). The appropriate rate of cesarean delivery is not easily determined as it varies according to multiple factors. While “case mix adjustment” for these factors has been proposed, there are limited data on which variables should be included in the adjustment when evaluating variations between individuals or institutions. Primary cesarean is defined as the first cesarean delivery. Given its effect on subsequent pregnancies, an understanding of the drivers behind the increase in primary cesarean delivery rates, and renewed effort to reduce them, may have a substantial effect on health care.
While the dramatic rise in the rate of cesarean delivery since 1995 is due in part to an increase in frequency of primary cesareans, it is also due to a decline in attempted trials of labor after cesarean. Of U.S. women who require an initial cesarean delivery, over 90% will have a subsequent repeat cesarean. Not only does cesarean delivery increase the risk of maternal complications in the index pregnancy, including intraoperative complications, it has serious implications for future gestations. Adhesions of uterus, bowel and bladder can result in trauma at surgery, while abnormal placentation (placenta previa, accreta, increta, percreta) and uterine rupture can be catastrophic for both mother and baby (4). Given the risks associated with the initial cesarean and its implications for subsequent pregnancies, the most effective approach to reducing overall morbidities related to cesarean delivery is to avoid the first cesarean. Incidences of maternal as well as perinatal morbidity and mortality should be kept to the lowest level achievable.
In order to synthesize the available information regarding factors leading to the first cesarean, including obstetric, maternal, and fetal indications for cesarean delivery, labor management and induction practices, and non-medical factors, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the Society for Maternal Fetal Medicine, and the American College of Obstetricians and Gynecologists convened a Workshop on February 7–8, 2012. Workshop participants also reviewed the implications of the first cesarean on future reproductive health, and considered recommendations for practice, opportunities for patient and community education, and potential areas for research, with the goals of determining the scope of the problem and identifying opportunities to reduce unnecessary first cesarean deliveries.
Examining Indications for Primary Cesarean
There are numerous obstetric, fetal, and maternal indications for primary cesarean delivery, some of which may be preventable (Table 1). Importantly, there are very few absolute indications for cesarean, such as complete placenta previa, vasa previa, or cord prolapse. Most indications depend on the caregiver’s interpretation, recommendation, or action in response to the developing situation, therefore making them modifiable and likely target to lower the cesarean rate (Tables 2 to 4). While each individual indication for cesarean delivery makes a finite contribution to the overall primary cesarean delivery rate, a measurable reduction could result if concerted interventions were adopted to avoid each and all unneeded surgeries.
Table 1.
Major Indications for Primary Cesarean Delivery
| Indication | % | |
|---|---|---|
| Prelabor | Malpresentation | 10–15* |
| Multiple gestation | 3 | |
| Hypertensive disorders | 3 | |
| Macrosomia | 3 | |
| Maternal request | 2–8 | |
| In labor | First-stage arrest | 15–30* |
| Second-stage arrest | 10–25 | |
| Failed induction | 10 | |
| Nonreassuring fetal heart rate | 10 |
Data from Zhang J, Troendle J, Reddy UM, Laughon SK, Branch DW, Burkman R, Landy HJ, Hibbard JU, Haberman S, Ramirez MM, Bailit JL, Hoffman MK, Gregory KD, Gonzalez-Quintero VH, Kominiarek M, Learman LA, Hatjis CG, van Veldhuisen P; Consortium on Safe Labor. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol 2010;203:326.e1-326.e10. Epub 2010 Aug 12 and Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol 2011 Jul;118:29–38.
Percentage of all cesareans that have this as a primary indication.
Some indications may occur both prelabor and in labor.
Table 2.
Selected Potentially Modifiable Obstetric Indications for First Cesarean Delivery
| Diagnostic Accuracy* |
Effect on Prevention of First Cesarean Delivery† |
Preventive Strategies | |
|---|---|---|---|
| Failed induction | Limited | Large | See Box 1 and Figure 1 |
| Arrest of labor | Limited | Large | See Box 1 and Figure 2 |
| Multiple gestation | High | Small | - Prevent multiple gestations: Encourage single embryo transfer - Safe trial of labor: training for vaginal twin delivery, simulation for cephalic version or breech extraction of second twin |
| Preeclampsia | High | Small | Education: preeclampsia is not an indication for cesarean delivery |
| Prior shoulder dystocia | Limited | Small | Improved documentation as to prior shoulder dystocia. Education regarding risk of recurrence based on estimated fetal weight. Prior shoulder dystocia is not an absolute indication for cesarean delivery |
| Prior myomectomy | Limited | Small | Improved documentation of prior myomectomy Education regarding impact of myomectomy on delivery. |
| Prior third-degree or fourth-degree laceration, prior breakdown of repair, fistula | High | Small | Education: not an absolute indication for cesarean delivery Education: limited ability to predict recurrence |
| Marginal and low lying placentation | High | Small | Education; attempt at vaginal delivery acceptable as long as placental is 1 cm or more from internal os (38) |
Diagnostic criteria accuracy: how readily and accurately cases can be diagnosed. The ability to diagnose multiple gestations is high, whereas the ability to identify all cases of shoulder dystocia is limited due to difficulty of the definition.
Effect on prevention of first cesarean delivery: Large means that modification of indication (eg, arrest of labor) could lead to a large decrease in cesarean deliveries. Small means that modification of indication (eg, prior shoulder dystocia) could lead to a small decrease in cesarean deliveries.
Table 4.
Selected Potentially Modifiable Maternal Indications for First Cesarean Delivery
| Diagnostic Criteria Accuracy* |
Effect on Prevention of First Cesarean Delivery† |
Strategies to Prevent First Cesarean Delivery |
|
|---|---|---|---|
| Obesity (BMI higher than 40) | High |
Small |
Weight loss preconception, and limited weigh gain in pregnancy Education: obesity is not an indication for cesarean delivery, and is a poor predictor of cesarean delivery |
| Infection (HSV, HCV, HIV) | High | Small | HIV-treatment to minimize viral load |
| Cardiovascular disease (acute HTN crisis, cardiomyopathy, pulmonary HTN, cerebral aneurysm, CVA) | High | Small | Education: not an indication for cesarean delivery |
| Inadequate pelvis | Limited | Small | Education: not an indication for cesarean delivery |
| Request (no maternal, obstetrical or fetal indication) | Not applicable |
Small |
Education of patient and provider regarding acute complications and long term risks, benefits and impact of cesarean on mom and baby. Specific education on fear of labor, etc |
BMI, body mass index; HSV, herpes simplex virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; HTN, hypertension; CVA, cerebrovascular accident.
Diagnostic criteria accuracy: how readily and accurately cases can be diagnosed. The ability to diagnose infection is high, whereas the ability to identify inadequate pelvis is limited due to difficulty of the definition.
Effect on prevention of first cesarean delivery: Small means that modification of indication (eg, infection) could lead to a small decrease in cesarean deliveries.
Patient and physician attitudes as well as their perceptions regarding the risks of vaginal delivery versus cesarean delivery are other potentially modifiable factors. Undue concern about vaginal delivery coupled with relative indifference regarding the risks of cesarean may lead to a decision that is not based on clinical evidence. Whenever cesarean delivery is planned or performed, the patient should be advised of the short and long term risks and benefits of the surgery both for herself and her offspring, present and future. The corollary is that the risks associated with vaginal delivery should be presented in an objective and unbiased manner. The indication for the surgery should be included in the consent and documented in the patient record. A cesarean that is performed without an accepted indication should be labeled as such, i.e. ‘non-indicated cesarean.’ The term ‘elective cesarean’ should be avoided. (5)
In addition to monitoring and providing feedback to clinicians regarding their indications for and rates of primary cesarean deliveries, institutions should identify those occurring without an accepted medical indication. Within those with specific indications attention should be paid to cesareans occurring after labor inductions, those labeled as for “non-reassuring fetal status”, and those occurring for labor arrest or “failed induction” without meeting accepted criteria (Boxes 1 and 2). A classification system is needed in order to track cesarean sections, compare rates between practices and over time, perform audits, provide feedback, and identify areas for potential intervention. (6) While not uniquely designed for primary cesarean sections, the Robson classification is an example of a simple method that allow comparison of cesarean section rates between practices as well as over time. (7–9)
Box 1. Definitions of Failed Induction and Arrest Disorders.
| Failed induction of labor: | Failure to generate regular (e.g. every 3 minutes) contractions and cervical change after at least 24 hours of oxytocin administration, with artificial membrane rupture if feasible |
| First-stage arrest | |
| Spontaneous labor: | ≥ 6cm dilation with membrane rupture and |
| ≥ 4 hours of adequate contractions (eg >200 Montevideo units) or |
|
| ≥ 6 hours if contractions inadequate with no cervical change |
|
| Induced labor: | ≥ 6cm dilation with membrane rupture or ≥ 5cm without membrane rupture and |
| ≥ 4 hours of adequate contractions (eg >200 Montevideo units), or |
|
| ≥ 6 hours if contractions inadequate with no cervical change | |
| Second-stage arrest: | No progress (descent or rotation) for |
| 4 hours or more in nulliparous women with an epidural | |
| 3 hours or more in nulliparous women without an epidural | |
| 3 hours or more in multiparous women with an epidural | |
| 2 hours or more in multiparous women without an epidural |
Box 2: Quality Measures to Track and Provide Feedback for Each Obstetrician-–Gynecologist Physician*.
Rate of nonmedically indicated cesarean
Rate of nonmedically indicated induction
Rate of labor arrest or failed induction diagnosed without meeting accepted criteria
Rate of cesareans for nonreassuring fetal heart rate by NICHD category
*For singleton gestation, vertex presentation, at 37 0/7 to 41 6/7 weeks.
NICHD, National Institute of Child Health and Human Development.
Labor management practices and primary cesarean
Antepartum and intrapartum management decisions can have a profound effect on the individual patient’s likelihood of cesarean delivery. The decision to induce labor for medical or non-medical indications, labor management style, the diagnosis and management of arrest disorders in the first and second stages of labor, the use of labor neuroaxial anesthesia, the use of operative vaginal delivery, and evaluation of fetal factors, as well as non-medical indications, may effect the potential for successful vaginal delivery.
Induction of Labor
The overall likelihood of vaginal delivery is lower after labor induction than after spontaneous labor, especially when labor induction is attempted in a nulliparous woman with an unfavorable cervix. Institutions should have a clear policy regarding labor induction, including a list of acceptable indications, and should specify the definitions of a favorable cervix, options for cervical ripening in the presence of an unripe cervix, oxytocin infusion protocols, and criteria for the diagnosis of failed induction. Labor induction with an unfavorable cervix should not be undertaken unless delivery is indicated for clear maternal or fetal benefit. Any time induction is undertaken, it should be clear that the goal is vaginal delivery.
Because an unfavorable cervix can negatively effect the labor course and increase the potential for cesarean delivery, this factor should be considered in decision making regarding the method of labor induction. However, the decision for induction should be considered first, and should be separate from the decision about whether or not to employ cervical ripening. Pragmatically, while the potential maternal and fetal risks related to induction with an unfavorable cervix should be incorporated into the overall risk-benefit evaluation when considering medically-indicated labor induction, the decision to proceed with induction should be made independent of the condition of the cervix and based on the specific indication(s). There is no single definition used to differentiate a favorable (“ripe”) from an unfavorable (“unripe”) cervix, whether in research or in clinical practice. In general, the Bishop’s score has most often been used to describe cervical ripeness. A Bishop’s score greater than 8 generally confers the same likelihood of vaginal delivery with induction of labor as that following spontaneous labor, and thus has been considered to indicate a favorable cervix (10). Conversely, a Bishop’s score of 6 or less has been used to denote an unfavorable cervix in many studies and has been associated with a higher risk of cesarean delivery when labor is induced compared with spontaneous labor. Since the Bishop’s score was originally developed to predict the likelihood of multiparous women at term to enter spontaneous labor, making it less predictive of outcome after labor induction in nulliparas, the affects of maternal parity and gestational age were also considered during the Workshop. Cervical ripening may be considered when there is a medical indication for induction. Since inductions without medical indication should not be done with an unripe cervix, cervical ripening would not be an option. (Box 1, Figure 1). Although cervical ripening agents have generally not been demonstrated to reduce the likelihood of cesarean delivery in prospective interventional trials, their use can effect the duration of labor.
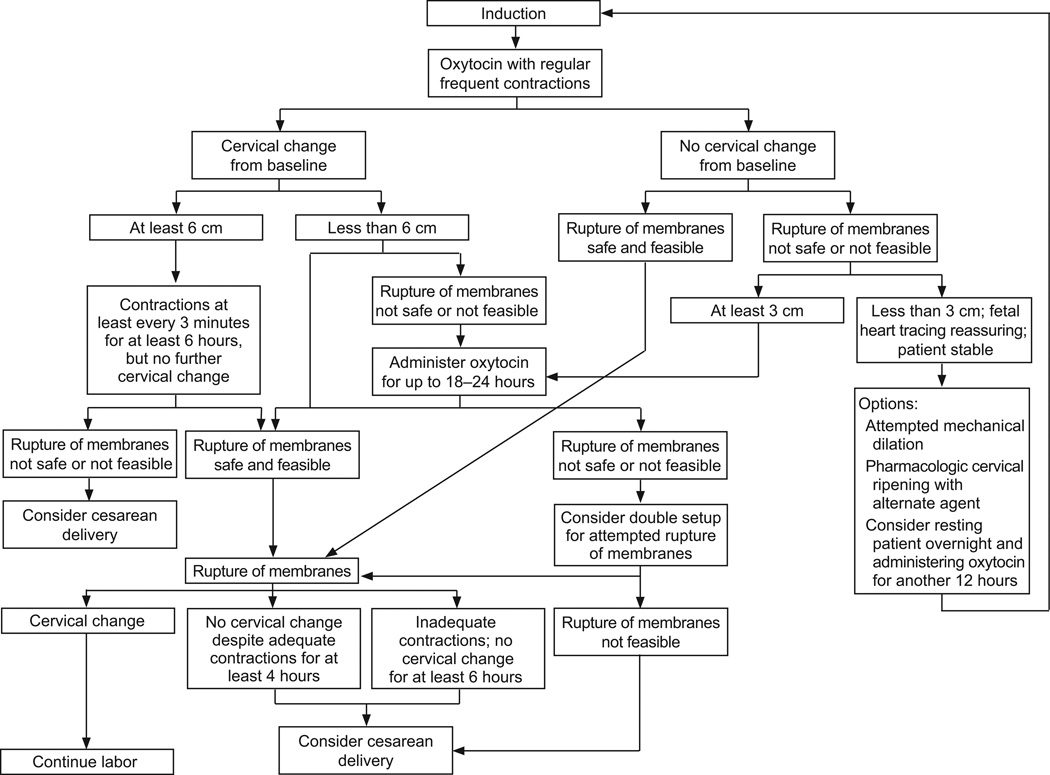
Figure 1.
Algorithm for induced labor.
Because the goal of labor induction is vaginal delivery, adequate time to enter into or progress in labor should be allowed provided the mother and baby are stable. The prudent use of labor induction, and the expectation that well-defined criteria be met before cesarean is performed for failure of induction or failure of progress in labor, may actually prevent many unnecessary first cesareans. During this evaluation, it is important to differentiate between “failed induction” and “arrest of labor” in the first stage. The diagnosis of failed induction should be reserved for those women who have failure to generate regular (e.g. every 3 minutes) contractions and cervical change after at least 24 hours of oxytocin administration, with artificial membrane rupture if feasible (after completion of cervical ripening, if performed; Box 1, Figure 1). Studies have shown that over half of the women undergoing labor induction remain in the latent phase for at least 6 hours, and nearly one-fifth remain in the latent phase for 12 hours or longer (11). In a multi-center study, nearly 40% of the women still in the latent phase after 12 hours of oxytocin and membrane rupture successfully delivered vaginally. These data suggest that induction should not be defined to have failed in the latent phase unless oxytocin has been administered for at least 24 hours, or for 12 hours after membrane rupture. (12,13) Numerous approaches to induction and cervical ripening have been published, and no single approach is considered superior to all others. Individual circumstances should be considered for each patient. The algorithm offered in Figure 1 provides a general approach once the decision has been made to proceed with labor induction.
There is much debate as to how long induction should be allowed to continue, and whether it is appropriate to “rest” the patient who does not progress after 12 or more hours of induction but who does not otherwise have a maternal or fetal reason for immediate delivery. In cases where induction is undertaken for specific maternal or fetal conditions that can worsen with time, then stopping the induction is not an appropriate option. Examples of such cases include preeclampsia, fetal growth restriction, diabetes, and ruptured membranes. On the other hand, induction is sometimes undertaken when neither the maternal nor fetal condition is expected to deteriorate rapidly. Examples include induction for social reasons or induction at 41 weeks. Despite this being a common obstetrical dilemma, guidance available from professional organizations do not provide clarity (14–16). Published trials allowed cervical ripening over a period ranging from a single dose to several doses over two days. In a trial of the Maternal-Fetal Medicine Units network, the study design specified at least 24 hours from start of oxytocin before declaring a failed induction. All trials have found good outcomes in the induction group despite waiting for at least 24 hours before failed induction was declared (Box 1, Figure 1). It is also important to note that in all induction trials, rupture of membranes was undertaken as soon as feasible and safe. Based on this indirect evidence, it is considered appropriate to temporize before declaring that an induction has failed in women being induced for conditions that are not likely to worsen with time and whose membranes remain intact. An arrest disorder should not be confused with failed induction. The diagnosis of an arrest disorder in women undergoing induction should not be made unless the woman has entered the active phase of labor, requiring that there be documented cervical change preceding the arrest in dilation (Box 1).Once 6 cm cervical dilation is reached and the active phase is entered, labor progress during induction is similar to the patient in spontaneous labor. However, the duration of the phase before 6 cm dilation is longer in women undergoing induction (17).
Labor Management Style
It has been suggested that the widely varying rates of cesarean delivery between providers may be the result of different labor management styles. Admission of women in the early latent phase of labor (e.g. <3cm dilated) has been associated with higher cesarean delivery rates. However, it is unclear whether the admission in early labor itself increases the risk for cesarean or if women requiring admission earlier in labor are actually more likely to have an abnormal labor course (e.g. abnormal contraction pattern resulting in excessive pain, and slower progress in early labor foreshadowing a subsequent arrest disorder). Hospital admission does provide more time to monitor labor progress and fetal well-being, as well as to implement interventions to facilitate labor. But early admission could also give the impression of a long labor and result in earlier abandonment if progress is not deemed adequate, or because of pressure from the patient or family. While it is prudent to avoid unneeded admissions (e.g. before 3cm of dilatation) and interventions (e.g. augmentation, artificial membrane rupture), there is limited information regarding the direct effect of these practices on primary cesarean delivery rates.
Provider type (e.g. MD, CNM) may also be related to labor outcomes. Whether this relationship is causal or merely by association is not clear. (18–20) It is possible that differences in the characteristics and expectations of women seeking different provider types may also affect the outcome – for example, the woman interested in delivering with a midwife or other low-risk provider may have an inherently different risk of cesarean than one who prefers the care of an obstetrician or maternal-fetal medicine subspecialist. Despite this, the same defined criteria for labor arrest and prolonged labor should be used regardless of provider or patient type.
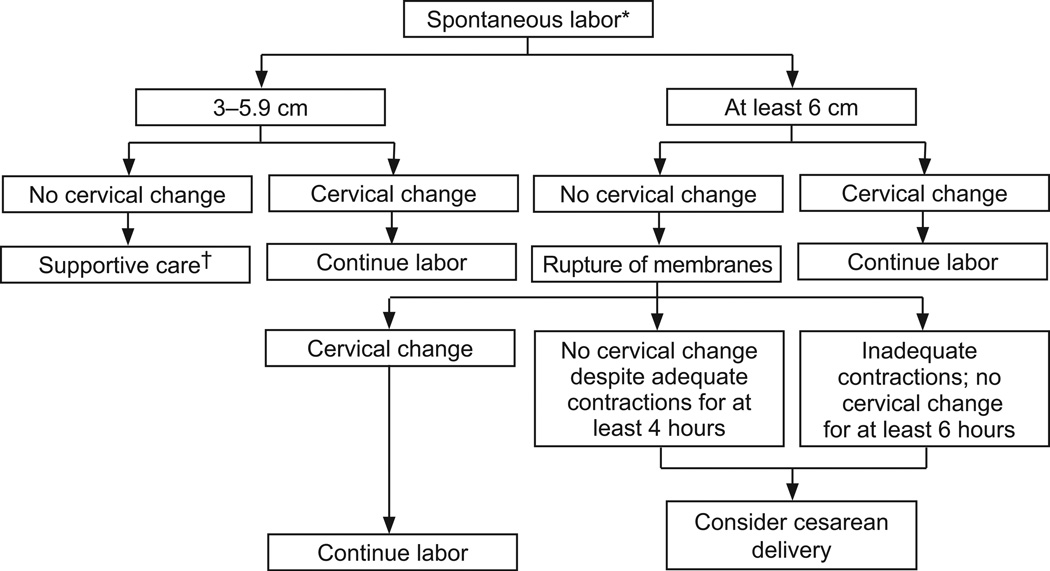
Diagnosis of Arrest Disorders
The concept of a prolonged or “protracted” first or second stage of labor should be considered distinct from that of an arrest disorder. Progress in the first stage should not be based solely on cervical dilation, but must also take into consideration change in cervical effacement and fetal station. Similarly, progress in the second stage involves not only descent, but also rotation of the fetal head as it traverses the maternal pelvis. Recognition of arrest of labor in the first or second stage of labor (Box 1) provides an opportunity to reassess maternal and fetal condition, to counsel the woman about the ongoing potential for successful vaginal delivery, and to address the maternal and perinatal risks of continued labor. However “protracted labor” alone should not be the sole indication for an operative vaginal or cesarean delivery if progress is being made and the maternal and fetal status are reassuring.
While the timing of labor onset in the patient entering spontaneous labor at home may be less clear, and the progress of labor prior to arrival to the hospital cannot be accurately assessed, there is no reason to differentiate between the diagnostic criteria for arrest disorders that occur after spontaneous labor versus labor induction. Pragmatically, arrest disorders in spontaneously laboring women are defined by clinical findings noted after admission. In both spontaneous as well as induced labor, the diagnosis of an arrest disorder should not be made before the patient has entered into the active phase. The definitions of arrest disorders listed in Box 1 vary somewhat from published criteria (10) in recognition of more recent findings regarding labor progress that challenge our long held practices based on the Friedman curve. For example, the acceleration phase in active labor may not begin until approximately 6 cm dilation rather than the previously recognized 4 cm cut-off, and multiparous women appear to have a steeper acceleration phase than previously thought.(21)
Data needed to establish the normal range for the duration of the latent phase are not readily available because the onset of the latent phase in most women in spontaneous labor occurs outside the hospital, and therefore cannot be accurately determined. Available evidence suggests that the duration of the latent phase is not different between nulliparous and multiparous women, a finding that contrasts with the overall length first and second stages of labor (21). Based on data from the safe labor consortium, nulliparous women in spontaneous labor entering the hospital have a median duration of 6 hours (95th percentile of 15.7 hours) to reach the active phase of labor (6cm dilation) if they enter the hospital at 2 cm dilation, and 4.2 hours (95th percentile 12.5 hours) if they enter at 3 cm (21). Nulliparous women admitted in spontaneous labor with a cervix between 2 to 4 cm may not change their cervix for up to 7 to 6 hours, respectively. (21)
The safe labor consortium analyzed the duration of labor in 62,415 women with a term singleton pregnancy and a normal outcome, and developed contemporary partograms for labor (21). Labor in nulliparous women took longer than expected based on the Friedman curves. The investigators found that labor can take over 6 hours to progress from 4 to 5 cm and over 3 hours to progress from 5 to 6 cm. The median duration of the active phase, from 6 cm to complete cervical dilation, was 2.1 hours in nulliparous woman and 1.5 hours in multiparous woman, with the 95th percentiles of 8.6 hours and 7.5 hours, respectively. The median and 95th percentiles for the cervical change before 6 cm are similar for nulliparous and multiparous women. After 6 cm, multiparous women had a slightly faster labor than nulliparous women. These data suggest that the historical criteria defining normal labor progress- cervical change of 1.2 cm/hour for nulliparous women and 1.5 cm/hour for multiparous women are no longer valid.
As for the second stage of labor, the data from the safe labor consortium showed the median duration (95th percentile) with epidural analgesia to be 1.1 (3.6), 0.4 (2.0) and 0.3 (1.6) hours for nulliparous, primiparous and multiparous women respectively, and 0.6 (2.8), 0.2 (1.3) and 0.1 (1.1) hours without epidural (21). Table 5 shows the median and 95th percentile duration for each centimeter change in nullliparous women in spontaneous labor.
Table 5.
Duration of Each Centimeter Change in Cervical Dilatation for Nulliparous Women With Spontaneous Onset of Labor*
| Cervical Change (cm) |
Median (Hour) | 95th Percentile (Hour) |
|---|---|---|
| 3–4 4–5 5–6 6–7 7–8 8–9 9–10 |
1.8 1.3 0.8 0.6 0.5 0.5 0.5 |
8.1 6.4 3.2 2.2 1.6 1.4 1.8 |
Modified from Zhang J, Landy HJ, Branch DW, Burkman R, Haberman S, Gregory KD, Hatjis CG, Ramirez MM, Bailit JL, Gonzalez-Quintero VH, Hibbard JU, Hoffman MK, Kominiarek M, Learman LA, Van Veldhuisen P, Troendle J, Reddy UM; Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol 2010;116:1281–7.
Labor Analgesia
Although it has been suggested that the use of neuraxial analgesia (epidural, spinal, or combined spinal-epidural) may prolong the latent phase of spontaneous labor, numerous trials have failed to find an increase in cesarean delivery with neuraxial analgesia, either during labor induction or after spontaneous labor. (22–24) As such, neuraxial analgesia should not be withheld or delayed because of concerns regarding the risk of cesarean delivery.
Operative Vaginal Delivery
Forceps and vacuum assisted operative vaginal delivery may avert a cesarean when maternal expulsive forces are inadequate or expedited delivery is needed (25). Many studies, including some that followed the offspring up to 18 years of age, have demonstrated that neonates delivered by operative vaginal delivery typically have a normal newborn transition period and normal long term outcomes.(26–29) Comparing the reported rates of cesarean versus operative vaginal delivery between US, Canadian, and European practices, it becomes clear that higher rates of operative vaginal delivery are often associated with lower cesarean delivery rates, and vice versa. Though plausible, a cause and effect relationship has not been established.
While operative vaginal delivery is acceptable in appropriate circumstances, it requires an operator who understands the indications and prerequisites, and is skilled in the technique. For this reason, the diminishing training and experience in operative vaginal delivery nationally is of concern. Important steps in providing initial training and in maintaining skills include not only increased supervised training during residency and supplemental training and skill maintenance simulations, but recognition by both patients and physicians that operative vaginal delivery is safe and can reduce perinatal morbidities when performed by an experienced practitioner. Training programs should have readily available skilled operators to teach these procedures, and mechanisms in place to provide training, including in actual cases as well as by simulation.
Evaluation of Fetal Status Before and During Labor
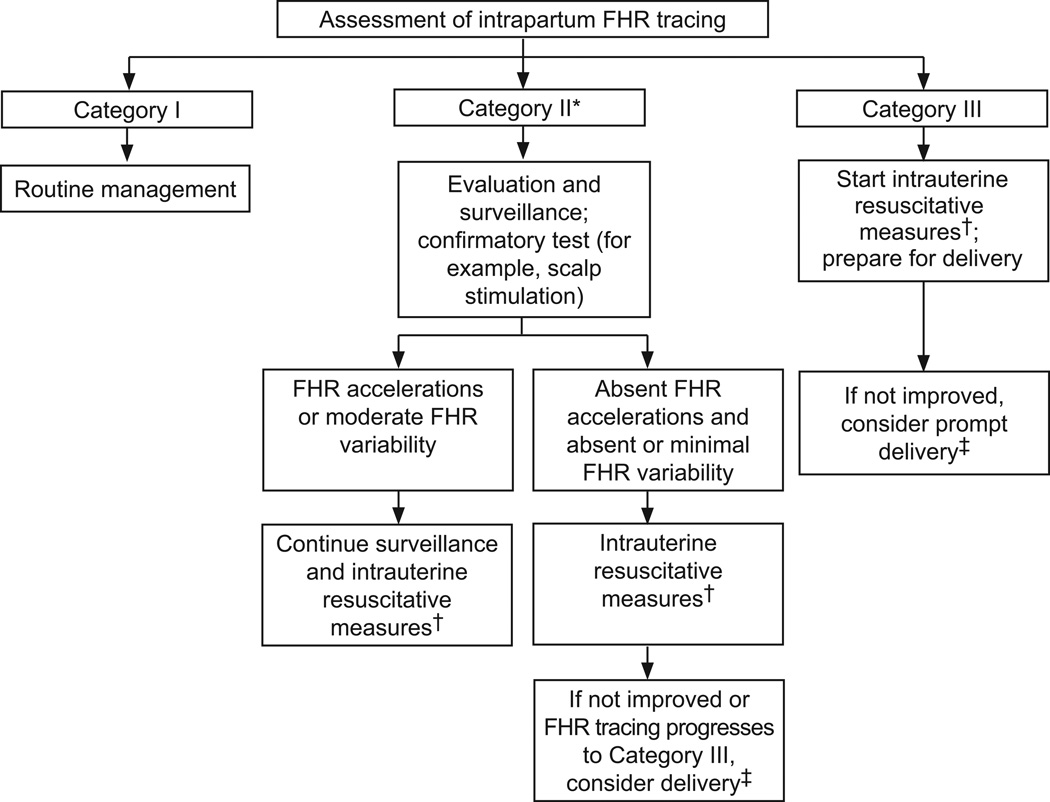
Electronic fetal heart monitoring remains the mainstay for assessment of fetal status during labor, and is often used to decide on the mode of delivery in a complicated pregnancy (Figure 3). Continuous intrapartum fetal heart rate monitoring has been used in over 85% of deliveries in the United States for more than a decade. (30) However, despite the expectation that continuous intrapartum fetal heart rate monitoring would improve perinatal outcomes and the concomitant rise in cesarean deliveries, there has been no reduction in the rate of cerebral palsy since its introduction in the United States and elsewhere. While studies have found no benefit of continuous monitoring over intermittent auscultation in low-risk women, intermittent auscultation requires one-to-one nursing throughout labor, and may not be appropriate in high risk women or when there are fetal heart rate abnormalities detected by auscultation. Although it is reasonable to provide intermittent auscultation for low risk women, guidelines defining appropriate candidates, the required frequency of auscultation, and criteria for conversion to continuous fetal heart rate monitoring should be in place and enforced.
Figure 3.
Assessment of intrapartum fetal heart rate monitoring. *Given the wide variation of fetal heart rate (FHR) tracings in Category II, this algorithm is not meant to represent assessment and management of all potential FHR tracings, but provide an action template for common clinical situations. † Intrauterine resuscitative measures may include oxygen supplementation, position change, intravenous fluids, stopping oxytocin, tocolysis, amnioinfusion, etc.
‡Timing and mode of delivery based on feasibility and maternal-fetal status. Modified from ACOG Practice Bulletin No. 116. Assessment of intrapartum fetal heart rate tracings. Obstet Gynecol 2010;116:1232–40.
Important limitations in the interpretation of continuous fetal heart rate monitoring include considerable interobserver variability in the identification of fetal heart rate patterns likely to be associated with fetal acidosis, and the fact that many patterns have a low positive predictive value for adverse outcomes. In 2008, the Eunice Kennedy Shriver National Institute for Child Health and Human Development revised the guidelines for interpretation of fetal heart rate patterns, creating a three-tiered interpretation system. Category I fetal heart rate tracings are strongly predictive of normal fetal acid-base status and are considered “normal”. Category III fetal heart rate patterns are predictive of abnormal fetal acid-base status at the time of observation and are considered “abnormal.” The intermediate Category II fetal heart rate patterns include those that cannot be classified as Category I or III.(31) The NICHD recommendations do not specify any particular intervention for Category I tracings, but do support prompt evaluation of Category III heart rate patterns. While interventions to resolve an abnormal Category III fetal heart rate pattern may help to avoid unneeded cesarean delivery, expeditious delivery is recommended if these efforts are unsuccessful. (Figure 3) The intermediate Category II fetal heart rate pattern requires a heightened level of attention, but does not by itself require immediate delivery; rather, evaluation and continued surveillance and reevaluation are recommended. Maneuvers to improve uteroplacental perfusion (e.g. adjustment of oxytocin infusion rate, administration of maternal oxygen, change of maternal position, treatment of maternal hypotension) may result in reversion to a Category I pattern.
Fetal heart rate acceleration in response to fetal scalp stimulation is supportive evidence suggesting the absence of fetal acidosis. Although fetal scalp sampling was previously used to determine scalp microcapillary pH, the hardware needed for bedside fetal scalp pH assessment is no longer available in the United States. The efficacy of other ancillary technologies (e.g. fetal pulse oximetry, fetal EKG ST-segment analysis, computerized fetal heart rate pattern interpretation) to improve the clinician’s ability to identify the fetus at risk for a poor outcome has not been confirmed as beneficial for infant outcomes. Until additional effective technologies become available, it is unlikely that the rate of cesarean delivery for fetal heart rate abnormalities will be reduced substantially.
It is important to remember that any test that depends on human interpretation will be subject to the pressures exerted on the individual making the decision and the individual’s responses to the environment. This will lead to either higher false negative or higher false positive test results depending on whether the decision-maker fears more the implications of a mistaken diagnosis or the implications of missing a diagnosis, respectively. In the case of electronic fetal monitoring, the major implication of a false positive interpretation is a potentially unnecessary operative delivery, while the implication of a false negative interpretation is an adverse outcome for the fetus, along with its associated consequences to the decision-maker and hospital. Even if one believes that continuous fetal heart rate monitoring may have prevented some adverse outcomes, the evidence is overwhelming that it has caused many more unnecessary interventions overall. The result is a rise in cesarean rates, which has led to an increased incidence of subsequent placenta accreta and associated maternal morbidities and mortality. When discussing continuous fetal heart rate monitoring, the fetus who was “saved” is frequently held as proof of benefit of this technology, but the many more women who underwent unnecessary procedures, had significant morbidity, or even died as a result of a false positive interpretation are rarely mentioned. Importantly, the fact that the risks of cesarean are cumulative over future pregnancies is frequently overlooked.
Given that interpretation of the fetal heart rate can be subjective, it is important that hospitals institute some form of quality control for operative deliveries with non-reassuring fetal heart rate as the indication. (Box 2) Including the fetal heart rate category in the indication should be essential. In the case of an indication with a Category II pattern, confirmatory testing should be documented. This may be a negative response to scalp stimulation or minimal variability. Regular audits and reports can be provided to the staff, with the rates of operative deliveries according to indications and stage of labor.
Non-Medical Factors
The relative safety of cesarean delivery has lowered both patient and physician apprehension regarding the risk of such surgery, especially in the face of borderline fetal heart rate abnormalities, protracted labor or arrest disorders, or after the development of obstetrical or medical complications. In general, the usual concerns regarding major surgery do not seem to apply as emphatically to cesarean delivery as to other operations. This is most evident among patients requesting a non-medically indicated cesarean and physicians who acquiesce to such requests. Patient perception and education, societal attitudes, and social media all play a role (32). In addition to considering the risk of the first cesarean, physicians and patients should be made aware of the potential complications resulting from repeated surgeries, both for the mother (e.g. adhesions, bowel/bladder trauma, abnormal placentation including placenta accreta, uterine rupture, hysterectomy) and the fetus (e.g. delayed delivery due extensive adhesions).
Institutional factors, such as time constraints for scheduling on the Labor and Delivery unit, varying operating room staff availability, and the inability to support prolonged inductions with resources and space that may be scarce, all play a role in the decision to proceed to cesarean. Physician factors such as fatigue, work load, and anticipated sleep deprivation likely also affect decision-making. Several studies have suggested that cesarean rates are influenced by the “leisure incentive”; when the provider can go to sleep or go home after the delivery, the cesarean rate, especially cesareans performed for “dystocia” (prolonged or dysfunctional labor) and “fetal intolerance of labor”, increases (33,34) . Financial incentives and disincentives related to work efficiency and staffing workload may also tilt the scale toward more liberal performance of scheduled cesarean deliveries. Given the time required to monitor a complicated labor, there is a financial disincentive to persevere when labor does not proceed efficiently or if borderline fetal heart patterns are present. Evidence suggests that doctors who are salaried and participate in profit sharing, thus reducing the financial incentive to limit the time spent managing labor, have lower cesarean rates (31).
The current medical legal climate has also made waiting for a vaginal delivery less attractive to many physicians when labor is not proceeding smoothly. In many centers, the number of cesareans performed for “non-reassuring fetal status” has increased more than any other indication, despite the fact that the number of women classified as high risk has not increased concomitantly (35,36). All of these factors are compounded by the belief among many patients that cesarean is safer for the fetus (37).
Patient expectations, the medical legal climate, and practice patterns regarding intrapartum management need to be addressed if the rate of primary cesarean delivery is to be reduced. Importantly, the misperception among reproductive age women that labor and vaginal delivery can harm the baby while cesarean insures a normal outcome must be recognized and corrected. Given the implications of primary cesarean on both pregnancy complications and subsequent deliveries, it is crucial to institute practice management that limits performance of the first cesarean (Box 1).
Conclusions
Although numerous factors contribute to the primary cesarean rate, the clinician’s ability to modify some of these and mitigate others is the first step toward lowering the primary cesarean rate (Tables 2–4; Boxes 1 and 3). The available information on maternal and fetal factors, labor management and induction, and non-medical factors leading to the first cesarean, as well as the implications of the first cesarean on future reproductive health were reviewed and critical key points were identified (Box 3). The implications of a cesarean rate of 30% or more have tremendous effects on the medical system as well as on the health of women and children. It is essential to embrace this concern and provide guidance on strategies to lower the primary cesarean rate. Education regarding the normal labor course and the implications of first cesarean may allow women and their providers to avoid practices that increase the potential for unneeded first cesarean deliveries.
Box 3: Key Points.
A cesarean that is performed without an accepted indication should be labeled as such, ie ”non-indicated cesarean.“ The term ”elective cesarean” should be avoided.
Labor induction should be performed only for medical indication; if done for nonmedical indications, the gestational age should be 39 weeks or more, and the cervix should be favorable (Bishop score 8 or higher), especially in the nulliparous patient.
Adequate time for normal latent and active phases of the first stage, and for the second stage, should be allowed unless expeditious delivery is medically indicated. (Box 1 and Figures 1 and 2)
The diagnosis of failed induction should only be made after an adequate attempt. Failed induction is defined as failure to generate regular (eg, every 3 minutes) contractions and cervical change after at least 24 hours of oxytocin administration, with artificial membrane rupture if feasible.
In the presence of reassuring maternal and fetal status, the diagnosis of arrest of labor should not be made until after adequate time is elapsed. This includes > 6cm dilation with membrane rupture and 4 or more hours of adequate contractions (eg, greater than 200 Montevideo units) or 6 hours or more if contractions inadequate with no cervical change for first-stage arrest. For second-stage arrest, no progress (descent or rotation) for more than 4 hours in nulliparous women with an epidural, more than 3 hours in nulliparous women without an epidural, more than 3 hours in multiparous women with an epidural, and more than 2 hours in multiparous women without an epidural should be considered, with no cesarean for this indication before these time limits. (Box 1).
Intermittent auscultation, if this can be done appropriately, is an acceptable method for labor management if the heart rate remains within normal limits. (Category I of the fetal heart rate categories)
Medically indicated operative vaginal delivery is an acceptable birth method. Given the current rates, it is critical that training and experience in operative vaginal delivery is augmented and encouraged.
Doctors who are salaried and participate in profit sharing, thus reducing the financial incentive to limit the time spent managing labor, have lower cesarean rates.
In the patient with moderate fetal heart rate variability, other findings have little association with neurologic damage or acidosis.
When discussing the first cesarean with a patient, counseling should include its effect on future reproductive health including subsequent pregnancy risks, such as uterine rupture and placental implantation abnormalities including placenta previa and accreta.
Figure 2.
Algorithm for spontaneous labor. *Try not to admit unless at least 3 cm dilated.
†Expectant management; no need for intervention.
Table 3.
Selected Potentially Modifiable Fetal Indications for First Cesarean Delivery
| Diagnostic Accuracy* |
Effect on Prevention of First Cesarean Delivery† |
Preventive Strategies | |
|---|---|---|---|
| Malpresentation | High | Large | External cephalic version |
| Nonreassuring antepartum or intrapartum fetal surveillance | Moderate | Large | Education regarding correct interpretation and management (Figure 3) Confirmatory tests (e.g. scalp stimulation) Intrauterine resuscitative measures (eg, IVF, position change, oxygen, etc) |
| Macrosomia | Limited |
Small |
Screen for and treat diabetes; limit weight gain in pregnancy |
| Malformations eg, NTD, SCT, EXIT procedure, hydrops |
Moderate |
Small |
Anecdotal for indication Education: cesarean delivery not indicated for abdominal wall defects Multidisciplinary education of subspecialists and counseling of patients |
IVF, in vitro fertilization; NTD, neural tube defects; SCT, sacrococcygeal teratoma; EXIT, ex utero intrapartum treatment.
Diagnostic criteria accuracy: how readily and accurately cases can be diagnosed. The ability to diagnose malpresentation is high, whereas the ability to identify macrosomia is limited. Moderate accuracy is between high and limited.
Effect on prevention of first cesarean delivery: Large means that modification of indication (eg, malpresentation) could lead to a large decrease in cesarean deliveries. Small means that modification of indication (eg, malformations) could lead to a small decrease in cesarean deliveries.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This article is an executive summary of a Society for Maternal-Fetal Medicine, Eunice Kennedy Shriver National Institute of Child Health and Human Development, and American College of Obstetricians and Gynecologists workshop that was held February 7–8, 2012, in Dallas, Texas.
Financial Disclosure: The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary Data for 2009. Hyattsville, MD: National Center for Health Statistics; 2010. Report No.: vol 59 no 3. [PubMed] [Google Scholar]
- 2.Healthy People 2020. [accessed April 30, 2012];Maternal, Infant, and Child Health. http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=26.
- 3.Healthy People 2010. Healthy People 2010 Operational Definition. http://www.google.com/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CCYQFjAA&url=ftp%3A%2F%2Fftp.cdc.gov%2Fpub%2Fhealth_statistics%2Fnchs%2Fdatasets%2Fdata2010%2Ffocusarea16%2FO1609a.pdf&ei=q-qeT8a_OaaV6AGT0MCBDw&usg=AFQjCNH-Hrxn-U0t3o3QSYuvwpGFSD277Q&sig2=sO1mzDOcj8QhZMhiggP6Uw.
- 4.Clark EA, Silver RM. Long-term maternal morbidity associated with repeat cesarean delivery. Am J Obstet Gynecol. 2011;205:S2–S10. doi: 10.1016/j.ajog.2011.09.028. Epub 2011 Oct 6. [DOI] [PubMed] [Google Scholar]
- 5.Berghella V, Blackwell SC, Ramin SM, Sibai BM, Saade GR. Use and misuse of the term "elective" in obstetrics. Obstet Gynecol. 2011 Feb;117((2 Pt 1)):372–376. doi: 10.1097/AOG.0b013e31820780ff. [DOI] [PubMed] [Google Scholar]
- 6.Torloni MR, Betran AP, Souza JP, Widmer M, Allen T, Gulmezoglu M, Merialdi M. Classifications for Cesarean Section: A Systematic Review. PLoS ONE. 6(1):e14566. doi: 10.1371/journal.pone.0014566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robson MS. Can we reduced the Caesarean Section Rate? Best Practice & Research Clinical Obstetrics & Gynecology. 2001;Vol 15(No 1):179–194. doi: 10.1053/beog.2000.0156. [DOI] [PubMed] [Google Scholar]
- 8.Brennan DJ, Murphy M, Robson MS, O’Herlihy C. The Singleton, Cephalic, Nulliparous Woman After 36 Weeks of Gestation. Obstet Gynecol. 2011;117:273–279. doi: 10.1097/AOG.0b013e318204521a. [DOI] [PubMed] [Google Scholar]
- 9.Brennan DJ, Robson MS, Murphy M, O’Herlihy Comparative analysis of international cesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. Am J Obstet Gynecol. 2009;201:308.e1–308.e8. doi: 10.1016/j.ajog.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 10.American College of Obstetricians and Gynecologists Practice Bulletin: Induction of Labor Number 107, August 2009 PB107, 2009 [Google Scholar]
- 11.Simon CE, Grobman WA. When has an induction failed? Obstet Gynecol. 2005;105:705–709. doi: 10.1097/01.AOG.0000157437.10998.e7. [DOI] [PubMed] [Google Scholar]
- 12.Harper LM, Caughey AB, Odibo AO, Roehl KA, Zhao Q. Normal Progress of Induced Labor. Obstet Gynecol. 2012;119:1113–1118. doi: 10.1097/AOG.0b013e318253d7aa. [DOI] [PubMed] [Google Scholar]
- 13.Rouse DJ, Weiner SJ, Bloom SL, Varner MW, Spong CY, Ramin SM, Caritis SN, Grobman WA, Sorokin Y, Sciscione A, Carpenter MW, Mercer BM, Thorp JM, Jr, Malone FD, Harper M, Iams JD, Anderson GD. Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units Network (MFMU).Failed labor induction: toward an objective diagnosis. Obstet Gynecol. 2011;117:267–272. doi: 10.1097/AOG.0b013e318207887a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heimstad R, Skogvoll E, Mattsson LA, Johansen OJ, Eik-New SH, Salvesen KA. Induction of Labor or Serial Antenatal fetal Monitoring in Postterm Pregnancy. Obstet Gynecol. 2007;109:609–617. doi: 10.1097/01.AOG.0000255665.77009.94. [DOI] [PubMed] [Google Scholar]
- 15.NICHD MFMU Network. A clinical trial of induction of labor versus expectant management in postterm pregnancy. Am J Obstet Gynecol. 1994;170:716–723. [PubMed] [Google Scholar]
- 16.Hannah ME, Hannah WJ, Hellmann J, Hewson S, Milner R. Willan A and the Canadian Multicenter Postterm Pregnancy Trial Group Induction of labor as compared with serial antenatal monitoring in post-term pregnancy. N Engl J Med. 1992;326:1587–1592. doi: 10.1056/NEJM199206113262402. [DOI] [PubMed] [Google Scholar]
- 17.Rouse DJ, Weiner SJ, Bloom SL, et al. Second-stage labor duration in nulliparous women: relationship to maternal and perinatal outcome. Am J Obstet Gynecol. 2009;201:357e1–357e7. doi: 10.1016/j.ajog.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatem M, Sandall J, Devane D, Soltani H, Gates S. Midwife-led versus other models of care for childbearing women. Cochrane Database Syst Rev. 2008;4:CD004667. doi: 10.1002/14651858.CD004667.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Rooks JP, Weatherby NL, Ernst EK, Stapleton S, Rosen D, Rosenfield A. Outcomes of care in birth centers. The National Birth Center Study. N Engl J Med. 1989;321:1804–1811. doi: 10.1056/NEJM198912283212606. [DOI] [PubMed] [Google Scholar]
- 20.Davis LG, Riedmann GL, Sapiro M, Minogue JP, Kazer RR. Cesarean section rates in low-risk private patients managed by certified nurse-midwives and obstetricians. J Nurse Midwifery. 1994;39:91–97. doi: 10.1016/0091-2182(94)90016-7. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J, Landy HJ, Branch W, et al. Contemporary Patterns of Spontaneous Labor with Normal Neonatal Outcomes. Obstet Gynecol. 2010;116:1281–1287. doi: 10.1097/AOG.0b013e3181fdef6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anim-Somuah M, Smyth RM, Jones L. Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev 12:CD000331. 2011 doi: 10.1002/14651858.CD000331.pub3. [DOI] [PubMed] [Google Scholar]
- 23.Sharma SK, McIntire DD, Wiley J, et al. Labor analgesia and cesarean delivery: an individual patient meta-analysis of nulliparous women. Anesthesiology. 2004;100:142–148. doi: 10.1097/00000542-200401000-00023. [DOI] [PubMed] [Google Scholar]
- 24.Wassen MM, Zuijlen J, Roumen FJ, et al. Early versus late epidural analgesia and risk of instrumental delivery in nulliparous women: a systematic review. BJOG. 2011;118:655–661. doi: 10.1111/j.1471-0528.2011.02906.x. [DOI] [PubMed] [Google Scholar]
- 25.Gei AF. Belfort MA Forceps-assisted vaginal delivery. Obstet Gynecol Clin North Am. 1999 Jun;26(2):345–370. doi: 10.1016/s0889-8545(05)70079-6. [DOI] [PubMed] [Google Scholar]
- 26.Demissie K, Rhoads GG, Smulian JC, et al. Operative vaginal delivery and neonatal and infant adverse outcomes: population based retrospective analysis. BMJ. 2004;329:1–6. doi: 10.1136/bmj.329.7456.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gardella C, Taylor M, Benedetti T, et al. The effect of sequential use of vacuum and forceps for assisted vaginal delivery on neonatal and maternal outcomes. Am J Obstet Gynecol. 2001;85:896–902. doi: 10.1067/mob.2001.117309. [DOI] [PubMed] [Google Scholar]
- 28.Wesley BD, van den Berg BJ, Reece EA. The effect of forceps delivery on cognitive development. Am J Obstet Gynecol. 1993 Nov;169(5):1091–1095. doi: 10.1016/0002-9378(93)90261-g. [DOI] [PubMed] [Google Scholar]
- 29.Seidman DS, Laor A, Gale R, Stevenson DK, Mashiach S, Danon YL. Long-term effects of vacuum and forceps deliveries. Lancet. 1991 Jun 29;337(8757):1583–1585. doi: 10.1016/0140-6736(91)93273-c. [DOI] [PubMed] [Google Scholar]
- 30.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep. 2003;52:1–113. [PubMed] [Google Scholar]
- 31.Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol. 2008 Sep;112(3):661–666. doi: 10.1097/AOG.0b013e3181841395. [DOI] [PubMed] [Google Scholar]
- 32.Murphy M, Hull PM. Choosing Cesarean: A Natural Birth Plan. Promethus Books 2012 [Google Scholar]
- 33.Klasko SK, Cummings RV, Balducci J, DeFulvio JD, Reed JF., 3rd The impact of mandated in-hospital coverage on primary cesarean delivery rates in a large nonuniversity teaching hospital. Am J Obstet Gynecol. 1995 Feb;172((2 Pt 1)):637–642. doi: 10.1016/0002-9378(95)90585-5. [DOI] [PubMed] [Google Scholar]
- 34.Spetz J, Smith MW, Ennis SF. Physician incentives and the timing of cesarean sections: evidence from California. Med Care. 2001 Jun;39(6):536–550. doi: 10.1097/00005650-200106000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011 Jul;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bailit JL, Love TE, Mercer B. Rising cesarean rates: are patients sicker? Am J Obstet Gynecol. 2004 Sep;191(3):800–803. doi: 10.1016/j.ajog.2004.01.051. [DOI] [PubMed] [Google Scholar]
- 37.Pang MW, Leung TN, Lau TK, Hang Chung TK. Impact of first childbirth on changes in women's preference for mode of delivery: follow-up of a longitudinal observational study. Birth. 2008 Jun;35(2):121–128. doi: 10.1111/j.1523-536X.2008.00225.x. [DOI] [PubMed] [Google Scholar]
- 38.Vergani P, Ornaghi S, Pozzi I, Beretta P, Russo FM, Follesa I, Ghidini A. Placenta previa: distance to internal os and mode of delivery. Am J Obstet Gynecol. 2009 Sep;201(3):266.e1–266.e5. doi: 10.1016/j.ajog.2009.06.009. Epub 2009 Jul 24. [DOI] [PubMed] [Google Scholar]
- 39.ACOG Practice Bulletin Assessment of Intrapartum Fetal Heart Rate Tracings. Number 116, Obstetrics & Gynecology. 2010;116:1232–1240. doi: 10.1097/AOG.0b013e3182004fa9. [DOI] [PubMed] [Google Scholar]