Abstract
Background
Ependymoma is the most common glial tumor of the adult spinal cord. Current consensus recommends surgical resection with gross total resection (GTR) whenever possible. We performed a comprehensive review of the literature to evaluate whether adjuvant radiotherapy after subtotal resection (STR) has any benefit.
Methods
A PubMed search was performed to identify adult patients with spinal cord ependymoma who underwent surgical resection. Only patients who had clearly defined extent of resection with or without adjuvant radiotherapy were included for analysis. Kaplan-Meier and multivariate Cox regression survival analyses were performed to determine the effects of adjuvant radiotherapy on progression-free survival (PFS) and overall survival (OS).
Results
A total of 348 patients underwent surgical resection of spinal cord ependymomas, where GTR was obtained in 77.0% (268/348) of patients. Among those who received STR, 58.8% (47/80) received adjuvant radiotherapy. PFS was significantly prolonged among those who received adjuvant radiotherapy after STR (log rank; P < .001). This prolonged PFS with adjuvant radiotherapy remained significant in multivariate Cox regression analysis (STR versus STR + RT group; hazard ratio (HR) = 2.26, P = .047). By contrast, improved OS was only associated with GTR (GTR versus STR + RT group; HR = 0.07, P = .001) and benign ependymomas (HR = 0.16, P = .001).
Conclusions
Surgery remains the mainstay treatment for spinal cord ependymomas, where GTR provides optimal outcomes with longest PFS and OS. Adjuvant radiotherapy prolongs PFS after STR significantly, and OS is improved by GTR and benign tumor grade only.
Keywords: ependymoma, extent of resection, radiotherapy, recurrence, spinal cord, spine
Spinal cord ependymomas are the most common intramedullary glial tumors in adults.1–7 A large population-based cancer registry (Surveillance, Epidemiology, and End Results study) has reported that ependymomas are more common in the spinal cord than in intracranial regions across all age groups (36.2% spine, 22.2% infratentorial, and 11.8% supratentorial), occurring more often in males (56.9%).8 Although spinal cord ependymomas generally have better prognosis than do other intramedullary glial tumors,4,9 factors affecting prognosis have not been clearly defined. Some studies indicate that older age and spinal cord tumor independently had better survival rates, compared with younger age and intracranial tumor (either supratentorial or infratentorial), respectively,10 although a consensus in prognostic factors has not been reached. Further studies identifying factors important for improving outcomes are critical to improve clinical management and prognosis. Ideally, an optimal treatment paradigm for an individual patient should be defined based on tumor features, such as histology, tumor location, radiographic findings, and presenting symptoms to provide optimal progression-free survival (PFS) and overall survival (OS).
Factors that have been shown previously to affect prognosis are tumor grade,11–13 tumor size,14 length of clinical history,15 preoperative neurological status,16 presence of distant metastasis,17 adjuvant radiotherapy,14,18–22 and extent of resection.1,23–27 Among these factors, extent of resection with gross total resection (GTR) seems to be the most consistent variable in predicting improved OS and PFS, whereas others remain controversial.3,7,28 Of importance, advancements in microsurgical techniques have allowed en bloc GTR over piecemeal subtotal resection (STR) as the standard of care for spinal cord ependymomas,15,16,23–27 despite a variety of complications associated with surgery.29 When GTR is not possible, however, because of infiltration into surrounding spinal cord or nerve roots, many authors have recommended adjuvant radiotherapy.7,14,18–22,28,30
Despite general recommendations supporting the role of adjuvant radiotherapy,14,18–22 there are controversies. For example, some studies failed to show significant improvement in postoperative outcomes26,31 with added morbidity associated with radiation.3,32–34 To help clarify this controversy, we performed a comprehensive review of the literature on patients with classic spinal cord ependymoma (World Health Organization [WHO] grade II and III) who underwent surgical resection to determine whether adjuvant radiotherapy improves tumor control.
Materials and Methods
Article Selection
A comprehensive systematic review of the English-language literature was performed. An integrative analysis was performed, in which individual patient data from studies were pooled and statistically analyzed. Aggregated data sets, in which individual patient data were grouped, were not included in this analysis because the goal of the study was to analyze the individual patient data with long follow-up periods to allow analysis of PFS and OS with use of Kaplan-Meier and Cox regression survival analyses. Articles were identified via PubMed search using the key word “ependymoma;” this resulted in 3765 articles published from 1965 through 2011. All articles were individually reviewed to identify patients with surgical spinal cord ependymoma in which the extent of resection (GTR vs. STR) was clearly identifiable. We initially identified 80 articles with a total of 425 patients who met the criteria. Seventy-seven of these patients with myxopapillary ependymomas, WHO grade I tumors, were not included in the analysis. The remaining 348 patients from 68 articles with WHO grade II and III spinal cord ependymomas were analyzed.16,20,21,25,27,30,35–96 Weighted meta-analysis (i.e., 5- and 10-year PFS and OS) could not be performed because these statistics were not consistently reported in large aggregated studies. The median follow-up period for all patients was 48 months, and the number of patients included from each study varied from 1 to 30 patients.
Data Extraction
Data from case reports and institutional series were extracted with the following information: age, sex, extent of resection (GTR vs. STR), adjuvant radiotherapy, morbidity, recurrence or progression of disease, time to recurrence or progression of disease, mortality, time to mortality, and duration of follow-up. Treatment paradigms were stratified into 4 groups: GTR, GTR + RT, STR, or STR + RT. Survival analyses were performed for GTR, STR, and STR + RT groups because the main goal of the study was to determine the role of adjuvant radiotherapy in patients receiving STR. Patients who underwent biopsy or surgery with chemotherapy were excluded.
Statistical Analysis
PFS and OS were analyzed using building Kaplan-Meier curves, and differences were assessed using log rank or Tarone-Ware (when curves cross each other) test. This analysis was followed by Cox proportional hazards analysis by backward stepwise model selection to adjust for confounding variables including age, sex, extent of resection, tumor grade (WHO II vs. III), morbidity, tumor location (upper: cervicomedullary to cervicothoracic; lower: thoracic, lumbar, and conus), and radiation treatment. Hazard ratios (HRs) with 95% confidence intervals (CIs) were estimated. Continuous variables were analyzed using the t test or analysis of variance with post hoc Tukey test, and categorical values were analyzed using the Pearson's χ2 test. Fisher's exact test was used if the expected cell count in a contingency table was <5. P <.05 was considered to be statistically significant. Analyses were performed using the statistical software package SPSS, version 20 (SPSS).
Results
Clinical Characteristics
The literature search yielded a total of 68 manuscripts with a total of 348 patients who underwent surgical treatment for classic spinal cord ependymomas with clearly identifiable extent of resection.16,20,21,25,27,30,35–96 The mean age was 41.0 years with a range of 18–73 years, and there were more males (57.6%) than females (42.4%) overall (Table 1).
Table 1.
Demographic characteristics of patients who underwent surgical resection for spinal cord ependymomas
| Characteristic | GTR | GTR + RT | STR | STR + RT | P |
|---|---|---|---|---|---|
| N | 258 | 10 | 33 | 47 | |
| Mean age ± SEM | 41.9 ± 0.8 | 39.0 ± 4.2 | 39.7 ± 2.6 | 37.2 ± 2.2 | .176a |
| Gender (male) | 56.4% | 62.5% | 58.1% | 63.2% | .874b |
| Anaplastic ependymomas | 0.8% (2/238) | 10% (1/10) | 13.3% (4/30) | 9.8% (4/41) | <.001c |
| Location of tumor | |||||
| Upper | 68.6% (177/258) | 30% (3/10) | 42.4% (14/33) | 48.9% (23/47) | |
| Lower | 31.4% (81/258) | 70% (7/10) | 57.6% (19/33) | 51.1% (24/47) | <.001b |
Mean age and gender did not differ across different treatment paradigms, while number of anaplastic ependymomas and location of tumors, broadly divided into upper and lower spinal cord, were significantly different across different treatment paradigms.
aAnalysis of variance.
bχ2 test.
cFisher's exact.
Of 348 patients, 268 (77.0%) received GTR, and the remaining 80 (23.0%) received STR. In the STR group, 47 (58.8%) of 80 received adjuvant RT, and only 10 (3.7%) of 268 received adjuvant radiotherapy after GTR. We grouped tumors into benign (WHO grade II) or anaplastic (WHO grade III) ependymomas. Overall, 11 (3.4%) of 319 tumors were anaplastic. The number of anaplastic ependymomas differed significantly across treatment paradigms with significantly more anaplastic tumors in the STR groups (8 [11.3%] of 71), compared with the GTR groups (3 [1.2%] of 248; P < .001) (Table 1). Moreover, ependymomas in the lower spinal cord had significantly lower GTR rate (67.2%, 88 of 131), compared with the tumors in the upper spinal cord (83.0%, 180 of 217; P < .001).
Adjuvant RT Improves PFS after STR
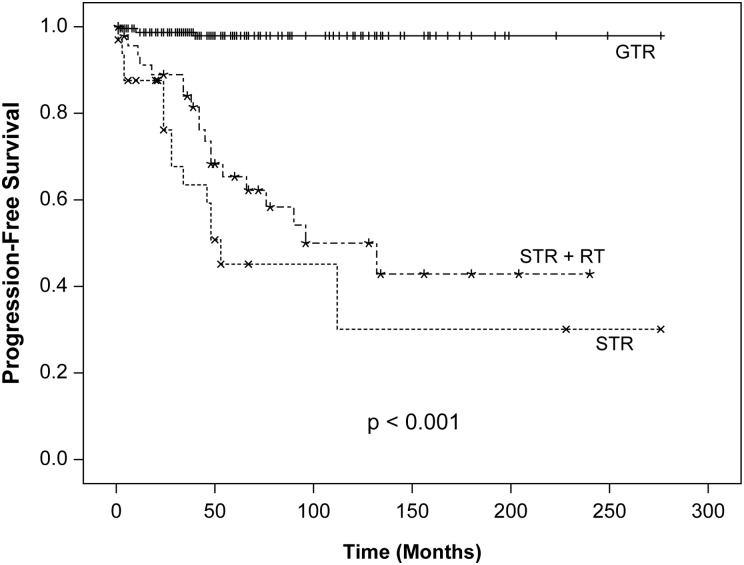
We first performed Kaplan-Meier analysis to determine whether adjuvant radiotherapy had a significant effect on PFS and OS after STR. It was clear from our analysis that GTR provided the best PFS and OS (log rank, P < .001; Fig. 1 and 2). Of importance, adjuvant RT significantly prolonged PFS in the STR group. The median survival time (50% PFS) was 48 months in the STR group, which was doubled to 96 months with adjuvant radiotherapy in the STR + RT group. Because of lack of sufficient events, median survival times could not be calculated for the GTR group. Five-year PFS rates for GTR, STR + RT, and STR groups were 97.9%, 65.3%, and 45.1%, respectively, with 20.2% improvement in PFS with adjuvant RT after STR. In contrast to PFS, adjuvant radiotherapy did not improve OS significantly in patients who received STR (pairwise Tarone-Ware, P = .643). Five-year OS for GTR, STR + RT, and STR groups was 98.8%, 79.3%, and 73.7%, respectively.
Fig. 1.
PFS by treatment paradigm. We built Kaplan-Meier curves to determine whether adjuvant RT prolongs PFS among patients who receive STR for spinal cord ependymomas. As seen in this figure, GTR provides the best PFS, which was significantly longer, compared with STR and STR + RT groups (log rank, P < .001). The median survival time (50% PFS) for the STR + RT group was twice as long (96 months), compared with the STR group (48 months).
Fig. 2.
OS, by treatment paradigm. In accordance with PFS, GTR provided the best OS, which was statistically longer, compared with that among STR or STR + RT groups (log rank; P < .001). However, there was no difference in OS between the STR and STR + RT groups.
Our previous analysis, however, revealed that the grades of tumors were significantly different across different treatment paradigms (Table 1); this could be responsible for the differences found in Kaplan-Meier analysis. Thus, we performed multivariate Cox proportional hazards analysis to determine whether adjuvant RT prolongs PFS after STR while accounting for other possible confounding variables, including age, sex, extent of resection, grade of tumor (WHO II vs III), morbidity, and tumor location. We found that different treatment paradigms resulted in significant difference in PFS (Table 2). Of most importance, STR alone had an HR of 2.26 (95% CI = 1.01–5.07; P = .047), compared with STR + RT. Consistent with the Kaplan-Meier analysis, GTR provided the best PFS outcomes, with HR of 0.06 (95% CI = 0.02–0.23; P < .001), compared with STR + RT. Furthermore, tumor grade remained significant in the analysis, with anaplastic WHO grade III tumors having HR of 2.88 (95% CI = 1.13–7.34; P = .026), compared with benign WHO grade II tumors. Other variables did not remain significant and were dropped from the analysis.
Table 2.
Multivariate Cox proportional hazards analysis of PFS
| Variable | HR | 95% CI | P |
|---|---|---|---|
| STR + RT | 1 | ||
| GTR | 0.06 | 0.02–0.23 | <.001 |
| STR | 2.26 | 1.01–5.07 | .047 |
| WHO grade III | 2.88 | 1.13–7.34 | .026 |
We performed backward stepwise model selection to determine the PFS benefit of adjuvant radiation treatment in patients who received STR while accounting for age, gender, extent of resection, tumor grade (WHO grade II vs. III), morbidity, and tumor location (upper: cervicomedullary to cervicothoracic, lower: thoracic, lumbar, and conus). We used STR + RT groups as the control for comparison. Only treatment paradigms and tumor grade remained significant in the analysis, with significantly improved PFS in the STR + RT group compared to STR group.
We then performed the same multivariate Cox regression analysis for OS while accounting for the same confounding variables (Table 3). In contrast to PFS, there were no significant improvements in OS with adjuvant RT after STR (STR: HR 1.01, P = .99, when compared with STR + RT). Best OS outcomes were achieved with GTR (HR 0.07, P = .001, 95% CI = 0.02–0.36, when compared with STR + RT). Tumor grade was again found to be a significant variable, with anaplastic tumors having HR of 6.08 (95% CI=2.01–18.37; P = .001), compared with benign tumors. As before, other variables did not remain significant and were dropped from the analysis.
Table 3.
Multivariate Cox proportional hazards analysis of OS
| Variable | HR | 95% CI | P |
|---|---|---|---|
| STR + RT | 1 | ||
| GTR | 0.07 | 0.02–0.36 | .001 |
| STR | 1.01 | 0.33–3.03 | .99 |
| WHO grade III | 6.08 | 2.01–18.37 | .001 |
We performed backward stepwise model selection to determine the OS benefit of adjuvant radiation treatment in the STR group while accounting for age, gender, extent of resection, tumor grade (WHO grade II vs. III), morbidity, and tumor location (upper: cervicomedullary to cervicothoracic, lower: thoracic, lumbar, and conus). Similar to PFS, only treatment paradigms and tumor grade remained significant in the analysis, but only GTR remained as the beneficial variable for improving OS with no improvement with adjuvant radiotherapy in the STR groups.
Radiation Dose Does Not Affect Recurrence or Survival
There is some evidence that total dose of radiotherapy may influence clinical outcomes in patients with spinal cord ependymomas who undergo STR.30 A study by Shaw et al., for example, used a median dose of 50 Gy, with a range of 36–57 Gy, and suggested that total dose >50 Gy may be superior.3,30 Thus, we stratified the patients treated with adjuvant RT into 2 groups: those treated with <50 Gy (40.7 ± 2.2 Gy; range, 20–48.6; n= 16) and those treated with ≥50 Gy (51.8 ± 0.5; range, 50–60 Gy; n = 24) of total radiation. The dose of radiation given was available for 40 patients, with 16 patients receiving <50 Gy and the remaining 24 patients receiving ≥50 Gy of total radiation. Overall, there were 6 recurrences in the <50 Gy group (37.5%) and 10 in the ≥50 Gy group (41.7%). We again constructed Kaplan-Meier curves, which showed that there were no significant differences between the 2 groups in PFS (P = .559) or OS (P = .510; Fig. 3A and B). Moreover, radiation dose did not remain as a significant variable in multivariate Cox regression analysis for both PFS and OS while accounting for other important confounding variables, such as extent of resection and tumor grade (data not shown).
Fig. 3.
Kaplan-Meier analysis of PFS and OS, by radiation dose. Neither PFS (A; P = .559) nor OS (B; P = .510) were significantly affected by radiation dose (<50 Gy vs. ≥50 Gy). These results were confirmed with multivariate Cox regression analysis (data not shown).
Discussion
Although adjuvant RT is routinely given by most providers after STR of spinal cord ependymomas, the benefit with respect to prolonging PFS and OS is controversial.14,18,19,21,22,26,31 Moreover, the recommended dose of radiation has not been clearly defined30 because high doses of radiation may be associated with increased risk of radiation myelopathy.32–34 Thus, we performed a comprehensive review of the literature by performing an integrative analysis (in which the previously reported individual cases are pooled and analyzed) to determine whether adjuvant RT can prolong PFS in patients with spinal cord ependymoma, specifically focusing on those who received STR.
Our results indicate that 77.0% of patients with spinal cord ependymoma who undergo surgical resection received a GTR. This treatment paradigm provides the best outcomes in terms of both PFS and OS (Fig. 1 and 2), which is consistent with previous reports.15,16,23–27 Five-year PFS and OS rates were 97.9% and 98.8%, respectively, in our study, suggesting that GTR can provide a definitive cure in most cases. Thus, GTR should be the goal of every spinal cord ependymoma surgery if significant neurological morbidity can be avoided.29
Spinal cord ependymomas that are subtotally resected tend to recur at rates up to 50%–70% without adjuvant therapy,2,7,97 which is consistent with the findings in our current study. Five-year recurrence rate after STR was 54.9%, with 5-year survival rate of 73.7% in this study. This high recurrence rate has promoted the use of adjuvant RT for patients receiving STR,14,19–21 although without clear evidence supporting improved outcomes. For example, a study by Celli et al. showed that postoperative RT did not affect outcomes in patients with filum terminale ependymomas.26 By contrast, a study by a group at the MD Anderson Cancer Center found favorable outcomes with adjuvant RT for myxopapillary ependymomas,18 which most often occur in the filum terminale. A study by Abdel-Wahab et al. found that adjuvant RT prolonged PFS in a univariate Cox proportional hazards model,31 and this was found to be not significant in a multivariable model. Clearly, one of the major difficulties in analyzing outcomes with different treatment paradigms has been to account for other confounding factors, such as grade of tumor and extent of resection. Thus, in this report, we performed a Kaplan-Meier and Cox regression survival analyses on patients with previously reported spinal cord ependymoma to determine whether adjuvant RT improves tumor control after STR.
Overall, our analysis showed a significantly prolonged PFS with adjuvant RT after STR. Five-year PFS was improved by 20.2% from 45.1% in the STR group to 65.3% in the STR + RT group. Because these results may have been confounded by the higher percentage of anaplastic ependymomas in the STR group (13.3%), compared with the STR + RT group (9.8%), we performed multivariate Cox regression analysis to account for other confounding variables, including tumor grade. This analysis confirmed prolonged PFS with adjuvant RT after STR in our dataset.
Surprisingly, OS among patients receiving STR was not affected by adjuvant RT. This could be attributable to the benign nature of the majority of spinal cord ependymomas with low mortality rates. Moreover, it was difficult to discern the true etiology of mortality in these patients on the basis of their description in the literature. It is possible that patients die more often of complications related to their disease (such as neurological deficits, immobility, deep venous thrombosis, and infections) and not directly due to disease recurrence. If such were the case, one would not expect to see similar correlations between PFS and OS, which may be partly responsible for the variable beneficial results for PFS and OS with adjuvant RT in the STR group.
The optimal dose of radiation for subtotally resected spinal cord ependymomas also still remains to be determined. A study by Shaw et al. found that 6 (35%) of 7 patients who received ≤50 Gy postoperative RT recurred, and only 1 (20%) of 5 recurred after receiving >50 Gy. Thus, they recommended delivering a total dose of 55 Gy, regardless of extent of surgery.30 In our study, however, we found no difference in outcomes for PFS and OS based on radiation dose, in both univariate and multivariate analyses. However, it is likely that there are many other confounding variables, such as whole spine versus local radiation, tumor grade, and histology, which may affect outcomes. Further studies are needed to delineate the effects of these variables. Most authors currently recommend doses of 45–54 Gy with long-term follow-up because recurrence can occur many years after initial treatment.19
Because this is a retrospective integrative analysis of pooled individual patient data from multiple studies, there are clear inherent limitations involved with this method. Studies in general may be more likely to only report cases with good outcomes, and thus, our results may be biased toward better outcomes than in reality. Furthermore, the differences in patient treatment at different institutions, such as surgeon's experience, whether adjuvant RT is used, follow-up protocol, and protocols involving treatment of recurrent tumors, were not taken into account and may have affected results presented in this study. Specifically, individual patient data used in this study may not completely reflect the patients with spinal cord ependymoma as a whole. Because aggregated patient data (where individual patient data are grouped) were not used in this study, our results can be biased by individual case reports or smaller studies presented by institutions with a relatively less experience in treating patients with spinal cord ependymomas. Although our study did not include some large studies that did not report individual patient data, a number of publications used in our study contained cohorts of patients >20 from authors with significant experience with spinal cord ependymoma surgery.16,20,25,35,39,56,58,60,83 Our results, thus, could represent the sum of results achieved at large referral centers to small institutions with relatively fewer experiences with spinal cord ependymomas and may not represent similar results obtained at busy institutions with large volumes of patients with spinal cord ependymoma. Overall, our findings would be best confirmed in a prospectively randomized trial conducted at multiple institutions with the capacity to treat spinal cord ependymomas with use of both surgical resection and adjuvant RT.
In summary, our results indicate that adjuvant RT can prolong PFS in patients with spinal cord ependymoma who receive STR, and OS is only improved by GTR and benign tumor grade. GTR provides optimal outcomes with longest PFS and OS, and thus, GTR should be the main goal of every spinal cord ependymoma surgery. When STR is the best achievable surgical outcome, adjuvant RT should be strongly considered with careful long-term follow-up.
Conclusion
Our results show that best outcomes for spinal cord ependymomas are achieved with GTR, which is consistent with previous findings.3,7,28 Moreover, adjuvant RT can prolong PFS among patients who receive STR. Although adjuvant RT may not ultimately affect OS, decreasing recurrence can appreciably benefit patient outcomes by avoiding repeated surgeries, which are associated with significant morbidities.29 Prolonged surveillance is recommended, regardless of extent of surgery or adjuvant therapies because recurrence can occur many years after surgical resection of spinal cord ependymomas.
Funding
This work was supported by National Research Service Award from the National Institutes of Health (F32NS073326-01 to M. C. O.) and Reza and Georgianna Khatib Endowed Chair in Skull Base Tumor Surgery (to A.T. P.).
Acknowledgments
Conflict of interest statement. None declared.
References
- 1.Abdelwahab M, Etuk B, Palermo J, et al. Spinal cord gliomas: A multi-institutional retrospective analysis. Int J Radiat Oncol Biol Phys. 2006;64(4):1060–1071. doi: 10.1016/j.ijrobp.2005.09.038. [DOI] [PubMed] [Google Scholar]
- 2.Cooper PR. Outcome after operative treatment of intramedullary spinal cord tumors in adults: intermediate and long-term results in 51 patients. Neurosurgery. 1989;25(6):855–859. doi: 10.1097/00006123-198912000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Gilbert MR, Ruda R, Soffietti R. Ependymomas in adults. Curr Neurol Neurosci Rep. 2010;10(3):240–247. doi: 10.1007/s11910-010-0109-3. [DOI] [PubMed] [Google Scholar]
- 4.Helseth A, Mork SJ. Primary intraspinal neoplasms in Norway, 1955 to 1986. A population-based survey of 467 patients. J Neurosurg. 1989;71(6):842–845. doi: 10.3171/jns.1989.71.6.0842. [DOI] [PubMed] [Google Scholar]
- 5.Parsa AT, Lee J, Parney IF, Weinstein P, McCormick PC, Ames C. Spinal cord and intradural-extraparenchymal spinal tumors: current best care practices and strategies. J Neurooncol. 2004;69(1–3):291–318. doi: 10.1023/b:neon.0000041889.71136.62. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz TH, McCormick PC. Intramedullary ependymomas: clinical presentation, surgical treatment strategies and prognosis. J Neurooncol. 2000;47(3):211–218. doi: 10.1023/a:1006414405305. [DOI] [PubMed] [Google Scholar]
- 7.Ruda R, Gilbert M, Soffietti R. Ependymomas of the adult: molecular biology and treatment. Curr Opin Neurol. 2008;21(6):754–761. doi: 10.1097/WCO.0b013e328317efe8. [DOI] [PubMed] [Google Scholar]
- 8.McGuire CS, Sainani KL, Fisher PG. Incidence patterns for ependymoma: a surveillance, epidemiology, and end results study. J Neurosurg. 2009;110(4):725–729. doi: 10.3171/2008.9.JNS08117. [DOI] [PubMed] [Google Scholar]
- 9.Tseng JH, Tseng MY. Survival analysis of 459 adult patients with primary spinal cancer in England and Wales: a population-based study. Surg Neurol. 2007;67(1):53–58. doi: 10.1016/j.surneu.2006.04.011. discussion 58. [DOI] [PubMed] [Google Scholar]
- 10.McGuire CS, Sainani KL, Fisher PG. Both location and age predict survival in ependymoma: a SEER study. Pediatr Blood Cancer. 2009;52(1):65–69. doi: 10.1002/pbc.21806. [DOI] [PubMed] [Google Scholar]
- 11.Waldron JN, Laperriere NJ, Jaakkimainen L, et al. Spinal cord ependymomas: a retrospective analysis of 59 cases. Int J Radiat Oncol Biol Phys. 1993;27(2):223–229. doi: 10.1016/0360-3016(93)90231-j. [DOI] [PubMed] [Google Scholar]
- 12.Mork SJ, Loken AC. Ependymoma: a follow-up study of 101 cases. Cancer. 1977;40(2):907–915. doi: 10.1002/1097-0142(197708)40:2<907::aid-cncr2820400247>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 13.Armstrong TS, Vera-Bolanos E, Bekele BN, Aldape K, Gilbert MR. Adult ependymal tumors: prognosis and the M. D. Anderson Cancer Center experience. Neuro-Oncology. 2010;12(8):862–870. doi: 10.1093/neuonc/noq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wahab SH, Simpson JR, Michalski JM, Mansur DB. Long term outcome with post-operative radiation therapy for spinal canal ependymoma. J Neurooncol. 2007;83(1):85–89. doi: 10.1007/s11060-006-9310-2. [DOI] [PubMed] [Google Scholar]
- 15.Cervoni L, Celli P, Fortuna A, Cantore G. Recurrence of spinal ependymoma. Risk factors and long-term survival. Spine (Phila Pa 1976) 1994;19(24):2838–2841. doi: 10.1097/00007632-199412150-00019. [DOI] [PubMed] [Google Scholar]
- 16.Hanbali F, Fourney DR, Marmor E, et al. Spinal cord ependymoma: radical surgical resection and outcome. Neurosurgery. 2002;51(5):1162–1172. doi: 10.1097/00006123-200211000-00010. discussion 1172–1164. [DOI] [PubMed] [Google Scholar]
- 17.Marks JE, Adler SJ. A comparative study of ependymomas by site of origin. Int J Radiat Oncol Biol Phys. 1982;8(1):37–43. doi: 10.1016/0360-3016(82)90382-0. [DOI] [PubMed] [Google Scholar]
- 18.Akyurek S, Chang EL, Yu TK, et al. Spinal myxopapillary ependymoma outcomes in patients treated with surgery and radiotherapy at M.D. Anderson Cancer Center. J Neurooncol. 2006;80(2):177–183. doi: 10.1007/s11060-006-9169-2. [DOI] [PubMed] [Google Scholar]
- 19.Gomez DR. High failure rate in spinal ependymomas with long-term follow-up. Neuro-Oncology. 2005;7(3):254–259. doi: 10.1215/S1152851704001231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin YH, Huang CI, Wong TT, et al. Treatment of spinal cord ependymomas by surgery with or without postoperative radiotherapy. J Neurooncol. 2005;71(2):205–210. doi: 10.1007/s11060-004-1386-y. [DOI] [PubMed] [Google Scholar]
- 21.Peschel RE, Kapp DS, Cardinale F, Manuelidis EE. Ependymomas of the spinal cord. Int J Radiat Oncol Biol Phys. 1983;9(7):1093–1096. doi: 10.1016/0360-3016(83)90402-9. [DOI] [PubMed] [Google Scholar]
- 22.Whitaker SJ, Bessell EM, Ashley SE, Bloom HJ, Bell BA, Brada M. Postoperative radiotherapy in the management of spinal cord ependymoma. J Neurosurg. 1991;74(5):720–728. doi: 10.3171/jns.1991.74.5.0720. [DOI] [PubMed] [Google Scholar]
- 23.Sonneland PR, Scheithauer BW, Onofrio BM. Myxopapillary ependymoma. A clinicopathologic and immunocytochemical study of 77 cases. Cancer. 1985;56(4):883–893. doi: 10.1002/1097-0142(19850815)56:4<883::aid-cncr2820560431>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 24.Asazuma T, Toyama Y, Suzuki N, Fujimura Y, Hirabayshi K. Ependymomas of the spinal cord and cauda equina: An analysis of 26 cases and a review of the literature. Spinal Cord. 1999;37(11):753–759. doi: 10.1038/sj.sc.3100902. [DOI] [PubMed] [Google Scholar]
- 25.McCormick PC, Torres R, Post KD, Stein BM. Intramedullary ependymoma of the spinal cord. J Neurosurg. 1990;72(4):523–532. doi: 10.3171/jns.1990.72.4.0523. [DOI] [PubMed] [Google Scholar]
- 26.Celli P, Cervoni L, Cantore G. Ependymoma of the filum terminale: treatment and prognostic factors in a series of 28 cases. Acta Neurochir (Wien) 1993;124(2–4):99–103. doi: 10.1007/BF01401130. [DOI] [PubMed] [Google Scholar]
- 27.Fischer G, Mansuy L. Total removal of intramedullary ependymomas: follow-up study of 16 cases. Surg Neurol. 1980;14(4):243–249. [PubMed] [Google Scholar]
- 28.Chamberlain MC. Ependymomas. Curr Neurol Neurosci Rep. 2003;3(3):193–199. doi: 10.1007/s11910-003-0078-x. [DOI] [PubMed] [Google Scholar]
- 29.Nagasawa DT, Smith ZA, Cremer N, Fong C, Lu DC, Yang I. Complications associated with the treatment for spinal ependymomas. Neurosurg Focus. 2011;31(4):E13. doi: 10.3171/2011.7.FOCUS11158. [DOI] [PubMed] [Google Scholar]
- 30.Shaw EG, Evans RG, Scheithauer BW, Ilstrup DM, Earle JD. Radiotherapeutic management of adult intraspinal ependymomas. Int J Radiat Oncol Biol Phys. 1986;12(3):323–327. doi: 10.1016/0360-3016(86)90345-7. [DOI] [PubMed] [Google Scholar]
- 31.Abdel-Wahab M, Etuk B, Palermo J, et al. Spinal cord gliomas: A multi-institutional retrospective analysis. Int J Radiat Oncol Biol Phys. 2006;64(4):1060–1071. doi: 10.1016/j.ijrobp.2005.09.038. [DOI] [PubMed] [Google Scholar]
- 32.Schultheiss TE, Stephens LC, Peters LJ. Survival in radiation myelopathy. Int J Radiat Oncol Biol Phys. 1986;12(10):1765–1769. doi: 10.1016/0360-3016(86)90317-2. [DOI] [PubMed] [Google Scholar]
- 33.van der Kogel AJ. Retreatment tolerance of the spinal cord. Int J Radiat Oncol Biol Phys. 1993;26(4):715–717. doi: 10.1016/0360-3016(93)90297-9. [DOI] [PubMed] [Google Scholar]
- 34.Wara WM, Sheline GE. Radiation therapy of malignant brain tumors. Clin Neurosurg. 1978;25:397–402. doi: 10.1093/neurosurgery/25.cn_suppl_1.397. [DOI] [PubMed] [Google Scholar]
- 35.Aghakhani N, David P, Parker F, Lacroix C, Benoudiba F, Tadie M. Intramedullary spinal ependymomas: analysis of a consecutive series of 82 adult cases with particular attention to patients with no preoperative neurological deficit. Neurosurgery. 2008;62(6):1279–1285. doi: 10.1227/01.neu.0000333299.26566.15. discussion 1285–1276. [DOI] [PubMed] [Google Scholar]
- 36.Ahyai A, Woerner U, Markakis E. Surgical treatment of intramedullary tumors (spinal cord and medulla oblongata). Analysis of 16 cases. Neurosurg Rev. 1990;13(1):45–52. doi: 10.1007/BF00638893. [DOI] [PubMed] [Google Scholar]
- 37.Akutsu H, Shibata Y, Okazaki M, Hyodo A, Matsumura A. Intramedullary clear cell ependymoma in the cervical spinal cord: case report. Neurosurgery. 2000;47(6):1434–1437. discussion 1437–1438. [PubMed] [Google Scholar]
- 38.Alvisi C, Cerisoli M, Giulioni M. Intramedullary spinal gliomas: long-term results of surgical treatments. Acta Neurochir (Wien) 1984;70(3–4):169–179. doi: 10.1007/BF01406647. [DOI] [PubMed] [Google Scholar]
- 39.Andrade FG, de Aguiar PH, Matushita H, et al. Intracranial and spinal ependymoma: series at Faculdade de Medicina, Universidade de Sao Paulo. Arq Neuropsiquiatr. 2009;67(3A):626–632. doi: 10.1590/s0004-282x2009000400010. [DOI] [PubMed] [Google Scholar]
- 40.Atalay B, Nurlu G, Oge K. Giant cervicomedullary ependymoma. Case illustration. J Neurosurg. 2003;99(1 suppl):138. doi: 10.3171/spi.2003.99.1.0138. [DOI] [PubMed] [Google Scholar]
- 41.Babu R, Jafar JJ, Huang PP, Budzilovich GN, Ransohoff J. Intramedullary abscess associated with a spinal cord ependymoma: case report. Neurosurgery. 1992;30(1):121–124. doi: 10.1227/00006123-199201000-00023. [DOI] [PubMed] [Google Scholar]
- 42.Balak N. Unilateral partial hemilaminectomy in the removal of a large spinal ependymoma. Spine J. 2008;8(6):1030–1036. doi: 10.1016/j.spinee.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 43.Baldwin H, Hadley MN, Pittman H, Spetzler RF, Drayer BP. Gadolinium-DTPA enhancement of a recurrent intramedullary ependymoma: a case report. Surg Neurol. 1989;31(3):220–223. doi: 10.1016/0090-3019(89)90121-3. [DOI] [PubMed] [Google Scholar]
- 44.Barbagallo GMV, Caltabiano R, Parisi G, Albanese V, Lanzafame S. Giant cell ependymoma of the cervical spinal cord: case report and review of the literature. Eur Spine J. 2008;18(S2):186–190. doi: 10.1007/s00586-008-0789-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boccardo M, Telera S, Vitali A. Tanycytic ependymoma of the spinal cord. Case report and review of the literature. Neurochirurgie. 2003;49(6):605–610. [PubMed] [Google Scholar]
- 46.Borkar SA, Satyarthee GD, Sharma BS. Conus ependymoma with holocord syringomyelia. Neurol India. 2009;57(3):353–354. doi: 10.4103/0028-3886.53271. [DOI] [PubMed] [Google Scholar]
- 47.Cammarota A, Gershanik OS, Garcia S, Lera G. Cervical dystonia due to spinal cord ependymoma: involvement of cervical cord segments in the pathogenesis of dystonia. Mov Disord. 1995;10(4):500–503. doi: 10.1002/mds.870100416. [DOI] [PubMed] [Google Scholar]
- 48.Chamberlain MC. Salvage chemotherapy for recurrent spinal cord ependymona. Cancer. 2002;95(5):997–1002. doi: 10.1002/cncr.10826. [DOI] [PubMed] [Google Scholar]
- 49.Clover LL, Hazuka MB, Kinzie JJ. Spinal cord ependymomas treated with surgery and radiation therapy. A review of 11 cases. Am J Clin Oncol. 1993;16(4):350–353. doi: 10.1097/00000421-199308000-00016. [DOI] [PubMed] [Google Scholar]
- 50.de Divitiis E, Spaziante R, Stella L. Giant intramedullary ependymoma. A case report. Neurochirurgia (Stuttg) 1978;21(2):69–72. doi: 10.1055/s-0028-1090325. [DOI] [PubMed] [Google Scholar]
- 51.Di Marco A, Griso C, Pradella R, Campostrini F, Garusi GF. Postoperative management of primary spinal cord ependymomas. Acta Oncol. 1988;27(4):371–375. doi: 10.3109/02841868809093557. [DOI] [PubMed] [Google Scholar]
- 52.Duffau H, Gazzaz M, Kujas M, Fohanno D. Primary intradural extramedullary ependymoma: case report and review of the literature. Spine (Phila Pa 1976) 2000;25(15):1993–1995. doi: 10.1097/00007632-200008010-00021. [DOI] [PubMed] [Google Scholar]
- 53.Elsenburg PH, Mauser HW, Veiga-Pires JA, van Veelen CW. Panmedullary ependymoma with multiple cysts complicated by fatty deposits in the proximal spinal cord. Clin Neurol Neurosurg. 1983;85(4):273–279. doi: 10.1016/0303-8467(83)90078-1. [DOI] [PubMed] [Google Scholar]
- 54.Fakhrai N, Neophytou P, Dieckmann K, et al. Recurrent spinal ependymoma showing partial remission under Imatimib. Acta Neurochirurgica. 2004;146(11):1255–1258. doi: 10.1007/s00701-004-0374-5. [DOI] [PubMed] [Google Scholar]
- 55.Fourney DR, Siadati A, Bruner JM, Gokaslan ZL, Rhines LD. Giant cell ependymoma of the spinal cord. Case report and review of the literature. J Neurosurg. 2004;100(1 Suppl Spine):75–79. doi: 10.3171/spi.2004.100.1.0075. [DOI] [PubMed] [Google Scholar]
- 56.Goto T, Ohata K, Takami T, et al. Prevention of postoperative posterior tethering of spinal cord after resection of ependymoma. J Neurosurg. 2003;99(2 suppl):181–187. doi: 10.3171/spi.2003.99.2.0181. [DOI] [PubMed] [Google Scholar]
- 57.Graca J, Gultasli N, D'Haene N, Brotchi J, Salmon I, Baleriaux D. Cystic extramedullary ependymoma. AJNR Am J Neuroradiol. 2006;27(4):818–821. [PMC free article] [PubMed] [Google Scholar]
- 58.Guidetti B. Intramedullary tumours of the spinal cord. Acta Neurochir (Wien) 1967;17(1):7–23. doi: 10.1007/BF01670413. [DOI] [PubMed] [Google Scholar]
- 59.Hentschel SJ, McCutcheon IE, Ginsberg L, Weinberg JS. Exophytic ependymomas of the spinal cord. Acta Neurochirurgica. 2004;146(9) doi: 10.1007/s00701-004-0275-7. [DOI] [PubMed] [Google Scholar]
- 60.Hoshimaru M, Koyama T, Hashimoto N, Kikuchi H. Results of microsurgical treatment for intramedullary spinal cord ependymomas: analysis of 36 cases. Neurosurgery. 1999;44(2):264–269. doi: 10.1097/00006123-199902000-00012. [DOI] [PubMed] [Google Scholar]
- 61.Ito T, Ozaki Y, Nakagawara J, Nakamura H, Tanaka S, Nagashima K. A case of cervicomedullary junction tanycytic ependymoma associated with marked cyst formation. Brain Tumor Pathol. 2005;22(1):29–33. doi: 10.1007/s10014-005-0174-5. [DOI] [PubMed] [Google Scholar]
- 62.Joaquim AF, Santos MJ, Tedeschi H. Surgical management of intramedullary spinal ependymomas. Arq Neuropsiquiatr. 2009;67(2A):284–289. doi: 10.1590/s0004-282x2009000200021. [DOI] [PubMed] [Google Scholar]
- 63.Kane PJ, el-Mahdy W, Singh A, Powell MP, Crockard HA. Spinal intradural tumours: Part II–Intramedullary. Br J Neurosurg. 1999;13(6):558–563. doi: 10.1080/02688699943051. [DOI] [PubMed] [Google Scholar]
- 64.Kaner T, Sasani M, Oktenoglu T, Solmaz B, Sarloglu AC, Ozer AF. Clinical analysis of 21 cases of spinal cord ependymoma : positive clinical results of gross total resection. J Korean Neurosurg Soc. 2010;47(2):102–106. doi: 10.3340/jkns.2010.47.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Katoh S, Ikata T, Inoue A, Takahashi M. Intradural extramedullary ependymoma. A case report. Spine (Phila Pa 1976) 1995;20(18):2036–2038. doi: 10.1097/00007632-199509150-00017. [DOI] [PubMed] [Google Scholar]
- 66.Katonis P, Kontakis G, Pasku D, Tzermiadianos M, Tzanakakis G, Hadjipavlou A. Intradural tumours of the lumbar spine presenting with low back pain: report of two cases and review of the literature. Acta Orthop Belg. 2008;74(2):282–288. [PubMed] [Google Scholar]
- 67.Kawano N, Yagishita S, Oka H, et al. Spinal tanycytic ependymomas. Acta Neuropathol. 2001;101(1):43–48. doi: 10.1007/s004010000265. [DOI] [PubMed] [Google Scholar]
- 68.Kim DJ, Kim TW, Kim Y, Park KH. Clear cell ependymoma occurring in the cauda equina. J Korean Neurosurg Soc. 2010;48(2):153–156. doi: 10.3340/jkns.2010.48.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim NR, Chung DH, Lee SK, Ha SY. Intramedullary clear cell ependymoma in the thoracic spinal cord: a case with its crush smear and ultrastructural findings. J Korean Med Sci. 2007;22(suppl):S149–S153. doi: 10.3346/jkms.2007.22.S.S149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kocak Z, Garipagaoglu M, Adli M, Uzal MC, Kurtman C. Spinal cord ependymomas in adults: analysis of 15 cases. J Exp Clin Cancer Res. 2004;23(2):201–206. [PubMed] [Google Scholar]
- 71.Kyoshima K, Akaishi K, Tokushige K, et al. Surgical experience with resection en bloc of intramedullary astrocytomas and ependymomas in the cervical and cervicothoracic region. J Clin Neurosci. 2004;11(6):623–628. doi: 10.1016/j.jocn.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 72.Langford LA, Barre GM. Tanycytic ependymoma. Ultrastruct Pathol. 1997;21(2):135–142. doi: 10.3109/01913129709021312. [DOI] [PubMed] [Google Scholar]
- 73.Lensgraf A, Young K. Ependymoma of the spinal cord presenting in a chiropractic practice: 2 case studies. J Manipulative Physiol Ther. 2006;29(8):676–681. doi: 10.1016/j.jmpt.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 74.Lonjon M, Goh KY, Epstein FJ. Intramedullary spinal cord ependymomas in children: treatment, results and follow-up. Pediatr Neurosurg. 1998;29(4):178–183. doi: 10.1159/000028718. [DOI] [PubMed] [Google Scholar]
- 75.Meneses MS, Leal AG, Periotto LB, et al. Primary filum terminale ependymoma: a series of 16 cases. Arq Neuropsiquiatr. 2008;66(3A):529–533. doi: 10.1590/s0004-282x2008000400017. [DOI] [PubMed] [Google Scholar]
- 76.Miller CA, Torack RM. Secretory ependymoma of the filum terminale. Acta Neuropathol. 1970;15(3):240–250. doi: 10.1007/BF00686770. [DOI] [PubMed] [Google Scholar]
- 77.Nadeem SQ, Feun LG, Bruce-Gregorios JH, Green B. Post radiation sarcoma (malignant fibrous histiocytoma) of the cervical spine following ependymoma (a case report) J Neurooncol. 1991;11(3):263–268. doi: 10.1007/BF00165536. [DOI] [PubMed] [Google Scholar]
- 78.Nishio S, Morioka T, Fujii K, Inamura T, Fukui M. Spinal cord gliomas: management and outcome with reference to adjuvant therapy. J Clin Neurosci. 2000;7(1):20–23. doi: 10.1054/jocn.1999.0128. [DOI] [PubMed] [Google Scholar]
- 79.Ogden AT, Fessler RG. Minimally Invasive Resection of Intramedullary Ependymoma. Neurosurgery. 2009;65(6):E1203–E1204. doi: 10.1227/01.NEU.0000360153.65238.F0. [DOI] [PubMed] [Google Scholar]
- 80.Ohata K, Takami T, Gotou T, et al. Surgical outcome of intramedullary spinal cord ependymoma. Acta Neurochir (Wien) 1999;141(4):341–346. doi: 10.1007/s007010050309. discussion 346–347. [DOI] [PubMed] [Google Scholar]
- 81.Okawara S. Ruptured spinal ependymoma simulating bacterial meningitis. Arch Neurol. 1983;40(1):54–55. doi: 10.1001/archneur.1983.04050010074023. [DOI] [PubMed] [Google Scholar]
- 82.Parekh HC, Sharma RR, Bertolis G, Davis CH, Prabhu S. Primary dorsal exophytic ependymoma. Br J Neurosurg. 1993;7(2):201–203. doi: 10.3109/02688699309103480. [DOI] [PubMed] [Google Scholar]
- 83.Peker S, Ozgen S, Ozek MM, Pamir MN. Surgical treatment of intramedullary spinal cord ependymomas: can outcome be predicted by tumor parameters? J Spinal Disord Tech. 2004;17(6):516–521. doi: 10.1097/01.bsd.0000129585.91599.5c. [DOI] [PubMed] [Google Scholar]
- 84.Plotkin SR, O'Donnell CC, Curry WT, Bove CM, MacCollin M, Nunes FP. Spinal ependymomas in neurofibromatosis Type 2: a retrospective analysis of 55 patients. J Neurosurg Spine. 2011;14(4):543–547. doi: 10.3171/2010.11.SPINE10350. [DOI] [PubMed] [Google Scholar]
- 85.Sato K, Kubota T, Ishida M, Handa Y. Spinal tanycytic ependymoma with hematomyelia—case report. Neurol Med Chir (Tokyo) 2005;45(3):168–171. doi: 10.2176/nmc.45.168. [DOI] [PubMed] [Google Scholar]
- 86.Schuurmans M, Vanneste JAL, Verstegen MJT, Furth WR. Spinal extramedullary anaplastic ependymoma with spinal and intracranial metastases. J Neurooncol. 2006;79(1):57–59. doi: 10.1007/s11060-005-9114-9. [DOI] [PubMed] [Google Scholar]
- 87.Scott M. Infiltrating ependymomas of the cauda equina. Treatment by conservative surgery plus radiotherapy. J Neurosurg. 1974;41(4):446–448. doi: 10.3171/jns.1974.41.4.0446. [DOI] [PubMed] [Google Scholar]
- 88.Shamji MF, Benoit BG, Perry A, Jansen GH. Giant cell ependymoma of the thoracic spine. Neurosurgery. 2009;64(3):E566–E567. doi: 10.1227/01.NEU.0000338428.01654.A4. [DOI] [PubMed] [Google Scholar]
- 89.Shintaku M, Nagata N, Itoh H. Tanycytic ependymoma of the spinal cord with anaplastic cytological features. Brain Tumor Pathol. 2009;26(1):7–10. doi: 10.1007/s10014-008-0239-3. [DOI] [PubMed] [Google Scholar]
- 90.Smith JA, Northcroft GB. Lumbar ependymoma. Br J Clin Pract. 1974;28(6):220–222. [PubMed] [Google Scholar]
- 91.Tait MJ, Chelvarajah R, Garvan N, Bavetta S. Spontaneous hemorrhage of a spinal ependymoma: a rare cause of acute cauda equina syndrome: a case report. Spine (Phila Pa 1976) 2004;29(21):E502–E505. doi: 10.1097/01.brs.0000143663.27275.7f. [DOI] [PubMed] [Google Scholar]
- 92.Takahashi H, Goto J, Emura I, Honma T, Hasegawa K, Uchiyama S. Lipidized (foamy) tumor cells in a spinal cord ependymoma with collagenous metaplasia. Acta Neuropathol. 1998;95(4):421–425. doi: 10.1007/s004010050819. [DOI] [PubMed] [Google Scholar]
- 93.Tsuji H, Kondo Y, Kobayashi H, Tuguro T. A huge intramedullary spinal cord ependymoma with complete recovery following total excision. No Shinkei Geka. 1975;3(1):75–79. [PubMed] [Google Scholar]
- 94.Wen BC, Hussey DH, Hitchon PW, et al. The role of radiation therapy in the management of ependymomas of the spinal cord. Int J Radiat Oncol Biol Phys. 1991;20(4):781–786. doi: 10.1016/0360-3016(91)90023-w. [DOI] [PubMed] [Google Scholar]
- 95.Wolfla CE, Azzarelli B, Shah MV. Primary extramedullary ependymoma of the thoracic spine. Case illustration. J Neurosurg. 1997;87(4):643. doi: 10.3171/jns.1997.87.4.0643. [DOI] [PubMed] [Google Scholar]
- 96.Yasui T, Hakuba A, Katsuyama J, Nishimura S. Microsurgical removal of intramedullary spinal cord tumors. Report of 14 cases. Neurol Med Chir. 1986;26(4):311–317. doi: 10.2176/nmc.26.311. [DOI] [PubMed] [Google Scholar]
- 97.Guidetti B, Mercuri S, Vagnozzi R. Long-term results of the surgical treatment of 129 intramedullary spinal gliomas. J Neurosurg. 1981;54(3):323–330. doi: 10.3171/jns.1981.54.3.0323. [DOI] [PubMed] [Google Scholar]