Abstract
To determine the association between individual substances of abuse and antiretroviral adherence, analyses require a large sample assessed using electronic data monitoring (EDM). In this analysis, EDM data from 1636 participants in 12 U.S. adherence-focused studies were analyzed to determine the associations between recent use of various substances and adherence during the preceding four weeks. In bivariate analyses comparing adherence among patients who had used a specific substance to those who had not, adherence was significantly lower among those who had recently used cocaine, other stimulants or heroin but not among those who had used cannabis or alcohol. In multivariate analyses controlling for sociodemographics, amount of alcohol use and recent use of any alcohol, cocaine, other stimulants and heroin each was significantly negatively associated with adherence. The significant associations of cocaine, other stimulants, heroin, and alcohol use with adherence suggest that these are important substances to target with adherence-focused interventions.
Keywords: HIV, AIDS, substance use, adherence, cannabis
INTRODUCTION
Substance-using individuals living with HIV/AIDS become ill more rapidly than those who do not use substances for many reasons including delays in initiating highly active antiretroviral therapy (HAART) (1, 2), a disproportionately high likelihood of dropping out of treatment (3) and addiction-related comorbidities such as cognitive impairment (4).
Sub-optimal adherence to HAART is a particularly important reason that drug users have worse viral load outcomes after beginning HAART (5). Sub-optimal adherence to HAART has been consistently associated with worse outcomes (6–9), with the specific thresholds at which non-adherence worsens outcomes depending on the regimen and resistance profile of the HIV virus (10, 11).
Identifying which substances may interfere with adherence to HAART and which do not is important for informing the best ways to improve adherence. Taken separately, studies conducted using electronic data monitoring (EDM) have modest statistical power to delineate the extent to which specific substances are independently associated with non-adherence in multivariate analyses that control for factors differentiating people who use substances from those who do not. Reviews of the literature linking substance use to non-adherence to HAART (12, 13) identify a limited number of studies using EDM (14–20).
Studies using EDM are particularly valuable when considering the association between use of specific substances and adherence because drug users appear disproportionately prone to self-report better adherence than is indicated by objective measures of adherence. In an analysis of people whose self-report was discrepant from electronically-measured adherence, recent substance use was associated with discrepant reporting (21). In a meta-analysis of the impact of alcohol use on adherence, studies that used EDM or other objective measures of adherence detected more alcohol-related lowering of adherence than studies relying on self-report (22).
In a review of published studies of HAART adherence among substance abusers, including those studies using self-report to measure adherence, only a limited number of the studies examined specific substances separately (12), and fewer still specified that the use of the substances had been recent. A study of 148 HIV-infected individuals in Los Angeles described an association between illicit drug use, but not alcohol use, and lower adherence (17). A contradictory finding from 201 former drug users who were starting a new HAART regimen found worse adherence among people who reported recent use of either alcohol or marijuana, but not among those who had used any other illicit drug (cocaine, heroin or methamphetamine) (18). A study of 85 current and former drug users prescribed methadone found a strong link between cocaine use and non-adherence but no significant effect of either heroin or alcohol use on adherence (14). A study in Los Angeles identified alcohol use and use of any illicit drug as independent predictors of non-adherence (19).
To better understand the findings from these separate studies, we examined the effect of individual substances of abuse on adherence using pooled data from the MACH14 cohort (Multisite Adherence Collaboration in HIV http://mach14.med.ucla.edu/). This study considered separately the effects of both any use and amount of use of each substance on adherence.
METHODS
Study Sample
As previously described (23), data were collected and pooled from 16 studies conducted at 14 sites across 12 states in the United States to compile the MACH14 cohort. Each study collected adherence data with EDM (e.g. MEMS™, Aardex) to estimate participants’ adherence to antiretroviral medication. This cross-sectional analysis used data from the first time-point of each study at which participants had been asked about their substance use and had EDM data for the preceding four weeks.
Measures
Different study sites had asked about substance use with different formats and over different time frames--“How many days in the last 7 did you drink alcohol?” “last 14 days,” etc. To derive a measure that could be extracted from different questions asked at different sites, substance use was standardized across sites as the proportion of measured days having used a given substance. For alcohol, the assessed timeframes ranged from 7 to 90 days with an average timeframe of 38.1 preceding days. The timeframes used were approximately the same for other substances.
Because instruments assessed substance use in the days and weeks preceding the survey administration, our estimates of HAART adherence were based on data collected during the four weeks preceding those same surveys. Adherence was measured by dividing the total number of openings by the number of prescribed doses for each medication. Adherence to any medication was capped at 100%. Adherence for a patient on multiple antiretrovirals was calculated by averaging the adherence to all measured antiretrovirals.
Data Analysis
The relationship between adherence and use of individual substances was analyzed in a series of bivariate analyses, and then in a multivariate analysis that controlled for potential confounding differences between people who did and did not use substances.
As expected, the distribution of proportion of days using each substance except alcohol was significantly positively skewed with a preponderance of zero values. Therefore, a series of bivariate analyses was conducted to determine the relationship between adherence and a dichotomous measure of “any use” or “not any use” during the measured timeframe. To determine alcohol’s effects, bivariate analyses compared alcohol abstainers to people who had used any alcohol, and to people who drank every day. Because some substances have been associated with non-adherence in women but not in men (24), a follow-up regression analysis was conducted to estimate the interaction between gender and substance use.
Next, a series of multivariate analyses were run to determine the effect of each substance after controlling for sociodemographic factors. To determine the sociodemographics to use for these analyses, potential covariates were entered into a regression model to determine which significantly (p<.05) predicted adherence. Those significantly associated with adherence were retained as covariates for all subsequent analyses. In these subsequent regressions, successive models were tested in which each substance was individually added to and withdrawn from a model with the sociodemographic variables. Two regressions were run for each substance: one with substance use as a dichotomous measure of “any use” and one with substance use as a continuous measure of the proportion of days of use.
A final multivariate regression model estimated the unique effect of each substance when all other substances of abuse were included in the model. Alpha was set at .05 for all analyses.
Sampling for Analyses
Data were drawn from twelve of the MACH14 sites that had adequate substance use and adherence data for the analyses, with sites contributing a mean of 136 participants (range between 16 and 257). The initial bivariate analysis used data from 1636 participants, and the multivariate analysis was restricted to the 1311 participants who also had data for all the covariates in these analyses.
RESULTS
Baseline Characteristics
Using data from the full (n=1636) sample, participants’ average age was 41.9 (S.D. 8.1), and racial/ethnic breakdown included 31.3% Caucasians, 46.2% African Americans, and 12.7% Hispanics. Altogether, 67.9% were male, and 40.1% were men who have sex with men (MSM). Many participants were indigent in that 80.0% had a total household income less than $20,000 per year and 57.3% had annual incomes below $10,000. Only 27.7% were employed.
A relatively high percentage reported recent alcohol use (47.7%) but only 1.8% reported drinking every day. The order of prevalence for recent use of illicit drugs was cannabis (23.6% from n of 1354 with this measure); heroin (15.3%, n=1279); cocaine (10.6%, n=1431); and other stimulants (4.1%, n=1216). The percentage of the combined sample recently using any illicit drug was 38.1% (n=1436), using any illicit drug or alcohol was 60.0% (n=1568), and using more than one substance was 22.1% (n=1568).
Mean EDM-measured adherence during the four weeks preceding the substance use assessment was 69.3% (S.D.=33.4%) and 23.5% of participants had taken 100% of their monitored antiretrovirals.
Bivariate Analyses
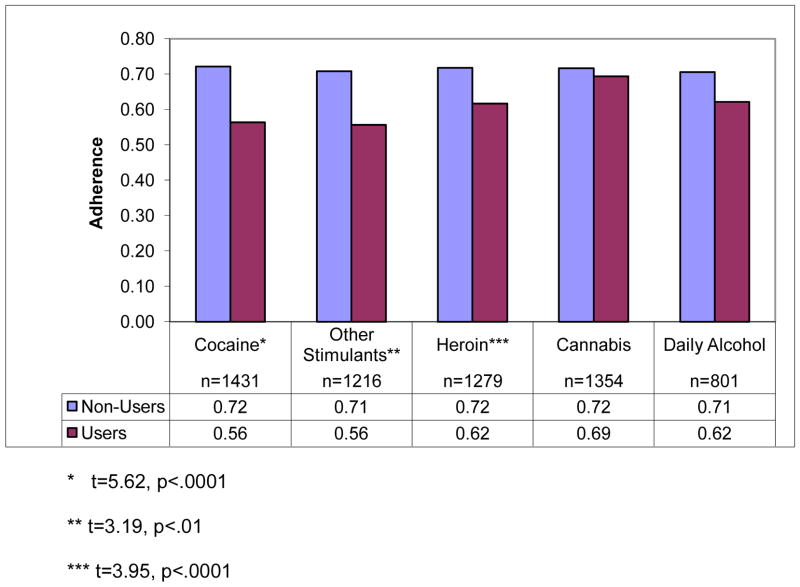
As shown in Figure 1, bivariate analyses revealed that for cocaine, other stimulants, or heroin, people who had used the substance had significantly lower adherence than people who had not used the substance. People who drank any alcohol did not have significantly lower adherence than people who had abstained from alcohol, and those people who drank alcohol every day had no lower adherence than those who did not drink at all (27 daily alcohol users and 774 abstainers; 62.1% vs.70.6% adherence, t=1.29, p= 0.196).
Figure 1.
Comparison of Adherence Among Users and Non-Users of Specific Substances
* t=5.62, p<.0001
** t=3.19, p<.01
*** t=3.95, p<.0001
To determine if the lack of main effects of any alcohol or of cannabis masked an effect limited to men or women, an analysis of the interaction of gender by substance of use was conducted. A main effect of gender was noted, with men more adherent than women, but there was no significant interaction between gender and either use of any alcohol or use of any cannabis.
Multivariate Analyses of Individual Substances
The model for determining the contribution of each substance after adjusting for other factors associated with adherence was created by regressing adherence on socio-demographic factors: age, gender, race, education (less than high school, high school, and above high school), employment (yes/no), and MSM (Men who have Sex with Men). Caucasian was the reference group for race. Factors that were significantly associated with adherence were retained and are as follows (with regression estimates in parentheses): African American (−0.050), Hispanic (−0.080), Asian American (0.037), and MSM (0.066). This model accounted for 2.8% of the variance in adherence.
A dichotomous measure of use (vs. no use) of each of the substances was then added in separate regression models controlling for these indicators of race and sexual practice. In these analyses (Table 1, column 3), any use of alcohol, cocaine, heroin, or stimulants was associated with lower adherence.
Table 1.
Multivariate Analysis of Relationship between Substance Use and Adherence
| Substance | n | B when Any Use (yes/no) Added | P- value | Variance Explained (R2) | B when Proportion Days Used Added | P- value | Variance Explained (R2) |
|---|---|---|---|---|---|---|---|
| Covariates only | 1311 | .028 | |||||
| Alcohol | 1216 | −0.039 | .03 | .036 | −0.097 | 0.04 | .035 |
| Cannabis | 1167 | −0.036 | NS | .034 | −0.050 | NS | .034 |
| Cocaine | 1166 | −0.142 | <.01 | .049 | −0.274 | <.01 | .038 |
| Stimulants | 1021 | −0.211 | <.01 | .043 | −0.316 | NS | .035 |
| Heroin | 1016 | −0.090 | <.01 | .054 | −0.352 | <.01 | .051 |
Covariates were: African American, Hispanic, Asian American, and Men who Have sex with Men. Caucasian was the reference group for race/ethnicity.
These multivariate models were then run again, substituting the continuous measures of the proportion days participants used each substance for the dichotomous measures of any use of each substance used in the prior analysis. Independent variables reflecting proportion days using alcohol, cocaine, or heroin each were significantly negatively associated with adherence in the regressions controlling for socio-demographics (shown in Table 1, columns 6–8); proportion days using cannabis and stimulants were not.
Multivariate Analyses Including All Substances
A multivariate analysis with all substances included in the same model was run to consider the extent to which substances independently impacted adherence. In the model with all substances and significant demographic variables, only any use of heroin (p=.03) was significantly associated with adherence.
Discussion
The finding of significant associations between adherence and recent use of cocaine, heroin, other stimulants, or alcohol replicates those found in smaller datasets. It is noteworthy that these effects emerge with this dataset, the largest dataset with measures of both use of individual substances and electronic measures of medication-taking. This study’s findings make it more likely that prior reports do not represent spurious associations between drug use and adherence, or associations that only apply to particular study settings.
However, overall effects were small, with even significant measures of substance use accounting for only 1% of the variance in adherence. The fact that data were pooled from many sites likely diluted the effect of drugs at particular sites. The regional variation in which drugs are popular has been well-reported, and pooling data from areas in which different substances are used (e.g. cocaine in New York and stimulants in California) dilutes the effect of each in the combined data.
Although small, the negative associations between recent cocaine or heroin use and adherence were consistent across our analyses, and are consistent with other studies that found lower adherence among people who recently used cocaine or heroin. Most studies have reported a link between stimulant use and non-adherence, and extensive qualitative data have described the disruptive effects of stimulant use on medication-taking (25). Alcohol use has also been associated with worse self-reported adherence in a meta-analysis of data from a variety of populations (22).
The lack of an association between cannabis use and adherence in this study is consistent with cannabis’ lack of effect on self-reported adherence in a large study of 764 patients at an inner city clinic (26). There are other settings in which cannabis use is somewhat less disruptive than other substance use. For example, among methadone-maintained patients, cannabis use has relatively few deleterious effects on outcome (28) and is therefore often tolerated by opioid treatment programs. However, the adherence data have not been consistent and several studies have reported worse adherence among recent cannabis users (29–31). One explanation might be that there may be different populations of cannabis users. In one interesting study of patients in Northern California, the lack of an overall association between cannabis use and adherence masked important sub-sample differences. Cannabis users who did not complain of nausea had lower adherence than non-users, but cannabis users who complained of nausea had higher adherence than patients who did not use cannabis (27).
When all the substances were added to our analyses, it was not possible to identify an effect of a specific substance other than heroin. To a large extent, the variance in adherence accounted for by other substances overlaps among substances. This shared variance may reflect common features of people who use different substances such as a lack of skills and knowledge to adhere regularly (32), or impairment that negatively impacts adherence on days when substances were used (33). It is also possible that a confounding variable such as depression is associated with both non-adherence and substance use.
There are limitations to this analysis that may have made it less able to detect effects of specific drugs. Substance use data were self-reported, and patients may have underestimated the extent of use (34). The association between alcohol use and adherence may have been stronger if data concerning quantity of alcohol use had been available instead of just frequency, as heavy drinking has been more strongly associated with non-adherence than drinking fewer drinks per day (35, 36). The summary variables mask the heterogeneity of how participants were asked questions and what time-frame was covered, thus adding noise to the signal of substance use.
Nevertheless, delineating the relationship between recent substance use and adherence has treatment implications. Knowing which substances are associated with non-adherence suggests where attention should be focused. These data suggest that it is important to address use of a variety of substances of abuse, although not necessarily cannabis, to understand non-adherence.
Contributor Information
M. I. Rosen, Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA. VA Connecticut Healthcare System, West Haven, CT, USA
A. C. Black, Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA. VA Connecticut Healthcare System, West Haven, CT, USA
J. H. Arnsten, Department of Medicine and Department of Psychiatry and Behavioral Sciences, Albert Einstein College of Medicine and Montefiore Medical Center, Einstein/Montefiore Center for AIDS Research, Bronx, New York, NY, USA
K. Goggin, Department of Psychology, University of Missouri-Kansas City, Kansas City, MO, USA
R. H. Remien, HIV Center for Clinical and Behavioral Studies, New York State Psychiatric Institute, Columbia University, New York, NY, USA
J. M. Simoni, Department of Psychology, University of Washington, Seattle, WA, USA
C. E. Golin, UNC Department of Medicine and Department of Health, Behavior and Health Education, UNC Center for AIDS, Research; Cecil G. Sheps Center for Health Services Research, Chapel Hill, NC, USA
D. R. Bangsberg, Mbarara University of Science and Technology, Boston, MA, Harvard Medical School, Boston, MA, USA. Ragon Institute of MGH, Harvard, and MIT, Boston, MA, USA. Center for Global Health, Massachusetts General Hospital, Boston, MA, USA
H. Liu, Division of Public Health and Community Dentistry, School of Medicine, University of California Los Angeles (UCLA)
References
- 1.Crystal S, Sambamoorthi U, Moynihan PJ, McSpiritt E. Initiation and continuation of newer antiretroviral treatments among medicaid recipients with AIDS. J Gen Intern Med. 2001;16(12):850–9. doi: 10.1111/j.1525-1497.2001.01025.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turner BJ, Fleishman JA, Wenger N, London AS, Burnam MA, Shapiro MF, et al. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. J Gen Intern Med. 2001;16(9):625–33. doi: 10.1046/j.1525-1497.2001.016009625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giordano TP, Gifford AL, White AC, Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44(11):1493–9. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 4.Hinkin CH, Castellon SA, Durvasula RS, Hardy DJ, Lam MN, Mason KI, et al. Medication adherence among HIV+ adults: Effects of cognitive dysfunction and regimen complexity. Neurology. 2002;59(12):1944–50. doi: 10.1212/01.wnl.0000038347.48137.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore RD, Keruly JC, Chaisson RE. Differences in HIV disease progression by injecting drug use in HIV-infected persons in care. J Acquir Immune Defic Syndr. 2004;35(1):46–51. doi: 10.1097/00126334-200401010-00006. [DOI] [PubMed] [Google Scholar]
- 6.Liu H, Golin CE, Miller LG, Hays RD, Beck CK, Sanandaji S, et al. A comparison study of multiple measures of adherence to HIV protease inhibitors. Ann Intern Med. 2001;134(10):968–77. doi: 10.7326/0003-4819-134-10-200105150-00011. [DOI] [PubMed] [Google Scholar]
- 7.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 8.Press N, Tyndall MW, Wood E, Hogg RS, Montaner JS. Virologic and immunologic response, clinical progression, and highly active antiretroviral therapy adherence. J Acquir Immune Defic Syndr. 2002;31(3):15. doi: 10.1097/00126334-200212153-00005. [DOI] [PubMed] [Google Scholar]
- 9.Vanhove GF, Schapiro JM, Winters MA, Merigan TC, Blaschke TF. Patient compliance and drug failure in protease inhibitor monotherapy. JAMA. 1996;276(24):1955–6. [PubMed] [Google Scholar]
- 10.Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43(7):939–41. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- 11.Perno CF, Ceccherini-Silberstein F, De Luca A, Cozzi-Lepri A, Gori C, Cingolani A, et al. Virologic correlates of adherence to antiretroviral medications and therapeutic failure. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S118–S22. doi: 10.1097/00126334-200212153-00006. [DOI] [PubMed] [Google Scholar]
- 12.Malta M, Strathdee SA, Magnanini MMF, Bastos FI. Adherence to antiretroviral therapy for human immunodeficiency virus/acquired immune deficiency syndrome among drug users: a systematic review. Addiction. 2008;103(8):1242–57. doi: 10.1111/j.1360-0443.2008.02269.x. [DOI] [PubMed] [Google Scholar]
- 13.Chander G, Himelhoch S, Moore RD, Chander G, Himelhoch S, Moore RD. Substance abuse and psychiatric disorders in HIV-positive patients: epidemiology and impact on antiretroviral therapy. Drugs. 2006;66(6):769–89. doi: 10.2165/00003495-200666060-00004. [DOI] [PubMed] [Google Scholar]
- 14.Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, et al. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. J Gen Intern Med. 2002;17(5):377–81. doi: 10.1046/j.1525-1497.2002.10644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McNabb J, Ross JW, Abriola K, Turley C, Nightingale CH, Nicolau DP. Adherence to Highly active antiretroviral therapy predicts virologic outcome at an inner-city human immunodeficiency virus clinic. Clin Infect Dis. 2001;33:700–705. doi: 10.1086/322590. [DOI] [PubMed] [Google Scholar]
- 16.Hinkin CH, Barclay TR, Castellon SA, Levine AJ, Durvasula RS, Marion SD, et al. Drug use and medication adherence among HIV-1 infected individuals. AIDS Behav. 2007;11(2):185–94. doi: 10.1007/s10461-006-9152-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hinkin CH, Hardy DJ, Mason KI, Castellon SA, Durvasula RS, Lam MN, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS. 2004;18:19–25. doi: 10.1097/00002030-200418001-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wagner G. Placebo practice trials: the best predictor of adherence readiness for HAART among drug users? HIV Clin Trials. 2003;4(4):269–81. doi: 10.1310/YVTR-T8EV-3TQ6-QAJC. [DOI] [PubMed] [Google Scholar]
- 19.Golin C, Liu H, Hays R, Miller L, Beck C, Ickovics J, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med. 2002;17(10):756–65. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Howard AA, Arnsten JH, Lo Y, Vlahov D, Rich JD, Schuman P, et al. A prospective study of adherence and viral load in a large multi-center cohort of HIV-infected women. AIDS. 2002;16(16):2175–82. doi: 10.1097/00002030-200211080-00010. [DOI] [PubMed] [Google Scholar]
- 21.Reinhard MJ, Hinkin CH, Barclay TR, Levine AJ, Marion S, Castellon SA, et al. Discrepancies between self-report and objective measures for stimulant drug use in HIV: cognitive, medication adherence and psychological correlates. Addict Behav. 2007;32(12):2727–36. doi: 10.1016/j.addbeh.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202. doi: 10.1097/QAI.0b013e3181b18b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu H, Wilson IB, Goggin K, Reynolds NR, Simoni JM, Golin CE, et al. MACH14: A multi-site collaboration on ART adherence among 14 institutions. doi: 10.1007/s10461-012-0272-4. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berg KM, Demas PA, Howard AA, Schoenbaum EE, Gourevitch MN, Arnsten JH. Gender Differences in factors associated with adherence to antiretroviral therapy. J Gen Intern Med. 2004;19(11):1111–7. doi: 10.1111/j.1525-1497.2004.30445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reback CJ, Larkins S, Shoptaw S. Methamphetamine abuse as a barrier to HIV medication adherence among gay and bisexual men. AIDS Care. 2003;15(6):775–85. doi: 10.1080/09540120310001618621. [DOI] [PubMed] [Google Scholar]
- 26.Lucas GM, Cheever LW, Chaisson RE, Moore RD. Detrimental effects of continued illicit drug use on the treatment of HIV-1 infection. J Acquir Immune Defic Syndr. 2001;27(3):251–9. doi: 10.1097/00126334-200107010-00006. [DOI] [PubMed] [Google Scholar]
- 27.De Jong BC, Prentiss D, McFarland W, MAchekano R, Israelski DM. Marijuana use and its association with adherence to antiretroviral therapy among HIV-infected persons with moderate to severe nausea. J Acquir Immune Defic Syndr. 2005;38(1):43–6. doi: 10.1097/00126334-200501010-00008. [DOI] [PubMed] [Google Scholar]
- 28.Epstein DH, Preston KL. Does cannabis use predict poor outcome for heroin-dependent patients on maintenance treatment? Past findings and more evidence against. Addiction. 2003;98(3):269–79. doi: 10.1046/j.1360-0443.2003.00310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kalichman SC, Rompa D. HIV treatment adherence and unprotected sex practices in people receiving antiretroviral therapy. Sex Transm Infect. 2003;79(1):59–61. doi: 10.1136/sti.79.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tucker JS, Burnam MA, Sherbourne CD, Kung F-Y, Gifford AL. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. Am J Med. 2003;114(7):573–80. doi: 10.1016/s0002-9343(03)00093-7. [DOI] [PubMed] [Google Scholar]
- 31.Corless IB, Lindgren T, Holzemer W, Robinson L, Moezzi S, Kirksey K, et al. Marijuana effectiveness as an HIV self-care strategy. Clin Nurs Res. 2009;18(2):172–93. doi: 10.1177/1054773809334958. [DOI] [PubMed] [Google Scholar]
- 32.Demas P, Schoenbaum EE, Wills TA, Doll LS, Klein RS. Stress, coping, and attitudes toward HIV treatment in injecting drug users: a qualitative study. AIDS Ed Prev. 1995;7(5):429–42. [PubMed] [Google Scholar]
- 33.Rosen MI, Rigsby MO, Dieckhaus KD, Cramer JA. Effects of illicit drug use on adherence to prescribed antiretroviral medication. Am J Addict. 2003;12(5):455–8. [PubMed] [Google Scholar]
- 34.Kosten TA, Rounsaville BJ. Sensitivity of psychiatric diagnosis based on the best estimate procedure. Am J Psych. 1992;149(9):1225–7. doi: 10.1176/ajp.149.9.1225. [DOI] [PubMed] [Google Scholar]
- 35.Braithwaite RS, Conigliaro J, McGinnis KA, Maisto SA, Bryant K, Justice AC. Adjusting alcohol quantity for mean consumption and intoxication threshold improves prediction of nonadherence in HIV patients and HIV-negative controls. Alcohol Clin Exp Res. 2008;32(9):1645–51. doi: 10.1111/j.1530-0277.2008.00732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lazo M, Gange SJ, Wilson TE, Anastos K, Ostrow DG, Witt MD, et al. Patterns and predictors of changes in adherence to highly active antiretroviral therapy: longitudinal study of men and women. Clin Infect Dis. 2007 Nov 15;45(10):1377–85. doi: 10.1086/522762. [DOI] [PubMed] [Google Scholar]