Abstract
Background
Spinal metastases are common in patients older than 60 years with cancer. Because of the uncertainty of survival and the high incidence of fatal complications, however, chemotherapy and radiotherapy generally have been considered preferable and surgery a treatment of last resort for these patients. Further, the selection criteria indicating surgery and reliable prognostic factors for survival remain controversial.
Questions/purposes
We therefore assessed surgical complications, postoperative function, and risk factors affecting their overall survival.
Methods
We retrospectively reviewed 92 patients 60 years or older (range, 60–81 years) who had surgery for spinal metastases. The surgical complications were recorded and a VAS pain score, Frankel grade, and Karnofsky score were obtained. Statistical analyses were performed to identify factors associated with survival. The minimum followup was 6 months (mean, 22 months; range, 6–78 months).
Results
Surgical complications occurred in 21 patients. Pain levels decreased postoperatively in 90% of patients and neurologic function improved in 78%. The Karnofsky status improved in 58 patients giving an improvement rate of 63%. The overall survival rates at 1 year and 3 years were 61% and 35% with a median of 15 months. Primary tumor type and Tokuhashi score independently predicted survival in patients with spinal metastases.
Conclusion
Our findings suggest surgery for spinal metastasis can achieve pain relief, neurologic improvement, and restoration of general condition but with a high risk of complications. Primary tumor type and Tokuhashi scoring independently predicted survival in patients with spinal metastases after surgery.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Bony metastases are frequent in patients affected by cancer. The spine is the most common site [3, 56], accounting for approximately 50% of bone metastases. Overall, 5% to 10% of patients with cancer eventually will have spinal metastases develop [13, 19, 38, 40, 56]. Patients aged 60 years or older are more likely to be affected by bony metastases than younger patients: the likelihood is reportedly four times greater for men and three times greater for women [1]. The most common spinal metastases (60%) are derived from breast, lung, or prostate cancer [20, 47]. All three of these metastasis types occur most frequently in patients older than 60 years [16]. Spinal metastases most often are located in the vertebral body [21]. Because vertebral destruction can lead to bone instability and spinal cord compression, these patients can present with intractable pain, impaired ambulatory ability, and neurologic dysfunction [41]. More than 90% of the patients with spinal metastases reportedly experience pain and approximately 20% have cord compression develop [19]. The situation is somewhat more complicated in older patients because clinical manifestations are more common in persons of advanced age, because most of the older people have degenerative disc diseases which can exacerbate radiculitis and spinal cord compression caused by spinal metastasis [1, 47], and most of these patients also have one or more age-related general diseases. Therefore, metastases have become a major issue in older people [1].
Some authors suggest surgically treating spinal metastatic tumors is important to relieve pain, restore neurologic function, and restore the immediate and permanent stability of the spine without excessive operative morbidity and mortality [12, 15, 16, 34, 39, 41]. Surgical complications, especially fatal cardiovascular and other systemic complications, occur more frequently in older patients than in younger patients, however [40]. Moreover, the goal of surgery in these patients is usually not to remove the entire tumor: radical operations for spinal metastases often are not possible and several studies [5, 22, 23] suggest surgery does not fundamentally change the survival rate of these patients. Furthermore, the local spinal tumor in question is only rarely the cause of patient mortality [12, 20, 29, 38, 57, 60]. Thus, the selection criteria and extent of the surgery in these patients remain controversial, and some surgeons tend to favor less invasive surgical options [32, 33]. Because most of the surgical options are palliative, Tokuhashi et al. [49] suggested it was important to base the decision to treat on the survival prognosis. That being the case, survival prognosis is one of the most important considerations in the decision to perform surgery and in determining the extent of surgery in patients with spinal metastases.
Several studies report age is one of the most important survival-related prognostic factors [1, 13, 59]. For example, 60-year-old patients have a 30% greater risk of dying of spinal metastases than do 30-year-old patients, and 70-year-old patients have a 10% greater risk of dying of spinal metastases than do 60-year-old patients [1]. Several large series [13, 40] have determined that male gender, primary tumors, comorbidities, and complications predict survival in all patients with spinal metastasis. However, it is unclear whether these factors remain predictors of survival in older patients. The lack of prognostic factors that can reliably and accurately predict individual survival in older patients complicates selecting patients for surgery and determining the magnitude of the surgery to be performed.
Therefore, we assessed patients older than 60 years with spinal metastases to (1) determine their surgical risk, especially surgical complications; (2) analyze postoperative function; and (3) determine risk factors affecting overall survival.
Patients and Methods
We retrospectively reviewed 115 patients 60 years or older with spinal metastases treated with surgery from February 2000 to September 2010. The indications for surgery [9] were (1) aggressive neurologic deficit; (2) intractable pain; (3) instability of the spine; and (4) isolated and local vertebral mass without symptoms. The contraindications for surgery were: (1) unstable cardiovascular and cerebrovascular diseases; (2) a Karnofsky performance score [28] of 30 or less; (3) local or general infection during the admission; and (4) life expectancy less than 6 months. For this study we included in-hospital patients who underwent surgery on the basis of the following criteria: (1) age 60 years or older when receiving the surgery; (2) epidural spinal metastasis with damaged spinal vertebrae; (3) clear diagnosis of the disorder; (4) CT or MRI confirmation; and (5) recorded Tomita staging [52] (Appendix 1). We excluded 23 patients with incomplete information including surgical complications, clinical outcome, and followup and imaging data for our analysis. These exclusions left 92 patients; of these 53 were men and 39 were women (a male-to-female ratio of 1.36:1) in the group. The average age of the patients at surgery was 68 years (range, 60–81 years). Sixty-one of the 92 patients had not returned for recent routine followup: 55 were contacted by telephone and six who could not be contacted by telephone were visited in their home. Of the 61 patients 50 had died and 11 were doing well at their last visits. The minimum followup was 6 months (median, 22 months; range, 6–78 months), during which 50 patients died (a mortality rate of 54%). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
The data of 92 patients who had complete information including surgical complications, clinical outcome, followup and imaging data in our database were analyzed in the study. Vertebral body lesions accounted for 96% of the vertebral metastases. In the 92 patients in our study, the most common sites of origin were the lung, kidney, and prostate, which together accounted for 54% of the cases (Table 1). Visceral metastases occurred in 19 patients and extraspinal bone metastases occurred in 47. Multiple vertebrae were involved in 39 patients and pathologic fractures were observed in 22. Relapse occurred in 15 patients and six of these patients underwent a second surgery. Other relevant data included Tomita staging, Tomita score [52], Tokuhashi score [51], re-Tokuhashi score [50], preoperative Frankel grade [14] (Appendix 1), and preoperative VAS pain score [7] (Table 2).
Table 1.
Primary tumor types of 92 patients in this study
| Primary tumor type | Number of patients | Percent |
|---|---|---|
| Breast | 4 | 4.3 |
| Colon | 7 | 7.6 |
| Kidney | 18 | 19.6 |
| Liver | 3 | 3.3 |
| Lung | 20 | 21.6 |
| Prostate | 12 | 13.0 |
| Thyroid | 7 | 7.6 |
| Unknown† | 9 | 9.8 |
| Sarcoma | 4 | 4.3 |
| Other* | 8 | 8.7 |
| Total | 92 | 100.0 |
* Others include gallbladder carcinoma, one case; uterus, two cases; larynx carcinoma, one case; lymphoma, one case; pancreas carcinoma, two cases; and malignant pheochromocytoma, one case; †unknown = patients whose primary tumor type was unclear.
Table 2.
Demographics of 92 patients older than 60 years in this study
| Factors | Number of patients | Percent |
|---|---|---|
| Age | ||
| Group 1 (≥ 70 years) | 29 | 31.5 |
| Group 2 (≥ 60 to < 70 years) | 63 | 68.5 |
| Primary tumor type | ||
| Group I (low-growth grade) | 12 | 13.0 |
| Group II (intermediate-growth grade) | 38 | 41.3 |
| Group III fast-growth grade) | 42 | 45.7 |
| Tomita stage | ||
| Intravertebral (Types 1–3) | 4 | 4.3 |
| Perivertebral involvement (Types 4–5) | 40 | 43.5 |
| Adjacent vertebral involvement (Type 6) | 18 | 19.6 |
| Multiple vertebral involvement (Type 7) | 30 | 32.5 |
| Tomita score | ||
| Group 1 (2–3 points) | 32 | 34.6 |
| Group 2 (4–5 points) | 30 | 32.6 |
| Group 3 (6–7 points) | 13 | 14.1 |
| Group 4 (8–10 points) | 17 | 18.4 |
| Tokuhashi score | ||
| Group 1 (1–4 points) | 9 | 9.8 |
| Group 2 (5–8 points) | 34 | 37.0 |
| Group 3 (9–12 points) | 49 | 53.3 |
| Re-Tokuhashi score | ||
| Group 1 (1–8 points) | 19 | 20.7 |
| Group 2 (9–11 points) | 36 | 39.1 |
| Group 3 (12–15 points) | 37 | 40.2 |
| Preoperative Frankel score | ||
| Grade A | 2 | 2.2 |
| Grade B | 4 | 4.3 |
| Grade C | 17 | 18.5 |
| Grade D | 19 | 20.6 |
| Grade E | 50 | 54.3 |
| Preoperative VAS score | ||
| Group 1 (1–4) | 12 | 13.0 |
| Group 2 (5–7) | 43 | 46.7 |
| Group 3 (8–10) | 37 | 40.2 |
| Preoperative Karnofsky score | ||
| Group 1 (0–40) | 23 | 25.0 |
| Group 2 (50–70) | 67 | 72.8 |
| Group 3 (80–100) | 2 | 2.2 |
| Overall | 92 | 100.0 |
Primary lesions involving the vertebral body occurred in the cervical spine in 12 patients, thoracic spine in 37, and lumbar spine in 43. Among patients with lesions in the cervical spine, seven had an anterior cervical tumor resection and reconstruction with vertebral bone or a titanium cage plus titanium plate fixation; three had a posterior cervical tumor resection and an occipitocervical fusion, lateral screw, or transpedicle screw fixation; and two had combined resection and fixation with a combination of anterior and posterior approaches. Among patients with lesions in the thoracic spine, four had anterior decompression or vertebral body tumor curettage and titanium mesh plus titanium plate fixation coupled with an anterior approach, 30 had a posterior tumor resection and bone graft or bone cement fusion plus pedicle screw fixation, and three had tumor resection and anterior vertebral bone or titanium cage reconstruction plus posterior pedicle screw fixation with combined approaches. Among patients with lesions in the lumbar spine, three had anterior decompression or vertebral tumor curettage and titanium mesh plus titanium plate fixation with an anterior approach, 30 had posterior tumor resection and fusion of a bone graft or bone cement plus pedicle screw fixation, and 10 had a combined approach consisting of vertebral body resection and reconstruction plus posterior pedicle screw fixation. From above, an anterior approach was used in 14 patients, a posterior approach was used in 63, and a combined anterior and posterior approach was used in 15. Although various prophylactic antibiotics were used during the long study period, we consistently used a single antibiotic administrated intravenously once 30 minutes before skin incision and continued for 3 days postoperatively.
Postoperatively, we saw most patients at 2 weeks, 3 months, and 6 months thereafter until 1 year, after which they were seen annually. We used medical records to collect demographic data, clinical function, results of the treatment, and radiographic data at each followup. We recorded and analyzed the operative blood loss, operative time, and major complications. Major complications included postoperative wound infection, mechanical complications related to graft hardware, and medical and/or surgical misadventures [11, 13]. VAS score, Frankel grade, and Karnofsky score were measured preoperatively and postoperatively. There were no missing data for VAS scores, Frankel grades, and Karnofsky scores for the 92 patients.
We used the Wilcoxon test to identify difference in the patients’ general characteristics including VAS score and Karnofsky score between preoperation and postoperation. The overall survival rate was assessed with a Kaplan-Meier life-table analysis [27]. The Kaplan-Meier method was used to estimate event–time distributions and the log-rank test to compare survival between the following groups: age (≥ 70 years or ≥ 60 to < 70 years) (Table 2), primary tumor type (low growth, intermediate growth, or fast growth), Tomita stage (intervertebral [Types 1–3], perivertebral [Types 4–5], adjacent vertebral [Type 6], or multiple vertebral [Type 7]), pathologic fracture, Tomita score, Tokuhashi score, re-Tokuhashi score, Frankel grade, VAS score, surgical complications, local recurrence, Karnofsky score, and extraspinal bone metastasis. Multivariate analysis by Cox proportional hazards model [10] was performed with all significant factors (p < 0.05) in univariate analysis to determine which independently predicted survival. All of the statistical analyses were conducted using SPSS 13.0 (SPSS Inc, Chicago, IL, USA). All of the tests were two-sided.
Results
Surgical complications occurred in 21 patients (Table 3). The most common complications were massive postoperative hemorrhage, wound infection, systemic infection, and cardiovascular disease. Three patients died in the hospital within 30 days after surgery of acute respiratory failure, heart failure, and multiple systemic infections, giving an in-hospital mortality rate of 3.4%. The average operative time was 170 ± 89 minutes (range, 72–530 minutes). The average blood loss was 1278 ± 941 mL (range, 100–4800 mL).
Table 3.
Postoperative complications of 92 patients
| Complication# | Number of patients | Percentage (%) |
|---|---|---|
| Massive hemorrhage | 11 | 12.0 |
| Would infection | 6 | 6.5 |
| Neurological injury | 4 | 4.3 |
| Systemic infection* | 5 | 5.4 |
| Implant failure | 2 | 2.2 |
| Cerebrospinal fluid leakage | 3 | 3.4 |
| Cardiovascular diseases† | 5 | 5.4 |
#Surgical complications occurred in 21 patients with one or multiple complications. One complication occurred in 12 patients, and multiple complications occurred in the remaining nine patients including two complications in five patients, three in two patients, and four in another two patients; *systemic infection includes pulmonary infection in one patient, urologic infection in one, and a combination of pulmonary and urologic infections in three; two patients died of acute respiratory failure and multiple systemic infections within 30 days after surgery; †cardiovascular diseases include heart failure in three patients and major vessel injury in two. Among them one patient died of heart failure within 30 days after surgery.
The median VAS score was 6 preoperatively while it was 2 at the final followup. Preoperative pain was reported in 89 patients (97%), whereas postoperative pain levels decreased (p < 0.001) in 81 patients, resulting in a pain relief rate of 88%. Preoperative neurologic dysfunction occurred in 73 patients (79%), and 78% improved postoperatively. The improvements were three grades in two patients, two in 24, and one in 31. The average degree of neurologic improvement was 1.2 grades (Table 4). The median postoperative Karnofsky scores increased from 60 (range, 40–80) to 70 (range, 0–80). Postoperative improvement (p < 0.001) in Karnofsky status was observed in 58 patients, resulting in an improvement rate of 63%.
Table 4.
Preoperative and postoperative neurologic function
| Preoperative Frankel score | Postoperative Frankel score | Total | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| A | 1 | 1 | 1 | 1 | 0 | 4 |
| B | 1 | 1 | 0 | 2 | 1 | 5 |
| C | 0 | 1 | 6 | 14 | 21 | 42 |
| D | 0 | 1 | 1 | 4 | 16 | 22 |
| E | 0 | 1 | 2 | 1 | 15 | 19 |
| Total | 2 | 5 | 10 | 22 | 53 | 92 |
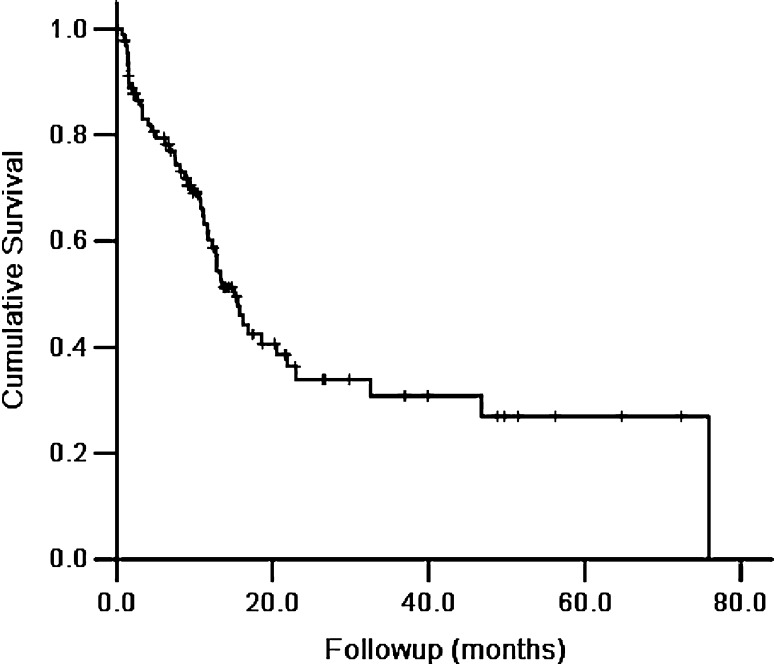
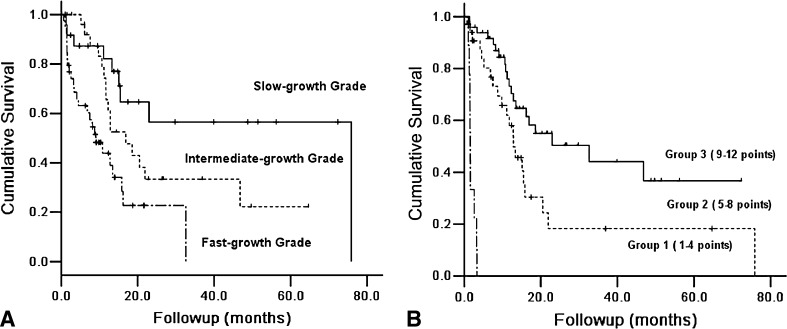
The overall survival rates for the 92 patients at 1 year and 3 years after surgery were 61% and 35%, respectively (Fig. 1) with a median survival of 15 months after surgery. The average and median intervals from surgery until death were 10 months and 7 months, respectively. Several factors were substantially associated with postoperative survival with a p value less than 0.05 (Table 5). The subsequent multivariate analysis showed that primary tumor type (hazard ratio [HR], 2.0; 95% CI, 1.4–3.1) and Tokuhashi score (HR, 0.27; CI, 0.14–0.45) independently predicted survival (Table 6). The survival curves reveal that a slow-growing primary tumor and high Tokuhashi score were associated with longer survival in patients with spinal metastases (Fig. 2). The patients with slow-growing primary tumors had an 83% survival rate at 1 year compared with 66% for intermediate-growth tumors and 35% for fast-growing tumors (Fig. 2A). The following 1-year survival rates were found for specific primary tumor types: 85% for thyroid cancer, 83% for breast, 74% for kidney, 64% for prostate, 47% for colon, 33% for liver, and 34% for lung. The Tokuhashi score also was predictive; the patients with scores of 1 to 4 had a 3.7% survival rate at 1 year compared with 53% for scores of 5 to 8 and 72% for scores of 9 to 12 (Fig. 2B). Two typical clinical patients are presented in this study, and one was diagnosed with cervical spinal metastasis from lung cancer (Fig. 3) and another with thoracic spinal metastasis from prostate cancer (Fig. 4). After surgery, both had a good clinical outcome and long-term survival. The Tokuhashi score accurately predicted survival for less than 3 months, 3 to 6 months, longer than 6 months in 78%, 41%, and 82% of the patients, respectively (Table 7).
Fig. 1.
The overall survival curve for the 92 elderly patients with spinal metastases showed the overall survival rates at 1 year and 3 years after surgery were 61% and 35%, respectively.
Table 5.
Univariate analysis of survival prognostic factors*
| Factors | p value** |
|---|---|
| Age | 0.468 |
| Primary type | 0.001 |
| Tomita stage | 0.018 |
| Visceral metastasis | 0.827 |
| Tomita score | 0.000 |
| Tokuhashi score | 0.000 |
| Revised Tokuhashi score | 0.000 |
| Preoperative Frankel score | 0.008 |
| Primary surgery | 0.062 |
| Preoperative VAS score | 0.018 |
| Preoperative Karnofsky score | 0.686 |
| Pathological fracture | 0.056 |
| Surgical complications | 0.283 |
| Extraspinal bone involved | 0.038 |
* log-rank test, n = 92; **significant at p < 0.05.
Table 6.
Multivariate analysis of survival prognostic factors (Cox proportional hazards model)
| Value | Regression coefficient | SE | Wald test | df | p value* | HR value | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Primary tumor type | 0.712 | 0.206 | 11.920 | 1 | 0.001 | 2.039 | 1.361 | 3.055 |
| Tokuhashi score | −1.298 | 0.259 | 25.114 | 1 | 0.000 | 0.273 | 0.164 | 0.454 |
* Significant at p < 0.05; SE = standard error; df = degree of freedom; HR = hazard ratio.
Fig. 2A–B.
The survival curves showed that (A) primary tumor type independently predicted survival (HR, 2.0; CI, 1.4–3.1); and (B) the Tokuhashi score also independently predicted survival (HR, 0.27; CI, 0.14–0.45).
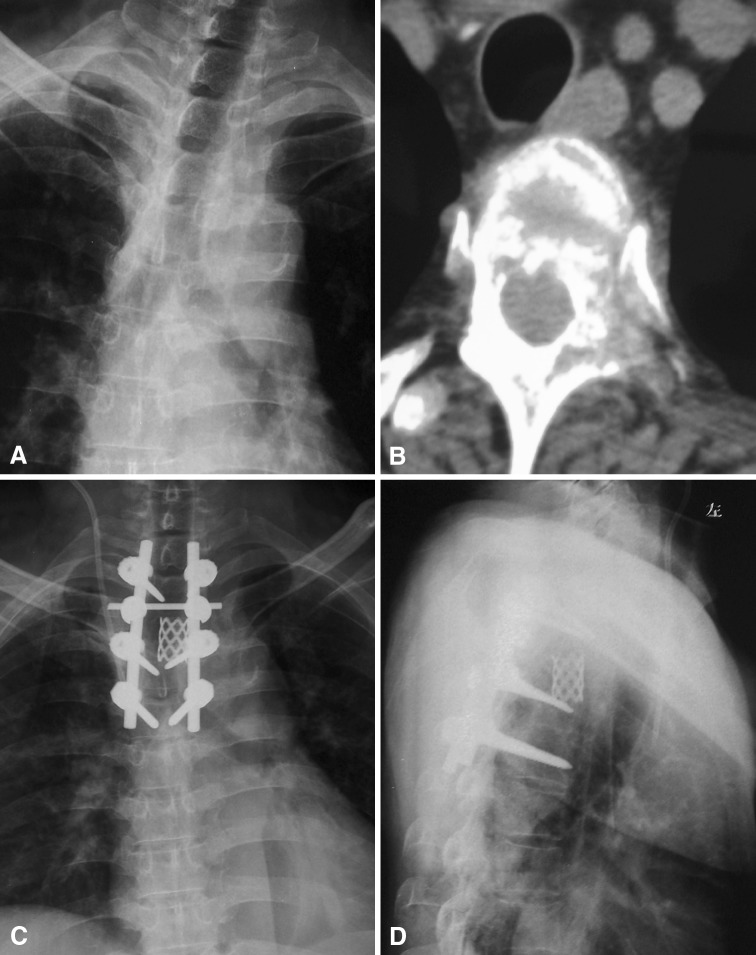
Fig. 3A–D.
A 61-year-old woman previously diagnosed with lung cancer had intractable neck pain, numbness, and weakness in the lower limbs with difficulty walking. Posterior decompression surgery with C3 tumor curettage, C2 pedicle screw fixation, C4–5 lateral mass screw fixation, and autograft fusion were performed. Pain relief and neurologic function were achieved at the 16-month postoperative followup, and the patient is still alive and ambulatory with a crutch. (A) The patient’s preoperative radiograph shows a destroyed C3 vertebra, and (B) her transverse CT scan shows an invasive mass that has destroyed the vertebra and invaded the paravertebral tissue and spinal canal, resulting in spinal cord compression. Postoperative (C) AP and (D) lateral view radiographs show stable fixation.
Fig. 4A–D.
A 65-year-old man previously diagnosed with prostate cancer had severe chest and back pain and weakness in both lower extremities. His radiograph and CT results revealed the T3 vertebra had been destroyed by an invasive mass and the spinal cord was compressed. Posterior total en bloc resection of the T3 tumor, bone graft fusion with titanium mesh, and pedicle screw fixation were performed. His pain was relieved and neurologic function was improved postoperatively. The patient was still alive at 41 months after the surgery with no recurrence. (A) A preoperative radiograph shows a destroyed T3 vertebra and vertebral pedicles, and (B) his transverse CT scan shows an invasive mass that has destroyed the vertebra and invaded the paravertebral tissue and spinal canal, resulting in spinal cord compression. (C) AP and (D) lateral view postoperative radiographs show stable fixation.
Table 7.
Survival predictive accuracy of Tokuhashi scores (n = 92)
| Original Tokuhashi score | Actual survival median (months) | Range (months) | Accuracy (%) | Number of patients |
|---|---|---|---|---|
| Group 1 (1–4) | ||||
| Predicted survival < 3 months | 1.6 | 1.0–3.3 | 78% | 9 |
| Group 2 (5–8) | ||||
| Predicted survival > 3 months | 10 | 0.2–78 | 41% | 34 |
| Group 3 (9–12) | ||||
| Predicted survival > 6 months | 13 | 0.7–72 | 82% | 49 |
Discussion
Because of lack of clinical reports with large sample sizes, the incidence of fatal complications and surgical outcomes in patients (≥ 60 years) with spinal metastases is uncertain. Survival prognosis is one of the most important considerations in the decision to perform surgery and in determining the extent of surgery in patients with spinal metastases. However, it is unclear which possible risk factors are reliable to predict survival. We therefore posed three questions: (1) What surgical risk occurs in patients (≥ 60 years) with spinal metastasis, especially surgery-related complications? (2) Does tumor removal with reconstruction improve the clinical status? (3) Which possible risk factors are reliable to predict survival after surgical interventions in patients affected by spine metastases?
We recognize some limitations in our study. First, the data for this study came from one clinical center, and the sample size was not large enough to draw definitive conclusions. Neoadjuvant and adjuvant radiotherapy and chemotherapy data were not included in our analysis, although these factors may substantially influence survival rates. This omission may overestimate the effect of surgical treatment on clinical function and survival. However, we believe that this effect was relatively low, since radiotherapy and chemotherapy reportedly do not influence survival in patients with spinal metastases [3, 17]. Second, because the surgeries were performed by different orthopaedic oncologists during a long interval, surgery and reconstruction methods were selected differently. For this reason, stratified analysis was not performed. Third, we excluded 23 patients with incomplete information. However, since these patients had similar distributions of primary tumor, sex, and age, we assumed these data would not substantially affect the results.
We observed major surgical complications in 21 patients, giving a 23% complication rate and a 3.4% 30-day in-hospital mortality rate. Other series have reported 30-day in-hospital mortality rates ranging from 3% to 13% [2, 3, 13, 18, 22, 23, 26, 37, 40, 42, 45, 46, 51, 60] (Table 8). Previous studies have reported major surgical complication rates of 14% to 34% [2, 3, 13, 18, 22, 23, 26, 37, 40, 42, 45, 46, 51, 57, 60] (Table 8). Systemic infections such as pulmonary infection and cardiovascular failure are more common in patients 60 years old or older than in other patients with spinal metastasis [1, 35]. In our study, the 29 patients who were 70 years or older had a systemic infection rate of 10% and a cardiovascular disease rate of 10%, whereas the patients younger than 70 years had a systemic infection rate of 3.1% and a cardiovascular disease rate of 3.1%. In a recent study of perioperative complications and prognosis in older patients (≥ 70 years) undergoing surgery for spinal metastases, pulmonary complications were observed in 19% of the patients, cardiovascular complications were observed in 9%, and delirium in 13%. In the younger patients, pulmonary complications occurred in only 2.5%, cardiovascular complications occurred in 0.6%, and delirium in 1.2% [35]. These findings should be considered carefully when deciding to pursue surgical treatment, especially in elderly patients.
Table 8.
Comparison of data from the literature
| Study | Patients (number) | Major surgical complication rate | Mean age of patients (years) | 30-day mortality rates | Neurologic function improvement rate | Median survival (months) | Prognostic factors | Minimal followup (months) |
|---|---|---|---|---|---|---|---|---|
| Wise et al. [60] | 80 | 13.8% | 56 | 5.7% | 97% | 15.7 | NR | 5 |
| Weigel et al. [57] | 76 | 19% | 59 | 2.6% | 58% | 13.1 | NR | 6 |
| Tomita et al. [52] | 67 | NR | 56 | NR | 74% | NR | Primary tumors; visceral metastases; bone metastases | NR |
| Finkelstein et al. [13] | 987 | 27% | 60 | 9% | NR | 7.6 | Increasing age; male sex; primary tumors | NR |
| North et al. [37] | 61 | 8.2% | 52 | 3.3% | 88% | 10 | Primary tumors; preoperative neurologic status | |
| Jansson & Bauer [26] | 282 | 20% | 66 | 13% | 70% | 6 | NR | 3 |
| Leithner et al. [31] | 69 | NR | 60 | NR | NR | 10 | Primary tumor; visceral metastases | 12 |
| Chaichana et al. [8] | 114 | 17% | 58 | 3% | NR | 7 | NR | 10.8* |
| Wibmer et al. [59] | 62 | NR | 60 | NR | NR | 10.6 | Systemic therapy; primary tumors; visceral metastases | 12 |
| Arrigo et al. [3] | 200 | 34% | 59 | 3% | NR | 8.0 | Charlson comorbidity index; preoperative ambulatory status; primary tumors | NR |
| Current study | 92 | 22.8% | 68 | 3.4% | 78% | 15 | Primary tumors; Tokuhashi score | 6 |
* Mean followup; NR = not reported.
We found pain levels decreased after surgery in 81 of the 92 patients for a pain relief rate of 88%, which is similar to reductions in pain in 89% to 100% of patients reported in the literature [6, 25, 57]. These findings all suggest surgery can substantially relieve pain, which is consistent with other reports [2, 3, 12, 16, 36, 41, 49, 51, 52, 58]. In our study, neurologic dysfunction was improved after surgery in 78% of these patients (Table 8). The improvement in overall neurologic function therefore was substantial, which is consistent with findings from other studies [25, 43, 57]. In our study, the Karnofsky score increased dramatically, and this result was largely consistent with the findings of previous studies [28, 49–51, 55, 59]. Therefore, restoring general health through partially or totally removing the tumor was relatively straightforward.
The median postsurgical survival of the 92 patients in our study was 15 months. This result compares favorably with those from other studies of surgically treated spinal metastases in which the median postoperative patient survival ranges from 6 to 16 months [8, 13, 22, 31, 33, 37, 51, 53] (Table 8). The relatively long survival times of the patients in our study may be related to the more conservative surgical selection criteria we used; some of the patients presenting to our department with severe metastases received percutaneous vertebroplasty and kyphoplasty and were excluded from our study. The survival analysis in our study revealed that the primary tumor type and Tokuhashi score were independent factors associated with survival. The univariate and multivariate analyses in our study revealed the pathological type of the primary tumor was a substantial predictor of survival, which is consistent with multiple reports [13, 22, 31, 33, 37, 48, 51, 52]. We found slow-growing primary tumors were associated with more favorable prognoses, whereas fast-growing tumors were linked to poorer prognoses, which is consistent with other studies [4, 24, 31, 48, 60]. Tomita et al. [52] and Tokuhashi et al. [49–51] regard the primary tumor type as the most important predictive factor in their respective scoring systems. Several prognostic scoring systems have been developed to facilitate selecting candidates for surgical treatment and determining the extent of surgery to be performed [30, 44, 50–52, 55]. We investigated the predictive value of three commonly used prognostic scoring systems: the Tomita score, the Tokuhashi score, and the re-Tokuhashi score [50–52, 54]. We found all of these scores were substantially associated with postoperative survival in the univariate analysis, but only the Tokuhashi score was independently associated with survival. Moreover, we further investigated the accuracy of the Tokuhashi score for predicting patient survival. We found Groups 1 to 4 and 9 to 12 of the Tokuhashi score predicted survival time in 78% and 82% of the patients, respectively, whereas Groups 5 to 8 were accurate in only 41% of the patients. This finding emphasizes the difficulty of accurately predicting individual survival, particularly of predicting which patients will survive for 3 to 6 months, although the Tokuhashi score was substantially correlated with survival time in the univariate and multivariate analyses. For this reason, we do not recommend using only the prognostic score to choose surgical treatment. Rather, our treatment algorithm considers pain, spinal cord compression, neurologic compromise, potential postoperative complications, and primary tumor type.
Our observations suggest surgery for spinal metastasis in patients older than 60 years can achieve pain relief, neurologic improvement, and restoration of general condition but with a high risk of complications. Primary tumor type and Tokuhashi scoring predicted survival in patients with spinal metastases after surgery. We recommend considering aggressive surgery for primary tumors with histopathologic features indicating slow growth. Despite limitations, our study provides insight into surgically treating patients with spinal metastases, a subject that has not received much attention from previous researchers.
Acknowledgments
We thank Wenling Gao PhD, Prince Philip Dental Hospital, University of Hong Kong, and Shengxue Wei PhD, Department of Statistics, Sun Yat-sen University, for statistical advice and for performing statistical analyses.
Appendix 1. Different Scoring Systems Used in our Study
Tomita Score [52]
According to the grade of malignancy, primary pathological tumor types are divided into three categories:
Grade 1, slow growth (breast, multiple myeloma, prostate, metastasizing hemangioendothelioma, hemangiopericytoma, thyroid, non-Hodgkin lymphoma).
Grade 2, moderate growth (kidney, uterus, tonsil, epipharynx, femoral synovial sarcoma, malignant thymoma).
Grade 3, rapid growth (lung, melanoma, malignant teratoma, liver, stomach, colon, sigma, rectum, pancreas).
Tomita scoring system for spinal metastases that was designed based on these data consists of three prognostic factors: (1) grade of malignancy (slow growth,1 point; moderate growth, 2 points; rapid growth, 4 points), (2) visceral metastases (no metastasis, 0 points; treatable, 2 points: untreatable, 4 points), and (3) bone metastases (solitary or isolated, 1 point; multiple, 2 points). These three factors were added together to give a prognostic score between 2 and 10.
Tokuhashi Scores [50, 51]
Tokuhashi scores (original and revised) include six parameters with 0 to 2 points (0 to 5 in the revised version), resulting in three prognostic groups.
The Revised Tokuhashi Score [50]
This score has the following parameters:
- General condition (Karnofsky)
- 0 points: poor (10%–40%)
- 1 point: moderate (50%–70%)
- 2 points: good (80%–100%)
Number of extraspinal bone metastases foci: 0 points: ≥ 3; 1 point: 1–2; 2 points: 1.
Number of metastases in the vertebral body: 0 points: ≥ 3; 1 point: 1–2; 2 points: 1.
Metastases to the major internal organs: 0 points: unremovable; 1 point: removable; 2 points: no metastases.
- Primary site of the cancer:
- 0 points: lung, osteosarcoma, stomach, bladder, esophagus, pancreas
- 1 point: liver, gallbladder, unidentified
- 2 points: others
- 3 points: kidney, uterus
- 4 points: rectum
- 5 points: thyroid, breast, prostate, carcinoid tumor)
Palsy: 0 points: complete (Frankel A, B); 1 point: incomplete (Frankel C, D); 2 points: none (Frankel E).
Survival prognosis: total score 0–8: lives < 6 months; total score 9–11: lives > 6 months; total score 12–15: lives > 1 year.
The Original Tokuhashi Score [51]
This is mostly the same as the revised version. Only the factor “primary site of the cancer” is different as it includes three ranks from 0–2 points:
0 points: lung, gastrointestinal tract, and other unknown reasons;
1 point: liver, kidney, uterus;
2 points: thyroid, rectum, breast, prostate, bone marrow.
Survival prognosis: total score 0–4: lives < 3 months; total score 5–8: lives > 3 months (and 30% > 1 year); total score 9–12: lives > 1 year.
Frankel Grade [14]
Complete neurological injury. No motor or sensory function detected below level of lesion.
Preserved sensation only. No motor function detected below level of lesion, some sensory function below level of lesion preserved.
Preserved motor, nonfunctional. Some voluntary motor function preserved below level of lesion but too weak to serve any useful purpose, sensation may or may not be preserved.
Preserved motor, functional. Functionally useful voluntary motor function below level of injury is preserved.
Normal motor function. Normal motor and sensory function below level of lesion, abnormal reflexes may persist.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
References
- 1.Aebi M. Spinal metastasis in the elderly. Eur Spine J. 2003;12(suppl 2):S202–S213. doi: 10.1007/s00586-003-0609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arrigo RT, Kalanithi P, Cheng I, Alamin T, Carragee EJ, Mindea SA, Boakye M, Park J. Charlson score is a robust predictor of 30-day complications following spinal metastasis surgery. Spine (Phila Pa 1976). 2011;36:E1274–E1280. doi: 10.1097/BRS.0b013e318206cda3. [DOI] [PubMed] [Google Scholar]
- 3.Arrigo RT, Kalanithi P, Cheng I, Alamin T, Carragee EJ, Mindea SA, Park J, Boakye M. Predictors of survival after surgical treatment of spinal metastasis. Neurosurgery. 2011;68:674–681. doi: 10.1227/NEU.0b013e318207780c. [DOI] [PubMed] [Google Scholar]
- 4.Bartels RH, Feuth T, van der Maazen R, Verbeek AL, Kappelle AC, Andre Grotenhuis J, Leer JW. Development of a model with which to predict the life expectancy of patients with spinal epidural metastasis. Cancer. 2007;110:2042–2049. doi: 10.1002/cncr.23002. [DOI] [PubMed] [Google Scholar]
- 5.Bauer HC, Wedin R. Survival after surgery for spinal and extremity metastases: prognostication in 241 patients. Acta Orthop Scand. 1995;66:143–146. doi: 10.3109/17453679508995508. [DOI] [PubMed] [Google Scholar]
- 6.Cahill DW, Kumar R. Palliative subtotal vertebrectomy with anterior and posterior reconstruction via a single posterior approach. J Neurosurg. 1999;90(1 suppl):42–47. doi: 10.3171/spi.1999.90.1.0042. [DOI] [PubMed] [Google Scholar]
- 7.Carlsson AM. Assessment of chronic pain: I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- 8.Chaichana KL, Pendleton C, Sciubba DM, Wolinsky JP, Gokaslan ZL. Outcome following decompressive surgery for different histological types of metastatic tumors causing epidural spinal cord compression: clinical article. J Neurosurg Spine. 2009;11:56–63. doi: 10.3171/2009.1.SPINE08657. [DOI] [PubMed] [Google Scholar]
- 9.Choi D, Crockard A, Bunger C, Harms J, Kawahara N, Mazel C, Melcher R, Tomita K. Review of metastatic spine tumour classification and indications for surgery: the consensus statement of the Global Spine Tumour Study Group. Eur Spine J. 2010;19:215–222. doi: 10.1007/s00586-009-1252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cox DR. Regression models and life-tables. J Royal Statistical Soc Series B (Methodological). 1972;34:187–220. [Google Scholar]
- 11.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Enkaoua EA, Doursounian L, Chatellier G, Mabesoone F, Aimard T, Saillant G. Vertebral metastases: a critical appreciation of the preoperative prognostic Tokuhashi score in a series of 71 cases. Spine (Phila Pa 1976). 1997;22:2293–2298. doi: 10.1097/00007632-199710010-00020. [DOI] [PubMed] [Google Scholar]
- 13.Finkelstein JA, Zaveri G, Wai E, Vidmar M, Kreder H, Chow E. A population-based study of surgery for spinal metastases: survival rates and complications. J Bone Joint Surg Br. 2003;85:1045–1050. doi: 10.1302/0301-620X.85B7.14201. [DOI] [PubMed] [Google Scholar]
- 14.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 15.Fujimaki Y, Tsuchiya H, Kawahara N, Tanzawa Y, Tomita K. [Surgical treatment for metastatic bone tumor][in Japanese] Clin Calcium. 2006;16:647–654. [PubMed] [Google Scholar]
- 16.Fukuhara A, Masago K, Neo M, Fujibayashi S, Fujita S, Hatachi Y, Irisa K, Sakamori Y, Togashi Y, Kim YH, Mio T, Mishima M. Outcome of surgical treatment for metastatic vertebra bone tumor in advanced lung cancer. Case Rep Oncol. 2010;3:63–71. doi: 10.1159/000299385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghogawala Z, Mansfield FL, Borges LF. Spinal radiation before surgical decompression adversely affects outcomes of surgery for symptomatic metastatic spinal cord compression. Spine (Phila Pa 1976). 2001;26:818–824. doi: 10.1097/00007632-200104010-00025. [DOI] [PubMed] [Google Scholar]
- 18.Gokaslan ZL, York JE, Walsh GL, McCutcheon IE, Lang FF, Putnam JB, Jr, Wildrick DM, Swisher SG, Abi-Said D, Sawaya R. Transthoracic vertebrectomy for metastatic spinal tumors. J Neurosurg. 1998;89:599–609. doi: 10.3171/jns.1998.89.4.0599. [DOI] [PubMed] [Google Scholar]
- 19.Greenlee RT, Murray T, Bolden S, Wingo PA. Cancer statistics, 2000. CA Cancer J Clin. 2000;50:7–33. doi: 10.3322/canjclin.50.1.7. [DOI] [PubMed] [Google Scholar]
- 20.Groot MT, Boeken Kruger CG, Pelger RC, Uyl-de Groot CA. Costs of prostate cancer, metastatic to the bone, in the Netherlands. Eur Urol. 2003;43:226–232. doi: 10.1016/S0302-2838(03)00007-1. [DOI] [PubMed] [Google Scholar]
- 21.Harrington KD. Orthopedic surgical management of skeletal complications of malignancy. Cancer. 1997;80(8 suppl):1614–1627. doi: 10.1002/(SICI)1097-0142(19971015)80:8+<1614::AID-CNCR12>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 22.Hirabayashi H, Ebara S, Kinoshita T, Yuzawa Y, Nakamura I, Takahashi J, Kamimura M, Ohtsuka K, Takaoka K. Clinical outcome and survival after palliative surgery for spinal metastases: palliative surgery in spinal metastases. Cancer. 2003;97:476–484. doi: 10.1002/cncr.11039. [DOI] [PubMed] [Google Scholar]
- 23.Holman PJ, Suki D, McCutcheon I, Wolinsky JP, Rhines LD, Gokaslan ZL. Surgical management of metastatic disease of the lumbar spine: experience with 139 patients. J Neurosurg Spine. 2005;2:550–563. doi: 10.3171/spi.2005.2.5.0550. [DOI] [PubMed] [Google Scholar]
- 24.Hosono N, Ueda T, Tamura D, Aoki Y, Yoshikawa H. Prognostic relevance of clinical symptoms in patients with spinal metastases. Clin Orthop Relat Res. 2005;436:196–201. doi: 10.1097/01.blo.0000160003.70673.2a. [DOI] [PubMed] [Google Scholar]
- 25.Hussein AA, El-Karef E, Hafez M. Reconstructive surgery in spinal tumours. Eur J Surg Oncol. 2001;27:196–199. doi: 10.1053/ejso.2000.1079. [DOI] [PubMed] [Google Scholar]
- 26.Jansson KA, Bauer HC. Survival, complications and outcome in 282 patients operated for neurological deficit due to thoracic or lumbar spinal metastases. Eur Spine J. 2006;15:196–202. doi: 10.1007/s00586-004-0870-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 28.Karnofsky DA. Problems and pitfalls in the evaluation of anticancer drugs. Cancer. 1965;18:1517–1528. doi: 10.1002/1097-0142(196512)18:12<1517::AID-CNCR2820181202>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 29.Katagiri H, Takahashi M, Inagaki J, Kobayashi H, Sugiura H, Yamamura S, Iwata H. Clinical results of nonsurgical treatment for spinal metastases. Int J Radiat Oncol Biol Phys. 1998;42:1127–1132. doi: 10.1016/S0360-3016(98)00288-0. [DOI] [PubMed] [Google Scholar]
- 30.Katagiri H, Takahashi M, Wakai K, Sugiura H, Kataoka T, Nakanishi K. Prognostic factors and a scoring system for patients with skeletal metastasis. J Bone Joint Surg Br. 2005;87:698–703. doi: 10.1302/0301-620X.87B5.15185. [DOI] [PubMed] [Google Scholar]
- 31.Leithner A, Radl R, Gruber G, Hochegger M, Leithner K, Welkerling H, Rehak P, Windhager R. Predictive value of seven preoperative prognostic scoring systems for spinal metastases. Eur Spine J. 2008;17:1488–1495. doi: 10.1007/s00586-008-0763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lemke DM, Hacein-Bey L. Metastatic compression fractures: vertebroplasty for pain control. J Neurosci Nurs. 2003;35:50–55. doi: 10.1097/01376517-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976). 2001;26:1631–1638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 34.Manabe J, Kawaguchi N, Matsumoto S, Tanizawa T. Surgical treatment of bone metastasis: indications and outcomes. Int J Clin Oncol. 2005;10:103–111. doi: 10.1007/s10147-005-0478-9. [DOI] [PubMed] [Google Scholar]
- 35.Murakami H, Kawahara N, Demura S, Kato S, Yoshioka K, Sasagawa T, Tomita K. Perioperative complications and prognosis for elderly patients with spinal metastases treated by surgical strategy. Orthopedics. 2010;Mar 10:165–168. doi: 10.3928/01477447-20100129-10. [DOI] [PubMed] [Google Scholar]
- 36.Murakami H, Kawahara N, Demura S, Kato S, Yoshioka K, Tomita K. Total en bloc spondylectomy for lung cancer metastasis to the spine. J Neurosurg Spine. 2010;13:414–417. doi: 10.3171/2010.4.SPINE09365. [DOI] [PubMed] [Google Scholar]
- 37.North RB, LaRocca VR, Schwartz J, North CA, Zahurak M, Davis RF, McAfee PC. Surgical management of spinal metastases: analysis of prognostic factors during a 10-year experience. J Neurosurg Spine. 2005;2:564–573. doi: 10.3171/spi.2005.2.5.0564. [DOI] [PubMed] [Google Scholar]
- 38.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin. 1999;49:33–64. doi: 10.3322/canjclin.49.1.33. [DOI] [PubMed] [Google Scholar]
- 39.Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, Mohiuddin M, Young B. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366:643–648. doi: 10.1016/S0140-6736(05)66954-1. [DOI] [PubMed] [Google Scholar]
- 40.Patil CG, Lad SP, Santarelli J, Boakye M. National inpatient complications and outcomes after surgery for spinal metastasis from 1993–2002. Cancer. 2007;110:625–630. doi: 10.1002/cncr.22819. [DOI] [PubMed] [Google Scholar]
- 41.Pointillart V, Vital JM, Salmi R, Diallo A, Quan GM. Survival prognostic factors and clinical outcomes in patients with spinal metastases. J Cancer Res Clin Oncol. 2011;137:849–856. doi: 10.1007/s00432-010-0946-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shehadi JA, Sciubba DM, Suk I, Suki D, Maldaun MV, McCutcheon IE, Nader R, Theriault R, Rhines LD, Gokaslan ZL. Surgical treatment strategies and outcome in patients with breast cancer metastatic to the spine: a review of 87 patients. Eur Spine J. 2007;16:1179–1192. doi: 10.1007/s00586-007-0357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siegal T, Siegal T. Current considerations in the management of neoplastic spinal cord compression. Spine (Phila Pa 1976). 1989;14:223–228. doi: 10.1097/00007632-198902000-00015. [DOI] [PubMed] [Google Scholar]
- 44.Simmons ED, Zheng Y. Vertebral tumors: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:233–247. doi: 10.1097/01.blo.0000198723.77762.0c. [DOI] [PubMed] [Google Scholar]
- 45.Sundaresan N, Digiacinto GV, Hughes JE, Cafferty M, Vallejo A. Treatment of neoplastic spinal cord compression: results of a prospective study. Neurosurgery. 1991;29:645–650. doi: 10.1227/00006123-199111000-00001. [DOI] [PubMed] [Google Scholar]
- 46.Sundaresan N, Rothman A, Manhart K, Kelliher K. Surgery for solitary metastases of the spine: rationale and results of treatment. Spine (Phila Pa 1976). 2002;27:1802–1806. doi: 10.1097/00007632-200208150-00021. [DOI] [PubMed] [Google Scholar]
- 47.Szpalski M, Gunzburg R, Melot C, Aebi M. The aging of the population: a growing concern for spine care in the twenty-first century. Eur Spine J. 2003;12(suppl 2):S81–S83. doi: 10.1007/s00586-003-0592-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tatsui H, Onomura T, Morishita S, Oketa M, Inoue T. Survival rates of patients with metastatic spinal cancer after scintigraphic detection of abnormal radioactive accumulation. Spine (Phila Pa 1976). 1996;21:2143–2148. doi: 10.1097/00007632-199609150-00017. [DOI] [PubMed] [Google Scholar]
- 49.Tokuhashi Y, Ajiro Y, Umezawa N. Outcome of treatment for spinal metastases using scoring system for preoperative evaluation of prognosis. Spine (Phila Pa 1976). 2009;34:69–73. doi: 10.1097/BRS.0b013e3181913f19. [DOI] [PubMed] [Google Scholar]
- 50.Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 2005;30:2186–2191. doi: 10.1097/01.brs.0000180401.06919.a5. [DOI] [PubMed] [Google Scholar]
- 51.Tokuhashi Y, Matsuzaki H, Toriyama S, Kawano H, Ohsaka S. Scoring system for the preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 1990;15:1110–1113. doi: 10.1097/00007632-199011010-00005. [DOI] [PubMed] [Google Scholar]
- 52.Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001;26:298–306. doi: 10.1097/00007632-200102010-00016. [DOI] [PubMed] [Google Scholar]
- 53.Ulmar B, Huch K, Naumann U, Catalkaya S, Cakir B, Gerstner S, Reichel H. Evaluation of the Tokuhashi prognosis score and its modifications in 217 patients with vertebral metastases. Eur J Surg Oncol. 2007;33:914–919. doi: 10.1016/j.ejso.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 54.Ulmar B, Richter M, Cakir B, Muche R, Puhl W, Huch K. The Tokuhashi score: significant predictive value for the life expectancy of patients with breast cancer with spinal metastases. Spine (Phila Pa 1976). 2005;30:2222–2226. doi: 10.1097/01.brs.0000181055.10977.5b. [DOI] [PubMed] [Google Scholar]
- 55.van der Linden YM, Dijkstra SP, Vonk EJ, Marijnen CA, Dutch Bone Metastasis Study Group Prediction of survival in patients with metastases in the spinal column: results based on a randomized trial of radiotherapy. Cancer. 2005;103:320–328. doi: 10.1002/cncr.20756. [DOI] [PubMed] [Google Scholar]
- 56.Walsh GL, Gokaslan ZL, McCutcheon IE, Mineo MT, Yasko AW, Swisher SG, Schrump DS, Nesbitt JC, Putnam JB, Jr, Roth JA. Anterior approaches to the thoracic spine in patients with cancer: indications and results. Ann Thorac Surg. 1997;64:1611–1618. doi: 10.1016/S0003-4975(97)01034-5. [DOI] [PubMed] [Google Scholar]
- 57.Weigel B, Maghsudi M, Neumann C, Kretschmer R, Muller FJ, Nerlich M. Surgical management of symptomatic spinal metastases: postoperative outcome and quality of life. Spine (Phila Pa 1976). 1999;24:2240–2246. doi: 10.1097/00007632-199911010-00012. [DOI] [PubMed] [Google Scholar]
- 58.Whitmore RG, Stephen J, Stein SC, Campbell PG, Yadla S, Harrop JS, Sharan AD, Maltenfort MG, Ratliff JK. Patient comorbidities and complications after spinal surgery: a societal-based cost analysis. Spine (Phila Pa 1976). 2012;37:1065–1071. doi: 10.1097/BRS.0b013e31823da22d. [DOI] [PubMed] [Google Scholar]
- 59.Wibmer C, Leithner A, Hofmann G, Clar H, Kapitan M, Berghold A, Windhager R. Survival analysis of 254 patients after manifestation of spinal metastases: evaluation of seven preoperative scoring systems. Spine (Phila Pa 1976). 2011;36:1977–1986. doi: 10.1097/BRS.0b013e3182011f84. [DOI] [PubMed] [Google Scholar]
- 60.Wise JJ, Fischgrund JS, Herkowitz HN, Montgomery D, Kurz LT. Complication, survival rates, and risk factors of surgery for metastatic disease of the spine. Spine (Phila Pa 1976). 1999;24:1943–1951. doi: 10.1097/00007632-199909150-00014. [DOI] [PubMed] [Google Scholar]