History
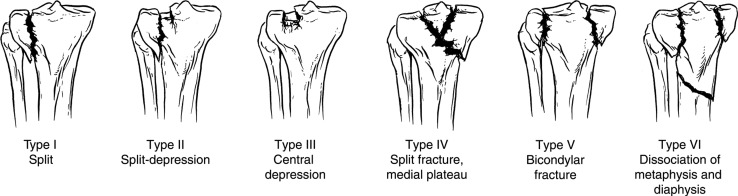
Early attempts at classifying tibial plateau fractures by Palmer in 1951 [25], Hohl and Luck in 1956 [15], and Hohl in 1967 [15] recognized some of the major themes common to many classification systems for these fractures: split of a condyle, subchondral depression, and comminuted bicondylar involvement. Schatzker et al. published their classification system in 1979 [29], deriving it from the AP radiographs of a series of 94 patients, most of whose tibial plateau fractures were treated nonoperatively [34]. They divided tibial plateau fractures into six types (Fig. 1): split fracture of the lateral tibial plateau (Type I), split depression of the lateral tibial plateau (Type II), central depression of the lateral plateau (Type III), split of the medial tibial plateau (Type IV), bicondylar tibial plateau fracture (Type V), and dissociation between the metaphysis and diaphysis (Type VI; also known as a Type C articular fracture in the AO/OTA classification). The first types involve only the lateral tibial plateau. Type III (depression) fractures were caused by low-energy injuries in osteopenic bone whereas all other types resulted from high-energy injuries [29]. Types IV to VI often result from motor vehicle collisions, motorcycle collisions, and falls from a height [1]. Finally, although the first four types are unicondylar fractures, Types V and VI are bicondylar.
Fig. 1.
The Schatzker classification system of tibial plateau fractures is shown. (Reprinted and published with permission from Berkson EM, Virkus WW. High-energy tibial plateau fractures. J Am Acad Orthop Surg. 2006;14:20–31.)
Schatzker et al. emphasized that their classification system, hereafter referred to as the Schatzker system, was based on fracture pattern. Also, each fracture’s pattern, as they classified, helped to direct the appropriate operative treatment modality, such as lag screws, buttress plates, or both (as sometimes is done for bicondylar fractures), and to point to the need for elevation of the depressed joint surface and maintenance with bone graft (for depressed fractures). They noted that operatively treated fractures had better results than those treated nonoperatively and that osteoporotic bone fared worse in patients treated operatively and nonoperatively [29].
Purpose
Tibial plateau fractures are relatively uncommon, representing approximately 1.2% of all fractures [10]. These fractures are seen predominantly in two groups: as higher-energy injuries in younger people and as lower-energy fractures in elderly patients secondary to osteopenia [10]. In the former population, in particular, these injuries are associated with an increased incidence of complications including nonunion, infection, loss of motion, and posttraumatic arthritis [26]. Classifying these injuries is important to guide treatment, categorize research into clinical interventions, describe prognosis, and facilitate communication regarding all patients with these injuries.
Tibial plateau fractures present across the full spectrum, from nondisplaced closed injuries that heal readily with protected weightbearing through complex fracture patterns that extend into the diaphysis and are associated with important soft tissue or neurovascular injuries that can threaten the limb [1, 4, 10, 11]. As with other intraarticular fractures, the goals of treatment of tibial plateau fractures include achieving a stable knee, restoring the joint surface, and preserving functional ROM. Although other classification systems have been described [15–17, 19, 25], two are in most common use: the AO/OTA and Schatzker systems [11]. Of those, the rubric used by the Schatzker system is perhaps the more popular and easily recognized, in large part because of its simplicity.
By classifying a tibial plateau fracture using this system, orthopaedic surgeons communicate information regarding the level of energy of the fracture (high versus low), the potential need for extensile or dual incisions to address fractures involving both condyles or those with significant posterior involvement, and the possibility of associated soft tissue injury (split-depression fractures are associated with lateral meniscal and medial collateral ligament (MCL) injuries [13]). Schatzker Types II and IV fractures have been associated with the highest frequency of soft tissue injury, including lateral meniscal and MCL injuries [4]. Eighteen percent of patients with Type VI fractures had compartment syndrome in a study by Stark et al. [30]. Type IV or medial plateau fractures often are thought to represent transient knee dislocation events; as such, these require careful neurovascular examination, including ankle-brachial indices and a thorough neurologic examination at a minimum.
Validation
A classification system’s reliability can be evaluated by measuring its interobserver and intraobserver agreement. The Schatzker system was designed to classify fracture patterns seen on plain radiographs, but when plain radiographs are used alone, interobserver kappa values have varied widely, from 0.38 to 0.68 [6, 8, 9, 21, 31, 34, 36]. Similarly, kappa values for intraobserver reliability have ranged from 0.57 to 0.91 [6, 8, 9, 21, 31, 34].
Since CT has become commonplace for preoperative planning, many studies have measured the effect of including CT on interobserver and intraobserver reliability [6, 8, 12, 13, 31]. Although this has not been systematically reviewed, authors generally have higher kappa coefficients when CT is used in addition to plain radiographs [6, 18, 36]. The addition of two-dimensional (2-D) CT has yielded interobserver kappa values ranging from 0.46 to 0.75 [6, 8, 12, 13, 31]. Including three-dimensional (3-D) reconstructions of CT images reportedly improves interobserver reliability to between 0.596 and 0.85 [12, 18]. The addition of MRI has yielded interobserver reliability at 0.85 in one study whose authors recommend routine preoperative MRI instead of CT of tibial plateau fractures for preoperative planning [36]; to our knowledge, this finding has not been confirmed by others. The broad range of kappa values for interobserver agreement among various studies likely results from differences in study design, in particular, the level of experience of the various observers chosen. Like interobserver agreement, intraobserver agreement has varied. Some of this variation depends on the imaging used; for example, when CT images are added to plain radiographs, the intraobserver reliability is generally good to excellent, ranging from 0.57 to 0.89 [6, 8, 12, 18, 31].
The other commonly used classification system for these fractures is the AO/OTA system. Neither has been proven superior to the other. Walton et al. [34] found the AO/OTA classification system to be more reliable among observers than the Schatzker system, but Maripuri et al. [21] concluded that the Schatzker system had higher interobserver reliability than other classification systems including the AO/OTA system. Although the interobserver reliability of the Schatzker system can be improved by adding 2-D CT [6, 36], 3-D CT [18], or MRI [36] to plain radiographs, authors have not recommended consistently that advanced imaging is advantageous for purposes of classification. For example, some authors have concluded that the added value of 3-D CT is limited [12], that CT should not be obtained routinely [31], and that CT should be obtained for preoperative planning rather than improvement in classification [8], although they note that classification, in this sense, is intended to guide treatment and, therefore, may be appropriate.
Limitations
Investigators have commented on numerous shortcomings of the Schatzker system. Because it was designed for classification based on AP radiographs, the system does not include injury patterns with major fracture lines in the coronal plane or those simply not visible on plain radiographs. Posteromedial fragments are seen in 59% to 74% of bicondylar fractures [3, 14]; these are important, because they affect the surgical plan in terms of patient positioning, surgical approach, and incision placement [1, 2, 5, 20, 27, 35]. To address this limitation, Luo et al. [20] developed a “three-column” model based on axial (CT) imaging to classify tibial plateau fractures as having medial, lateral, and posterior column involvement. This system identifies posterior fractures needing posterior fixation. Although such fractures are typical of Types V and VI of the Schatzker system, the Schatzker system is not able to indicate if a posterior approach would be necessary [20].
Type IV fractures, or medial plateau fractures, were further classified by Wahlquist et al. [33] by categorizing fractures by their articular exit point relative to the tibial spine, because considering the injuries in this way may help predict the presence of an important soft tissue component to these injuries that is not captured by using the Schatzker system alone. In particular, Wahlquist et al. found that the incidence of compartment syndrome was 14% for Type A, 33% for Type B, and 67% for Type C, where Types A, B, and C are medial to, at, and lateral to the level of the tibial spine, respectively. Some rare fracture types are unclassifiable, such as a horizontal shear of the entire plateau reported by Mohanlal and Nathan [23]. Recognizing that treatment of high-energy, comminuted bicondylar plateau fractures represents a particular challenge, in 1992, Honkonen and Järvinen expanded the Schatzker classification by subclassifying Type VI (bicondylar) fractures into those with lateral (valgus) tilt and medial (varus) tilt [17]. In 2000, Khan et al. introduced a topographic and morphologic classification system that introduced a new fracture type: subcondylar, bicondylar with coronal split [19].
The condition of the soft tissue envelope is another important consideration in preoperative planning, treatment, and prognosis for fractures of the tibial plateau, and, obviously, this important clinical element lies outside the scope of the rubric of the Schatzker system. Some argue that fracture classification should indicate the severity of the associated soft tissue injuries including the collateral and cruciate ligaments, menisci, and neurovascular structures [7, 32], although most classification schemes do not include these elements.
Fracture-dislocation injuries of the knee can be distinguished from tibial plateau fractures [24], but certain plateau fracture patterns, namely posterior, posteromedial, and medial plateau shear-type fractures, may represent a transient dislocation event and warrant appropriate workup including neurologic and vascular assessments. These, too, lie outside the scope of the Schatzker system.
Conclusions
Classifying tibial plateau fractures is important for physician-to-physician communication (for clinical and research purposes), for estimation of prognosis, and for planning surgery; however, the possible patterns of injury are innumerable, and no classification system can capture all injuries. Moreover, many variables contribute to preoperative planning, positioning, surgical approach, method of fixation, and prognosis; many relate to the soft tissue envelope (compartment syndrome), associated injuries (meniscal or ligamentous), and the overall condition of the patient who often has polytrauma.
Although the Orthopaedic Trauma Association uses the AO/OTA fracture classification system owing to its applicability to many extremities, the classification described by Schatzker et al. remains a relatively simple and familiar system for the tibial plateau.
However, its inconsistent and somewhat limited interobserver reliability is a shortcoming, and one suspects future classification systems or modifications to this one likely will incorporate axial imaging to describe comminuted, oblique, and sagittal fracture patterns; this is all the more important where high-energy injuries are concerned. Accurate surgical treatment requires a detailed 3-D description and understanding of fracture anatomy.
Even so, the Schatzker system has many advantages, including its familiarity, ease of use, and generally good reliability. Its major shortcomings come into play where complex, high-energy fracture patterns are concerned, and when 3-D imaging tools are required, findings from which were not included in the original rubric.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke SK. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg. 2006;88:1713–1721. doi: 10.2106/JBJS.E.00907. [DOI] [PubMed] [Google Scholar]
- 2.Barei DP, O’Mara TJ, Taitsman LA, Dunbar RP, Nork SE. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma. 2008;22:176–182. doi: 10.1097/BOT.0b013e318169ef08. [DOI] [PubMed] [Google Scholar]
- 3.Berkson EM, Virkus WW. High-energy tibial plateau fractures. J Am Acad Orthop Surg. 2006;14:20–31. doi: 10.5435/00124635-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Bennett WF, Browner B. Tibial plateau fractures: a study of associated soft tissue injuries. J Orthop Trauma. 1994;8:183–188. doi: 10.1097/00005131-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharyya T, McCarty LP, 3rd, Harris MB, Morrison SM, Wixted JJ, Vrahas MS, Smith RM. The posterior shearing tibial plateau fracture: treatment and results via a posterior approach. J Orthop Trauma. 2005;19:305–310. doi: 10.1097/01.bot.0000180369.24416.28. [DOI] [PubMed] [Google Scholar]
- 6.Brunner A, Horisberger M, Ulmar B, Hoffman A, Babst R. Classification systems for tibial plateau fractures: does computed tomography scanning improve their reliability? Injury. 2010;41:173–178. doi: 10.1016/j.injury.2009.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Carlson DA. Posterior bicondylar tibial plateau fractures. J Orthop Trauma. 2005;19:73–78. doi: 10.1097/00005131-200502000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Chan PS, Klimkiewicz JJ, Luchetti WT, Esterhai JL, Kneeland JB, Dalinka MK, Heppenstall RB. Impact of CT scan on treatment plan and fracture classification of tibial plateau fractures. J Orthop Trauma. 1997;11:484–489. doi: 10.1097/00005131-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Charalambous CP, Tryfonidis M, Alvi F, Moran M, Fang C, Samaraji R, Hirst P. Inter- and intra-observer variation of the Schatzker and AO/OTA classifications of tibial plateau fractures and a proposal of a new classification system. Ann R Coll Surg Engl. 2007;89:400–404. doi: 10.1308/003588407X187667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cole P, Levy B, Schatzker J, Watson JT. Tibial plateau fractures. In: Browner B, Levine A, Jupiter J, Trafton P, Krettek C, editors. Skeletal Trauma: Basic Science Management and Reconstruction. Philadelphia, PA: Saunders Elsevier; 2009. pp. 2201–2287. [Google Scholar]
- 11.Dirschl DR, Dawson PA. Injury severity assessment in tibial plateau fractures. Clin Orthop Relat Res. 2004;423:85–92. doi: 10.1097/01.blo.0000132626.13539.4b. [DOI] [PubMed] [Google Scholar]
- 12.Doornberg JN, Rademakers MV, van den Bekerom MP, Kerkhoffs GM, Ahn J, Steller EP, Kloen P. Two-dimensional and three-dimensional computed tomography for the classification and characterization of tibial plateau fractures. Injury. 2011;42:1416–1425. doi: 10.1016/j.injury.2011.03.025. [DOI] [PubMed] [Google Scholar]
- 13.Gardner MJ, Yacoubian S, Geller D, Pode M, Mintz D, Helfet DL, Lorich DG. Prediction of soft-tissue injuries in Schatzker II tibial plateau fractures based on measurements of plain radiographs. J Trauma. 2006;60:319–323. doi: 10.1097/01.ta.0000203548.50829.92. [DOI] [PubMed] [Google Scholar]
- 14.Higgins TF, Kemper D, Klatt J. Incidence and morphology of the posteromedial fragment in bicondylar tibial plateau fractures. J Orthop Trauma. 2009;23:45–51. doi: 10.1097/BOT.0b013e31818f8dc1. [DOI] [PubMed] [Google Scholar]
- 15.Hohl M. Tibial condylar fractures. J Bone Joint Surg Am. 1967;49:1455–1467. [PubMed] [Google Scholar]
- 16.Hohl M, Luck JV. Fractures of the tibial condyle: a clinical and experimental study. J Bone Joint Surg Am. 1956;38:1001–1018. [PubMed] [Google Scholar]
- 17.Honkonen SE, Järvinen MJ. Classification of fractures of the tibial condyles. J Bone Joint Surg Br. 1992;74:840–847. doi: 10.1302/0301-620X.74B6.1447244. [DOI] [PubMed] [Google Scholar]
- 18.Hu YL, Ye FG, Ji AY, Qiao GX, Liu HF. Three-dimensional computed tomography imaging increases the reliability of the classification systems for tibial plateau fractures. Injury. 2009;40:1282–1285. doi: 10.1016/j.injury.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 19.Khan RM, Khan SH, Ahmad AJ, Umar M. Tibial plateau fractures: a new classification scheme. Clin Orthop Relat Res. 2000;375:231–242. doi: 10.1097/00003086-200006000-00028. [DOI] [PubMed] [Google Scholar]
- 20.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24:683–692. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 21.Maripuri SN, Rao P, Manoj-Thomas A, Mohanty K. The classification systems for tibial plateau fractures: how reliable are they? Injury. 2008;39:1216–1221. doi: 10.1016/j.injury.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 22.Markhardt BK, Gross JM, Monu JU. Schatzker classification of tibial plateau fractures: use of CT and MR imaging improves assessment. Radiographics. 2009;29:585–597. doi: 10.1148/rg.292085078. [DOI] [PubMed] [Google Scholar]
- 23.Mohanlal P, Nathan S. An unusual shear type variant of tibial plateau fracture: a case report. Injury Extra. 2006;37:204–207. doi: 10.1016/j.injury.2005.11.015. [DOI] [Google Scholar]
- 24.Moore TM. Fracture-dislocation of the knee. Clin Orthop Relat Res. 1981;156:128–140. [PubMed] [Google Scholar]
- 25.Palmer I. Fractures of the upper end of the tibia. J Bone Joint Surg Br. 1951;33:160–166. [PubMed] [Google Scholar]
- 26.Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury. 2006;37:475–484. doi: 10.1016/j.injury.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 27.Potocnik P, Acklin YP, Sommer C. Operative strategy in postero-medial fracture-dislocation of the proximal tibia. Injury. 2011;42:1060–1065. doi: 10.1016/j.injury.2011.03.041. [DOI] [PubMed] [Google Scholar]
- 28.Schatzker J. Compression in the surgical treatment of fractures of the tibia. Clin Orthop Relat Res. 1974;105:220–239. doi: 10.1097/00003086-197411000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: the Toronto experience: 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 30.Stark E, Stucken C, Trainer G, Tornetta P., 3rd Compartment syndrome in Schatzker type VI plateau fractures and medial condylar fracture-dislocations treated with temporary external fixation. J Orthop Trauma. 2009;23:502–506. doi: 10.1097/BOT.0b013e3181a18235. [DOI] [PubMed] [Google Scholar]
- 31.te Stroet MA, Holla M, Biert J, van Kampen A. The value of a CT scan compared to plain radiographs for the classification and treatment plan in tibial plateau fractures. Emerg Radiol. 2011;18:279–283. doi: 10.1007/s10140-010-0932-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tscherne H, Lobenhoffer P. Tibial plateau fractures: management and expected results. Clin Orthop Relat Res. 1993;292:87–100. [PubMed] [Google Scholar]
- 33.Wahlquist M, Iaguilli N, Ebraheim N, Levine J. Medial tibial plateau fractures: a new classification. J Trauma. 2007;63:1418–1421. doi: 10.1097/TA.0b013e3181469df5. [DOI] [PubMed] [Google Scholar]
- 34.Walton NP, Harish S, Roberts C, Blundell C. AO or Schatzker? How reliable is classification of tibial plateau fractures? Arch Orthop Trauma Surg. 2003;123:396–398. doi: 10.1007/s00402-003-0573-1. [DOI] [PubMed] [Google Scholar]
- 35.Weil YA, Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Posteromedial supine approach for reduction and fixation of medial and bicondylar tibial plateau fractures. J Orthop Trauma. 2008;22:357–362. doi: 10.1097/BOT.0b013e318168c72e. [DOI] [PubMed] [Google Scholar]
- 36.Yacoubian SV, Nevins RT, Sallis JG, Potter HG, Lorich DG. Impact of MRI on treatment plan and fracture classification of tibial plateau fractures. J Orthop Trauma. 2002;16:632–637. doi: 10.1097/00005131-200210000-00004. [DOI] [PubMed] [Google Scholar]