Abstract
Background
While surgical navigation offers the opportunity to accurately place an acetabular component, questions remain as to the best goal for acetabular component positioning in individual patients. Overall functional orientation of the pelvis after surgery is one of the most important variables for the surgeon to consider when determining the proper goal for acetabular component orientation.
Questions/Purposes
We measured the variation in pelvic tilt in 30 patients before THA and the effect of THA on pelvic tilt in the same patients more than a year after THA.
Methods
Each patient had a CT study for CT-based surgical navigation and standing and supine radiographs before and after surgery. Pelvic tilt was calculated for each of the radiographs using a novel and validated two-dimensional/three-dimensional matching technique.
Results
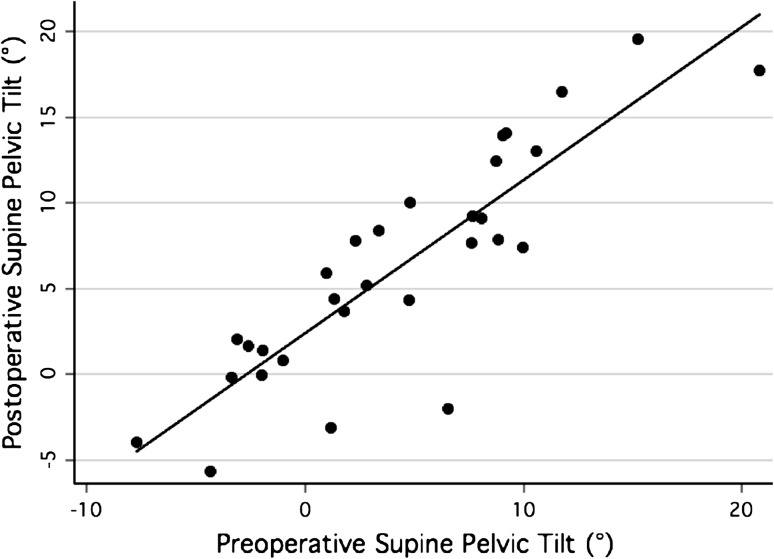
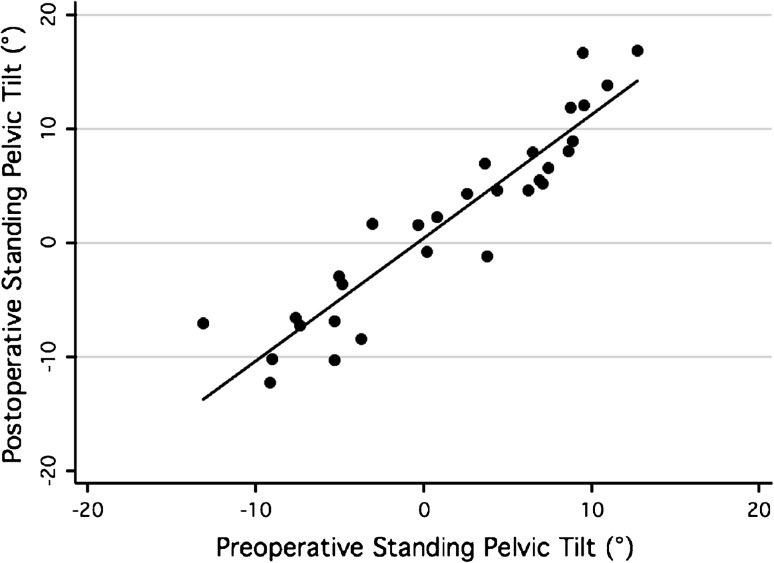
Mean supine pelvic tilt changed less than 2°, from 4.4° ± 6.4° (range, −7.7° to 20.8°) before THA to 6.3° ± 6.6° (range, −5.7° to 19.6°) after THA. Mean standing pelvic tilt changed less than 1°, from 1.5° ± 7.2° (range, −13.1° to 12.8°) before THA to 2.0° ± 8.3° (range, −12.3° to 16.8°) after THA. Preoperative pelvic tilt correlated with postoperative tilt in both the supine (r2 = 0.75) and standing (r2 = 0.87) positions.
Conclusions
In this population, pelvic tilt had a small and predictable change after surgery. However, intersubject variability of pelvic tilt was high, suggesting preoperative pelvic tilt should be considered when determining desired acetabular component positioning on a patient-specific basis.
Introduction
Acetabular component positioning is directly related to the incidences of hip dislocation and wear, the two most common causes of THA failure [5, 14, 20]. Factors to consider for optimization of cup orientation [15] on a patient-specific basis include femoral anteversion, fundamental hip biomechanical considerations [2], intraoperative assessment, and the position of the pelvis in functional positions [1]. However, as improved methods of achieving desired cup orientation are developed [1, 7, 9, 11–13, 16, 18, 21, 22], questions concerning the proper orientation of the acetabular component on a patient-specific basis become increasingly relevant [24].
Pelvic tilt, or the relationship between the spine and the pelvis in the sagittal plane [6, 8], directly affects the functional orientation of the acetabular component and therefore the biomechanics, impingement-free motion, and stability of the joint. Wolf et al. [25] developed a kinematic error model to predict cup malposition based on pelvic tilt. One study of pelvic tilt by Babish et al. [1] suggest that supine pelvic tilt should be incorporated, degree for degree, into cup orientation goals. Conversely, a gait study by Parratte et al. [19] reported pelvic tilt change after surgery is so variable that accurate navigation of cup orientation may potentially lead in some cases to improper functional cup orientation. However, a radiographic study by Blondel et al. [4] demonstrated no difference between standing pelvic tilt before and after THA. These contradictory study results leave uncertainty concerning both pelvic tilt and the effect of THA on pelvic tilt.
In an effort to improve our understanding of this issue, we used two-dimensional (2D)/three-dimensional (3D) matching methods [3] to measure the effect of THA on pelvic tilt in both the supine and standing positions.
Patients and Methods
This study assessed pelvic tilt change after THA in 15 women and 15 men who underwent computer-assisted CT-based navigation of acetabular component insertion during THA. Each patient had AP pelvis radiographs in the standing and supine positions before surgery. A high-resolution pelvis CT scan [10] was obtained for surgical navigation and preoperative planning. To be enrolled in the cohort, the inclusion criteria required that each subject needed standing and supine radiographs both before and after surgery with the anterior superior iliac spines and pubic symphsis visible to ensure accuracy of the analysis. The mean age was 59.9 years (range, 37–80 years). Nineteen patients had a diagnosis of osteoarthrosis or femoroacetabular impingement, 10 patients had developmental dysplasia of the hip, and one patient had protrusio. All patients gave informed consent to participate in this institutional review board-approved study.
All surgeries were performed by one of the senior authors (SBM) between July 2007 and May 2010.
Pre- and postoperative supine and standing AP pelvic radiographs were again acquired at a minimum of 1 year after surgery. The beam to x-ray plate distance was 102 cm. The patients had blocks placed under the foot if necessary to level the pelvis for the standing radiographs. For each image, pelvic tilt was calculated using a validated noncommercial 2D/3D matching application (HipMatch; Institut for Surgical Technology and Biomechanics, Bern, Switzerland) [23, 26]. This software application allows the user to calculate the pelvic tilt, or the angular difference between the patient’s anterior pelvic plane (APP) and the plane of the radiograph. HipMatch uses a fully automated registration procedure that can match the 3D model of the preoperative CT with the projected pelvis on each radiograph. The details of the graphic matching algorithm, reproducibility, and reliability have been reported previously [23, 25].
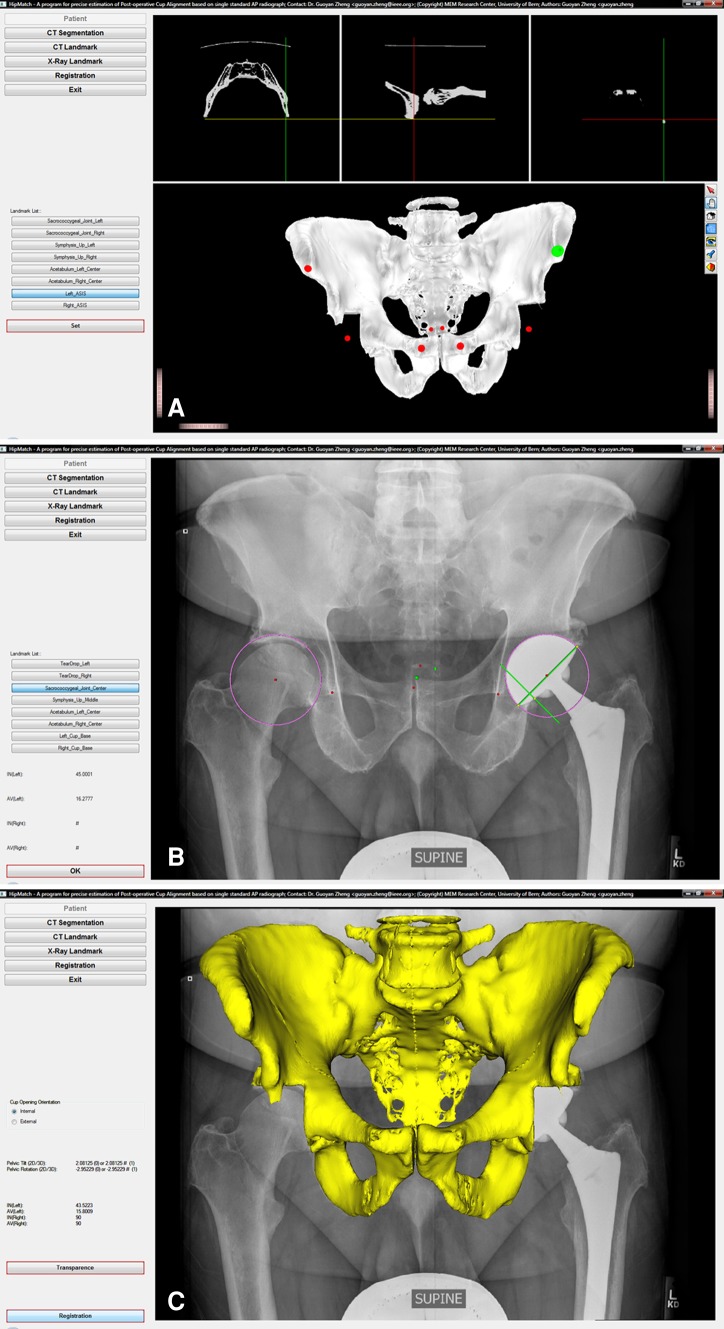
To calculate pelvic tilt, a CT scan for each patient was segmented and a 3D model pelvis was produced. Points were placed on the 3D model pelvis to determine the APP (Fig. 1A). Landmarks were also entered onto the radiograph to allow for initial approximate alignment to minimize subsequent matching calculations (Fig. 1B). HipMatch then performed an automated 2D/3D matching algorithm to calculate the 3D position of the pelvis at the time the radiograph was acquired and superimposed a 3D model of the pelvis onto the radiograph at the completion of the calculation (Fig. 1C). HipMatch recorded the angle of the APP on the radiograph and reported the pelvic tilt as the angle in the sagittal plane between the APP and the plane of the radiograph. Pelvic tilt was positive if the anterior superior iliac spines were anterior to the pubic symphysis and negative if the pubic symphysis was anterior to the anterior superior iliac spines. We tested the assumption of data normality with the Shapiro-Wilk test and compared average preoperative and postoperative pelvic tilt with a two-tailed Student’s t-test. We determined the correlation of the preoperative pelvic tilt on standing and supine radiographs and that of the postoperative pelvic tilt on standing and supine radiographs with a Pearson’s correlation. All statistical analyses were performed with STATA® statistical software (Release 10; StataCorp LP, College Station, TX, USA).
Fig. 1A–C.
(A) In the initial steps of HipMatch, the CT data are segmented, a 3D model of the pelvis is formed, and the APP coordinate system is defined. (B) The plain radiograph is then prepared with preliminary landmarks to minimize subsequent matching calculations. (C) HipMatch then matches the 3D model to the plain radiograph, thereby determining the 3D position of the pelvis in space when the radiograph was taken.
Results
Supine and standing pelvic tilt data before and after hip arthroplasty are summarized (Table 1). Mean supine pelvic tilt changed (p = 0.004) after THA; however, the magnitude of this change was less than 2°. Mean standing pelvic tilt did not change (p = 0.34) after THA. Preoperative pelvic tilt was predictive of postoperative tilt in both the supine (r2 = 0.75, Fig. 2) and standing (r2 = 0.87, Fig. 3) positions. Ninety percent of patients had a change in pelvic tilt within 5°. Only two patients experienced change in pelvic tilt of more than 5°. Preoperative supine pelvic tilt correlated with (r2 = 0.57) preoperative standing tilt and postoperative supine pelvic tilt correlated with (r2 = 0.61) postoperative standing tilt.
Table 1.
Preoperative and postoperative supine and standing pelvic tilt values
| Variable | Mean (°) | SD (°) | Range (°) | p value |
|---|---|---|---|---|
| Preoperative supine pelvic tilt | 4.4 | 6.4 | (−7.7, 20.8) | |
| Preoperative standing pelvic tilt | 1.5 | 7.2 | (−13.1, 12.8) | |
| Postoperative supine pelvic tilt | 6.3 | 6.6 | (−5.7, 19.6) | |
| Postoperative standing pelvic tilt | 2 | 8.3 | (−12.3, 16.8) | |
| Change in supine pelvic tilt | 1.9 | 3.3 | (−8.5, 5.5) | 0.004 |
| Change in standing pelvic tilt | 0.5 | 3 | (−5, 7.15) | 0.34 |
Fig. 2.
The correlation between supine pelvic tilt before and 1 year after THA is shown (r2 = 0.75).
Fig. 3.
The correlation between standing pelvic tilt before and 1 year after THA is shown (r2 = 0.87).
Discussion
Recent advances in surgical navigation have made component positioning in THA increasingly accurate relative to the stated goal of cup position. However, surgeons must ultimately decide their goal of acetabular orientation regardless of what method of component alignment is used during surgery. When navigation methods are used, this goal can be stated in any coordinate system but is typically stated with reference to the conventional APP coordinate system. Improvement in our understanding of the effect of THA on pelvic tilt will improve our ability to predict the functional position of the pelvis after surgery. This information may be used to further refine the goal for optimal cup orientation on an individual patient basis. We therefore used novel 2D/3D matching methods to measure the effect of THA on pelvic tilt in both the supine and standing positions.
Our study is limited in several ways. First, the study population is currently limited to 30 patients. Second, all radiographic studies are limited in that the radiographic view is of a single position at a single moment in time whereas the relationship between the spine and pelvis is dynamic. Still, the position of the pelvis in a standing position is well correlated with the position of the acetabulum during walking with implications for wear and edge loading [2].
We found pelvic tilt typically changes little as a result of surgery and preoperative pelvic tilt is predictive of postoperative pelvic tilt in both the standing and supine positions. These findings therefore suggest preoperative pelvic tilt may be used as a variable in determining appropriate component positioning. These findings are also consistent with the study of Blondel et al. [4], which showed standing pelvic tilt, as measured on standing lateral radiographs, did not change as a result of THA. Specifically, their study used lateral radiographs in 50 patients and demonstrated, 3 years after THA, 95% of subjects had a change in tilt of less than 5°. The other 5% of patients had variation of less than 10°. Similarly, in a CT-based study of 74 patients with THA, Nishihara et al. [17] also showed all but one patient had an alteration in pelvic tilt of less than 10° after surgery. The correlation coefficient was 0.86 for supine radiographs and 0.77 for standing films.
Prior work on pelvic positioning and THA by Blondel et al. [4], DiGioia et al. [6], Nishihara et al. [17], and Parratte et al. [19] all showed high intersubject variability, whether supine or standing. Similarly, our study also showed a high intersubject variability of pelvic tilt with a range of 21° to −8° in the supine and 13° to −13° in the standing positions. This fact, combined with the finding that pelvic tilt changes very little as a result of surgery, supports the suggestions of Wolf et al. [25] and Babisch et al. [1] that knowledge about patient-specific preoperative pelvic tilt should be a factor to consider when determining the optimal goal for acetabular component positioning for each patient.
Our study and those of Blondel et al. [4] and Nishihara et al. [17] all have consistent findings in that pelvic tilt changed minimally as a result of THA. By contrast, the study of 21 patients by Parratte et al. [19] is the only study that showed a greater degree of variability in pelvic tilt after THA. Their study however used gait analysis with superficial skin markers, a technique that requires inference of pelvic position by indirect means. The other studies assessed the position of the pelvis using direct radiographic techniques; the current method of 2D/3D matching has a high degree of accuracy, reproducibility, and reliability [23].
It may well be that there is no true optimal orientation of an acetabular component on an individual patient basis in part because activities related to dislocation are so variable and idiosyncratic. This issue is well described by Widmer [24]. Optimal cup orientation for maximal hip stability, impingement-free ROM, and minimization of contact pressure during walking and other activities may all be different positions. Still, improved understanding of pelvic tilt may eventually allow for more comprehensive patient-specific cup alignment optimization, taking stability, motion, and wear minimization into account, potentially reducing the incidence of instability and wear-associated loosening, the two most common reasons for revision hip arthroplasty.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
This work was performed at the Center for Computer Assisted and Reconstructive Surgery, New England Baptist Hospital, Boston, MA, USA.
References
- 1.Babisch JD, Layher F, Maiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–365. doi: 10.2106/JBJS.F.00628. [DOI] [PubMed] [Google Scholar]
- 2.Bergmann G, Deuretzbacher G, Heller F, Graichen F, Rohlmann A, Strauss J, Duda GN. Hip contact forces and gait patterns from routine activities. J Biomech. 2001;34:859–871. doi: 10.1016/S0021-9290(01)00040-9. [DOI] [PubMed] [Google Scholar]
- 3.Blendea S, Eckman K, Jaramaz B, Levison TJ, DiGioia AM., 3rd Measurements of acetabular cup position and pelvic spatial orientation after total hip arthroplasty using computed tomography/radiography matching. Comput Aided Surg. 2005;10:37–41. doi: 10.3109/10929080500178032. [DOI] [PubMed] [Google Scholar]
- 4.Blondel B, Parratte S, Tropiano P, Pauly V, Aubaniac JM, Argenson JN. Pelvic tilt measurement before and after total hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:568–572. doi: 10.1016/j.otsr.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 6.DiGioia AM, 3rd, Hafez MA, Jaramaz B, Levison TJ, Moody JE. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272–276. doi: 10.1097/01.blo.0000238862.92356.45. [DOI] [PubMed] [Google Scholar]
- 7.Ecker TM, Tannast M, Murphy SB. Computed tomography-based surgical navigation for hip arthroplasty. Clin Orthop Relat Res. 2007;465:100–105. doi: 10.1097/BLO.0b013e3181591c7d. [DOI] [PubMed] [Google Scholar]
- 8.Eckman K, Hafez MA, Ed F, Jaramaz B, Levison TJ, DiGioia AM., 3rd Accuracy of pelvic flexion measurements from lateral radiographs. Clin Orthop Relat Res. 2006;451:154–160. doi: 10.1097/01.blo.0000238809.72164.54. [DOI] [PubMed] [Google Scholar]
- 9.Hube R, Birke A, Hein W, Klima S. CT-based and fluoroscopy-based navigation for cup implantation in total hip arthroplasty (THA) Surg Technol Int. 2003;11:275–280. [PubMed] [Google Scholar]
- 10.Huppertz A, Radmer S, Asbach P, Juran R, Schwenke C, Diederichs G, Hamm B, Sparmann M. Computed tomography for preoperative planning in minimal-invasive total hip arthroplasty: radiation exposure and cost analysis. Eur J Radiol. 2011;78:406–413. doi: 10.1016/j.ejrad.2009.11.024. [DOI] [PubMed] [Google Scholar]
- 11.Jaramaz B, DiGioia AM, 3rd, Blackwell M, Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop Relat Res. 1998;354:70–81. doi: 10.1097/00003086-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179. doi: 10.1097/01.blo.0000141903.08075.83. [DOI] [PubMed] [Google Scholar]
- 13.Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg. 2002;7:99–106. doi: 10.3109/10929080209146021. [DOI] [PubMed] [Google Scholar]
- 14.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 15.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 16.Murphy SB, Ecker TM, Tannast M. THA performed using conventional and navigated tissue-preserving techniques. Clin Orthop Relat Res. 2006;453:160–167. doi: 10.1097/01.blo.0000246539.57198.29. [DOI] [PubMed] [Google Scholar]
- 17.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140–151. doi: 10.1097/01.blo.0000069891.31220.fd. [DOI] [PubMed] [Google Scholar]
- 18.Nogler M, Kessler O, Prassi A, Donnelly B, Streicher R, Siedge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163. doi: 10.1097/01.blo.0000141902.30946.6d. [DOI] [PubMed] [Google Scholar]
- 19.Parratte S, Pagnano MW, Coleman-Wood K, Kaufman KR, Berry DJ. The 2008 Frank Stinchfield Award. Variation in postoperative pelvic tilt may confound the accuracy of hip navigation systems. Clin Orthop Relat Res. 2009;467:43–49. doi: 10.1007/s11999-008-0521-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patil S, Bergula A, Chen PC, Colwell CW, D’Lima DD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85(suppl 4):56–63. doi: 10.2106/00004623-200300004-00007. [DOI] [PubMed] [Google Scholar]
- 21.Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grutzner PA, Steffen R, von Knoch M, Holland-Letz T, Bernsmann K. [Cup placement in hip replacement surgery—a comparison of free-hand and computer assisted cup placement in total hip arthroplasty—a multi-center study] [in German] Z Orthop Ihre Grenzgeb. 2004;142:286–291. doi: 10.1055/s-2004-822696. [DOI] [PubMed] [Google Scholar]
- 22.Steppacher SD, Kowal JH, Murphy SB. Improving cup positioning using a mechanical navigation instrument. Clin Orthop Relat Res. 2011;469:423–428. doi: 10.1007/s11999-010-1553-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steppacher SD, Tannast M, Zheng G, Zhang X, Kowal J, Anderson SE, Siebenrock KA, Murphy SB. Validation of a new method for determination of cup orientation in THA. J Orthop Res. 2009;27:1583–1588. doi: 10.1002/jor.20929. [DOI] [PubMed] [Google Scholar]
- 24.Widmer KH. Containment versus impingement: finding a compromise for cup placement in total hip arthroplasty. Int Orthop. 2007;31(suppl 1):S29–S33. doi: 10.1007/s00264-007-0429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolf A, DiGioia AM, 3rd, Mor AB, Jaramaz B. Cup alignment error model for total hip arthroplasty. Clin Orthop Relat Res. 2005;437:132–137. doi: 10.1097/01.blo.0000164027.06880.3a. [DOI] [PubMed] [Google Scholar]
- 26.Zheng G, Zhang X, Steppacher SD, Murphy SB, Siebenrock KA, Tannast M. HipMatch: an object-oriented cross-platform program for accurate determination of cup orientation using 2D-3D registration of single standard x-ray radiograph and a CT volume. Comput Methods Programs Biomed. 2009;95:236–248. doi: 10.1016/j.cmpb.2009.02.009. [DOI] [PubMed] [Google Scholar]