Abstract
Background
Currently, the two most commonly used options for the revision of femoral components in North America are: cylindrical, nonmodular, cobalt-chromium stems and tapered, fluted, modular, titanium (TFMT) stems. Previous reports have cited high failure rates with cylindrical cobalt chrome stems in large femoral defects but the longer term survival of the fluted stems is unknown.
Questions/Purposes
We examined the 5- to 10-year survival of TFMT stems implanted for severe femoral defects.
Methods
We reviewed all 65 patients with severe proximal bone defects revised with the TMFT stem between January 2000 and 2006. Ten were lost to followup and seven were dead, leaving 48 patients for followup at 5 to 10 years (mean, 84 months; range, 60–120 months). All patients completed five quality-of-life (QOL) questionnaires. Radiographs were evaluated for loosening, subsidence, and preservation of proximal host bone stock.
Results
Implant survivorship was 90%. No patient underwent revision for either subsidence or loosening. Subsidence occurred in seven patients (average, 12.3 mm) but all achieved secondary stability. Five patients underwent revision as a result of fracture of the stem and all had the original standard stem design, which has since been modified. All five implant fractures occurred at the modular stem junction. Mean QOL outcomes were: WOMAC = 81 (pain), Oxford = 75, SF-12 = 54 (mental) and 38 (physical), UCLA Activity = 4, and satisfaction overall = 73.
Conclusions
Midterm survivorship of modular titanium stems in large femoral defects is high; however, ongoing surveillance of stem junctional fatigue life is required.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Most surgeons in North America use one of two cementless distal fixation options when revising a THA femoral component: cylindrical, nonmodular fully porous, cobalt-chromium (CNCC) stems and tapered, fluted, modular, titanium (TFMT) stems. Both options are available in modular and nonmodular configurations, but for the most part, nonmodular fully porous-coated stems and modular tapered fluted titanium stems have been the most popular in North America. CNCC fully porous-coated stems have been traditionally regarded as the gold standard for femoral revision with long-term survival rates ranging from 89% to 98% [8, 10, 12, 16, 21, 24, 26, 28, 37]. However, concern has been raised regarding the use of these stems in patients with severe proximal femoral bone loss, thin cortices, and large ectatic canals where less than 4 cm of scratch fit can be obtained at the level of the isthmus. Sporer and Paprosky [34] showed mechanical failure rate of these fully porous-coated CNCC stems in patients with major bone deficiency and in canals greater than 19 mm in diameter can be as much as 18% to 38%. Other potential disadvantages of these CNCC fully porous-coated stems include: increased prevalence of postoperative thigh pain, increased incidence of intraoperative insertional fractures, and further stress shielding of the proximal femur [16, 23, 24, 37].
TFMT stems have been designed to address many of these disadvantages. Their titanium composition means a lower modulus of elasticity for any given diameter as compared with cobalt-chromium, which translates into reduced stem stiffness for equivalent stem diameters. The theoretical result would be that titanium stems have reduced incidence of thigh pain and less proximal femoral stress shielding. Their modularity allows for intraoperative adjustment of leg length, horizontal offset, and neck version. Torsional stability is controlled by the flutes that cut into the diaphysis and the tapered geometry provides axial stability. In two studies, we compared these two revision femoral stem designs (CNCC versus TFMT stems) in terms of quality-of-life (QOL) outcomes, intraoperative complications, and preservation of femoral host bone stock [9, 32] (Table 1). Both studies demonstrated that the patient satisfaction and QOL outcome scores substantially favored the TFMT stems. We also demonstrated a lower incidence of intraoperative fractures (9% for TFMT versus 25% for CNCC) and better restoration of proximal femoral bone stock.
Table 1.
Comparison of our study and other studies in the literature evaluating tapered, fluted, modular, titanium stems
| Study | Year | Number of patients | Length of followup | Bone deficiency | Quality-of-life instrument(s) used |
|---|---|---|---|---|---|
| Garbuz et al. [9] | 2006 | 220 | 24 months (median) | Not assessed | WOMAC, SF-12, Oxford-12, Satisfaction |
| Kang et al. [13] | 2008 | 42 | 2–5 years | Paprosky Type 2, 3A, 3B | WOMAC, Harris hip score |
| Koster et al. [15] | 2008 | 73 | 5–10 years | Harris hip score | |
| Lakstein et al. [18] | 2010 | 69 | 5–10 years | Saleh Type II, III, IV, V | Harris hip score |
| Lakstein et al. [19] | 2011 | 6 | 13–80 months | Gross Classification 2 and 4 | Not assessed |
| McInnis et al. [22] | 2006 | 70 | Mean, 47 months | Pak Type 1, 2A-C, 3A-C; Bohm and Bischel Type 1A-B, 2A-B, 3A-B. | Oxford hip score |
| Ovesen et al. [27] | 2010 | 125 | 2–7 years | Saleh Type I, II, III, IV, V, VI | Harris hip score |
| Park et al. [29] | 2010 | 59 | Mean, 8 years | Paprosky Type 1, 2, 3A, 3B, 4 | Harris hip score |
| Richards et al. [32] | 2010 | 200 | Mean, 37 months | Paprosky Type 3B and 4 | WOMAC, SF-12, Oxford-12, UCLA Activity Level |
| Sporer and Paprosky [35] | 2004 | 16 | Mean, 2 years | Paprosky Type 3B and 4 | D’Aubigne and Postel Functional score |
| Weiss et al. [38] | 2011 | 90 | 5–11 years | Paprosky Type 1, 2, 3A, 3B, 4 | Harris hip score |
| Current study | 48 | 5–10 years (mean, 84 months) | Paprosky Type 3B and 4 | WOMAC, SF-12, Oxford-12, UCLA Activity Level |
Despite the patient satisfaction and QOL scores, concern exists over the potential long-term fixation of these TFMT implants over time. Previous studies have shown a risk of implant fracture at the level of the modular junction [19, 27, 32] (Table 1). Concern seems to be heightened where there is poor proximal femoral bony support around the modular junction. A number of studies reporting early (minimum 2-year) followup demonstrate implant survival rates ranging from 94% to 99% [9, 13, 17, 22, 25, 27, 30–33]. More recently mid- to long-term followup studies (minimum 5 years) are now being reported with implant survival rates ranging from 91% to 98% [15, 18, 29, 38] (Table 1). However, the majority of these studies have not distinguished between patients with adequate proximal femoral bone stock and those with severe bone deficiencies. Only one such study has examined the outcome of these TFMT stems in patients with severe proximal femoral bone defects in isolation. Sporer and Paprosky [35] followed a small cohort of 16 patients with severe femoral deficiency (Type 3B and 4) that underwent revision with TFMT stems. They demonstrated one failure among the 16 cases at only a 2-year followup. They advocated longer followup before the use of this stem can be recommended in all patients with severe proximal femoral deficiency. Thus, it is unclear whether the earlier high survival rate will persist with longer followup.
We therefore assessed the 5- to 10-year survivorship of TFMT stems in patients with severe proximal femoral bone defects at the time of revision hip arthroplasty.
Patients and Methods
We retrospectively reviewed all 65 patients undergoing revision THA with severe proximal femoral bone defects between January 2000 and January 2006. All patients had TFMT stems, which were part of the Zimmer Modular Revision Hip system (ZMR®; Zimmer, Warsaw, IN, USA). Of the 65 patients, 10 were lost to followup and seven patients were dead, leaving 48 patients available for QOL outcome and radiographic evaluation. None of the deaths were related to complications from their revision hip arthroplasty. The average time from surgery to death was 63 months (range, 28–82 months) and the average age at time of death was 82 years (range, 72–92 years). We contacted next of kin for each patient who had died and confirmed each of the hips was functioning satisfactorily at the time of death. One patient had both of her THAs revised for 49 hips in 48 patients. The mean age at the time of surgery was 70 years (range, 41–87 years). Sex distribution for hips, was nearly equal with 24 (49%) males and 25 (51%) females. The indications for the revisions were as follows: 35 (71%) for aseptic loosening, six (12%) for periprosthetic fracture, and eight (16%) for infection (two-stage revision). The minimum followup was 5 years (mean, 84 months; range, 60–120 months). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
Preoperative bone deficiency was classified based on the classification system described by Della Valle and Paprosky [6] and Sporer and Paprosky [34]. This classification has intra- and interobserver reliability of 0.54 and 0.42, respectively [11]. According to this classification system (referred to as “Paprosky”), Type 3B defects involve metaphyseal bone loss with less than 4 cm of possible scratch fit at the level of the isthmus. Type 4 defects are characterized by extensive metadiaphyseal damage resulting in thin cortices and a widened femoral canal. In the current study, 42 (86%) of the hips had Type 3B preoperative proximal femoral bone defects and seven (14%) were Type 4. We only included patients with Paprosky Type 3B or 4 femoral defects.
The operation was performed by one of the four senior authors (DSG, BAM, CPD, NVG), who each specialize in adult reconstructive arthroplasty. In 46 (94%) of the cases, the surgeon used the posterolateral approach with the remaining patients undergoing a direct lateral approach. The acetabular cup was revised in addition to the femoral component in the majority of cases. Thirty-nine (80%) hips underwent a combined acetabular and femoral revision, six (12%) received an isolated liner exchange with the femoral revision, and four (8%) had the femoral revision performed alone. An extended trochanteric osteotomy (ETO) was carried out in 28 (57%) cases and for each of these patients, a prophylactic cerclage wire was placed distal to the osteotomy site to decrease the risk of intraoperative fracture during stem insertion. The previous femoral component that was extracted during the operation was cemented in 41 (84%) hips and cementless in the remaining eight (16%) hips. To augment femoral bone stock, a cortical strut allograft was used in 15 (31%) hips. In general, a strut was used to augment poor lateral bone stock and reinforce the ETO fragment. This augmentation with cortical allograft struts was largely used early in the study period. As time progressed, we decreased the use of these strut allografts even in the face of poor proximal femoral host bone.
The ZMR® modular revision hip system comes in varying stem lengths and diameters, variable neck lengths and offsets, and a modular junction between the body and stem components. The body is available in several geometries (cone, spout, calcar, taper), each with its own size/geometry. The systems consist of two main designs, the original standard design and the ZMR® XL design. Twenty-seven (55%) hips received the standard ZMR® implant and 22 (45%) received the ZMR® XL stem. Stem lengths varied across the three standard lengths (170, 185, 235 mm) with the majority (67%) having the 185-mm stem length. Stem diameters averaged 19 mm (range, 15–23 mm). Extended femoral neck offsets were used in 38 (78%) hips with the remaining 11 (22%) hips receiving a standard femoral neck offset. Neck lengths varied from: −3.5 mm (31%), 0 mm (25%), +3.5 mm (21%), +7 mm (14%), and +10.5 mm (5%) and head diameters averaged 32.7 mm (range, 26–40 mm).
The postoperative protocol was the same for all patients. Patients were kept nonweightbearing for a period of 6 weeks followed by partial weightbearing with gradual progression to full weightbearing by 3 months postoperatively. Hip flexion and rotation precautions were maintained for the initial 3 months postoperatively and patients receiving an ETO were restricted from performing any active hip abduction exercises for the first 6 weeks.
All patients were seen in the clinic at 6 weeks, 3 months, 12 months, and then at variable time lengths after 1 year. All patients were seen at a minimum of 5 years postoperatively for QOL assessment and radiographic analysis. All patients completed five validated QOL outcome questionnaires: the Oxford-12 hip score [5] as a joint-specific instrument, WOMAC [2] as a disease-specific instrument, the SF-12 as a generic health quality instrument [36], the UCLA Activity Score [1], and the hip and knee arthroplasty satisfaction questionnaire [14, 20]. We obtained informed consent from all patients as per our institutional review board approval. The Oxford hip score and the WOMAC scores were normalized to a range of 0 to 100 with 0 being the worst and 100 being the best.
Charts were reviewed for incidence of major complications after the revision procedures. These included: infection, intraoperative fracture, stem fracture, and hip instability or dislocation.
We obtained radiographs preoperatively, immediately after surgery, and then at each of the followup intervals including a minimum of 5 years after revision surgery. Radiographic analysis consisted of a standard AP pelvis, crosstable lateral hip, and AP and lateral views of the femur. All of the radiographs were reviewed by one of the authors (APVH) who was not involved in any of the patients’ care. The preoperative radiographs were assessed to confirm their Paprosky classification. All postoperative radiographs were evaluated for loosening, subsidence, and preservation or restoration of the proximal femur host bone. The initial postoperative radiographs served as the baseline with which the long-term radiographs were then compared. Loosening was determined by analysis of the followup radiographs. For porous-coated stems, the Engh fixation scale [7] has been used. However, because these stems are not porous-coated, the Engh scale would not be appropriate. For this reason, we used subsidence as an indication of initial loosening. Subsidence was determined by measuring the distance between a fixed point on the femoral component (typically the modular junction or center of the femoral head) and a fixed point on the femur (the lesser trochanter if available). A difference of 5 mm or more in the measured distance between the immediate postoperative radiograph and the long-term followup radiograph, after adjusting for magnification, was considered as significant subsidence [13, 18, 35]. We used a 25-mm radiographic marker for all radiographs because this is the routine at our center. The same author (APVH) classified the radiographic changes in the proximal femoral bone stock at the time of latest followup using a method previously described by Bohm and Bischel [3] and used in the previous study performed by the senior authors [32]. Change in proximal femoral bone stock was simply classified as A (increasing defects), B (constant defects), or C (osseous restoration) for each of the patients in this study [3].
Results
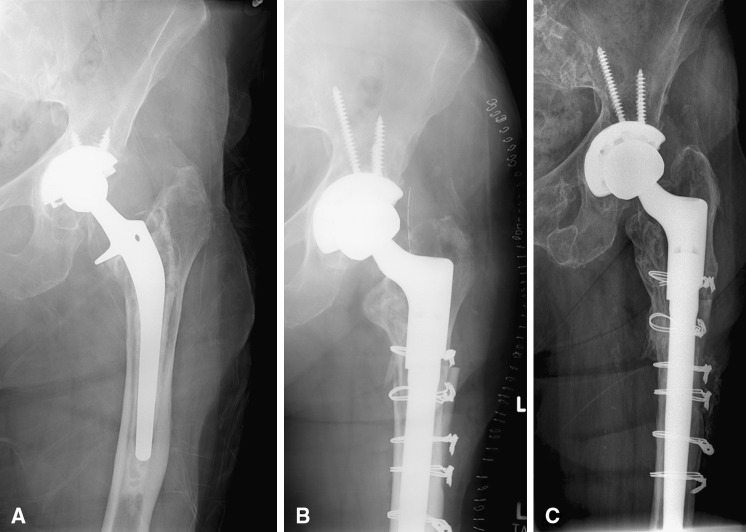
The QOL functional outcome results were encouraging and comparable to previous published results of patients with revision THA with TMFT stems. The mean WOMAC score was 78, mean Oxford score was 75, and the mean UCLA activity score was 4.3 (Table 2). Only six (12%) hips were noted to have a decrease in proximal femoral bone stock (Type A). Twenty-seven (55%) hips demonstrated no change (Type B) in proximal femoral bone stock and 16 (33%) have radiographic evidence of osseous restoration (Type C). At latest followup, all stems were considered stable. Radiographic analysis revealed no cases of implant loosening. Substantial implant subsidence (> 5 mm) occurred in six patients with an average subsidence of 12.3 mm (range, 5–20 mm). No patient underwent revision for either loosening or continuous subsidence. Each of the six patients who demonstrated major subsidence was followed with serial radiographs and demonstrated achievement of secondary stability during the first postoperative year (Fig. 1). When comparing the QOL results of these subsidence patients with mean scores of the entire study group, they demonstrated similar, if not, higher outcome scores at the latest followup (Table 3). On the latest followup radiographs in approximately 16 (33%) of the patients, bone trabeculation was seen bridging between the inner cortex and the distal tip of the stem. This finding was also noted in a previous 5- to 10-year followup study involving a different type of TFMT stem (Profemur-R revision stem; Wright Medical, Arlington, VA, USA) [15]. This group reported a rate of 37% of osseous hypertrophy at the tip of the implant.
Table 2.
Quality-of-life outcome scores: comparison with our previous studies
| Quality-of-life measure | Mean scores from Garbuz et al. [9] (minimum 1-year followup) | Mean scores from Richards et al. [32] (minimum 2-year followup) | Mean scores from the current study (minimum 5-year followup) |
|---|---|---|---|
| Oxford hip score* | 79 | 77 | 75 |
| SF-12 mental component | 56 | 53 | 54 |
| SF-12 physical component | 41 | 39 | 38 |
| Satisfaction overall score | 97 | 90 | 73 |
| WOMAC pain* | 84 | 84 | 81 |
| WOMAC stiffness* | – | 76 | 75 |
| WOMAC function* | 75 | – | 77 |
| WOMAC global* | – | – | 78 |
| UCLA Activity score | – | 5.1 | 4.3 |
* Oxford hip score and the WOMAC scores are normalized to a range of 0 to 100 with 0 being the worst and 100 being the best.
Fig. 1A–C.
AP pelvic radiographs showing a patient who had subsidence of the stem and it achieved secondary stability. (A) Preoperative view, (B) immediately postoperative, and (C) 5 years and 7 months postoperatively.
Table 3.
Quality-of-life outcome scores: comparison of patients who experienced major subsidence versus the entire study group
| Quality-of-life measure | Subsidence patients (mean scores) | Entire study group (mean scores) |
|---|---|---|
| Oxford hip score* | 80 | 75 |
| SF-12 mental component | 62 | 54 |
| SF-12 physical component | 45 | 38 |
| Satisfaction overall score | 93 | 73 |
| WOMAC pain* | 90 | 81 |
| WOMAC stiffness* | 83 | 75 |
| WOMAC function* | 82 | 77 |
| WOMAC global* | 87 | 78 |
| UCLA activity score | 5.0 | 4.3 |
* Oxford hip score and the WOMAC scores are normalized to a range of 0 to 100 with 0 being the worst and 100 being the best.
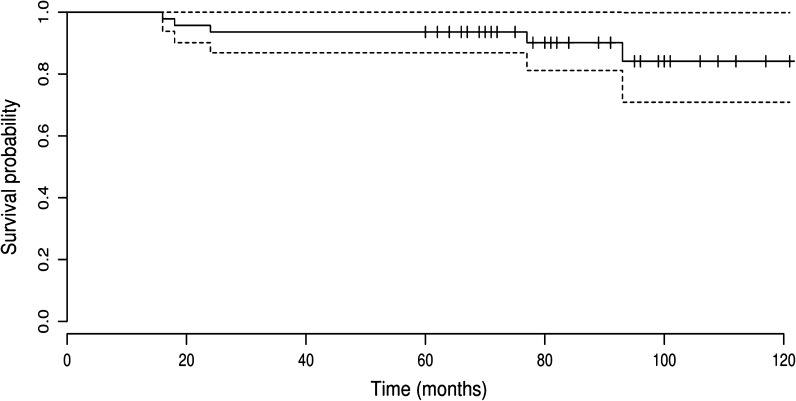
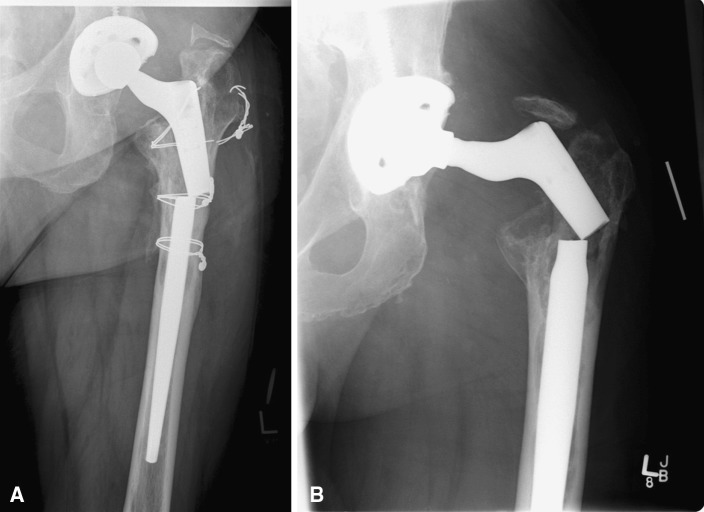
The cumulative 5-year survival rate with repeat femoral revision for any reason as the end point was 94% (95% CI, 87%–100%) and the cumulative 10-year survival rate was 84% (95% CI, 71%–99%) (Fig. 2). Five stems were revised, all for the same reason: fracture of the femoral component at the modular junction (Fig. 3). All of these fractures were in the standard ZMR® stem design for a total fracture rate of five of 27 (18.5%) (Table 4).
Fig. 2.
Kaplan-Meier survivorship curve. Survival rates at 5 and 10 years are 94% and 84%, respectively (95% CI).
Fig. 3A–B.
Preoperative AP pelvic radiographs showing a fractured standard ZMR® tapered modular revision stem in (A) a 64-year-old female patient and (B) a 65-year-old male patient.
Table 4.
Clinical and operative details for patients who sustained fracture of the femoral stem
| Case number | Age (years) | Sex | Paprosky defect | BMI (kg/m2) | Time to fracture (months) | ZMR type | ETO done? | Allograft strut used? | Stem length (mm) | Stem diameter (mm) | Femoral offset | Reconstruction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 65 | M | 3B | 39 | 77 | Std* | Yes | No | 185 | 16 | Ext† | Revitan TFMT |
| 2 | 64 | F | 3B | 35 | 93 | Std | Yes | No | 220 | 19 | Ext | Revitan TFMT |
| 3 | 70 | M | 3B | 30 | 24 | Std | Yes | Yes | 185 | 17 | Ext | Stryker GMRS |
| 4 | 58 | M | 3B | 35 | 16 | Std | Yes | No | 185 | 17 | Ext | Solution CNCC |
| 5 | 65 | M | 3B | 36 | 18 | Std | No | No | 185 | 20 | Ext | Solution CNCC |
* Standard tapered femoral stem; †extended femoral neck offset; BMI = body mass index; ETO = extended trochanteric osteotomy; M = male; F = female; TFMT = tapered, fluted, modular, titanium; CNCC = cylindrical, nonmodular, cobalt-chromium.
Eight patients sustained an intraoperative fracture (16%). All of these were managed with cable fixation. Previous studies have demonstrated the intraoperative fracture rates with CNCC stems can be more prevalent as compared with TFMT stems. Using the Solution stem (DePuy, Warsaw, IN, USA) for similar patients, we have previously reported an intraoperative fracture rate of 29 of 114 (25%) [32]. Five patients (10%) had at least one dislocation within 6 months of operation. All five patients were treated with acetabular revision to larger cup and femoral head sizes. One patient required revision to a constrained liner. For the eight patients who were revised for chronic periprosthetic infection, all of these patients received a two-stage revision. The first stage consisted of meticulous débridement of all the infected tissue with removal of infected implants and cement followed by implantation of a PROSTALAC® (DePuy) articulated antibiotic-loaded spacer. These patients then received intravenous antibiotic therapy for a minimum of 6 weeks followed by revision to the definitive THA using the TFMT stem. At the last followup, six of the eight patients (75%) had successful eradication of the infection. The remaining two patients are currently on long-term antibiotic suppression. There were no infections in the group of patients who did not have an infection before their revision surgery.
Discussion
CNCC fully porous-coated stems for revision femoral arthroplasty have shown long-term survival rates ranging from 89% to 98% [8, 10, 12, 16, 21, 24, 26, 28, 37]. However, Sporer and Paprosky [34] have raised concerns regarding the use of these stems in patients with severe proximal femoral bone loss. The mechanical failure rate of these CNCC stems in patients with Type 3B or 4 proximal femoral bone deficiencies was as high as 38%. In contrast, TFMT stems have shown to have good short-term functional results [9, 32] (Table 1). The literature is lacking midterm followup of these TFMT stems currently being used for revision hip arthroplasty. There seems to be concern over the potential long-term failure of these TFMT implants over time, especially dealing with the issue of implant fracture at the level of the modular junction [19, 27, 32]. In the context of poor proximal femoral bony support around the modular junction, these concerns seem to be further warranted. Thus, we attempted to address these gaps in the literature by reporting the clinical and radiographic outcomes after revision hip arthroplasty using TFMT stems in patients with severe proximal femoral bone defects.
Our study is associated with a number of limitations. First, we lacked preoperative QOL outcome scores. These are an important predictor of postoperative outcomes and absence of these is a potential confounder. Second, we had 17 patients lost to followup (10 patients lost to followup, seven patients died). This is somewhat anticipated given that the patients are typically at an advanced age at the time of the index operation and with longer followup, losing patients as a result of relocation or death is expected. Our lost to followup numbers are similar to other studies published in the literature regarding this topic [15, 18, 29, 38] (Table 1). Finally, the study was not randomized and we had no control group to compare or contrast outcomes.
Radiographic analysis revealed no cases of implant loosening. Early implant subsidence occurred in a limited number of patients but did not impact these patients’ QOL outcome scores. Eighty-eight percent of patients had either no change in their proximal femoral bone stock or demonstrated osseous restoration. This lack of severe stress shielding and even evidence of bone formation is consistent with similar studies involving radiographic followup of TFMT stems [15, 27, 32, 38] (Table 1).
We had no revisions for stem loosening or subsidence at a mean followup of 84 months. In comparison to series with fully porous-coated stems, we noted a unique complication in this series. There were five fractures of the modular junction, all in patients with the standard ZMR® design, and none in the ZMR®-XL, which was a reinforced junction. This 18.5% rate of fracture is unacceptable, and this particular stem design (ie, ZMR® Standard taper body design) is no longer in use. As has been previously reported [19], we noted that fracture of the modular junction was related to an increase in body mass index, small stem diameter, and the use of an extended trochanteric osteotomy for exposure. It is of interest to note that fracture of the stem can also occur in patients who receive a nonmodular distally fixed cobalt-chrome stem. In a study by Busch et al. [4], they noted a fracture rate of 2.3%. Risk factors for fracture included small stem diameter, use of an ETO, and poor proximal bone. In this article, we had five fractures in total and all occurred in patients with poor proximal femoral bone stock. Nevertheless, the fracture rate using the ZMR®-taper body stem (not the ZMR®-XL) was much higher at 18.5% and is unacceptable.
Lastly, our QOL measures were similar to those of previous studies performed by us [9, 32], despite the fact that these patients represent a cohort with more severe preoperative femoral bone defects and a longer followup interval (Table 2). This suggests the QOL outcome results are stable over time. In comparison to results from other centers, our results are similar to previous reported results [13, 18, 22] (Table 1).
Our data support the use of TFMT stems in cases with severe proximal femoral bone loss. We do not believe these results are generalizable to all stem types, because the stem used in this study has a 3.5° taper and many other stems have a 2° taper. This sharp taper may be responsible for the ability to secondarily stabilize in cases of early subsidence. If at all possible we continue to use this stem type in Paprosky 3B and 4 defects. However, we are concerned about fracture of the modular junction over time. For these reasons, we currently use a stronger junction in all cases in which a modular stem is used such as the ZMR®-XL modular revision hip. If the femur is not able to accommodate this junction as a result of the small size of the proximal femur, we favor a nonmodular tapered titanium stem in these cases as a result of the increased risk of fracture associated with the smaller stems and junctions.
Acknowledgments
We thank Daphné Savoy for her assistance in the preparation of the manuscript.
Footnotes
One of the authors (CPD) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of $10,000, from a commercial entity (Zimmer, Inc, Warsaw, IN, USA) related to this work. One of the authors (BAM) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of $10,000, from a commercial entity (Zimmer, Inc) related to this work. One of the authors (DSG) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of $10,000, from a commercial entity (Zimmer, Inc) related to this work. The institution of one or more the authors (APVH, CPD, BAM, NVG, DSG) has received funding from Zimmer Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 3.Bohm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revision followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;83:1023–1031. doi: 10.1302/0301-620X.83B7.11413. [DOI] [PubMed] [Google Scholar]
- 4.Busch CA, Charles MN, Haydon CM, Bourne RB, Rorabeck CH, MacDonald SJ, McCalden RW. Fractures of distally-fixed femoral stems after revision arthroplasty. J Bone Joint Surg Br. 2005;87:1333–1336. doi: 10.1302/0301-620X.87B10.16528. [DOI] [PubMed] [Google Scholar]
- 5.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190. [PubMed] [Google Scholar]
- 6.Della Valle CJ, Paprosky WG. Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J Bone Joint Surg Am. 2003;85:1–6. [DOI] [PubMed]
- 7.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 8.Engh CA, Jr, Ellis TJ, Koralewicz LM, McAuley JP, Engh CA., Sr Extensively porous-coated femoral revision for severe femoral bone loss: minimum 10-year follow-up. J Arthroplasty. 2002;17:955–960. doi: 10.1054/arth.2002.35794. [DOI] [PubMed] [Google Scholar]
- 9.Garbuz DS, Toms A, Masri BA, Duncan CP. Improved outcome in femoral revision arthroplasty with tapered fluted modular titanium stems. Clin Orthop Relat Res. 2006;453:199–202. doi: 10.1097/01.blo.0000238875.86519.cf. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Cimbrelo E, Garcia-Rey E, Cruz-Pardos A, Madero R. Stress-shielding of the proximal femur using an extensively porous-coated femoral component without allograft in revision surgery: a 5-to-17-year follow-up study. J Bone Joint Surg Br. 2010;92:1363–1369. doi: 10.1302/0301-620X.92B10.24317. [DOI] [PubMed] [Google Scholar]
- 11.Gozzard C, Blom A, Taylor A, Smith E, Learmonth I. A comparison of the reliability and validity of bone stock loss classification systems used for revision hip surgery. J Arthroplasty. 2003;18:638–642. doi: 10.1016/S0883-5403(03)00107-4. [DOI] [PubMed] [Google Scholar]
- 12.Hamilton WG, Cashen DV, Ho H, Hopper RH, Jr, Engh CA. Extensively porous-coated stems for femoral revision: a choice for all seasons. J Arthroplasty. 2007;22(Suppl 1):106–110. doi: 10.1016/j.arth.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Kang MN, Huddleston JI, Hwang K, Imrie S, Goodman SB. Early outcome of a modular femoral component in revision total hip arthroplasty. J Arthroplasty. 2008;23:220–225. doi: 10.1016/j.arth.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Katz JN, Phillips CB, Baron JA, Fossel AH, Mahomed NN, Barrett J, Lingard EA, Harris WH, Poss R, Lew RA, Guadagnoli E, Wright EA, Losina E. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003;48:560–569. doi: 10.1002/art.10754. [DOI] [PubMed] [Google Scholar]
- 15.Koster G, Walde TA, Willert HG. Five-to-10-year results using a noncemented modular revision stem without bone grafting. J Arthroplasty. 2008;23:964–970. doi: 10.1016/j.arth.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 16.Krishnamurthy AB, MacDonald SJ, Paprosky WG. 5-to-13-year follow-up study on cementless femoral components in revision surgery. J Arthroplasty. 1997;12:839–847. doi: 10.1016/S0883-5403(97)90152-2. [DOI] [PubMed] [Google Scholar]
- 17.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2-to-6-year follow-up study. J Arthroplasty. 2003;18(Suppl 1):94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 18.Lakstein D, Backstein D, Safir O, Kosashvilli Y, Gross AE. Revision total hip arthroplasty with a porous-coated modular stem: 5 to 10 years followup. Clin Orthop Relat Res. 2010;468:1310–1315. doi: 10.1007/s11999-009-0937-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lakstein D, Eliaz N, Levi O, Backstein D, Kosashvili Y, Safir O, Gross AE. Fracture of cementless femoral stems at the mid-stem junction in modular revision hip arthroplasty systems. J Bone Joint Surg Am. 2011;93:57–65. doi: 10.2106/JBJS.I.01589. [DOI] [PubMed] [Google Scholar]
- 20.Losina E, Plerhoples T, Fossel AH, Mahomed NN, Barrett J, Creel AH, Wright EA, Katz JN. Offering patients the opportunity to choose their hospital for total knee replacement: impact on satisfaction with the surgery. Arthritis Rheum. 2005;53:646–652. doi: 10.1002/art.21469. [DOI] [PubMed] [Google Scholar]
- 21.McAuley JP, Engh CA., Jr Femoral fixation in the face of considerable bone loss: cylindrical and extensively coated femoral components. Clin Orthop Relat Res. 2004;429:215–221. doi: 10.1097/01.blo.0000150274.21573.f4. [DOI] [PubMed] [Google Scholar]
- 22.McInnis DP, Horne G, Devane PA. Femoral revision with a fluted, tapered, modular stem seventy patients followed for a mean of 3.9 years. J Arthroplasty. 2006;21:372–380. doi: 10.1016/j.arth.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 23.Meek RM, Garbuz DS, Masri BA, Greidanus NV, Duncan CP. Intraoperative fracture of the femur in revision total hip arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am. 2004;86:480–485. doi: 10.2106/00004623-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Moreland JR, Bernstein ML. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin Orthop Relat Res. 1995;319:141–150. [PubMed] [Google Scholar]
- 25.Murphy SB, Rodriguez J. Revision total hip arthroplasty with proximal bone loss. J Arthroplasty. 2004;19(Suppl 1):115–119. doi: 10.1016/j.arth.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 26.Nadaud MC, Griffin WL, Fehring TK, Bohannon Mason J, Tabor OB, Jr, Odum S, Nussman DS. Cementless revision total hip arthroplasty without allograft in severe proximal femoral defects. J Arthroplasty. 2005;20:738–744. doi: 10.1016/j.arth.2004.12.053. [DOI] [PubMed] [Google Scholar]
- 27.Ovesen O, Emmeluth C, Hofbauer C, Overgaard S. Revision total hip arthroplasty using a modular tapered stem with distal fixation: good short-term results in 125 revisions. J Arthroplasty. 2010;25:348–354. doi: 10.1016/j.arth.2008.11.106. [DOI] [PubMed] [Google Scholar]
- 28.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 29.Park MS, Lee JH, Park JH, Ham DH, Rhee YK. A distal fluted, proximal modular femoral prosthesis in revision hip arthroplasty. J Arthroplasty. 2010;25:932–938. doi: 10.1016/j.arth.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 30.Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty. 2007;22:993–999. doi: 10.1016/j.arth.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 31.Restrepo C, Mashadi M, Parvizi J, Austin MS, Hozack WJ. Modular femoral stems for revision total hip arthroplasty. Clin Orthop Relat Res. 2011;469:476–482. doi: 10.1007/s11999-010-1561-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richards CJ, Duncan CP, Masri BA, Garbuz DS. Femoral revision hip arthroplasty: a comparison of two stem designs. Clin Orthop Relat Res. 2010;468:491–496. doi: 10.1007/s11999-009-1145-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rodriguez JA, Fada R, Murphy SB, Rasquinha VJ, Ranawat CS. Two-year to five-year follow-up of femoral defects in femoral revision treated with the Link MP modular stem. J Arthroplasty. 2009;24:751–758. doi: 10.1016/j.arth.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Sporer SM, Paprosky WG. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;417:203–209. doi: 10.1097/01.blo.0000096803.78689.0c. [DOI] [PubMed] [Google Scholar]
- 35.Sporer SM, Paprosky WG. Femoral fixation in the face of considerable bone loss: the use of modular stems. Clin Orthop Relat Res. 2004;429:227–231. doi: 10.1097/01.blo.0000150120.80409.0d. [DOI] [PubMed] [Google Scholar]
- 36.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17(Suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 38.Weiss RJ, Beckman MO, Enocson A, Schmalholz A, Stark A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty. 2011;26:16–23. doi: 10.1016/j.arth.2009.11.009. [DOI] [PubMed] [Google Scholar]