Abstract
Background
When considering arthroscopic surgery for treatment of hip pain, it is important to understand the influence of joint degeneration on the likelihood of success. Previous research has shown poorer outcomes among patients with osteoarthritis but new arthroscopic techniques including femoroacetabular impingement correction and microfracture may lead to better arthroscopic outcomes.
Questions/Purposes
We investigated the effect of intraarthroscopic articular and rim cartilage degeneration on the outcome after hip arthroscopy using contemporary techniques.
Methods
The modified Harris hip score (MHHS) and nonarthritic hip score (NAHS) were completed preoperatively and 12 months postoperatively by 560 patients undergoing hip arthroscopy after March 2007. Change in these scores was compared between patients with and without acetabular or femoral articular cartilage degeneration and between patients with and without rim cartilage degeneration. Correlation and regression analyses were used to predict the change in outcome scores based on the severity of cartilage degeneration.
Results
Hips without degeneration had greater improvement in the outcome scores. The presence of cartilage degeneration showed negative correlations with change in outcomes. The best model to explain change in MHHS included preoperative score, articular cartilage degeneration grade, and rim lesion grade (adjusted R2 = 0.24).
Conclusions
Our data support previous findings regarding the negative influence of cartilage degeneration on improvement after hip arthroscopy. Nevertheless, many patients with cartilage degeneration still improved and the severity of degeneration accounts for little of the resulting variance in change. Future studies must determine the clinical importance of the improvements gained by patients with cartilage degeneration and identify other predictors of outcome.
Level of Evidence
Level III, prognostic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Minimally invasive surgical intervention (arthroscopy) is increasingly used in the assessment and treatment of hip and groin pain. In Australia in 2011, the Australian government-funded healthcare service (Medicare) provided full or part funding for 2974 hip arthroscopies in private hospitals [5]. Many more were performed in public hospitals or were funded from other sources. The number of Medicare-funded hip arthroscopies has been growing by an average of 24% each year for the past decade [5]. A large number of patients undergoing hip arthroscopy have degenerative changes attributable to osteoarthritis (OA) in the joint. For example, 63% of a cohort of patients treated with arthroscopy was found to have acetabular articular cartilage lesions [17], and 88% of patients who did not have significant OA observed on preoperative radiographs before having arthroscopic femoroacetabular impingement (FAI) correction had intraoperative acetabular cartilage lesions [14]. Cartilage degeneration can occur at both articular surfaces of the femur and acetabulum and also the acetabular rim cartilage or labrum. Rim cartilage degeneration is considered to be part of an early arthritic process [23], with severe rim cartilage lesions consistent with a diagnosis of OA. Arthroscopy primarily for treatment of hip OA, or for treatment of other causes when articular or rim cartilage degeneration is present in the joint, remains contentious, and further information regarding postsurgical prognosis may assist surgeons in choosing the most appropriate procedures for patients with hip OA and/or rim cartilage degeneration.
Previous research has shown degeneration of the femoral and/or acetabular articular cartilage is related to relatively poorer clinical outcome after arthroscopy [6, 20], and rim lesions (in particular full-thickness wear) may lead to reduced benefit from arthroscopic procedures [11]. The findings have led to the use of hip arthroscopy generally being supported in cases where OA is mild to moderate [13, 17, 22], whereas severe OA has been seen as a contraindication [3, 14, 16]. Arthroscopic surgical techniques and instrumentation have undergone major changes during the past decade. Techniques such as femoral osteochondroplasty to correct cam-type FAI (asymmetric femoral head and neck relationship), labral repair and reconstruction, and microfracture have been developed. These techniques have required the development of novel instrumentation. Accordingly, reevaluation of clinical outcomes after hip arthroscopy in light of recent surgical advances is needed to determine the impact of the presence of cartilage degeneration when current hip arthroscopic techniques, including FAI correction and microfracture, are used.
We therefore determined whether arthroscopic evidence of cartilage degeneration (articular cartilage or rim cartilage degeneration) influenced the improvement gained at 12 months after contemporary hip arthroscopy. We hypothesized the presence of intraoperative articular cartilage or rim cartilage degeneration would lead to less improvement in self-reported functioning. To better understand the magnitude of the influence of cartilage degeneration on self-reported functioning, secondary analyses investigated (1) whether there is an association between the patient-perceived change in function and the degree of cartilage (articular and rim) degeneration found intraoperatively and (2) the proportion of the variation in change in function explained by the degeneration.
Patients and Methods
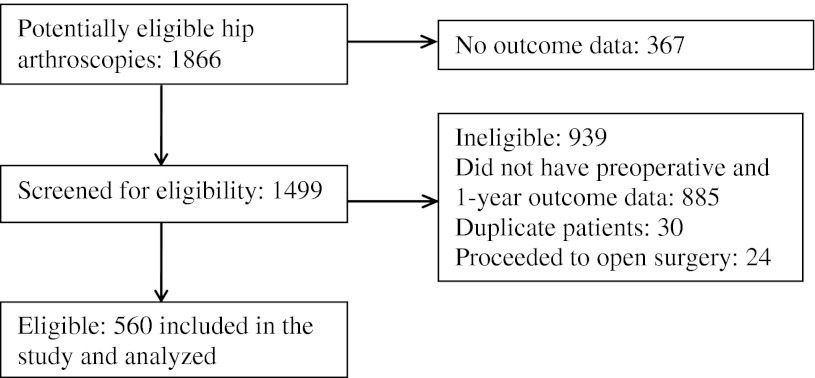
This was a retrospective cohort study that used data from consecutive patients who underwent hip arthroscopy by one of us (JO) in Melbourne, Australia (Mercy Private and Bellbird Private Hospitals) between March 2007 and May 2010. Of the 1866 patients, 67% did not have preoperative and 12-month outcome data and therefore were unable to be included in the analysis (Fig. 1). For patients who had more than one hip arthroscopy during the inclusion period (duplicate patients), only outcomes pertaining to the latter surgery were included in the analysis. Patients who were converted to having open surgery during the arthroscopic procedure also were excluded. Patients with previous ipsilateral or contralateral hip arthroscopy were not excluded. We included 560 patients with a mean age of 41.5 years in the analysis (Table 1). All patients gave written consent for their data to be used for research purposes and the study was approved by The University of Melbourne Human Research Ethics Committee.
Fig. 1.
A flowchart shows selection of study participants. Duplicate patients are those who had two or more hip arthroscopies during the inclusion period. Only outcomes from the latter surgery were included.
Table 1.
Descriptive characteristics of the cohort grouped by presence of intraoperative osteoarthritis* and rim cartilage degeneration**
| Characteristic | All patients | Osteoarthritis† | Rim cartilage degeneration‡ | ||
|---|---|---|---|---|---|
| No | Yes | No | Yes | ||
| Number of patients | 560 | 449 (81%) | 108 (19%) | 275 (49%) | 283 (51%) |
| Age at surgery (years)§ | 41.5 (15.1) | 38.7 (14.9) | 52.5 (10.1) | 39.3 (16.5) | 43.7 (13.3) |
| Male | 283 (51%) | 222 (49%) | 58 (54%) | 85 (31%) | 197 (70%) |
| Surgically treated hip, left | 256 (46%) | 208 (46%) | 47 (44%) | 125 (46%) | 129 (46%) |
| Synovitis greater than 25% (moderate or severe) | 242 (44%) | 149 (34%) | 91 (88%) | 66 (24%) | 176 (64%) |
| Ligamentum teres lesion (partial or complete rupture) | 190 (34%) | 140 (31%) | 48 (44%) | 103 (38%) | 87 (31%) |
| Labral disorder (mostly labral tears) | 136 (24%) | 103 (23%) | 33 (31%) | 82 (30%) | 54 (19%) |
* Articular cartilage degeneration ≥ Grade 1; **rim lesion ≥ Grade 3; †three patients are missing osteoarthritis grade; ‡two patients are missing rim lesion grade; §values are expressed as mean, with SD in parentheses; the remaining values are expressed as number of patients, with percentage in parentheses.
The indication for hip arthroscopy was hip pain accompanied by mechanical symptoms that were not responsive to nonoperative treatment (eg, NSAIDs, intraarticular joint injections, and/or physiotherapy) for at least 12 weeks. All patients also had painful ROM on physical examination, specifically, a positive impingement test (pain provoked by flexion, adduction, and internal rotation movement). Patients with Tönnis Grade 1 or 0 OA were recommended arthroscopy and those with Tönnis Grade 3 OA were offered arthroplasty. Patients with Tönnis Grade 2 OA were offered arthroplasty if symptoms warranted; otherwise, they were offered arthroscopy. Almost all patients offered arthroscopy elected to have arthroscopy. The arthroscopy technique used a lateral decubitus position, general anesthesia (without muscle relaxants), and traction for the surgically treated hip [15], and all surgeries were performed by the same experienced surgeon (JO). Surgical procedures consisted of femoral ostectomy with capsular release (61%), ligamentum teres débridement (22%), acetabular ostectomy (21%), labral repair (13%), gluteus medius decompression or repair (11%), microfracture (for localized acetabular lesions less than 3–4 cm2 [4]) (14%), and bursectomy (6%). Other techniques used rarely (2% or less) included removal of loose bodies, synovectomy, avascular necrosis débridement, and extraarticular procedures such as psoas tenotomy. The specific surgical techniques used for ostectomy of cam-type FAI (asymmetric femoral head and neck relationship) and treatment of acetabular labral tears have been reported [10, 11]. At the end of the surgical procedure, the joint was lavaged and injected with local anesthetic (ropivacaine [150 mg]) and morphine (5 mg). Betamethasone (11.4 mg) also was injected if there had not been any bone resection.
Postoperatively, patients were advised to weightbear as tolerated with the aid of crutches for a few days and to avoid hip flexion beyond 90°. The patients also were referred to a formal physiotherapy program; however, data regarding participation in this service are unavailable.
The presence and degree of articular cartilage and rim cartilage degeneration were scored during arthroscopy. The observed area and thickness of articular cartilage loss were graded as follows: Grade 0 = no degeneration; Grade 1 = localized articular cartilage loss (partial-thickness acetabulum); Grade 2 = partial-thickness loss at the acetabulum and femoral head (< 30% of the acetabular anterior wall width involved, with full-thickness articular cartilage loss); Grade 3 = full-thickness acetabulum (> 30%) and partial-thickness femoral head; and Grade 4 = full-thickness loss on both surfaces [9]. This grading system was based on the early Outerbridge system for grading patellofemoral degeneration [19]. Grades 1 and higher were classified as OA for the purpose of the primary analysis. Acetabular rim cartilage lesions were classified as follows: Grade 0 = no abnormality; Grade 1 = acetabular edge softening; Grade 2 = labral separation; Grade 3 = full-thickness loss of articular cartilage with a maximum width less than 30% of the distance from the acetabular edge to the fovea; Grade 4 = full-thickness loss of articular cartilage greater than 30%; and Grade 5 = loss of articular cartilage from the femoral head and acetabular rim [11]. Grades 3 and higher were classified as rim cartilage degeneration for the purpose of the primary analysis.
Nineteen percent of patients (n = 108) had intraoperative articular cartilage degeneration of Grade 1 or higher: Grade 1 (two patients, 0.4%), Grade 2 (16 patients, 3%), Grade 3 (39 patients, 7%), and Grade 4 (51 patients, 9%). Fifty-one percent of patients (n = 283) had Grade 3 or higher rim cartilage degeneration: Grade 0 (146 patients, 26%), Grade 1 (46 patients, 8%), Grade 2 (83 patients, 15%), Grade 3 (157 patients, 28%), Grade 4 (40 patients, 7%), and Grade 5 (86 patients, 15%).
Other features also graded intraoperatively for descriptive purposes included synovitis (Grade 0 = no synovitis; Grade 1 = mild [< 25%]; Grade 2 = moderate [25%–50%]; or Grade 3 = severe [> 50%]) and ligamentum teres lesions (partial or complete rupture [7]).
Patients routinely were asked to complete two questionnaires preoperatively and 12 months postoperatively to determine change in clinical status. These questionnaires included the modified Harris hip score (MHHS) and the nonarthritic hip score (NAHS). The MHHS is a condition-specific outcome instrument that has been used widely after hip arthroscopy [8]. The eight questions measure domains of pain, gait function, and functional activities. The scale has high construct validity [21, 24]. Scores range from 0 (poor) to 100.1 (ideal). The NAHS is a validated, self-administered questionnaire designed to assess nonarthritic hip pain in patients with high activity demands and expectations [2]. Domains of pain and other symptoms, function, and sporting activities are measured with 20 questions. Scores range from 0 (poor) to 100 (ideal). It has high content validity [2] and fair internal consistency, construct validity, and reproducibility [24].
We evaluated the kurtosis and skewness of the distribution of our outcome data. In addition, we performed a Shapiro-Wilks test for normality and as most data were normally distributed we used parametric tests. Independent t-test on the change scores (calculated as 12-month scores minus preoperative scores) were used for each outcome measure to compare patients with and without articular cartilage degeneration (≥ Grade 1) and patients with and without rim cartilage degeneration (≥ Grade 3). Paired t-tests were used to compare preoperative scores with 12-month scores in the subgroup of moderate/severe (Grade 3 or 4) OA. Spearman’s rho correlations were performed to assess relationships between grade of articular cartilage degeneration and grade of rim lesion and change in each outcome measure after 12 months. Stepwise multiple linear regression analyses were performed with change in outcome score as the dependent variable and grades of articular cartilage degeneration and rim lesion, age, sex, and preoperative outcome score as the independent variables. The stepwise method used F-value significance of p = 0.05 for entry and p = 0.1 for removal. We used SPSS® Statistics 19 (IBM Corp, Armonk, NY, USA) for statistical analyses, and significance level was set at p = 0.05.
Results
For the MHHS and NAHS, we found differences in change from preoperative to 12 months between patients with and without articular cartilage degeneration of Grade 1 or higher and between patients with and without rim cartilage degeneration of Grade 3 or higher (Table 2). The mean difference (standard error) in change between patients with and without articular cartilage degeneration was 7 (2) for the MHHS and 7 (2) for the NAHS, favoring patients without degeneration. The mean difference in change between patients with and without rim cartilage degeneration was 9 (2) for the MHHS and 8 (2) for the NAHS, again favoring patients without degeneration. All p values were 0.001 or less.
Table 2.
Changes in outcome scores 12 months after surgery
| Score | All patients (n = 560) | Osteoarthritis* | Rim cartilage degeneration† | ||
|---|---|---|---|---|---|
| No (n = 449) | Yes (n = 108) | No (n = 275) | Yes (n = 283) | ||
| MHHS | |||||
| Preoperative‡ | 67.3 (16.1) | 68.6 (16.6) | 61.5 (12.6) | 66.3 (15.9) | 68.3 (16.3) |
| 12 months‡ | 80.7 (18.6) | 83.4 (17.6) | 69.6 (18.3) | 84.1 (17.4) | 77.5 (19.1) |
| Change‡,§ | 13.5 (18.3) | 14.8 (18.1) | 8.1 (18.2) | 17.7 (17.5) | 9.2 (18.1) |
| Difference between groups‖ | 6.8 (0.001, 2.9–10.6) | 7.0 (0.000, 5.5–11.4) | |||
| NAHS | |||||
| Preoperative‡ | 66.4 (17.6) | 67.4 (17.9) | 61.8 (15.8) | 65.2 (18.2) | 67.8 (16.9) |
| 12 months‡ | 80.0 (18.7) | 82.6 (17.5) | 69.0 (19.2) | 82.9 (17.4) | 77.2 (19.5) |
| Change‡,§ | 13.4 (18.2) | 14.9 (17.4) | 7.9 (20.2) | 17.4 (17.1) | 9.6 (18.4) |
| Difference between groups‖ | 8.5 (0.000, 3.1–10.9) | 7.9 (0.000, 4.9–10.9) | |||
* According to presence of intraoperative osteoarthritis (articular cartilage degeneration C Grade 1); †rim cartilage degeneration (rim lesion C Grade 3); *three patients are missing osteoarthritis grade; †two patients are missing rim lesion grade; ‡values are expressed as mean, with SD in parentheses; §change = 12-month score – preoperative score; ‖values are expressed as mean, with p value and 95% CI in parentheses; MHHS = modified Harris hip score; scores range from 0 to 100.1, with higher scores indicating optimal outcome; NAHS = nonarthritic hip score; scores range from 0 to 100, with higher scores indicating optimal outcome.
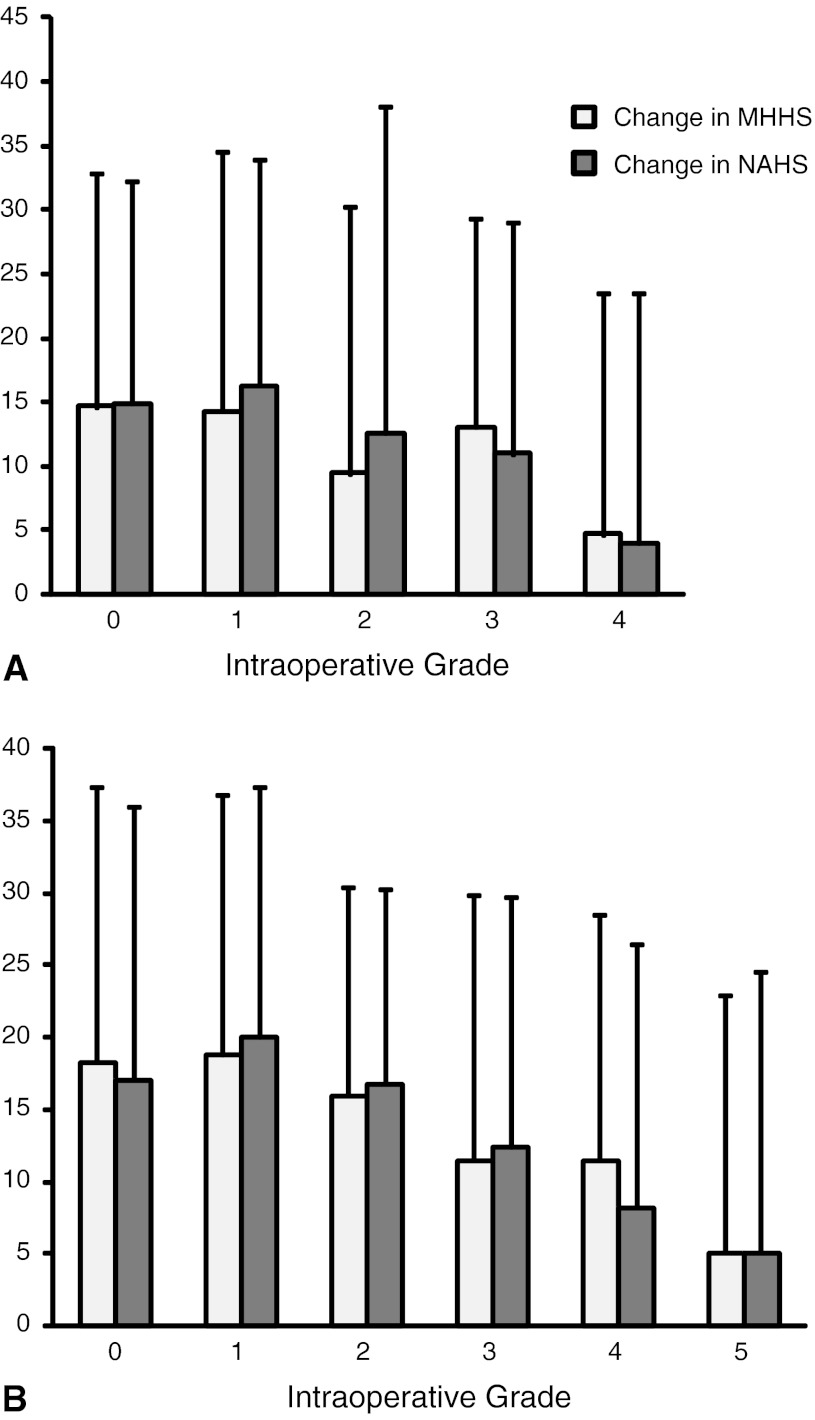
Fifty-five percent of patients with Grade 4 articular cartilage degeneration reported higher MHHS scores at followup than preoperatively, whereas 59% reported higher NAHS scores. Similarly, 74% and 62% of patients with Grade 3 articular cartilage degeneration reported higher scores a year after surgery for the MHHS and NAHS, respectively. The changes in clinical outcome across each grade of articular cartilage degeneration and rim lesion are shown (Fig. 2). The subgroup of patients with either Grade 3 or 4 intraoperative articular cartilage degeneration improved as a group 12 months after surgery with a mean 8-point improvement (SD, 18 points; 95% CI, 4–11 points; p < 0.001) in the MHHS and mean 7-point improvement (SD, 19 points; 95% CI, 3–11 points; p = 0.002) in the NAHS. Patients with at least Grade 3 rim lesions also showed improvement as a group after 12 months with a mean 9-point improvement (SD, 18 points; 95% CI, 7–11 points; p < 0.001) in the MHHS and mean 10-point improvement (SD, 18 points; 95% CI, 7–12 points; p < 0.001) in the NAHS.
Fig. 2A–B.
The mean (SD) change in the MHHS and the NAHS after 12 months for each grade of (A) articular cartilage degeneration and (B) rim cartilage degeneration are shown. MHHS = modified Harris hip score; NAHS = nonarthritic hip score.
Articular and rim cartilage degeneration showed small but significant negative correlations with changes in outcome at 12 months. Spearman’s rho correlations for grade of articular cartilage degeneration was r = −0.15 (p = 0.001) for the MHHS and r = −0.14 (p = 0.001) for the NAHS. Spearman’s rho correlations for grade of rim lesion was r = −0.24 (p < 0.001) for the MHHS and r = −0.21 (p < 0.001) for the NAHS. Preoperative scores were found to be moderately negatively correlated with the change scores: r = −0.42 (p < 0.001) for the MHHS and r = −0.46 (p < 0.001) for the NAHS. Age and sex were not correlated with change in scores.
The final regression model to best explain the change in the MHHS at 12 months included preoperative MHHS score (β2 = 0.19), grade of articular cartilage degeneration (β2 = 0.02), and grade of rim lesion (β2 = 0.02). The model explained 24% of the variance in scores (adjusted R2 = 0.24). Change in the NAHS was best explained by preoperative NAHS score (β2 = 0.25), grade of articular cartilage degeneration (β2 = 0.02), age (β2 = 0.01), and grade of rim lesion (β2 = 0.01), with the model accounting for 27% of the variance (adjusted R2 = 0.27).
Discussion
To better understand the influence of cartilage degeneration on patient-perceived clinical outcome after arthroscopy for hip pain, we evaluated in this cross-sectional study whether evidence of intraoperative cartilage degeneration predicted change in self-reported function scores 12 months postoperatively.
The study was well powered for the analyses, used patient-reported outcomes, considered change in scores rather than postoperative values, and analyzed data from more contemporary arthroscopic procedures than some previous reports [6, 11, 20]. However, there are several limitations that must be considered. First, only 30% of the patients who had hip arthroscopy during the inclusion period were included in the analyses. It is possible the 560 patients included in this study were not a random sample and they may have differed from the total patient cohort regarding some important characteristic(s) likely to influence outcome. The demographics of the sample, however, were consistent with the demographics of the total cohort; for example, total cohort mean (SD) age was 40 years (15 years) and 18% had arthroscopic articular cartilage degeneration. In this study, arthroscopy was performed by only one surgeon and therefore the findings may not be generalizable to patients undergoing arthroscopy with other surgeons. The data cannot be used to determine the effectiveness of hip arthroscopy, which would require a randomized controlled trial. Finally, the 12-month followup is relatively short, and it will take time before the long-term outcomes from contemporary surgical interventions are known.
Our results showed articular and rim cartilage degeneration reduced the amount of improvement reported a year after surgery; that is, patients with worse intraoperative cartilage degeneration (either articular or rim) had less improvement in MHHS and NAHS scores after arthroscopy than patients without degeneration. However, the subgroups of patients with articular or rim cartilage degeneration, and even the subgroup of patients with moderate to severe articular cartilage degeneration, all showed improvement from their presurgical levels. The minimal clinically important difference (MCID) for the NAHS and MHHS are presently unknown. Thus, it is difficult to interpret whether the changes we observed are clinically meaningful.
The correlation and regression analyses also showed articular cartilage degeneration severity and rim lesion severity had negative influences on outcome. Articular and rim cartilage degeneration were predictive of change in outcome independent of age, sex, and preoperative score for the outcome measure. However, the relationships were small, explaining only 1% to 2% of the variance in change.
The findings of our analysis of outcomes after contemporary arthroscopy are largely in concordance with previous case series [6, 10, 18]. Degree of intraoperative cartilage lesions plus degree of synovitis were found to have a negative influence on clinical outcome, together explaining 17% of variance in postoperative scores in a group of patients receiving arthroscopic treatment for acetabular labral tears [10]. Meftah et al. [18] and Farjo et al. [6] found radiographic OA and arthroscopically determined femoral and acetabular cartilage degeneration correlated with postoperative self-reported symptoms and function among patients who underwent labral débridement (R2 = 0.31) or repair of tears, respectively.
Studies on outcomes after arthroscopic correction of FAI have found negative influences of OA on postoperative outcomes [14, 20, 21]. Preoperative radiographic joint space narrowing, together with preoperative MHHS score, and labral débridement or repair, predicted 35% of postoperative MHHS [20], and generalized severe cartilage lesions intraoperatively led to high rates of arthroplasty within 3 years of arthroscopy [12]. Increasing preoperative joint space narrowing has been shown to be an independent predictor for poorer outcome with respect to postoperative MHHS scores and undergoing arthroplasty in a recent cohort undergoing arthroscopy for FAI [14].
The main differences with the current study are the inclusion of all arthroscopies rather than only labral or FAI correction procedures and the use of change in scores as the dependent variable rather than postoperative score. Given that patients with greater OA changes tend to have lower preoperative scores and patients with lower preoperative scores tend to have lower postoperative scores [20], analyzing factors predictive of postoperative score may overlook the benefit that can be gained by patients with OA. Our finding, and that of Byrd and Jones [1], that preoperative scores are negatively associated with change in scores shows patients with lower starting scores can make the greatest improvements.
Some previous studies fail to report actual magnitudes of associations between OA changes and outcomes [1, 6]. We showed, despite associations, articular and rim cartilage degeneration explain little of the outcome. Age and sex also are not predictive of change in outcome after arthroscopy. Some of the previous studies also found no associations between age or sex and postoperative score [1, 6, 18, 20]. Age is related to OA incidence and severity and therefore would be expected to be associated with outcome if OA was an important factor in response to the intervention.
With only a total of 24% to 27% of the variance in outcome explained by our predictive models, there obviously are other factors influencing much of the variation in clinical outcome at 12 months. These may include patient characteristics such as motivation and other psychologic factors, physical activity levels, nature and extent of other soft tissue problems, type and intensity of rehabilitation, and measurement error. Preoperative score was the strongest factor associated with change found in our analysis such that lower preoperative scores were predictive of greater improvement.
Despite degree of OA being inversely related to amount of improvement, our data also showed patients with moderate to severe articular cartilage degeneration or rim lesions had improved outcome scores 12 months after surgery. The clinical significance of these changes of 8 or 9 points in the MHHS, respectively, or 7 or 10 points in the NAHS, respectively, is not known. There currently are no published data on minimal clinically important change for either measure. However Harris’ original scheme for the MHHS (90–100 = excellent; 80–90 = good; 70–80 = fair; < 70 = poor), indicates a 10-point change may be clinically important [8]. On this basis, the differences between the groups (with versus without cartilage degeneration) or the improvements gained by the moderate and severe OA subgroups may not be large enough to be clinically worthwhile. Minimal clinically important change needs to be determined more accurately before conclusions regarding clinical importance can be drawn.
The value of arthroscopic techniques for primary symptoms and/or prevention of OA remains unclear. Randomized controlled trials to evaluate efficacy are needed, particularly targeting patients with presentations where there remains uncertainty of efficacy such as for patients with articular or rim cartilage degeneration. However, our results provide preliminary support for the benefits of hip arthroscopy even in patients with more severe OA.
Acknowledgments
We thank Jess O’Donnell BA, BComm, for assisting with extraction of data from the database for this study.
Footnotes
One of the authors (JO) certifies that he has or may receive payments or benefits, during the study period, an amount of $10,000 to $100,000, from Smith & Nephew Inc (Memphis, TN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at The University of Melbourne, Carlton, VIC, Australia.
References
- 1.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 2.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75–83. doi: 10.1097/00003086-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Clohisy JC, Wright RW. Hip arthroscopy in the treatment of osteoarthritis. Oper Tech Sports Med. 2002;10:219–223. doi: 10.1053/otsm.2002.35877. [DOI] [Google Scholar]
- 4.Crawford K, Philippon MJ, Sekiya JK, Rodkey WG, Steadman JR. Microfracture of the hip in athletes. Clin Sports Med. 2006;25:327–335, x. [DOI] [PubMed]
- 5.Department of Human Services. Medicare. Available at: http://www.medicareaustralia.gov.au/. Accessed March 9, 2012.
- 6.Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15:132–137. doi: 10.1053/ar.1999.v15.015013. [DOI] [PubMed] [Google Scholar]
- 7.Gray AJ, Villar RN. The ligamentum teres of the hip: an arthroscopic classification of its pathology. Arthroscopy. 1997;13:575–578. doi: 10.1016/S0749-8063(97)90182-1. [DOI] [PubMed] [Google Scholar]
- 8.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 9.Haviv B, O’Donnell J. The incidence of total hip arthroplasty after hip arthroscopy in osteoarthritic patients. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:18. doi: 10.1186/1758-2555-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haviv B, O’Donnell J. Arthroscopic treatment for acetabular labral tears of the hip without bony dysmorphism. Am J Sports Med. 2011;39(suppl):79S–84S. doi: 10.1177/0363546511412915. [DOI] [PubMed] [Google Scholar]
- 11.Haviv B, Singh PJ, Takla A, O’Donnell J. Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J Bone Joint Surg Br. 2010;92:629–633. doi: 10.1302/0301-620X.92B5.23667. [DOI] [PubMed] [Google Scholar]
- 12.Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoral acetabular impingement in patients with preoperative generalized degenerative changes. Arthroscopy. 2010;26:623–629. doi: 10.1016/j.arthro.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Kelly BT, Williams RJ, 3rd, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 14.Larson CM, Giveans MR, Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res. 2011;469:1667–1676. doi: 10.1007/s11999-010-1741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mason JB, McCarthy JC, O’Donnell J, Barsoum W, Mayor MB, Busconi BD, Krebs VE, Owens BD. Hip arthroscopy: surgical approach, positioning, and distraction. Clin Orthop Relat Res. 2003;406:29–37. doi: 10.1097/00003086-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 16.McCarthy JC. Hip arthroscopy: when it is and when it is not indicated. Instr Course Lect. 2004;53:615–621. [PubMed] [Google Scholar]
- 17.McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The watershed labral lesion: its relationship to early arthritis of the hip. J Arthroplasty. 2001;16(8 suppl 1):81–87. doi: 10.1054/arth.2001.28370. [DOI] [PubMed] [Google Scholar]
- 18.Meftah M, Rodriguez JA, Panagopoulos G, Alexiades MM. Long-term results of arthroscopic labral debridement: predictors of outcomes. Orthopedics. 2011;34:e588–e592. doi: 10.3928/01477447-20110826-04. [DOI] [PubMed] [Google Scholar]
- 19.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 20.Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 21.Potter BK, Freedman BA, Andersen RC, Bojescul JA, Kuklo TR, Murphy KP. Correlation of Short Form-36 and disability status with outcomes of arthroscopic acetabular labral debridement. Am J Sports Med. 2005;33:864–870. doi: 10.1177/0363546504270567. [DOI] [PubMed] [Google Scholar]
- 22.Richmond J, Hunter D, Irrgang J, Jones MH, Levy B, Marx R, Snyder-Mackler L, Watters WC, 3rd, Haralson RH, 3rd, Turkelson CM, Wies JL, Boyer KM, St Andre J, McGowan R, American Academy of Orthopaedic Surgeons Treatment of osteoarthritis of the knee (nonarthroplasty) J Am Acad Orthop Surg. 2009;17:591–600. doi: 10.5435/00124635-200909000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH., Jr Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232–240. doi: 10.1097/00003086-200101000-00031. [DOI] [PubMed] [Google Scholar]
- 24.Tijssen M, van Cingel R, van Melick N, de Visser E. Patient-Reported Outcome questionnaires for hip arthroscopy: a systematic review of the psychometric evidence. BMC Musculoskelet Disord. 2011;12:117. doi: 10.1186/1471-2474-12-117. [DOI] [PMC free article] [PubMed] [Google Scholar]