Abstract
Background
The issue of rising costs will likely dominate the healthcare debate in the forthcoming years.
Questions/Purposes
We assessed factors including surgeon volume that were associated with lower hospital costs and variations in surgical treatment for proximal humeral fractures.
Methods
We used national databases for 2001 to 2008 to extract information on 25,731 patients undergoing surgery for proximal humeral fractures. We calculated hospital cost by converting hospital charges based on the hospital accounting reports collected by the Centers for Medicare & Medicaid Services.
Results
In a multivariate linear regression analysis, higher surgeon volume, open reduction and internal fixation (versus hemiarthroplasty), and lower burden of comorbidities were associated with lower hospital cost. Higher surgeon volume was linearly associated with lower hospital costs such that, on average, adjusting for all other factors, a surgeon performing 20 shoulder arthroplasties per year saves a hospital approximately US $1800 per surgery. Factors associated with higher utilization of hemiarthroplasty included high surgeon volume (odds ratio [OR] = 1.46; 95% CI = 1.43, 1.97; as compared with low surgeon volume) and earlier years of our study period (OR = 0.61; 95% CI = 0.56, 0.66; for hemiarthroplasty in 2007–2008 versus 2001–2002).
Conclusions
Higher surgeon volume was associated with lower hospital costs for proximal humeral fractures. Therefore, policies on minimum volume requirements by hospitals may result in substantial cost savings. There is provider-based practice variation in the surgical treatment of proximal humeral fractures and evidence-based guidelines in this area are needed.
Level of Evidence
Level III, economic analysis. See Instructions for Authors for a complete description of levels of evidence.
Introduction
The issue of rising healthcare costs will likely dominate the healthcare debate in the forthcoming years [34, 44]. It is possible that limited resources in the future may necessitate cost-cutting measures, as is already the case in several healthcare settings. Musculoskeletal care and orthopaedic procedures are major cost drivers for payers and hospitals [5]. Hospitals often operate at small margins. Therefore, an analysis of factors that determine higher hospital costs is valuable and may result in cost savings.
In the emerging value-based healthcare environment, data on comparative effectiveness of surgical procedures will become increasingly salient for reimbursement purposes [13, 20, 29, 35, 43]. This was highlighted in the 2009 Institute of Medicine report [21] and was an emphasis of the American Recovery and Reinvestment Act [13]. Does operative intervention lead to better outcomes as compared with nonoperative treatment? Are outcomes improved with advanced and often more expensive surgical interventions? These questions are addressed using comparative effectiveness methods. Unfortunately, these questions often are addressed based on the expertise and opinion of the treating surgeon in orthopaedic care. This is especially true when applied to scenarios where the role or ability of a patient to make an informed decision is compromised owing to the emergent nature of the issue, such as in some cases of proximal humeral fractures. A previous study showed, using data from 1990 through 2000, there are racial differences in types of surgical procedures used for treatment of proximal humeral fractures [23].
Proximal humeral fractures account for 10% of all fractures in the elderly and result in substantial healthcare resource utilization [8]. In the absence of evidence-based practice guidelines on surgical treatment of proximal humeral fractures, a study of the comparative effectiveness of hemiarthroplasty and open reduction and internal fixation (ORIF) would provide useful data. Before designing such a study, it is essential to determine current practice patterns across provider and patient characteristics. If practice patterns vary, it also would be helpful to understand the factors that most contribute to this variation.
Our aims in performing this study were to assess the current clinical practice in the surgical treatment of proximal humeral fractures across the United States. We also analyzed factors associated with hospital costs for ORIF and hemiarthroplasty in the treatment of proximal humeral fractures. Specifically, we assessed whether age, surgeon volume, hospital teaching status and location, and location of fracture were associated with whether ORIF or hemiarthroplasty was performed. We assessed surgical outcomes by surgeon volume. Finally, we studied the association of hospital cost with surgeon volume, patient sex and age, procedure performed, comorbidities, and payer.
Materials and Methods
We used the Nationwide Inpatient Sample (NIS) databases for 2001 through 2008. The NIS is managed by the Healthcare Cost and Utilization Project, that is made possible by a Federal-State-Industry partnership sponsored by the Agency for Healthcare Research and Quality [3]. The NIS is a 20% stratified sample of community hospitals in the United States [2]. The NIS sampled hospitals according to five hospital characteristics: geographic region (Northeast, North Central, West, and South); ownership (public, private not-for-profit, and private investor-owned); location (urban, rural); teaching status (teaching hospital, nonteaching hospital); and bed size (small, medium, and large).
Information on validation and quality control can be found in detail on the HCUP website [1]. The NIS also was validated extensively against the National Hospital Discharge Survey and confirmed to perform very well for many estimates [45].
The NIS has information on primary ICD-9-CM diagnosis and procedure codes and 14 secondary diagnosis and procedure codes for each patient record. We selected admissions with an ICD-9-CM primary diagnosis code for closed proximal humeral fracture (812.00, 812.01, 812.02, 812.03, and 812.09) and a primary procedure code for hemiarthroplasty (81.81), ORIF (79.31), and total shoulder arthroplasty (81.80). Patients with procedure codes for hemiarthroplasty or total shoulder arthroplasty and ORIF were included in our analysis (n = 563) as these are likely patients who had a proximal humeral fracture and a humeral shaft fracture. Because such patients likely underwent arthroplasty for the proximal humeral fracture, they contribute to hemiarthroplasty and total shoulder arthroplasty data in our analysis. One patient had a procedure code for hemiarthroplasty and total shoulder arthroplasty. This likely represents a coding error, and therefore this patient was excluded from our analysis. The final data set included 25,731 records. Each record in the data sets represented a single patient admission and had a unique identification number.
The majority of patients were 65 years or older (61%). Approximately 73% of patients were female. The majority of patients underwent ORIF (62.2% of patients) as compared with hemiarthroplasty (35.2% patients) (Table 1).
Table 1.
Characteristics of patients with proximal humeral fractures treated surgically
| Characteristic | ORIF | Hemiarthroplasty | Total shoulder arthroplasty |
|---|---|---|---|
| Number of patients | 15,999 (62.2) | 9067 (35.2) | 665 (2.6) |
| Age | |||
| < 50 years | 3504 (89)‡ | 389 (10) | 20 (1%) |
| 50–64 years | 4050 (66)‡ | 1926 (32) | 123 (2) |
| 65–79 years | 5172 (54)‡ | 4055 (43) | 313 (3) |
| ≥ 80 years | 3271(53)‡ | 2694 (44) | 208 (3) |
| Sex | |||
| Female | 10,977 (58)‡ | 7346 (39) | 535 (3) |
| Male | 5009 (73)‡ | 1718 (25) | 129 (2) |
| Primary payer | |||
| Medicare | 8171 (55)‡ | 6325 (42) | 501 (3) |
| Medicaid | 763 (77)‡ | 211 (21) | 22 (2) |
| Private insurance | 5292 (72)‡ | 1986 (27) | 116 (2) |
| Other* | 1732 (76)‡ | 535 (23) | 26 (1) |
| Surgeon volume (shoulder arthroplasty)† | |||
| < 5 procedures/year | 8972 (66)‡ | 4361 (32) | 273 (2) |
| 5–14 procedures/year | 1102 (50) | 1014 (46) | 105 (5) |
| ≥ 15 procedures/year | 416 (46) | 419 (47) | 64 (7) |
| Hospital volume (shoulder arthroplasty)† | |||
| < 5 procedures/year | 3537 (72)‡ | 1328 (27) | 79 (2) |
| 5–14 procedures/year | 4993 (61)‡ | 3035 (37) | 158 (2) |
| 15–29 procedures/year | 3450 (59)‡ | 2229 (38) | 157 (3) |
| ≥ 30 procedures/year | 4019 (59)‡ | 2475 (37) | 271 (4) |
| Hospital location and teaching status | |||
| Rural | 1999 (60)‡ | 1194 (36) | 131 (4) |
| Urban nonteaching | 6285 (61)‡ | 3811 (37) | 273 (3) |
| Urban teaching | 6240 (64)‡ | 3315 (34) | 210 (2) |
| Year | |||
| 2001–2002 | 2911 (57)‡ | 1998 (39) | 164 (3) |
| 2003–2004 | 3523 (60)‡ | 2243 (38) | 122 (2) |
| 2005–2006 | 4058 (63)‡ | 2211 (34) | 148 (2) |
| 2007–2008 | 5507 (66)‡ | 2615 (31) | 231 (3) |
| Mean hospital cost (2001 US dollars) | $12,141‡ | $13,669 | $15,288 |
Values are expressed as number of patients, with percentage in parentheses; numbers missing: age = 6; sex = 100; payer = 100; hospital location and teaching status = 100; * other includes Workers Compensation, Civilian Health and Medical Program of Uniformed Service, Civilian Health and Medical Program of the Department of Veterans Affairs, Title V, and other government programs; †hospital and surgeon volume of shoulder arthroplasty includes total shoulder arthroplasty and hemiarthroplasty; surgeon identifier not present for surgeons in CA, CT, GA, HI, IL, IN, KS (2001–2004), MA, NC, OH, OK (2005–2008), and UT, VT, WI, WV (2004–2008); ‡variable differs between ORIF and hemiarthroplasty (p < 0.05); ORIF = open reduction and internal fixation.
We categorized age into younger than 50 years, 50 to 64 years, 65 to 79 years, and 80 years and older based on clinically meaningful cutoffs. Primary payer in the databases indicates the expected primary payer for the hospital admission. Patient comorbidity was assessed using the Charlson Comorbidity Index (CCI) (categorized into 0, 1, and ≥ 2 by two of us [IK, NBJ]) [12], as modified for administrative data by Deyo et al. [14]. The comorbidities used to calculate the CCI were based on discharge diagnoses from the index admission included in the NIS databases. Each of the diagnoses for every record was used to generate a composite CCI score. We divided the study period into 2001 to 2002, 2003 to 2004, 2005 to 2006, and 2007 to 2008 based on equal intervals.
Hospital teaching status for a given year was obtained from the NIS database [2]. The NIS classifies a hospital as teaching if it had an American Medical Association-approved residency program, was a member of the Council of Teaching Hospitals, or had a ratio of full-time equivalent interns and residents to beds of 0.25 or higher. Hospitals were characterized as urban by the NIS if they were in a metropolitan statistical area and rural if they were in a nonmetropolitan statistical area [23]. Geographic location of the hospital was divided by NIS into Northeast, South, Midwest, and West, as determined by census regions. We calculated hospital volume and surgeon volume per year for shoulder arthroplasty (total shoulder arthroplasty and hemiarthroplasty) using unique hospital and surgeon identifiers for states that provide these data [23]. Annual hospital volume of shoulder arthroplasty was further categorized into fewer than five procedures (low volume), five to 14 procedures (medium volume), 15 to 29 procedures (medium volume), and 30 or more procedures (high volume), based on clinically meaningful cutoffs and our previous work [23]. Annual surgeon volume of shoulder arthroplasty was categorized into fewer than five procedures (low volume), five to 14 procedures (medium volume), and 15 or more procedures (high volume), based on previous publications and clinically meaningful cutoffs [19, 22].
Disposition of patient on discharge was coded into routine and nonroutine dispositions. Nonroutine disposition includes transfer to a short-term hospital, skilled nursing facility, intermediate care facility, and another type of facility or home health care. Routine disposition reflects patients who were discharged home. We also assessed in-hospital complications that included patients with a secondary diagnosis of postoperative infections, pulmonary embolism, and thrombophlebitis or other vascular and nonvascular complications of the procedure. Cases that were likely revisions after a previous primary surgery also were assessed based on diagnostic codes that implied previous device complications. A complete listing of diagnostic codes used to categorize complications and revisions can be obtained from the corresponding author (NBJ).
The NIS includes data on total hospital charges. Generally, total charges do not include professional fees and noncovered charges. If the source provides total charges with professional fees, the professional fees are removed from the charge during database processing. We used the hospital-specific cost-to-charge ratios based on all-payer inpatient cost to convert hospital charges to hospital cost. Cost information was obtained from the hospital accounting reports collected by the Centers for Medicare & Medicaid Services. All hospital costs were discounted to the base year of our study (2001) to adjust for inflation during our study period. The Consumer Price Index for Medical Care based on the US Bureau of Labor Statistics for each year was used to adjust for inflation [42].
We studied the distribution of demographic, clinical, and other variables such as patient age and sex, surgeon volume, location of fracture across ORIF, hemiarthroplasty, and total shoulder arthroplasty using means and proportions. Outcomes such as in-hospital mortality and length of hospital stay across categories of surgeon volume also were assessed. We used a linear regression model to assess the association between hospital cost and demographic and provider variables for hemiarthroplasty and ORIF. Multivariate logistic regression was used to assess the association of demographic, clinical, and provider variables with the surgical procedure (ORIF versus hemiarthroplasty). Total shoulder arthroplasty was not included in regression models as it is not frequently performed for proximal humeral fractures and clinical characteristics of such patients are usually different from those of patients undergoing hemiarthroplasty or ORIF. However, with the advent of reverse shoulder arthroplasty, this trend may change and it is possible that patients coded as having total shoulder arthroplasty underwent reverse arthroplasty in our study. We performed a stepwise regression analysis by including variables significant at the 0.05 level or those that altered the odds ratio of surgeon volume by 10% or more for the linear and logistic regression models [38]. Statistical analyses were performed with Intercooled STATA® for Windows® (Version 11.2; Stata Corp, College Station, TX, USA) and SAS® for Windows® (Version 9.1; SAS Institute Inc, Cary, NC, USA).
Results
ORIF was performed more frequently in patients younger than 50 years (89%) than in patients 80 years or older (53%). The proportion of patients undergoing hemiarthroplasty operated on by high-volume surgeons (47%) was higher than the proportion operated on by low-volume surgeons (32%). This trend also was observed across hospital volume. There was little variation in the proportion of patients undergoing hemiarthroplasty across hospital teaching status (Table 1) and hospital geographic location (data not shown). As expected, most patients with a fracture of the surgical neck underwent ORIF (75%) (Table 2). However, contrary to expectation, only 49% of patients with a fracture of the anatomic neck underwent hemiarthroplasty. Mortality, length of stay, and rate of in-hospital complications were similar for hemiarthroplasty and ORIF (Table 3). A higher proportion of patients undergoing ORIF were discharged home as compared with those undergoing hemiarthroplasty. Revision procedures were more likely to be hemiarthroplasties than ORIF.
Table 2.
Clinical characteristics of patients with proximal humeral fracture treated surgically
| Clinical characteristic | ORIF | Hemiarthroplasty | Total shoulder arthroplasty |
|---|---|---|---|
| Number of patients | 15,999 (62.2) | 9067 (35.2) | 665 (2.6) |
| Diagnosis (ICD-9-CM) | |||
| Closed fracture of unspecified part of upper end of humerus (812.00) | 4736 (61)† | 2771 (36) | 247 (3) |
| Closed fracture of surgical neck of humerus (812.01) | 5593 (75)† | 1729 (23) | 121 (2) |
| Closed fracture of anatomic neck of humerus (812.02) | 284 (49) | 286 (49) | 12 (2) |
| Closed fracture of greater tuberosity of humerus (812.03) | 2717 (76)† | 820 (23) | 47 (1) |
| Closed fracture of head or upper epiphysis of humerus (812.09) | 3887 (45)† | 4435 (52) | 293 (3) |
| Charlson Comorbidity Index | |||
| 0 | 10,678 (64)† | 5520 (33) | 404 (2) |
| 1 | 1775 (61)† | 1072 (37) | 78 (3) |
| ≥ 2 | 3546 (57)† | 2475 (40) | 183 (3) |
| Admission type | |||
| Emergency | 7238 (68)† | 3218 (30) | 198 (2) |
| Urgent | 2436 (62)† | 1379 (35) | 102 (3) |
| Elective | 5655 (55)† | 4222 (41) | 354 (4) |
| Other* | 670 (72)† | 248 (27) | 11 (1) |
Values are expressed as number of patients, with percentage in parentheses; * other includes delivery, trauma center, newborn, other admission types, and missing data; †variable differs between ORIF and hemiarthroplasty (p < 0.05); ORIF = open reduction and internal fixation.
Table 3.
Outcomes of patients with proximal humeral fractures treated surgically
| Clinical characteristics | ORIF | Hemiarthroplasty | Total shoulder arthroplasty |
|---|---|---|---|
| Number of patients | 15,999 (62.2) | 9067 (35.2) | 665 (2.6) |
| Mortality | |||
| Died | 83 (0.5) | 47 (0.5) | 5 (0.8) |
| Missing | 41 (0.3) | 26 (0.3) | 1 (0.2) |
| Disposition on discharge | |||
| Routine | 8257 (52)† | 3595 (40) | 265 (40) |
| Nonroutine | 6947(43)† | 5016 (55) | 371 (56) |
| Data missing, patient died or left against medical advice | 795 (5) | 456 (5) | 29 (4) |
| Revision | 73 (0.4)† | 64 (0.7) | 12 (1.8) |
| Hospital length of stay (days)* | 4.9 ± 5.8 | 5.0 ± 4.7 | 4.9 ± 5.0 |
| Complications | 215 (1.3) | 138 (1.5) | 16 (2.4) |
* Values are expressed as mean ± standard error; the remaining values are expressed as number of patients, with percentage in parentheses; †variable differs between ORIF and hemiarthroplasty (p < 0.05); ORIF = open reduction and internal fixation.
Surgeons with high procedure volume had lower in-hospital mortality rates (0.2%) and lower length of stay than surgeons with low procedure volume (0.6%). Their length of stay was 3.4 days (p < 0.01) versus 5.5 days for low volume surgeons (Table 4). The distribution of clinical characteristics of the patient such as comorbid status (CCI) and diagnosis was similar across surgeon volume categories (data not shown). Adjusting for confounders, the odds of a patient undergoing hemiarthroplasty were 1.68 times (95% CI = 1.43, 1.97) when operated on by a high-volume surgeon versus a low-volume surgeon (Table 5). Conversely, the odds of undergoing hemiarthroplasty were 0.61 times (95% CI = 0.56, 0.66) in 2007 to 2008 as compared with 2001 to 2002.
Table 4.
Outcomes of patients according to surgeon volume
| Surgeon volume* | Number of patients | Mortality | Length of stay (days)† | Complications |
|---|---|---|---|---|
| ORIF | ||||
| < 5 procedures/year | 8972 | 59 (0.7) | 5.3 ± 6.4 | 121 (1.3) |
| 5–14 procedures/year | 1102 | 2 (0.2) | 3.2 ± 3.5‡ | 11 (1.0) |
| ≥ 15 procedures/year | 416 | 0 (0) | 2.8 ± 3.2‡ | 2 (0.5) |
| Hemiarthroplasty | ||||
| < 5 procedures/year | 4361 | 26 (0.6) | 5.5 ± 5.4 | 77 (1.8) |
| 5–14 procedures/year | 1014 | 4 (0.4) | 3.8 ± 3.0‡ | 12 (1.2) |
| ≥ 15 procedures/year | 419 | 1 (0.2) | 3.4 ± 3.1‡ | 4 (1.0) |
* Hospital and surgeon volume of shoulder arthroplasty includes total shoulder arthroplasty and hemiarthroplasty; surgeon identifier not present for surgeons in CA, CT, GA, HI, IL, IN, KS (2001–2004), MA, NC, OH, OK (2005–2008), and UT, VT, WI, WV (2004–2008); †values are expressed as mean ± standard error; the remaining values are expressed as number of patients, with percentage in parentheses; ‡p < 0.01, compared with less than five procedures; ORIF = open reduction and internal fixation.
Table 5.
Factors associated with surgical procedure (hemiarthroplasty versus ORIF) for treatment of proximal humeral fracture
| Factor | Total number of patients | Number of patients with hemiarthroplasty | Crude odds ratio (95% CI) | Adjusted odds ratio (95% CI) |
|---|---|---|---|---|
| Surgeon volume* | ||||
| < 5 procedures/year | 13,606 | 4361 | 1.00 | 1.00 |
| 5–14 procedures/year | 2221 | 1014 | 1.75 (1.60, 1.91) | 1.46 (1.32, 1.61) |
| ≥ 15 procedures/year | 899 | 419 | 1.91 (1.66, 2.19) | 1.68 (1.43, 1.97) |
| Age | ||||
| < 50 years | 3913 | 389 | 0.13 (0.12, 0.15) | 0.15 (0.13, 0.17) |
| 50–64 years | 6099 | 1926 | 0.58 (0.54, 0.62) | 0.58 (0.52, 0.65) |
| 65–79 years | 9540 | 4055 | 0.95 (0.89, 1.02) | 0.86 (0.80, 0.93) |
| ≥ 80 years | 6173 | 2694 | 1.00 | 1.00 |
| Sex | ||||
| Female | 18,858 | 7346 | 1.95 (1.83, 2.08) | 1.30 (1.21, 1.39) |
| Hospital volume* | ||||
| < 5 procedures/year | 4944 | 1328 | 1.00 | 1.00 |
| 5–14 procedures/year | 8186 | 3035 | 1.62 (1.50, 1.75) | 1.68 (1.54, 1.83) |
| 15–29 procedures/year | 5836 | 2229 | 1.72 (1.58, 1.87) | 1.74 (1.58, 1.90) |
| ≥ 30 procedures/year | 6765 | 2475 | 1.64 (1.51, 1.78) | 1.72 (1.57, 1.89) |
| Year | ||||
| 2001–2002 | 5073 | 1998 | 1.00 | 1.00 |
| 2003–2004 | 5888 | 2243 | 0.93 (0.86, 1.00) | 0.91 (0.83, 0.99) |
| 2005–2006 | 6417 | 2211 | 0.79 (0.74, 0.86) | 0.73 (0.67, 0.80) |
| 2007–2008 | 8353 | 2615 | 0.69 (0.64, 0.74) | 0.61(0.56, 0.66) |
| Primary payer | ||||
| Medicare | 14,997 | 6325 | 1.00 | 1.00 |
| Medicaid | 996 | 211 | 0.36 (0.31, 0.42) | 0.93 (0.77, 1.12) |
| Private insurance | 7394 | 1986 | 0.49 (0.46, 0.52) | 0.85 (0.77, 0.93) |
| Other† | 2293 | 535 | 0.40 (0.36, 0.44) | 0.88 (0.78, 1.01) |
| Diagnosis (ICD-9-CM) | ||||
| Closed fracture of unspecified part of upper end of humerus (812.00) | 7754 | 2771 | 1.00 | 1.00 |
| Closed fracture of surgical neck of humerus (812.01) | 7443 | 1729 | 0.59 (0.55, 0.63) | 0.61 (0.57, 0.65) |
| Closed fracture of anatomic neck of humerus (812.02) | 582 | 286 | 2.13 (1.79, 2.53) | 2.58 (2.15, 3.10) |
| Closed fracture of greater tuberosity of humerus (812.03) | 3584 | 820 | 0.54 (0.49, 0.58) | 0.60 (0.55, 0.65) |
| Closed fracture of head or upper epiphysis of humerus (812.09) | 8615 | 4435 | 2.47 (2.32, 2.62) | 2.78 (2.61, 2.96) |
| Admission type | ||||
| Emergency | 10,654 | 3218 | 1.00 | 1.00 |
| Urgent | 3917 | 1379 | 1.27 (1.18, 1.38) | 1.18 (1.09, 1.29) |
| Elective | 10,231 | 4222 | 1.68 (1.58, 1.78) | 1.48 (1.39, 1.58) |
| Other‡ | 929 | 248 | 0.83 (0.72, 0.97) | 1.07 (0.90, 1.27) |
* Hospital volume of shoulder arthroplasty represents volume of total shoulder arthroplasty and hemiarthroplasty; †other includes Workers Compensation, Civilian Health and Medical Program of Uniformed Service, Civilian Health and Medical Program of the Department of Veterans Affairs, Title V, and other government programs; ‡other includes delivery, trauma center, newborn, other admission types, and missing data; ORIF = open reduction and internal fixation.
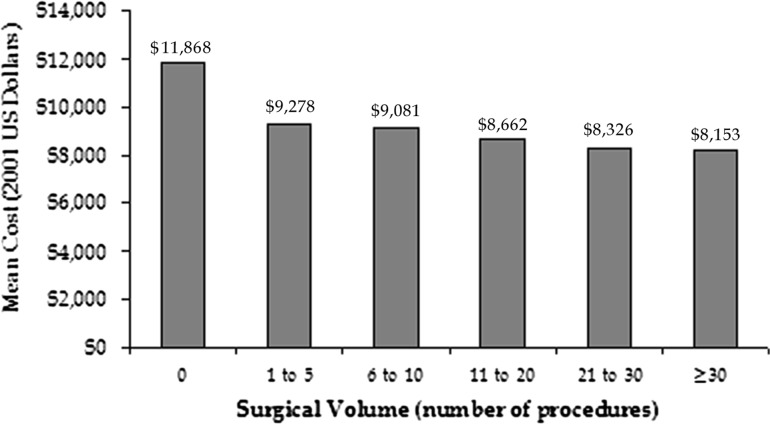
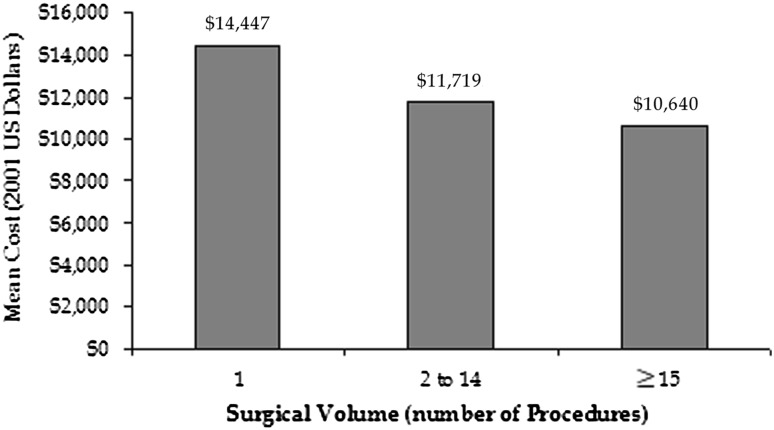
Because the relationship between hospital cost and surgeon volume was linear (Figs. 1 and 2), surgeon volume was used as a continuous variable in the regression analysis for hospital cost. Factors that contributed to lower hospital cost included higher surgeon volume, female sex, ORIF (versus hemiarthroplasty), lower burden of comorbidities (as measured by CCI), younger age, and Medicare as the primary payer (Table 6). Adjusting for sex, procedure, CCI, age, and payer, on average, the hospital cost per procedure was reduced by $90 for each additional arthroplasty performed by a surgeon.
Fig. 1.
Linear decrease in hospital cost of ORIF with surgeon arthroplasty volume (n = 14,342). Note: Procedures with hospital cost greater than US $50,000 were excluded to avoid outliers (n = 270).
Fig. 2.
Linear decrease in hospital cost of hemiarthroplasty with surgeon arthroplasty volume (n = 8115).
Table 6.
Determinants of hospital cost of ORIF and hemiarthroplasty
| Factor | Cost (US dollars) (n = 14,202) |
|---|---|
| Surgeon volume*,† | −90 ± 11‖ |
| Female | −2864 ± 296‖ |
| Hemiarthroplasty‡ | 2414 ± 197‖ |
| Charlson Comorbidity Index† | 394 ± 27‖ |
| Age | |
| < 50 years | 1301.81 ± 554 |
| 50–64 years | −11 ± 404 |
| 65–79 years | −168 ± 205 |
| ≥ 80 years | Reference group |
| Primary payer | |
| Medicaid | 2536 ± 920‖ |
| Private insurance | 1046 ± 382‖ |
| Other§ | 1489 ± 527‖ |
| Medicare | Reference group |
Values are expressed as mean ± standard error; * surgeon volume includes total shoulder arthroplasty and hemiarthroplasty; surgeon identifier not present for surgeons in CA, CT, GA, HI, IL, IN, KS (2001–2004), MA, NC, OH, OK (2005– 2008), and UT, VT, WI, WV (2004–2008); †used as a continuous variable; ‡compared with ORIF; §other includes Workers Compensation, Civilian Health and Medical Program of Uniformed Service, Civilian Health and Medical Program of the Department of Veterans Affairs, Title V, and other government programs; ‖p < 0.01; ¶p < 0.05; ORIF = open reduction and internal fixation.
Discussion
The issue of rising costs will likely dominate the healthcare debate in the forthcoming years. Limited resources may necessitate cost-cutting measures. Proximal humeral fractures account for 10% of all fractures in the elderly. We therefore assessed factors associated with lower hospital costs and variations in surgical treatment for proximal humeral fractures.
The limitations of our study include nonavailability of data for patients who did not undergo surgery because the NIS includes only inpatient admissions. The databases also do not provide information regarding degree of displacement or fracture classifications. Long-term functional outcomes such as pain and ROM also are not available in the NIS. We also do not have information for patients who were managed nonoperatively.
We found there was a linear association between reduced hospital costs and higher shoulder arthroplasty volume of the surgeon for treatment of proximal humeral fractures. We also found there was variation in practice patterns for surgical treatment of proximal humeral fractures. High-volume surgeons and hospitals were more likely to perform hemiarthroplasty as compared with ORIF, after adjusting for potential confounders. Contrary to expectation, the odds of a patient undergoing hemiarthroplasty were reduced during our study period from 2001 to 2008. The length of stay for patients operated on by high-volume surgeons was approximately 40% shorter than for patients operated on by low-volume surgeons.
As is evident from the current healthcare debate, issues relating to cost will be critical. This especially will be the case for costs associated with surgical procedures. Cost-cutting measures may not only aim at eliminating procedures and treatments that are not supported by outcome data but also at assessing factors that contribute to increased costs. Several studies have reported on the association of higher surgical volume with better outcomes [11, 17, 22, 24–28]. However, to our knowledge, no prior study has assessed the association between surgical volume and hospital costs for orthopaedic procedures. Auerbach et al. [6] reported lowest-volume hospitals had 19.8% higher costs and low surgeon volume was associated with 3.1% higher costs for coronary artery bypass grafting. Gourin et al. [16] also reported a negative correlation between hospital volume and hospital costs for laryngeal cancer surgery. However, for complex cancer surgery, Auerbach et al. [7] reported there were no consistent associations between higher hospital or surgeon volume and mortality, readmission, length of stay, or costs. Studies in the orthopaedic literature also have reported on the association of provider volume and hospital charges [17, 26, 28]. However, hospital charges are often an overestimation and offer little insight into the true costs or reimbursement associated with a procedure. Our results provide evidence that surgeons with high volumes of shoulder arthroplasties per year are associated with lower hospital costs. As an example, on average, adjusting for all other factors, a surgeon performing 20 shoulder arthroplasties per year saves a hospital approximately US $1800 in costs per surgery performed for proximal humeral fractures. This saving amounts to approximately 15% of the cost of an ORIF and 13% of the cost of a hemiarthroplasty. This is substantial from a hospital perspective given a flat rate of reimbursement provided for by Diagnostic Related Groups. Our finding is of critical importance to hospital leaderships and administrators as it may help to guide policies requiring a minimum procedure volume criterion during the hospital credentialing of surgeons.
The treatment of proximal humeral fractures has been debated by experts in several reports [18, 32, 36]. Studies in this area have provided little guidance owing to small sample sizes, lack of comparison groups, and bias in subject selection and study execution [15, 33, 37, 41, 46]. Petit et al. [36] provided evidence for poor agreement between shoulder and trauma surgeons regarding treatment of proximal humeral fractures. A Cochrane Review in 2010 concluded there was insufficient evidence to inform management of proximal humeral fractures, and it was unclear whether surgery provided better long-term outcomes [18]. Moreover, in the future it is likely that patients with proximal humeral fractures will be older with more comorbidities. Thus, optimal treatment in such patients, including nonoperative management, needs further investigation. Many shoulder surgeons use Neer’s classification of two- versus three- versus four-part fractures for classifying proximal humeral fractures [30, 31]. However, there is no evidence that this classification informs surgical decision making. Moreover, several studies have reported poor agreement among surgeons for the Neer classification [10, 39, 40].
Our data show there is considerable variation in the surgical treatment of proximal humeral fractures by surgeon and hospital volume. Moreover, time trends show patients were more likely to undergo ORIF as compared with hemiarthroplasty in the later parts of our study. It is possible the increase in ORIF was attributable to the increased use of locking plates during the later years of the study [4]. However, this information is not available from our data sets. Although, total shoulder arthroplasty is not performed routinely for proximal humeral fractures, 2.6% of patients in our study underwent total shoulder arthroplasties. These patients likely had a chronic fracture or had failure of the hemiarthroplasty. It also is possible that these patients underwent reverse shoulder arthroplasty. Bell et al. [9] reported substantial regional variation in surgical versus nonsurgical treatment of proximal humeral fractures. They did not report on the variation in use of hemiarthroplasty versus ORIF. We did not find regional variations in the use of hemiarthroplasty versus ORIF likely because we studied broad regions in the United States (Northeast, Midwest, South, and West).
To our knowledge, this is the first study to report on the association of higher surgeon volume and lower hospital costs in the area of musculoskeletal care. Because our findings can result in substantial savings, hospital leaderships and administrators should consider framing policies on minimum volume requirements for orthopaedic procedures if our findings are confirmed in future studies. Our study also provides evidence for provider-driven practice variations in the surgical treatment of proximal humeral fractures. This is likely because of the absence of evidence-based treatment guidelines. In the future, reimbursement for orthopaedic procedures will likely be driven by data on comparative effectiveness and will not be based on individual provider practices. Therefore, it is essential for clinicians providing musculoskeletal care to offer evidence for their practices in addition to focusing on improvisation of surgical and nonsurgical techniques.
Footnotes
One of the authors (NBJ) certifies that he, or a member of his immediate family, has received or may receive payments or benefits, during the study period, from National Institute of Arthritis and Musculoskeletal and Skin Diseases Project Number 1K23AR059199, Foundation for Physical Medicine and Rehabilitation (Rosemont, IL, USA), and Biomedical Research Institute (Boston, MA, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Brigham and Women’s Hospital, Boston, MA, USA.
References
- 1.Agency for Healthcare Research and Quality. HCUP Quality Control Procedures. Available at: http://www.ahrq.gov/data/hcup/sasddocu/techsupp2.pdf . Accessed May 17, 2012.
- 2.Agency for Healthcare Research and Quality. NIS Database Documentation. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed May 17, 2012.
- 3.Agency for Healthcare Research and Quality. Overview of the HCUP Nationwide Inpatient Sample (NIS) 2000. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/Overview_of_NIS_2000.pdf. Accessed May 17, 2012.
- 4.Agudelo J, Schurmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, Bahrs C, Parekh A, Ziran B, Williams A, Smith W. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21:676–681. doi: 10.1097/BOT.0b013e31815bb09d. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Orthopaedic Surgeons, American Academy of Physical Medicine and Rehabilitation, American College of Rheumatology, American Society for Bone and Mineral Research, Arthritis Foundation, National University of Health Sciences, Orthopaedic Research Society, Scoliosis Research Society, United States Bone and Joint Decade. The Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal, and Economic Cost. Rosemont, IL: American Academy of Orthopedic Surgeons; 2008. Available at: www.boneandjointburden.org. Accessed June 22, 2012.
- 6.Auerbach AD, Hilton JF, Maselli J, Pekow PS, Rothberg MB, Lindenauer PK. Case volume, quality of care, and care efficiency in coronary artery bypass surgery. Arch Intern Med. 2010;170:1202–1208. doi: 10.1001/archinternmed.2010.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Auerbach AD, Maselli J, Carter J, Pekow PS, Lindenauer PK. The relationship between case volume, care quality, and outcomes of complex cancer surgery. J Am Coll Surg. 2010;211:601–608. doi: 10.1016/j.jamcollsurg.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, Keller RB. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, Tosteson AN. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernstein J, Adler LM, Blank JE, Dalsey RM, Williams GR, Iannotti JP. Evaluation of the Neer system of classification of proximal humeral fractures with computerized tomographic scans and plain radiographs. J Bone Joint Surg Am. 1996;78:1371–1375. doi: 10.2106/00004623-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Conway PH, Clancy C. Comparative-effectiveness research: implications of the Federal Coordinating Council’s report. N Engl J Med. 2009;361:328–330. doi: 10.1056/NEJMp0905631. [DOI] [PubMed] [Google Scholar]
- 14.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 15.Duralde XA, Leddy LR. The results of ORIF of displaced unstable proximal humeral fractures using a locking plate. J Shoulder Elbow Surg. 2010;19:480–488. doi: 10.1016/j.jse.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 16.Gourin CG, Forastiere AA, Sanguineti G, Koch WM, Marur S, Bristow RE. Impact of surgeon and hospital volume on short-term outcomes and cost of laryngeal cancer surgical care. Laryngoscope. 2011;121:85–90. doi: 10.1002/lary.21348. [DOI] [PubMed] [Google Scholar]
- 17.Hammond JW, Queale WS, Kim TK, McFarland EG. Surgeon experience and clinical and economic outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2003;85:2318–2324. doi: 10.2106/00004623-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Handoll HH, Ollivere BJ. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2010;12:CD000434. [DOI] [PubMed]
- 19.Hasan SS, Leith JM, Smith KL, Matsen FA., 3rd The distribution of shoulder replacement among surgeons and hospitals is significantly different than that of hip or knee replacement. J Shoulder Elbow Surg. 2003;12:164–169. doi: 10.1067/mse.2003.23. [DOI] [PubMed] [Google Scholar]
- 20.Iglehart JK. Prioritizing comparative-effectiveness research: IOM recommendations. N Engl J Med. 2009;361:325–328. doi: 10.1056/NEJMp0904133. [DOI] [PubMed] [Google Scholar]
- 21.Initial National Priorities for Comparative Effectiveness Research. Washington, DC: National Academy Press; 2009. [Google Scholar]
- 22.Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins LD. The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2004;86:496–505. doi: 10.1302/0301-620X.86B7.14546. [DOI] [PubMed] [Google Scholar]
- 23.Jain NB, Higgins LD, Losina E, Pietrobon R, Katz JN. Racial differences in type of surgical procedure performed for proximal humeral fractures. Eur J Orthop Surg Traumatol. 2011;21:569–578. doi: 10.1007/s00590-011-0762-5. [DOI] [Google Scholar]
- 24.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83:1622–1629. doi: 10.1302/0301-620X.83B3.10487. [DOI] [PubMed] [Google Scholar]
- 25.Katz JN, Phillips CB, Baron JA, Fossel AH, Mahomed NN, Barrett J, Lingard EA, Harris WH, Poss R, Lew RA, Guadagnoli E, Wright EA, Losina E. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003;48:560–568. doi: 10.1002/art.10754. [DOI] [PubMed] [Google Scholar]
- 26.Kreder HJ, Deyo RA, Koepsell T, Swiontkowski MF, Kreuter W. Relationship between the volume of total hip replacements performed by providers and the rates of postoperative complications in the state of Washington. J Bone Joint Surg Am. 1997;79:485–494. doi: 10.2106/00004623-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Lavernia CJ. Hemiarthroplasty in hip fracture care: effects of surgical volume on short-term outcome. J Arthroplasty. 1998;13:774–778. doi: 10.1016/S0883-5403(98)90029-8. [DOI] [PubMed] [Google Scholar]
- 28.Lavernia CJ, Guzman JF. Relationship of surgical volume to short-term mortality, morbidity, and hospital charges in arthroplasty. J Arthroplasty. 1995;10:133–140. doi: 10.1016/S0883-5403(05)80119-6. [DOI] [PubMed] [Google Scholar]
- 29.Martin DF, Maguire MG, Fine SL. Identifying and eliminating the roadblocks to comparative-effectiveness research. N Engl J Med. 2010;363:105–107. doi: 10.1056/NEJMp1001201. [DOI] [PubMed] [Google Scholar]
- 30.Neer CS., 2nd Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 31.Neer CS., 2nd Displaced proximal humeral fractures: II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52:1090–1103. [PubMed] [Google Scholar]
- 32.Nho SJ, Brophy RH, Barker JU, Cornell CN, MacGillivray JD. Management of proximal humeral fractures based on current literature. J Bone Joint Surg Am. 2007;89(suppl 3):44–58. doi: 10.2106/JBJS.G.00648. [DOI] [PubMed] [Google Scholar]
- 33.Noyes MP, Kleinhenz B, Markert RJ, Crosby LA. Functional and radiographic long-term outcomes of hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2011;20:372–377. doi: 10.1016/j.jse.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 34.Orszag PR, Emanuel EJ. Health care reform and cost control. N Engl J Med. 2010;363:601–603. doi: 10.1056/NEJMp1006571. [DOI] [PubMed] [Google Scholar]
- 35.Peterson ED. Innovation and comparative-effectiveness research in cardiac surgery. N Engl J Med. 2009;361:1897–1899. doi: 10.1056/NEJMe0907887. [DOI] [PubMed] [Google Scholar]
- 36.Petit CJ, Millett PJ, Endres NK, Diller D, Harris MB, Warner JJ. Management of proximal humeral fractures: surgeons don’t agree. J Shoulder Elbow Surg. 2010;19:446–451. doi: 10.1016/j.jse.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 37.Robinson CM, Page RS, Hill RM, Sanders DL, Court-Brown CM, Wakefield AE. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am. 2003;85:1215–1223. doi: 10.1302/0301-620X.85B7.13959. [DOI] [PubMed] [Google Scholar]
- 38.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 39.Sidor ML, Zuckerman JD, Lyon T, Koval K, Cuomo F, Schoenberg N. The Neer classification system for proximal humeral fractures: an assessment of interobserver reliability and intraobserver reproducibility. J Bone Joint Surg Am. 1993;75:1745–1750. doi: 10.2106/00004623-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Sjoden GO, Movin T, Guntner P, Aspelin P, Ahrengart L, Ersmark H, Sperber A. Poor reproducibility of classification of proximal humeral fractures: additional CT of minor value. Acta Orthop Scand. 1997;68:239–242. doi: 10.3109/17453679708996692. [DOI] [PubMed] [Google Scholar]
- 41.Sudkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, Konrad G. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate: results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320–1328. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 42.US Department of Labor Bureau of Labor Statistics. Measuring price change for medical care in the CPI. Available at: http://www.bls.gov/cpi/cpifact4.htm. Accessed March 2, 2011.
- 43.VanLare JM, Conway PH, Sox HC. Five next steps for a new national program for comparative-effectiveness research. N Engl J Med. 2010;362:970–973. doi: 10.1056/NEJMp1000096. [DOI] [PubMed] [Google Scholar]
- 44.Weinstein MC, Skinner JA. Comparative effectiveness and health care spending—implications for reform. N Engl J Med. 2010;362:460–465. doi: 10.1056/NEJMsb0911104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Whalen D, Houchens R, Elixhauser A. Final 2000 NIS Comparison Report. 2003. HCUP Methods Series Report #2003-1. ONLINE. February 28, 2003. US Agency for Healthcare Research and Quality. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/reports/NIS_Comparison_Report_2000.pdf. Accessed May 17, 2012.
- 46.Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br. 1997;79:412–417. doi: 10.1302/0301-620X.79B3.7419. [DOI] [PubMed] [Google Scholar]