Abstract
Study Design
In vitro biomechanical study of flexibility with finite element simulation to estimate screw stresses.
Objective
To compare cervical spinal stability after a standard plated three-level corpectomy with stability after a plated three-level “skip” corpectomy where the middle vertebra is left intact (i.e., two one-level corpectomies), and to quantify pullout forces acting on the screws during various loading modes.
Summary of Background Data
Clinically, three-level cervical plated corpectomy has a high rate of failure, partially because only four contact points affix the plate to the upper and lower intact vertebrae. Leaving the intermediate vertebral body intact for additional fixation points may overcome this problem while still allowing dural sac decompression.
Methods
Quasistatic nonconstraining torque (maximum 1 Nm) induced flexion, extension, lateral bending, and axial rotation while angular motion was recorded stereophotogrammetrically. Specimens were tested intact and after corpectomy with standard plated and strut-grafted three-level corpectomy (7 specimens) or ‘skip’ corpectomy (7 specimens). Screw stresses were quantified using a validated finite element model of C3–C7 mimicking experimentally tested groups. Skip corpectomy with C5 screws omitted was also simulated.
Results
Plated skip corpectomy tended to be more stable than plated standard corpectomy, but the difference was not significant. Compared to standard plated corpectomy, plated skip corpectomy reduced peak screw pull-out force during axial rotation (mode of loading of highest peak force) by 15% (4-screw attachment) and 19% (6-screw attachment).
Conclusions
Skip corpectomy is a good alternative to standard three-level corpectomy to improve stability, especially during lateral bending. Under pure moment loading, the screws of a cervical multilevel plate experience the highest pullout forces during axial rotation. Thus, limiting this movement in patients undergoing plated multilevel corpectomy may be reasonable, especially until solid fusion is achieved.
Keywords: Biomechanics, multilevel corpectomy, anterior cervical plating
Introduction
Multilevel corpectomy in the cervical spine is a commonly performed procedure and may be required to treat numerous conditions such as cervical spondylosis, ossification of the posterior longitudinal ligament, trauma, tumors, infections and cervical kyphosis.1–10 Reconstruction, intended to provide adequate spinal stability and a scaffold for bone fusion, is challenging after corpectomy.11 Strut-graft reconstruction followed by application of an anterior cervical plate with fixation to terminal vertebrae at both ends of the strut is often applied to achieve fusion.12 However, the associated complication rate, including graft dislodgement, hardware failure, and pseudarthrosis related to anterior long-strut graft fixation, is high. Hardware failure rates as high as 50–80% have been reported.13–19 Multilevel corpectomy involving bone graft and a plate has a much lower clinical success rate than single-level corpectomy, indicating suboptimal stabilization.20–23
Segmental fixed constructs, which allow large cantilever forces generated across the cervical spine to be diffused across multiple screw-host interfaces, application of larger screws, or supplemental posterior fixation, have all been suggested to overcome the clinical difficulties associated with the plate-assisted multilevel cervical corpectomy and to enhance biomechanical stability.24–26 Particularly, an intermediate point of fixation can be used to provide additional stability, acting as a fulcrum for three-point bending as well as providing an additional point through which stress is dissipated.27
Clinical reports have shown that two one-level corpectomies leaving the middle vertebra intact to achieve a three-level “skip” corpectomy configuration is effective.28 This technique involves the insertion of two additional screws in the spared middle vertebra and thus provides six points of fixation instead of four. Despite the presence of an additional partial vertebral body in the middle of the operative field, the skip corpectomy technique can still provide adequate visualization for dural sac decompression.27 We hypothesized that the inclusion of these two additional fixation points can provide a biomechanical advantage, increasing the number of load-sharing fixation points, decreasing the chance for the screw-bone interfaces to fail and improving resistance to multiplanar loads. Compared to a standard multilevel corpectomy, the use of shorter grafts in this configuration can be another factor that helps resist graft dislodgment. The primary objective of this study was to evaluate the biomechanical soundness of this new technique in comparison with a standard three-level model.
Anterior cervical plate stabilization depends on the holding strength of the bone screws; loosening, back-out, and breakage of screws are major concerns, especially in long constructs.29, 30 A secondary aim of this study was to quantify the tendency for screw pullout in standard three-level and skip corpectomy plated constructs. Finite element simulations were used to quantify which screws were under the greatest axial load during physiological movements in plated standard and skip corpectomy constructs.
Material and Methods
Specimen Preparation
Fourteen unembalmed human cadaveric cervical specimens (C2-T1) were harvested from 9 men and 5 women whose mean age at death was 55 years (range 36–66 years). Based on direct inspection and plain film x-rays, no spine had evidence of fracture of the vertebral elements or ankylosis of the intervertebral disc. Specimens were stored frozen at a temperature of −20°C. At the time of testing, the cervical spine specimens were thawed to room temperature in a bath of saline and dissected free of all musculature and other nonligamentous soft tissue. All osteoligamentous structures were preserved.
Bone mineral density (BMD) was determined from lateral scans of the vertebral bodies at the C4-C6 levels using dual energy x-ray absorptiometry (DEXA), and the cadaveric specimens were separated into two groups of seven with closely matched BMDs (0.949 ± 0.207 g/cm2 in the standard corpectomy group, 0.949 ± 0.192 g/cm2 in the skip corpectomy group). Household wood screws were inserted in the exposed distal ends of C2 and T1, and the screw heads and parts of the exposed terminal vertebrae were potted in cylindrical aluminum fixtures using polymethylmethacrylate.
Surgical Procedures
One group of seven specimens received a standard three-level corpectomy and fibular strut graft. C3-C4, C4-C5, C5-C6, and C6-C7 discectomies were performed first by using scalpel, curette, and pituitary rongeurs, simulating clinical procedures. The dissection proceeded to the medial border of the Luschka joints. After removal of the disc material and transection of the posterior longitudinal ligament, a corpectomy channel approximately 1.5 cm wide was created through the C4, C5, and C6 vertebral bodies using a high-speed pneumatic drill (Medtronic Midas Rex, Fort Worth, TX). Posterior longitudinal ligament remnants were removed. The rostral and caudal vertebral endplates were flattened, and a shelf of bone approximately 2 mm high was created in the posterior 5 mm of each endplate to prevent dislodgment of the graft posteriorly. A strut graft from cadaveric fibula or iliac crest was also prepared with a high-speed drill for each specimen and sized to provide a good fit, as would be done clinically. The graft was pushed posteriorly until it contacted the posterior shelf of bone.
The second group of seven specimens received the three-level skip corpectomy construct. The middle vertebra (C5) was left intact while C4 and C6 received 1-level corpectomies. Rostrally and caudally, the C5 vertebra was drilled at an angle in the posteriormost 2–3 mm of the endplates to provide a trajectory to decompress the posterior part of the C5 vertebra. This undercutting technique simulates the decompression that would typically be performed clinically and that is necessary to achieve decompression comparable to that of a three-level corpectomy. A shelf of bone was also created in the posterior 5 mm of each endplate within the corpectomy defects, and cadaveric strut grafts were sized and inserted using the aforementioned technique.
A nonconstraining titanium anterior cervical plate (ACP system, Codman, Johnson & Johnson Professional Inc., Raynham, MA) was applied to the specimens of both groups from C3 to C7 (Figure 1). Plate length was selected according to the dimensions of each specimen (74–96 mm). In the standard three-level corpectomy group, two screws were inserted in C3 and two screws in C7 for a total of 4 screws. Likewise, skip corpectomy specimens received screws in C3 and C7, and two additional screws were placed in the intermediate intact vertebra (C5) (total of 6 screws).
Figure 1.
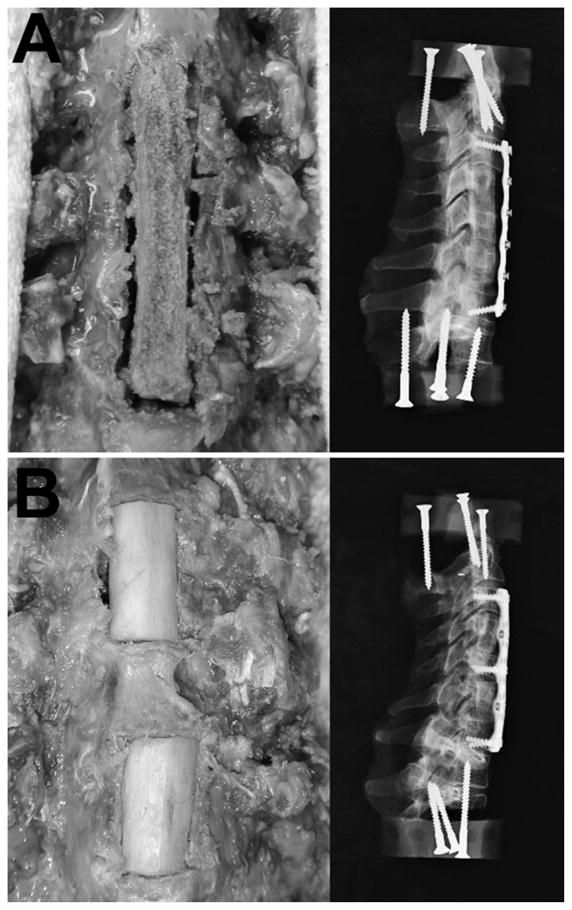
Anterior photographs and lateral x-rays of instrumented cervical corpectomy constructs tested. (A) Standard plated and grafted three-level corpectomy, (B) Skip corpectomy with the middle vertebra left intact allowing two additional fixation points. Both standard and skip corpectomies span the same number of levels. Used with permission from Barrow Neurological Institute.
The self-tapping 12-mm long screws (outer diameter 4 mm) were cannulated with a 1.25-mm core and instrumented with strain gauges with the intention of directly measuring pullout forces. However, the strain gauge data proved unreliable and were not used. Cannulation and gauging did not affect the screw threads and therefore should not have affected the screw’s holding strength or deformability under the load range studied.
Flexibility Tests
Multidirectional flexibility tests were used to document the stability of the constructs. Nondestructive, nonconstraining pure moments were applied to specimens using a servohydraulic test system (MTS Systems, Minneapolis, MN) in conjunction with a system of strings and pulleys.31 Before data were collected, specimens were preconditioned three times at 1.0 Nm for 60 seconds followed by 60 seconds at zero load. After preconditioning, data were acquired at 2 Hz while specimens were loaded in 0.25-Nm increments to a maximum of 1.0 Nm. At each increment, loading was held for 45 seconds. This peak load (1.0 Nm) is the same as previously used in testing multilevel corpectomy constructs,32 but it was less than is typical for flexibility testing of shorter or more robust cervical constructs.33
Motion was recorded independently at C3, C4, C5, C6, and C7 from infrared-emitting diodes glued to the ends of three 1.25-mm diameter surgical guide wires inserted in each vertebra. Diode motion was recorded stereophotogrammetrically (Optotrak 3020, Northern Digital, Waterloo, ON, Canada). The anatomical coordinate system of each motion segment was related to marker position by using a digitizing probe (accessory to the Optotrak).34 Custom software converted the marker coordinates to angles about each anatomical axis, represented independently at C3-C4, C4-C5, C5-C6 and C6-C7. Angles were determined using the “tilt/twist” method, which represents two vertebrae in a motion segment as stacked cylinders.35
Data Analysis
Based on the raw data, the angular range of motion (ROM), lax zone (LZ), and stiff zone (SZ) were quantified during all loading modes to assess construct stability. The ROM refers to the angle of the spine during application of the maximum load (1.0 Nm), whereas the LZ and SZ refer to the portions of the ROM where motion occurs with little or substantial resistance, respectively.36 The transition angle from LZ to SZ was determined by linearly extrapolating load vs. angle data from the upper SZ to zero load. For separating flexion from extension, the neutral position was defined as the midpoint of the bidirectional LZ. Data were determined in terms of degrees and also as dimensionless ratios normalized to the intact condition. Normalization mitigates the effects of variability in stiffness naturally expected in human cadaveric specimens. Results were compared between groups using nonpaired two-tailed Student’s t-tests. Within each group, one-way repeated-measures analysis of variance was used to assess whether contributions of individual motion segments to the total ROM differed among constructs. In all comparisons, a probability value less than 0.05 was considered significant.
Finite Element Analysis
Bony geometry and spacing for a three-dimensional model of C3-C7, including intervening discs, were obtained from a computed tomography (CT) scan of a cadaveric human spine from a 43-year-old male using Scan-FE software (Simpleware, Exeter, UK). The CT scan was captured using a LightSpeed scanner (General Electric Medical Systems, Milwaukee, WI) with axial slice spacing of 0.625 mm.
Geometry was meshed using ICEM (ANSYS, Inc., Canonsburg, PA). Cortical bone was meshed with shell elements and cancellous bone with 10-node tetrahedral elements. Different material properties were assigned to each. Cortical bone elastic modulus was E = 12 GPa. Poisson’s ratio was υ = 0.3. Cancellous bone material properties were set at E = 100 MPa and υ = 0.2. Constant cortical thickness (0.28 mm) and nonlinear material properties were assumed. Ligamentous elements representing interspinous ligaments, capsular ligaments, and ligamentum flavum were included. Anterior longitudinal ligament, posterior longitudinal ligament, and intervertebral disc were simulated in the intact model but were removed in the instrumented models. The intervertebral disc was represented as 63% annulus fibrosus and as 37% nucleus pulposus using a Mooney-Rivlin formulation to simulate incompressible hyperelastic behavior of annulus and nucleus.
Titanium plates (2.58 mm thick) and screws were modeled using 10-node tetrahedral elements with an elastic modulus of 113 GPa and Poisson’s ratio of 0.3. Since the parameter of interest was axial load on screws and not screw-bone mechanics, screws were modeled as smooth cylinders (without threads) of 5.0 mm diameter and with immovable interface between screw and bone. Because of difficulties modeling plate-bone contact, plates were represented elevated away from the bone by 1 mm.
The finite element model was validated by comparing the ROMs from simulations of the intact condition during flexion, extension, lateral bending, and axial rotation to the mean experimental data obtained from the flexibility tests. Simulations gave ROM values that were within 10% of experimental data during all loading modes, indicating acceptable accuracy. It was expected that simulations would appear more stable than experimental data with hardware in place because of the rigid screw-bone interface.
Simulations of three conditions were run using ANSYS Mechanical v.12.0. (ANSYS, Inc.). One condition modeled a standard corpectomy with a four-level plate and four screws; the second condition modeled a skip corpectomy with a four-level plate and six screws. The third condition modeled a skip corpectomy with a four-level plate and four screws (Figure 2). Pure moment loads of 1.5 Nm were applied to a point offset above C3 and connected to multiple nodes on C3 via bar elements, avoiding stress concentration that would occur if the moment was applied to one node. C7 was fixed along the inferior vertebral endplate.
Figure 2.
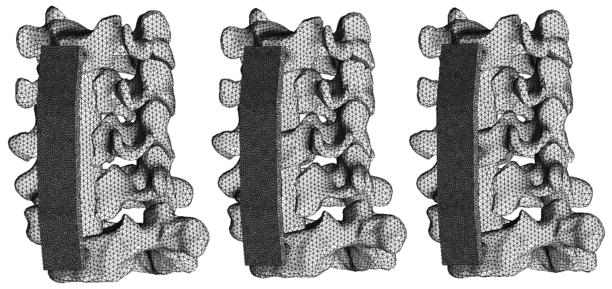
Geometric representations of the three conditions studied using finite element modeling. Standard plated corpectomy (left), skip corpectomy with four screws (center), and skip corpectomy with six screws (right). Used with permission from Barrow Neurological Institute.
The computations were performed on a 4-processor (Intel Xeon) 3.0 GHz personal computer with 16 gigabytes of RAM. Solutions of models required approximately 1.5 hours of computational time for each loading modality.
After simulations were completed, axial forces on each screw were calculated through a cross-section (area = 19.6 mm2) of the shaft of each screw. The cross section was 2.0 mm distal to the point where the screw passed the inside surface of the plate.
Results
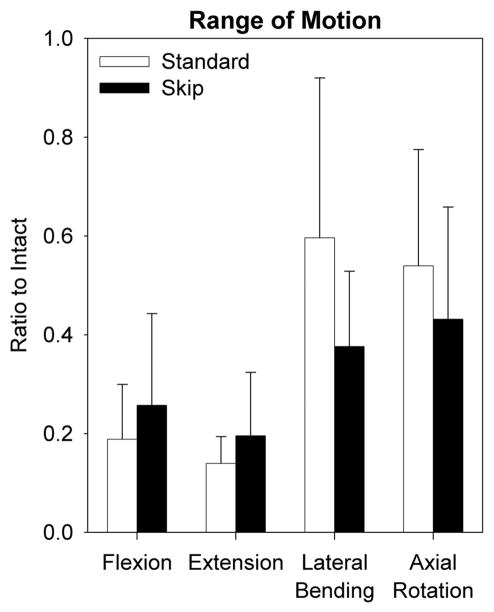
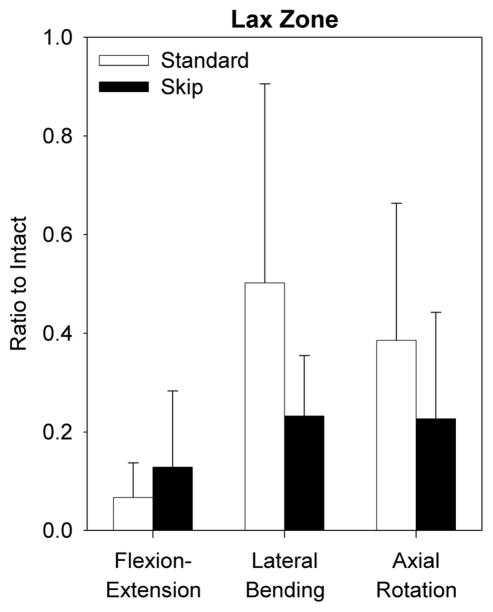
In both standard three-level and skip corpectomy constructs, angular ROM values for C3-C7 were significantly reduced in all directions of loading when compared with the normal conditions (p<0.03). Expressed as normalized values (Figure 3), the relative decrease in ROM for either corpectomy configuration was greater during flexion and extension than during lateral bending or axial rotation, indicating greatest stability after anterior plating during these loading modes. A skip corpectomy limited the ROM slightly more than a standard corpectomy during lateral bending (p=0.13) and axial rotation (p=0.40). In contrast, a standard corpectomy limited the ROM slightly more than a skip corpectomy during flexion (p = 0.42) and extension (p = 0.31). The trends for LZ and SZ after skip and standard corpectomies were similar to those for ROM (Figures 4 and 5). There were no significant differences during flexion (LZ p = 0.35, SZ p = 0.43), extension (LZ p = 0.35, SZ p = 0.07), lateral bending (LZ p = 0.12, SZ p = 0.77), or axial rotation (LZ p = 0.25, SZ p = 0.33).
Figure 3.
Mean normalized unidirectional angular range of motion (ROM) summed across C3-C7 in each direction of loading after standard and skip corpectomy. Error bars show standard deviations. Used with permission from Barrow Neurological Institute.
Figure 4.
Mean normalized bidirectional angular lax zone (LZ) summed across C3-C7 in each direction of loading after standard and skip corpectomy. Error bars show standard deviations. Used with permission from Barrow Neurological Institute.
Figure 5.
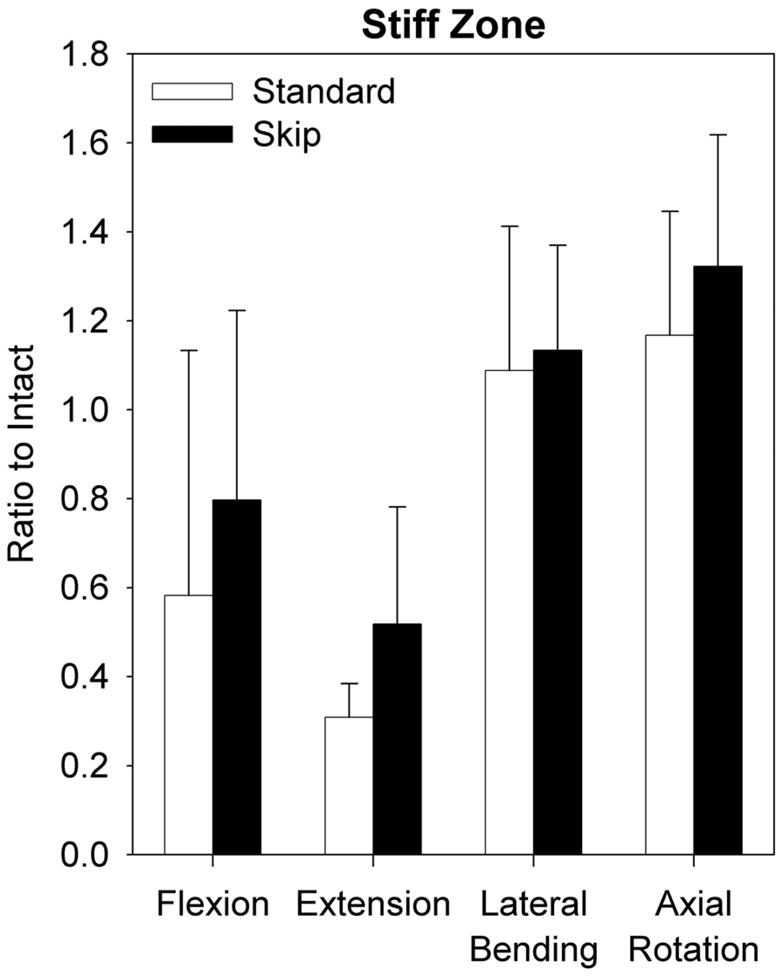
Mean normalized unidirectional angular stiff zone (SZ) summed across C3-C7 in each direction of loading after standard and skip corpectomy. Error bars show standard deviations. Used with permission from Barrow Neurological Institute.
Based on within-groups comparisons of the mean contribution to ROM by level, no level within either construct contributed a lesser or greater amount to the overall ROM during any loading mode (p > 0.12, Figure 6). The distribution of ROM by level did not appear to differ between skip and standard corpectomies during lateral bending or axial rotation. During flexion-extension, ROM was more limited at C4-5 in the skip corpectomy group than in the standard group, but this difference did not reach significance (p = 0.15, non-paired t-test).
Figure 6.
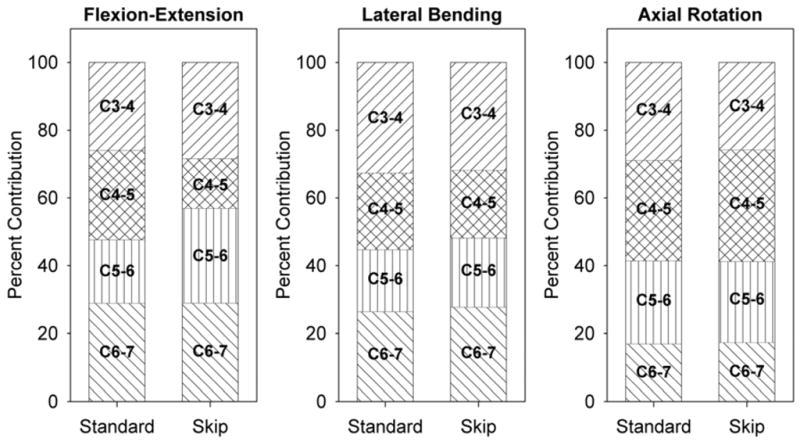
Mean contribution to C3-C7 ROM of individual motion segments within skip and standard corpectomy constructs during each loading mode. Used with permission from Barrow Neurological Institute.
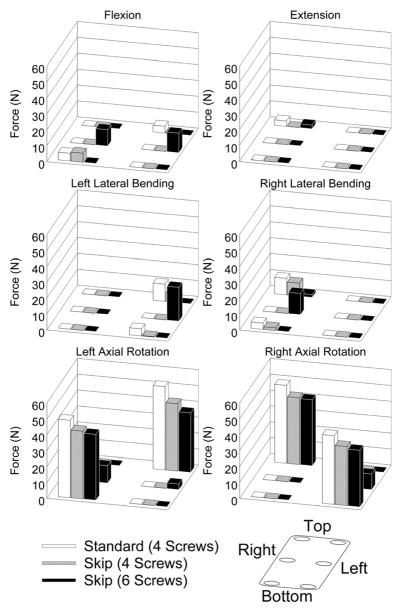
Finite element analysis showed that the greatest tensile force (tendency for pullout) on any one screw occurred during axial rotation in the standard three-level corpectomy plated configuration (52 N) and in the four-screw (43 N) and six-screw (41 N) skip corpectomy configurations (Figure 7). Flexion, extension, and lateral bending induced by pure moments showed little difference among constructs.
Figure 7.
Predictions of tensile force on each screw and in each loading mode from finite element analysis. Compressive forces are not shown (displayed as zero). Used with permission from Barrow Neurological Institute.
Discussion
The concept of a skip technique for the surgical treatment of cervical spondylotic myelopathy was first reported by Shiraishi as a posterior approach to the cervical spine.37 If performed according to this technique, it is still possible to achieve multilevel decompression although intermediate laminae are left intact.38, 39 From a theoretical perspective, the application of this technique to anterior cervical surgery by leaving the corpus of the middle vertebra intact when multilevel corpectomies are anticipated for decompression is attractive. By providing a more favorable load distribution, such a technique would be expected to reduce many of the complications of multilevel cervical corpectomy procedures, especially graft-related problems.27 Although recently described clinically,40 this technique has not previously been studied biomechanically.
In any plated construct, the lever arms at the distal ends of the plate are proportional to the plate’s length; therefore, greater load is placed on the screws with longer plates, with almost three times higher loads possible on a three-level plate than on a one-level plate. This leverage effect can explain the high failure rates associated with long plated constructs.27, 41–43 To overcome this problem, different construct configurations and surgical techniques have been studied clinically, biomechanically, or both. In a biomechanical comparison of two-level corpectomy and aggressive discectomy with three-level standard corpectomy, the first construct provided slightly better stability, especially resisting flexion-extension and lateral bending.44 Singh et al. 45 also studied multilevel discectomy and corpectomy combined with discectomy followed by segmental plate fixation. Their results also showed that it was possible to achieve decompression and biomechanical rigidity comparable to that of constructs having end fixation only.46 George et al.47 reported favorable clinical results with multilevel oblique corpectomy as an alternative to standard multilevel corpectomy for the treatment of multisegmental cervical spondylotic myelopathy, and Cagli et. al. studied this technique biomechanically.48 In our study the skip corpectomy provided immediate postoperative stability that was comparable to that of standard plated corpectomy.
Based on our results, despite mild alteration of the segmental distribution of ROM, the skip corpectomy technique did not decrease motion compared to standard corpectomy during flexion and extension loading modes. In contrast, previous investigators have reported increased rigidity associated with segmental fixation constructs during flexion and extension.49, 50 With the skip corpectomy technique, the segmental fixation point is in the middle of the surgical area of interest (the middle intact vertebral body). The previous studies focused on single-level discectomy/corpectomy models with the point of segmental fixation toward one end of the construct. This difference in construct geometry can explain the different biomechanical behavior of skip corpectomy constructs. Segmental versus long fixation is not necessarily always expected to lead to smaller ROM. As in our study, Galler et al.51 found no significant difference between multilevel plated corpectomy and multilevel plated discectomy despite the additional points of fixation at each intermediate vertebra in the multilevel discectomy construct.
Segmental contribution to ROM within each plated corpectomy construct was studied to determine whether either fusion construct might be more effective in limiting ROM at certain levels than at others. In extreme circumstances, such a property could theoretically result in partial fusion across the construct or in unpredictable final fused lordosis if one portion remained mobile while another portion fused. That no significant difference was found within or between groups indicates comparable environments for fusion.
One technical concern with skip corpectomy might be whether adequate decompression of the posterior part of the middle vertebra can be achieved using this method. However, cervical stenosis is typically confined to adjacent-level degenerated discs with little bony ridging behind the vertebral bodies in most cases.52 Furthermore, in the rare cases when the posterior part of the corpus contributes to stenosis, it is still possible to decompress the intact vertebra from an angled approach with extirpation of the osteophytes along with adequate visualization and decompression of the dural sac. To simulate the real surgery, we used angled curettes and the pneumatic drill to trim the posterior 2 to 3 mm of the superior and inferior endplate surfaces of the middle vertebra with a slight slope in the skip corpectomy group from both rostral and caudal approaches before flexibility testing. Our qualitative observations also confirmed that a skip corpectomy could be performed with decompression equivalent to that of a standard corpectomy.
The incidence of pseudarthrosis may increase as the number of surfaces that must fuse increases.53–55 The skip corpectomy model requires four graft-host surfaces for fusion whereas a three-level corpectomy requires only two surfaces. This difference could be considered a drawback of the skip technique. However, Wang et al.56 found that the incidence of graft migration was directly proportional to the length of the graft and the number of levels involved in the surgery; single-level corpectomies had the lowest incidence of graft migration. Therefore, the increased chance of migration of the longer graft must be weighed against the increased number of fusion surfaces of the shorter grafts. Prospective or retrospective clinical studies are needed to clarify the relative weight of these two factors.
One method of preventing construct failure in long constructs is the provision of additional implant-bone interfaces. The bone graft can be used as an intermediate hardware attachment site.27 This technique has been studied biomechanically. In some cases, the addition of a screw to the strut graft does increase stability, especially during flexion and lateral bending.57 However, the graft is not a biomechanically rigid place to anchor screws, and perforation of the graft by the screw can weaken the graft structurally, facilitating subsequent graft breakage. In the skip corpectomy technique, the intermediate vertebral body can be a very effective attachment site for segmental fixation.
Cervical spine kyphosis often is associated with cervical spondylotic myelopathy or posterior decompressive laminectomy. Corpectomy is a possible alternative to correct this pathology.58, 59 The effects of aging, along with osteoporosis, which is common in patients with cervical kyphosis, can hinder the success rate of ventral deformity correction because of suboptimal bony fixation sites for plates. The skip corpectomy technique may offer an additional advantage in the treatment of kyphotic deformity. During screw tightening, the intermediate vertebral body is effectively pulled anteriorly, forcing contact with the contoured plate and facilitating reversal of kyphosis. Further experimental and clinical comparisons of the ability of skip and standard corpectomies to reverse kyphosis are needed.
Most complications associated with constructs used for the reconstruction of multilevel cervical corpectomies arise from failure at the screw-bone interface. However, a few biomechanical studies have involved the screws of these constructs, and most of them have focused on the pullout resistance of the cervical pedicle or lateral mass plates or screws used for salvage procedures.60–62 More studies of ways to reduce loads on screws within constructs are needed to develop strategies for overcoming screw-bone failures.
To the best of our knowledge, forces acting on the screws in cervical plate constructs have not been quantified previously. One aim of this study was to assess axial tensile forces acting on the screws in cervical plating constructs during in vitro loading, using specially produced screws with four semiconductor strain gauges along the perimeter inside the cannulation of each screw. Unfortunately, this method was infeasible because the strain gauges could not be calibrated accurately enough to account for off-axis forces. A validated finite element model was a suitable if indirect alternative for studying these forces.
Panjabi et al. studied screw loosening in one- and three-level constructs and found that fatigue caused excessive screw-vertebra motion at the lower end of the three-level corpectomy model.63 A skip corpectomy construct can be viewed as two separate one-level constructs (albeit connected to the same plate). It can therefore be expected to be more resistant to screw loosening. Although we studied neither load to failure nor failure with fatigue, data from the finite element analysis showed that the four screws holding an anterior plate in place in a skip corpectomy construct were subjected to 15% lower maximum tensile force during axial rotation compared to those holding the same plate in place in a standard corpectomy construct with four screws. Furthermore, the finite element analysis showed that incorporating additional screws to hold the anterior plate in place to the intermediate vertebral body in a skip corpectomy construct can reduce the peak tensile forces on screws expected to occur during physiologic movement by another 4%.
Although intuitively extension would be predicted to cause substantial screw pullout forces with an anterior cervical plate because the plate should act in this mode like the claw of a hammer pulling on the heads of the screws, little net tensile load across the shaft of the screw was seen in finite element simulations of extension with any of the three plated conditions. However, this result may reflect the application of pure moment loads to induce extension to match experimentally applied loads. Because of difficulty in modeling the forces of the plate against bone that would have occurred with a nonrigid screw-plate-bone interface, plates were modeled as being offset from the bone by 1 mm. If additional modeling of this interaction had been applied, including toggling of screws relative to the plate, and if more physiologic loading to induce extension had been used, greater pullout forces on screws would likely have been observed in this mode of simulation.
An important finding of the finite element analysis is that the greatest tendency for screw pullout occurred during axial rotation in all three corpectomy configurations. These data suggest that patients who have undergone corpectomy with anterior plating should be cautioned, especially about voluntary axial rotation of the neck. To some extent, as compared to other movement patterns, this type of movement should be restricted for a more prolonged period until solid fusion is achieved.
In terms of relative LZ, SZ, and ROM allowed, the skip corpectomy model provided stability equivalent to standard corpectomy. This finding suggests that the skip corpectomy construct offers a comparable environment for fusion compared to the standard corpectomy construct. Analysis of the contribution of individual levels to restriction of ROM found no significant differences between skip and standard corpectomy groups, indicating the two techniques offer equivalent environments for fusion. Finite element analysis indicated that skip corpectomy reduced peak axial loads in the screws by about 15% compared to standard corpectomy. That is, skip corpectomy lowers the risk for screw pullout compared to standard corpectomy during physiologic movement. Finite element analysis simulations also suggested that adding screw attachment points to the skipped intermediate vertebral body may reduce the risk for screw pullout even further by decreasing peak tensile loads an additional 4%. Hence, a three-level plated skip corpectomy may be less likely to fail by screw pullout than a three-level plated standard corpectomy using the same size plate. However, additional biomechanical studies, such as comparisons of experimental load to failure with both models and clinical studies focusing on the outcome of patients, fusion, and complication rates, are needed to clarify the clinical usefulness and safety of the cervical skip corpectomy model.
Acknowledgments
This work was partially supported by the National Institutes of Health, Grant 1R01EB006135.
Reference List
- 1.Albert TJ, Klein GR, Vaccaro AR. Image-guided anterior cervical corpectomy. A feasibility study. Spine (Phila Pa 1976) 1999;24:826–30. doi: 10.1097/00007632-199904150-00017. [DOI] [PubMed] [Google Scholar]
- 2.Choi S, Lee SH, Lee JY, et al. Factors affecting prognosis of patients who underwent corpectomy and fusion for treatment of cervical ossification of the posterior longitudinal ligament: analysis of 47 patients. J Spinal Disord Tech. 2005;18:309–14. doi: 10.1097/01.bsd.0000161236.94894.fc. [DOI] [PubMed] [Google Scholar]
- 3.Cooper PR. Anterior cervical vertebrectomy: tips and traps. Neurosurgery. 2001;49:1129–32. doi: 10.1097/00006123-200111000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Epstein N. The surgical management of ossification of the posterior longitudinal ligament in 51 patients. J Spinal Disord. 1993;6:432–54. doi: 10.1097/00002517-199306050-00011. [DOI] [PubMed] [Google Scholar]
- 5.Fessler RG, Steck JC, Giovanini MA. Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery. 1998;43:257–65. doi: 10.1097/00006123-199808000-00044. [DOI] [PubMed] [Google Scholar]
- 6.Kirkpatrick JS, Levy JA, Carillo J, et al. Reconstruction after multilevel corpectomy in the cervical spine. A sagittal plane biomechanical study. Spine (Phila Pa 1976) 1999;24:1186–90. doi: 10.1097/00007632-199906150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Macdonald RL, Fehlings MG, Tator CH, et al. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg. 1997;86:990–7. doi: 10.3171/jns.1997.86.6.0990. [DOI] [PubMed] [Google Scholar]
- 8.Ozgen S, Naderi S, Ozek MM, et al. A retrospective review of cervical corpectomy: indications, complications and outcome. Acta Neurochir (Wien) 2004;146:1099–105. doi: 10.1007/s00701-004-0327-z. [DOI] [PubMed] [Google Scholar]
- 9.Wang JC, Hart RA, Emery SE, et al. Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine (Phila Pa 1976) 2003;28:1016–21. doi: 10.1097/01.BRS.0000061998.62204.D7. [DOI] [PubMed] [Google Scholar]
- 10.Zdeblick TA, Bohlman HH. Cervical kyphosis and myelopathy. Treatment by anterior corpectomy and strut-grafting. J Bone Joint Surg Am. 1989;71:170–82. [PubMed] [Google Scholar]
- 11.Singh K, Vaccaro AR, Kim J, et al. Biomechanical comparison of cervical spine reconstructive techniques after a multilevel corpectomy of the cervical spine. Spine (Phila Pa 1976) 2003;28:2352–8. doi: 10.1097/01.BRS.0000085344.22471.23. [DOI] [PubMed] [Google Scholar]
- 12.Singh K, Vaccaro AR, Kim J, et al. Enhancement of stability following anterior cervical corpectomy: a biomechanical study. Spine (Phila Pa 1976) 2004;29:845–9. doi: 10.1097/00007632-200404150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Lowery GL, McDonough RF. The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine (Phila Pa 1976) 1998;23:181–6. doi: 10.1097/00007632-199801150-00006. [DOI] [PubMed] [Google Scholar]
- 14.Paramore CG, Dickman CA, Sonntag VK. Radiographic and clinical follow-up review of Caspar plates in 49 patients. J Neurosurg. 1996;84:957–61. doi: 10.3171/jns.1996.84.6.0957. [DOI] [PubMed] [Google Scholar]
- 15.Phillips FM, Carlson G, Emery SE, et al. Anterior cervical pseudarthrosis. Natural history and treatment. Spine (Phila Pa 1976) 1997;22:1585–9. doi: 10.1097/00007632-199707150-00012. [DOI] [PubMed] [Google Scholar]
- 16.Porter RW, Crawford NR, Chamberlain RH, et al. Biomechanical analysis of multilevel cervical corpectomy and plate constructs. J Neurosurg. 2003;99:98–103. doi: 10.3171/spi.2003.99.1.0098. [DOI] [PubMed] [Google Scholar]
- 17.Vaccaro AR, Falatyn SP, Scuderi GJ, et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410–5. [PubMed] [Google Scholar]
- 18.Ikenaga M, Shikata J, Tanaka C. Anterior corpectomy and fusion with fibular strut grafts for multilevel cervical myelopathy. J Neurosurg Spine. 2005;3:79–85. doi: 10.3171/spi.2005.3.2.0079. [DOI] [PubMed] [Google Scholar]
- 19.Isomi T, Panjabi MM, Wang JL, et al. Stabilizing potential of anterior cervical plates in multilevel corpectomies. Spine (Phila Pa 1976) 1999;24:2219–23. doi: 10.1097/00007632-199911010-00008. [DOI] [PubMed] [Google Scholar]
- 20.Saunders RL, Pikus HJ, Ball P. Four-level cervical corpectomy. Spine (Phila Pa 1976) 1998;23:2455–61. doi: 10.1097/00007632-199811150-00022. [DOI] [PubMed] [Google Scholar]
- 21.Galler RM, Dogan S, Fifield MS, et al. Biomechanical comparison of instrumented and uninstrumented multilevel cervical discectomy versus corpectomy. Spine (Phila Pa 1976) 2007;32:1220–6. doi: 10.1097/01.brs.0000270104.95045.24. [DOI] [PubMed] [Google Scholar]
- 22.Benzel EC. Biomechanics of Spine Stabilization. Rolling Meadows, IL: American Association of Neurological Surgeons; 2001. [Google Scholar]
- 23.Dalbayrak S, Yilmaz M, Naderi S. “Skip” corpectomy in the treatment of multilevel cervical spondylotic myelopathy and ossified posterior longitudinal ligament. J Neurosurg Spine. 2010;12:33–8. doi: 10.3171/2009.7.SPINE08965. [DOI] [PubMed] [Google Scholar]
- 24.Griffith SL, Zogbi SW, Guyer RD, et al. Biomechanical comparison of anterior instrumentation for the cervical spine. J Spinal Disord. 1995;8:429–38. [PubMed] [Google Scholar]
- 25.Ryken TC, Clausen JD, Traynelis VC, et al. Biomechanical analysis of bone mineral density, insertion technique, screw torque, and holding strength of anterior cervical plate screws. J Neurosurg. 1995;83:325–9. [PubMed] [Google Scholar]
- 26.Crawford NR, Brantley AG, Dickman CA, et al. An apparatus for applying pure nonconstraining moments to spine segments in vitro. Spine (Phila Pa 1976) 1995;20:2097–100. doi: 10.1097/00007632-199510000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Panjabi MM, Isomi T, Wang JL. Loosening at the screw-vertebra junction in multilevel anterior cervical plate constructs. Spine (Phila Pa 1976) 1999;24:2383–8. doi: 10.1097/00007632-199911150-00016. [DOI] [PubMed] [Google Scholar]
- 28.Wilke HJ, Wenger K, Claes L. Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J. 1998;7:148–54. doi: 10.1007/s005860050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crawford NR, Dickman CA. Construction of local vertebral coordinate systems using a digitizing probe. Technical note. Spine (Phila Pa 1976) 1997;22:559–63. doi: 10.1097/00007632-199703010-00020. [DOI] [PubMed] [Google Scholar]
- 30.Crawford NR, Yamaguchi GT, Dickman CA. A new technique for determining 3-D joint angles: the tilt/twist method. Clin Biomech (Bristol, Avon ) 1999;14:153–65. doi: 10.1016/s0268-0033(98)00080-1. [DOI] [PubMed] [Google Scholar]
- 31.Crawford NR, Peles JD, Dickman CA. The spinal lax zone and neutral zone: measurement techniques and parameter comparisons. J Spinal Disord. 1998;11:416–29. [PubMed] [Google Scholar]
- 32.Shiraishi T. Skip laminectomy--a new treatment for cervical spondylotic myelopathy, preserving bilateral muscular attachments to the spinous processes: a preliminary report. Spine J. 2002;2:108–15. doi: 10.1016/s1529-9430(01)00118-8. [DOI] [PubMed] [Google Scholar]
- 33.Shiraishi T, Fukuda K, Yato Y, et al. Results of skip laminectomy-minimum 2-year follow-up study compared with open-door laminoplasty. Spine (Phila Pa 1976) 2003;28:2667–72. doi: 10.1097/01.BRS.0000103340.78418.B2. [DOI] [PubMed] [Google Scholar]
- 34.George B, Gauthier N, Lot G. Multisegmental cervical spondylotic myelopathy and radiculopathy treated by multilevel oblique corpectomies without fusion. Neurosurgery. 1999;44:81–90. doi: 10.1097/00006123-199901000-00046. [DOI] [PubMed] [Google Scholar]
- 35.Cagli S, Chamberlain RH, Sonntag VK, et al. The biomechanical effects of cervical multilevel oblique corpectomy. Spine (Phila Pa 1976) 2004;29:1420–7. doi: 10.1097/01.brs.0000129896.80044.b6. [DOI] [PubMed] [Google Scholar]
- 36.Emery SE, Bohlman HH, Bolesta MJ, et al. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. 1998;80:941–51. doi: 10.2106/00004623-199807000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Groff MW, Sriharan S, Lee SM, et al. Partial corpectomy for cervical spondylosis. Spine (Phila Pa 1976) 2003;28:14–20. doi: 10.1097/00007632-200301010-00005. [DOI] [PubMed] [Google Scholar]
- 38.Ou Y, Lu J, Mi J, et al. Extensive anterior decompression for mixed cervical spondylosis. Resection of uncovertebral joints, neural and transverse foraminotomy, subtotal corpectomy, and fusion with strut graft. Spine (Phila Pa 1976) 1994;19:2651–6. [PubMed] [Google Scholar]
- 39.Eleraky MA, Llanos C, Sonntag VK. Cervical corpectomy: report of 185 cases and review of the literature. J Neurosurg. 1999;90:35–41. doi: 10.3171/spi.1999.90.1.0035. [DOI] [PubMed] [Google Scholar]
- 40.Conrad BP, Cordista AG, Horodyski M, et al. Biomechanical evaluation of the pullout strength of cervical screws. J Spinal Disord Tech. 2005;18:506–10. doi: 10.1097/01.bsd.0000140196.99995.65. [DOI] [PubMed] [Google Scholar]
- 41.Hitchon PW, Brenton MD, Coppes JK, et al. Factors affecting the pullout strength of self-drilling and self-tapping anterior cervical screws. Spine (Phila Pa 1976) 2003;28:9–13. doi: 10.1097/00007632-200301010-00004. [DOI] [PubMed] [Google Scholar]
- 42.Pitzen T, Franta F, Barbier D, et al. Insertion torque and pullout force of rescue screws for anterior cervical plate fixation in a fatigued initial pilot hole. J Neurosurg Spine. 2004;1:198–201. doi: 10.3171/spi.2004.1.2.0198. [DOI] [PubMed] [Google Scholar]