Abstract
Considerable excitement and interest have arisen recently concerning the role that acute emotional triggers may play in precipitating a myocardial infarction (MI). Observational studies have found repeatedly that patients report excessive anger, anxiety, sadness, grief, or acute stress immediately prior to onset of MI, and recent meta-analyses summarizing these findings reported strong associations between MI occurrence and many of these acute emotions. However, it is unclear whether and through what mechanisms acute emotional triggers might influence MI, and whether there is any clinical utility in knowing if or how emotions trigger MI. We debate whether emotional triggers matter by reviewing the recent evidence for the association between acute emotional triggers and MI and by describing the potential pathophysiological characteristics and mechanisms underlying this association and the preventive strategies that could be used to mitigate the risk of acute MI. We also examine whether the study of emotional triggers could influence clinical risk management or changes in clinical practice/management. We offer suggestions for research that might shed light on whether emotional triggers could initiate a paradigm shift in preventive cardiology, or whether acute emotional triggers are either intractable catalysts for, or merely an epiphenomenon of, some MIs.
Keywords: Myocardial infarction, Emotional triggers, Risk factors, Epidemiology
An acute trigger refers to an event or reaction to an event in the immediate moments or hours before the onset of a myocardial infarction (MI).1,2 In recent years, a number of such triggers, including environmental factors, patient behaviours, and extreme emotional reactions, have been studied for their proximate association to MI onset.1,3,4 These triggers—which may in turn cause an extreme emotional disturbance—range from external events of short duration, such as earthquakes5–9 or a beloved team's loss of a football match,4,10 to acute manifestations of more chronic internal emotional dispositions.11,12 While a number of methods have been used to study acute triggers, the best method used to date has been a retrospective case-crossover study design comparing the reported occurrence of a trigger in the hours preceding MI onset (called the hazard period) with the expected frequency of this trigger using matched (non-hazard period) historical control data from the same patient. Excellent reviews of the effect of environmental and behavioural triggers on acute cardiovascular events have been published.13,14
Chronic psychological disorders such as depression and anxiety are known to increase the risk of long-term cardiovascular disease (CVD),15 but recent meta-analyses suggest that MI occurrence is strongly associated with acute experiences of anger, anxiety, sadness, grief, and stress.13,16 There is also some evidence that patients who experience an MI triggered by acute emotions fare worse psychologically after the MI.17 Tofler and Muller18 laid out potential public health strategies to counter the risk associated with all of the physical and emotional triggers then known, and Nawrot13 systematically reviewed all known triggers for MI. Herein, we consider recent observational and mechanistic research specifically on emotional triggers, and we offer the argument for, and against, whether they warrant clinical attention. We believe that carefully delineating the reasoning for, and against, the position that emotional triggers matter allows the next generation of research to be conducted more systematically. Thus, we focus on the acute experiences of anger, depression/sadness/grief, and anxiety as triggers of MI. Other types of stress-induced cardiac events (e.g. Takotsubo cardiomyopathy) deserve attention, but are not considered here.
To identify all relevant articles and avoid bias in the review, we conducted searches in MEDLINE and PsycINFO, with all variations on the association between emotional and psychosocial factors and CVD, key subject headings and text words combined, and all languages and study designs considered. We subsequently conducted weekly systematic scans of a wide range of journal titles in the areas of general medicine, cardiology, health psychology, and psychiatry, as well as databases and websites for systematic reviews and meta-analyses.
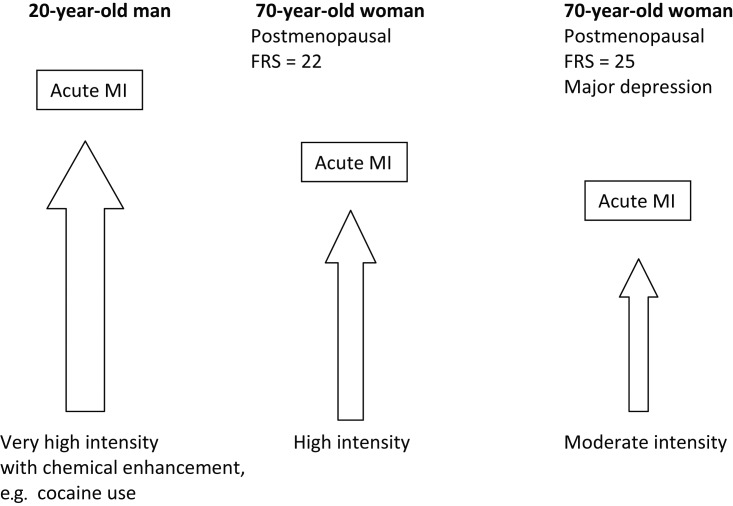
A summary of the strength of the association between episodes of acute negative emotions and acute MI1 is given in Figure 1. The role of anger as a trigger for acute cardiovascular events has been studied most extensively, although observations of the strength of the association have varied widely. For example, Mittleman et al.11 found that the odds ratio for an MI within 2h of an anger episode was 2.3 [95% confidence interval (CI), 1.7–3.2] using the retrospective case-crossover design, whereas Möller et al.19 estimated that individuals were 9.0 (95% CI, 4.4–18.2) times more likely to experience an MI in the hour after an episode of anger than at other times using similar study methods.
Figure 1.
Associations of four emotional triggers and occurrence of acute myocardial infarctiona. aData are taken from Nawrot et al.13 bBars indicate 95% confidence intervals.
Also using the retrospective case-crossover design, Steptoe et al.13 demonstrated that the risk of MI was 2.5 (95% CI, 1.1–6.6) times greater in the 24h following an acute episode of depressed mood. In this population, the relative risk of MI increased with increasing chronic depressive symptom severity, suggesting that background levels of long-term emotional experience may increase the impact of acute negative emotions on acute MI occurrence. More recently, Mostofsky et al.3 demonstrated a 21-fold increased (95% CI, 13.1–34.1) incidence rate of acute MI within 24h of the death of a significant person, a risk that declined steadily on each subsequent day. Importantly, for individuals at low (5%) 10-year MI risk, the absolute risk of MI associated with grief was 1 excess MI per approximately 1400 exposed, but for individuals at high (20%) 10-year MI risk, the grief-related risk was much higher (1 per 320 individuals exposed).2 This suggests that acute emotional triggers may matter most in individuals with an elevated baseline risk for CVD.
Although anxiety has received less attention, there is some evidence to support its role as an acute trigger of MI. Mittleman et al.12 found that patients reported significantly higher levels of anxiety during the 2 h hazard window prior to an MI than during comparison control periods. In that study, the risk of MI was 1.6 times greater (95% CI, 1.1–2.2) for patients with high levels of chronic anxiety.11 Additionally, in a recent study of the effect of dream anxiety on MI occurrence, Selvi et al.20 found an association in univariate analyses between sleep anxiety, disrupted sleep, and near-term MI risk.
This focused literature review suggests that it may be important to study acute emotional triggers of MI, and that further study of these triggers may even provide some insight into how long-term emotional states contribute to CVD risk. However, methodological concerns regarding the influence of recall bias on the reporting of acute emotional triggers, and conceptual ambiguity regarding the relationship between trigger frequency and baseline cardiovascular risk have led some to wonder whether emotional triggers warrant further investigation. A recent meta-analysis by Nawrot et al.13 found that only about 1.2–2.7% of patients were exposed to anger and negative emotions such as depression and anxiety during the window of risk prior to their MI (pooled odds ratio, 3.11–4.46). Thus, a debate as to whether acute emotional triggers are worthy of our collective attention is warranted. Table 1 presents the primary arguments for and against the proposition that emotional triggers of MI should be a major focus of research and clinical practice.
Table 1.
Arguments for and against the importance of emotional triggers of myocardial infarction
| Issue | Emotional triggers matter | Emotional triggers don't matter |
|---|---|---|
| 1. Causal implications | Retrospective case-crossover suggest possible cause of MI1,13,26,65 | Appearance of causality is epiphenomenal, or a product of recall bias24 |
| 2. Pathophysiology | May be implicated in all stages of disease process53 | Merely accelerate existing disease processes66 |
| 3. Risk stratification | Increased accuracy in predicting risk for and timing of MI56 | Vast majority of emotional experiences are identical to triggers, but do not result in MI65 |
| 4. Therapy | Understanding emotional triggers could lead to novel therapies26 | Those at greatest risk for emotional triggers are already being treated with the therapies that work best—and very little evidence that interventions decrease emotional triggers67 |
Arguments that acute emotional triggers matter
Arguments in favour of a focus on acute emotional triggers suggest that they are important for the field in four distinct ways. First, they may represent the final step in a pathophysiological pathway that culminates in a frank occlusion/thrombosis, either by triggering the occlusion through vasoconstriction, or by exacerbating an already ongoing occlusion through prothrombotic effects. If they are causally implicated in this final step of triggering transient vasoconstrictive and/or prothrombotic effects, by studying experimental or naturalistic exposure to acute emotions, we can begin to understand the neuroendocrine/vascular/thrombotic reactions to emotion that might then be targets for future novel and preventive therapies.
Second, although conventional cardiovascular risk factors explain much of the variance in who will ultimately develop CVD,21 they do not predict well who will develop disease imminently3 or when an MI will occur. The study of emotional triggers offers the possibility of 1 day isolating the 2 h window in which a given patient's MI will occur. By including the report of emotional triggers in future cohort and randomized clinical trials, we might improve our predictive models.22
Third, acute emotional triggers cause an MI in some but not all persons. Investigating who is and who is not vulnerable to these types of acute emotional triggers—genetically, by type of vulnerable atherosclerotic plaque, or by type of microvascular disease—could reveal which patients are at risk of an MI in the near term.3 This investigation could lead to both pathophysiological insights and new inputs to improve risk stratification.
Fourth, once acute emotional triggers and their mechanisms of action are understood and patients at risk are identified, strategies could be crafted for preventing or minimizing risk from these triggers. Although it is difficult to speculate on the types of interventions that would be useful, examples of possible prevention strategies include prophylactic therapies for high-risk populations, such as offering anger or stress management or prescribing β-adrenergic blocking agents prophylactically or advocating avoidance of the known trigger(s).18
Arguments that acute emotional triggers do not matter
While the arguments in favour of increased attention to acute emotional triggers are compelling, there are formidable counterarguments. The most glaring concern about the proliferation of research on the putative link between emotional triggers and near-term MI risk is the possibility that this association may be epiphenomenal. For example, risk factors such as anaemia are common to both acute coronary syndrome (ACS) risk and negative mood states,23 and so acute emotional triggers may only be epiphenomenal , and it is the anaemia that caused both the ACS and the exacerbation of negative mood. It is also possible that retrospective reports of emotional triggers are reflections of patients' ideas about cardiac event causation,24–26 known in the field of behavioural medicine as illness perceptions.27 As long as researchers rely on designs featuring retrospective reports without control cohorts, it will be impossible to rule out the possibility that reports of emotions as triggers reflect little more than the fact that some patients believe a priori that heart disease is caused by strong negative emotions.28 The use of case-crossover designs in recent studies of bereavement and cardiac events1,2 is an improvement over earlier approaches, but this design is still subject to reporting bias; that is, when two major events occur that may be cognitively linked a priori, they may be recalled as more proximate to each other than they actually were. This is particularly true for cardiac events, which often induce extreme emotions.29
As such, we know very little about the prevalence or severity of the naturally occurring acute emotional triggers. Ecological momentary assessment (EMA; i.e. the automatic alerting of participants to record subjective reports) results can now be collected on a multitude of devices with minimal interference with daily activities.30 Such patient-reported measures are now considered by the US Food and Drug Administration to represent the gold standard method of measurement for subjective phenomena,31 such as the experience of emotion. Use of EMA methods in a naturalistic study from a representative sample could tell us the prevalence of severe acute emotional triggers in apparently healthy persons. Further, even though the required sample size would be quite large, asking those at high risk for an MI (a very high FRS score) and those at risk for another acute hospitalization (for diagnoses other than MI) to complete EMAs of acute emotions across several weeks or months by adding EMA to large, ongoing epidaemiological studies (e.g. MESA,32 ARIC,33 REGARDS34) would be a pragmatic way to gather data on those emotions that trigger an MI without incurring large costs. In contrast, the number of participants required to capture data on emotions immediately prior to a first MI would be prohibitively large. Obviously, if the prevalence of acute emotional triggers is similar in the periods immediately prior to an MI and those not immediately prior to an MI, then the acute triggers did not precipitate the MI. This type of study would be invaluable for determining if triggers might still be viewed as potentially causal or whether the field should move to other avenues of investigation instead.
It is also possible that emotional triggers exist and are reported accurately but should be thought of as emotional indicators of cardiac event onset, or prodromes. Some have suggested that the sudden surge in inflammation during the onset of ACS35 may account for the acute negative emotions reported by patients,26 as inflammation has been shown to induce negative emotions acutely.36
Methodological issues aside, it might still be the case that emotional triggers do not matter because there is nothing to be done about them that we are not already doing.18 Even the most convincing research suggests that emotions trigger an MI mostly in high-risk patients who are already targeted for risk factor management, and no treatment yet exists to mitigate the biochemical consequences of natural emotions such as grief. Stated differently, since we cannot predict the occurrence of acute strong emotions, efforts should focus instead on traditional, recognized risk factors that we can reliably identify and act on.
Were we to accept that emotions do trigger events, that they can be predicted, and that no practical issues will stop us from preventing them, we might still conclude that emotional triggers do not matter because the attributable risk is small. While risk ratios for cardiac events associated with emotional triggers vary between 1.911 and 21,2 the proportion of MI patients subject to those risks is small, suggesting that the proportion of individuals at risk for an emotionally triggered MI may not be substantial. There is a counterargument that the much smaller population attributable fraction for influenza and respiratory infection as an acute MI trigger37 has generated substantial justified interest. However, interest in an infectious disease that initiates contact between the patient and medical treatment, and for which treatments exist, is importantly distinct from a relatively common emotional experience for which no similarly effective treatments exist.
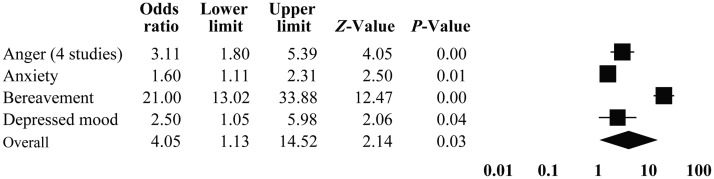
Finally, the effect of acute emotional triggers on acute MI occurrence is likely not uniform and may be modified by multiple factors. Figure 2 applies the recent conceptual model introduced by Wittstein38 to represent the potential interactions between baseline cardiovascular risk, underlying non-cardiovascular vulnerabilities, intensity of emotional triggers, and risk of acute MI. One example of the potential complex interplay of these factors is the use of tricyclic antidepressants, which have been linked to increased CVD events, independent of concomitant mood disorders.39 As some of the cardiotoxic effects of tricyclic antidepressants may operate through haemodynamic pathways similar to those affected by emotional triggers,40 the relationship between emotional triggers and MI may be stronger in patients taking tricyclic antidepressants, regardless of baseline risk determined by the Framingham risk score (FRS). Similarly, mood disorders such as depression have been repeatedly associated with CVD risk,41 which may also strengthen the relationship between acute emotional triggers and acute MI occurrence. In this example, it becomes difficult to identify the MI risk attributable to emotional triggers in the presence of concomitant mood disorders and pharmacotherapy that may also increase MI risk.
Figure 2.
Theoretical model of the interaction of baseline risk of cardiovascular disease and intensity of acute emotion on triggering of acute myocardial infarction. FRS, Framingham risk score; MI, myocardial infarction.
Mechanisms
Animal studies suggest that stressors presumed to provoke acute negative emotions affect cardiovascular physiological characteristics and risk of sudden cardiac death through haemodynamic and electrophysiological pathways.
Some of the haemodynamic effects of acute psychological stressors have been described in the prairie vole, an animal with patterns of autonomic nervous system activation and social interaction similar to those of human and non-human primates. Grippo et al.42 described a greater increase in heart rate and a lack of heart rate variability in response to an acute crowding stressor (thought to provoke anxiety) among voles subjected to social isolation compared with voles allowed to exist in their normal monogamous pairings. Similarly, Stojičić et al.43 reported marked increases in systolic blood pressure, diastolic blood pressure, and heart rate in rats following a startle response to a jet airplane stressor, also thought to provoke anxiety, and found that this response was markedly attenuated following selective intracerebral blockade of the V1/V2 vasopressin receptors. Further, Cyr et al.44 reported that birds captured in the wild demonstrated marked increases in heart rate and decreases in heart rate variability in response to the capture stress.
Other investigations have described cardiac electrical instability and risk of irregular ventricular rhythms, and possibly cardiac arrest, in response to different acute laboratory stressors. In one early study, Skinner et al.45 studied the effects of varying degrees of acute psychological stress thought to provoke anxiety in pigs on the occurrence of ventricular fibrillation following coronary artery occlusion. Pigs acclimatized to the stress of an unfamiliar laboratory environment, again thought to provoke acute anxiety, were significantly less likely than pigs newly introduced to the laboratory to develop ventricular fibrillation in response to occlusion of the left anterior descending coronary artery. In two studies,38,39 Sgoifo et al. reported that the stress of defeat (an acute exposure to depression) in an intruder-resident paradigm in rats was the most potent stimulus for catecholamine increase and ventricular arrhythmias.46,47 Increased ventricular arrhythmogenesis was also demonstrated following the stress of acute crowding in prairie voles following social isolation.42 Evidence from animal research studies clearly demonstrates that acute emotional stressors have important haemodynamic and electrophysiologic effects. However, we believe that the relative dearth of animal studies in this area48 even though there are multiple, well-accepted emotion induction manipulations for various species,49 suggests that the intersection of emotion, heart, and pathophysiological studies in animals is a neglected area and one that could serve us well in truly understanding if emotional triggers matter for MI onset in humans.
The extant research in animals may be applicable to humans, and they suggest that the strongest argument for a focus on acute emotional triggers in humans appears to lie in their potential as a fenestra into the mechanisms by which emotions influence cardiac events. Many of the putative mechanisms underlying emotional triggers and MI risk can be drawn from laboratory studies of the relationship between mental stress and myocardial ischaemia.50,51 In general, these studies use standardized protocols of laboratory psychological stress, such as public speaking, mental arithmetic, or Stroop colour-word tasks, to provoke mental stress, followed by the evaluation of markers of cardiac ischaemia, such as ischaemic patterns on surface electrocardiogram, abnormalities in left ventricular wall motion, and myocardial perfusion defects on nuclear scintigraphy.50–52
In humans, emotional triggers lead to activation of the sympathetic branch of the autonomic nervous system, the cardiovascular effects of which occur predominantly through two pathways: (i) alterations in haemodynamics and (ii) alterations in haemostasis. Alterations in haemodynamics and in haemostasis lead to coronary artery thrombosis either through direct haemodynamic effects on the vulnerable atherosclerotic plaque or through activation of procoagulant factors and de novo thrombosis.1
Emotional triggers lead to neurohormonal activation, which has both systemic and local haemodynamic effects. First, the neurohormonal response to an emotional trigger leads to systemic vasoconstriction and an increase in arterial blood pressure.53 Second, this response increases sinus node firing rates and atrioventricular conduction velocity, increasing heart rate. Increases in heart rate and blood pressure lead to increases in myocardial oxygen consumption and myocardial work and may precipitate rupture of vulnerable atherosclerotic plaque.54 Third, the systemic neurohormonal effects of emotional triggers lead to decreases in heart rate variability (largely through decreases in parasympathetic tone), a known risk factor for cardiovascular morbidity and mortality.55 The haemodynamic effects of emotional triggers act in concert with the two main local neurohormonal effects of emotional triggers.
The haemostatic and procoagulant effects of emotional triggers can be grouped into three categories. First, emotional triggers increase platelet activity and aggregation, largely through activation of the sympathetic nervous system and the effects of catecholamines on platelet function and aggregation.56 Second, emotional triggers increase levels of immunomodulatory, proinflammatory cytokines that lead to atherosclerotic plaque destabilization and monocyte chemotaxis, tissue factor release, and thrombus formation; endothelin, a potent procoagulant, is also released through this process.57 Third, acute emotional triggers may lead to changes in blood viscosity, likely through stimulating the hepatic production of fibrinogen, an acute-phase protein important in both coagulation and whole blood viscosity.57
There are established experimental protocols for inducing acute negative (and positive) emotions in humans, as well as in animals, and these have been used relatively sparsely in explicitly testing the mechanisms hypothesized to link acute emotional triggers to MI onset. Furthermore, investigators have rarely explicitly tested these mechanisms in participants with high FRS, who are most likely to be at high risk for acute emotional triggers. Thus, randomizing a patient with a high FRS to experience (in counterbalanced order) a neutral mood vs. acute sadness vs. acute anxiety vs. acute anger while assessing the putative mechanisms could definitively disprove some hypothesized pathways, while proving others.
In a different study, using the same protocol, immediate post-MI participants could be compared with those without an MI for differences in hyperresponsivity. The use of standard cardiovascular medication after MI (such as β-blockers) may obfuscate the results of this testing paradigm, and there are ethical reasons not to withhold medications from these patients, although the mental-stress ischaemia literature suggests that these protocols might be conducted during a brief medication hiatus without incurring untoward cardiovascular risk.58–60 However, an intriguing recent hypothesis postulates that the excess risk conferred by the acute emotional triggers may operate on mechanisms or pathways not blocked by the current evidence-based cardiac regimen (e.g. 5HTA platelet aggregation),61 and therefore these pathways could be ethically tested in post-MI patients. One excellent example of this type of research was conducted by Strike et al.,53 who carried out acute stress testing in ACS patients, and found that those who reported an emotional trigger of their ACS showed significantly greater increases in monocyte-platelet, leucocyte-platelet, and neutrophil-platelet aggregation in response to stress relative to the non-trigger group.
Regardless of the mechanism, the MI risk associated with emotional triggers varies by baseline CVD risk. Thus, as described by Mittleman and Mostofsky,1 the absolute impact of acute emotional triggers will be greater among individuals with an elevated baseline CVD risk, such that the effect of two episodes of anger daily would vary from approximately one excess cardiovascular event per 1000 person-years in a low-risk population (10-year FRS of 5%) to approximately five excess cardiovascular events per 1000 person-years in a high-risk population (10-year FRS of 20%).62 As such, reduction in cardiovascular risk through management of risk factors for CVD (such as dyslipidaemia, hypertension, and smoking) may be an effective means of preventing an emotionally triggered MI. However, there is also limited evidence to suggest that strategies specifically targeting emotional triggers and stress management are effective in MI prevention. Blumenthal et al.58 reported that in patients with coronary artery disease and an ischaemic response to mental stress testing, compared with a regimen of exercise, a program of stress management led to significant improvements in left ventricular wall motion during mental stress and to a reduction in ischaemia during ambulatory monitoring. Tofler and Muller18 describe a unifying paradigm of triggered acute risk prevention, in which protocols of stress reduction and/or management might play a role—alongside traditional CVD risk modification—in prevention of emotionally triggered MI.
Conclusions
In the face of limited research funding, the choice to investigate acute emotional triggers of MI precludes research related to other phenomena that may occur more frequently. However, some research that focuses on very rare phenomena or syndromes provides great scientific and clinical insight into the cure or prevention of diseases (e.g. Brugada syndrome63 or early repolarization syndrome64). To determine whether acute emotional triggers matter, it is perhaps time to test some of the novel hypotheses and study designs described above (and in Table 2), and so add high-quality evidence to this interesting debate.
Table 2.
Possible study designs to determine the importance of emotional triggers of myocardial infarction
| Study design | Purpose | Strengths and weaknesses |
|---|---|---|
| EMA study in high FRS participants to compare emotions experienced in hours immediately preceding MI to all other hours | Determine the true prevalence of emotional triggers | Limits recall bias; improves causal inference |
| Large sample size required; expensive | ||
| Animal studies that manipulate emotional triggers to determine effect on cardiac event risk | Determine the causal role of emotional triggers on cardiac event risk | Not possible in humans; allows for manipulation of initial cardiac risk and emotional trigger intensity |
| Validity in humans questionable | ||
| Experimental manipulation of acute negative emotions in high FRS participants to determine effect on hypothesized emotional trigger mechanisms | Identify plausible mechanisms and potential treatments | Develops a plausible biological pathway in a causal model |
| External validity of laboratory emotions questionable |
EMA, ecological momentary assessment; FRS, Framingham risk score.
Funding
This work was supported by grants HL-088117, HL-47540, HL-101663, HL-84034, and 5T32HL007854-16 from the NIH, Bethesda, MD, and grant KM1 CA-156709 from the National Cancer Institute, Bethesda. Supported in part by Columbia University's CTSA grant UL1 RR024156 from the National Center for Advancing Translational Sciences/NIH, National Institutes of Health, Bethesda. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest: none declared.
References
- 1.Mittleman MA, Mostofsky E. Physical, psychological and chemical triggers of acute cardiovascular events. Circulation. 2011;124:346–354. doi: 10.1161/CIRCULATIONAHA.110.968776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mostofsky E, Maclure M, Sherwood JB, Tofler GH, Muller JE, Mittleman MA. Risk of acute myocardial infarction after the death of a significant person in one's life: clinical perspective. Circulation. 2012;125:491–496. doi: 10.1161/CIRCULATIONAHA.111.061770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eagle KA, Ginsburg GS, Musunuru K, Aird WC, Balaban RS, Bennett SK, Blumenthal RS, Coughlin SR, Davidson KW, Frohlich ED. Identifying patients at high risk of a cardiovascular event in the near future. Circulation. 2010;121:1447–1454. doi: 10.1161/CIRCULATIONAHA.109.904029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Čulić V. Football matches and acute cardiac events: potential effects of a complex psychosocial phenomenon on cardiovascular health. Int J Epidemiol. 2011;40:1422–1425. doi: 10.1093/ije/dyr060. [DOI] [PubMed] [Google Scholar]
- 5.Brown DL. Disparate effects of the 1989 Loma Prieta and 1994 Northridge earthquakes on hospital admissions for acute myocardial infarction: importance of superimposition of triggers. Am Heart J. 1999;137:830–836. doi: 10.1016/s0002-8703(99)70406-0. [DOI] [PubMed] [Google Scholar]
- 6.Dobson A, Alexander H, Malcolm J, Steele P, Miles T. Heart attacks and the Newcastle earthquake. Med J Aust. 1991;155:757. doi: 10.5694/j.1326-5377.1991.tb94029.x. [DOI] [PubMed] [Google Scholar]
- 7.Leor J, Kloner RA. The Northridge earthquake as a trigger for acute myocardial infarction. Am J Cardiol. 1996;77:1230–1232. doi: 10.1016/s0002-9149(96)00169-5. [DOI] [PubMed] [Google Scholar]
- 8.Ogawa K, Tsuji I, Shiono K, Hisamichi S. Increased acute myocardial infarction mortality following the 1995 Great Hanshin-Awaji earthquake in Japan. Int J Epidemiol. 2000;29:449–455. [PubMed] [Google Scholar]
- 9.Suzuki S, Sakamoto S, Miki T, Matsuo T. Hanshin-Awaji earthquake and acute myocardial infarction. Lancet. 1995;345:981. doi: 10.1016/s0140-6736(95)90727-0. [DOI] [PubMed] [Google Scholar]
- 10.Carroll D, Ebrahim S, Tilling K, Macleod J, Smith GD. Admissions for myocardial infarction and World Cup football: database survey. BMJ. 2002;325:1439–1442. doi: 10.1136/bmj.325.7378.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mittleman MA, Maclure M, Sherwood JB, Mulry RP, Tofler GH, Jacobs SC, Friedman R, Benson H, Muller JE for the Determinants of Myocardial Infarction Onset Study Investigators. Triggering of acute myocardial infarction onset by episodes of anger. Circulation. 1995;92:1720–1725. doi: 10.1161/01.cir.92.7.1720. [DOI] [PubMed] [Google Scholar]
- 12.Steptoe A, Strike PC, Perkins-Porras L, McEwan JR, Whitehead DL. Acute depressed mood as a trigger of acute coronary syndromes. Biol Psychiatry. 2006;60:837–842. doi: 10.1016/j.biopsych.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 13.Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet. 2011;377:732–740. doi: 10.1016/S0140-6736(10)62296-9. [DOI] [PubMed] [Google Scholar]
- 14.Kloner RA. Natural and unnatural triggers of myocardial infarction. Prog Cardiovasc Dis. 2006;48:285–300. doi: 10.1016/j.pcad.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27:2763–2774. doi: 10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- 16.Eterovi D, Miri D. Meta-analysis of possible external triggers of acute myocardial infarction. Int J Cardiol. 2005;99:1–8. doi: 10.1016/j.ijcard.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 17.Bhattacharyya MR, Perkins-Porras L, Wikman A, Steptoe A. The long-term effects of acute triggers of acute coronary syndromes on adaptation and quality of life. Int J Cardiol. 2010;138:246–252. doi: 10.1016/j.ijcard.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 18.Tofler GH, Muller JE. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation. 2006;114:1863–1872. doi: 10.1161/CIRCULATIONAHA.105.596189. [DOI] [PubMed] [Google Scholar]
- 19.Möller J, Hallqvist J, Diderichsen F, Theorell T, Reuterwall C, Ahlbom A. Do episodes of anger trigger myocardial infarction? A case-crossover analysis in the Stockholm Heart Epidemiology Program (SHEEP) Psychosom Med. 1999;61:842–849. doi: 10.1097/00006842-199911000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Selvi Y, Aydin A, Gumrukcuoglu HA, Gulec M, Besiroglu L, Ozdemir PG, Kilic S. Dream anxiety is an emotional trigger for acute myocardial infarction. Psychosomatics. 2011;52:544–549. doi: 10.1016/j.psym.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 21.Canto JG, Iskandrian AE. Major risk factors for cardiovascular disease. JAMA. 2003;290:947–949. doi: 10.1001/jama.290.7.947. [DOI] [PubMed] [Google Scholar]
- 22.Fox K, Dabbous O, Goldberg R, Pieper KS, Eagle KA, Van de Werf F, Avezum A, Goodman SG, Flather MD, Anderson FA, Granger CB. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE) BMJ. 2006;333:1091. doi: 10.1136/bmj.38985.646481.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steptoe A, Wikman A, Molloy GJ, Kaski J-C. Anaemia and the development of depressive symptoms following acute coronary syndrome: longitudinal clinical observational study. BMJ Openz. 2012;2 doi: 10.1136/bmjopen-2011-000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.French DP, Senior V, Weinman J, Marteau TM. Causal attributions for heart disease: a systematic review. Psychol Health. 2001;16:77–98. [Google Scholar]
- 25.Strike PC, Steptoe A. Psychosocial factors in the development of coronary artery disease. Prog Cardiovasc Dis. 2004;46:337–347. doi: 10.1016/j.pcad.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 26.Strike PC, Steptoe A. Behavioral and emotional triggers of acute coronary syndromes: a systematic review and critique. Psychosom Med. 2005;67:179–186. doi: 10.1097/01.psy.0000155663.93160.d2. [DOI] [PubMed] [Google Scholar]
- 27.Petrie KJ, Weinman J. Patients' perceptions of their illness: the dynamo of volition in health care. Curr Dir Psychol Sci. 2012;21:60–65. [Google Scholar]
- 28.Davidson KW, Holderby AD, Willis S, Barksdale CD, Richardson TN, Loppie CJ, Van Roosmalen EH. Three top Canadian and personal health concerns of a random sample of Nova Scotian women. Can J Public Health. 2000;22:S172. doi: 10.1007/BF03404845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steptoe A, Molloy GJ, Messerli-Bürgy N, Wikman A, Randall G, Perkins-Porras L, Kaski JC. Fear of dying and inflammation following acute coronary syndrome. Eur Heart J. 32:2405–2411. doi: 10.1093/eurheartj/ehr132. [DOI] [PubMed] [Google Scholar]
- 30.Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavorial medicine. Ann Behav Med. 1994;16:199–202. [Google Scholar]
- 31.US Department of Health and Human Services Food and Drug Administration. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims. 2009 [Google Scholar]
- 32.Bild DE, Bluemke DA, Burke GL, Detrano R, Roux AVD, Folsom AR, Greenland P, Jacobs DR, Jr, Kronmal R, Liu K. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 33.Folsom AR, Wu KK, Rosamond WD, Sharrett AR, Chambless LE. Prospective study of hemostatic factors and incidence of coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 1997;96:1102–1108. doi: 10.1161/01.cir.96.4.1102. [DOI] [PubMed] [Google Scholar]
- 34.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 35.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–1143. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 36.Strike PC, Wardle J, Steptoe A. Mild acute inflammatory stimulation induces transient negative mood. J Psychosom Res. 2004;57:189–194. doi: 10.1016/S0022-3999(03)00569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Warren-Gash C, Smeeth L, Hayward AC. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: a systematic review. Lancet Infect Dis. 2009;9:601–610. doi: 10.1016/S1473-3099(09)70233-6. [DOI] [PubMed] [Google Scholar]
- 38.Wittstein IS. Stress cardiomyopathy: a syndrome of catecholamine-mediated myocardial stunning? Cell Mol Neurobiol. 2012:1–11. doi: 10.1007/s10571-012-9804-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hamer M, Batty GD, Seldenrijk A, Kivimaki M. Antidepressant medication use and future risk of cardiovascular disease: the Scottish Health Survey. Eur Heart J. 2011;32:437–442. doi: 10.1093/eurheartj/ehq438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol Psychiatry. 2010;67:1067–1074. doi: 10.1016/j.biopsych.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 41.Lichtman JH, Bigger JT, Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES. Depression and coronary heart disease recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 42.Grippo AJ, Sgoifo A, Mastorci F, McNeal N, Trahanas DM. Cardiac dysfunction and hypothalamic activation during a social crowding stressor in prairie voles. Auton Neurosci. 2010;156:44–50. doi: 10.1016/j.autneu.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stojičić S, Milutinović-Smiljanić S, Šarenac O, Milosavljevic S, Paton JFR, Murphy D, Japundzic-Zigon N. Blockade of central vasopressin receptors reduces the cardiovascular response to acute stress in freely moving rats. Neuropharmacology. 2008;54:824–836. doi: 10.1016/j.neuropharm.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 44.Cyr NE, Dickens MJ, Romero LM. Heart rate and heart-rate variability responses to acute and chronic stress in a wild-caught passerine bird. Physiol Biochem Zool. 2009;82:332–344. doi: 10.1086/589839. [DOI] [PubMed] [Google Scholar]
- 45.Skinner JE, Lie J, Entman M. Modification of ventricular fibrillation latency following coronary artery occlusion in the conscious pig. Circulation. 1975;51:656–667. doi: 10.1161/01.cir.51.4.656. [DOI] [PubMed] [Google Scholar]
- 46.Sgoifo A, De Boer SF, Buwalda B, Korte-Bouws G, Tuma J, Bohus B, Zaagsma J, Koolhaas JM. Vulnerability to arrhythmias during social stress in rats with different sympathovagal balance. Am J Physiol Heart Circ Physiol. 1998;275:H460–H466. doi: 10.1152/ajpheart.1998.275.2.H460. [DOI] [PubMed] [Google Scholar]
- 47.Sgoifo A, Stilli D, de Boer SF, Koolhaas JM, Musso E. Acute social stress and cardiac electrical activity in rats. Aggress Behav. 1998;24:287–296. [Google Scholar]
- 48.Stemmler G, Aue T, Wacker J. Anger and fear: separable effects of emotion and motivational direction on somatovisceral responses. Int J Psychophys. 2007;66:141–153. doi: 10.1016/j.ijpsycho.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 49.Grippo AJ. The utility of animal models in understanding links between psychosocial processes and cardiovascular health. Soc Pers Psyc Comp. 2011;5:164–179. doi: 10.1111/j.1751-9004.2011.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rozanski A, Bairey CN, Krantz DS, Friedman J, Resser KJ, Morell M, Hilton-Chalfen S, Hestrin L, Bietendorf J, Berman DS. Mental stress and the induction of silent myocardial ischemia in patients with coronary artery disease. N Engl J Med. 1988;318:1005–1012. doi: 10.1056/NEJM198804213181601. [DOI] [PubMed] [Google Scholar]
- 51.Stone PH, Krantz DS, McMahon RP, Goldberg AD, Becker LC, Chaitman BR, Taylor HA, Cohen JD, Freedland KE, Bertolet BD, Coughlan C, Pepine CJ, Kaufmann PG, Sheps DS for the PIMI Study Group. Relationship among mental stress-induced ischemia and ischemia during daily life and during exercise: the Psychophysiologic Investigations of Myocardial Ischemia (PIMI) study. J Am Coll Cardiol. 1999;33:1476–1484. doi: 10.1016/s0735-1097(99)00075-3. [DOI] [PubMed] [Google Scholar]
- 52.Burg MM, Jain D, Soufer R, Kerns RD, Zaret BL. Role of behavioral and psychological factors in mental stress-induced silent left ventricular dysfunction in coronary artery disease. J Am Coll Cardiol. 1993;22:440–448. doi: 10.1016/0735-1097(93)90048-6. [DOI] [PubMed] [Google Scholar]
- 53.Strike PC, Magid K, Whitehead DL, Brydon L, Bhattacharyya MR, Steptoe A. Pathophysiological processes underlying emotional triggering of acute cardiac events. Proc Natl Acad Sci USA. 2006;103:4322. doi: 10.1073/pnas.0507097103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Braunwald E. Unstable angina: an etiologic approach to management. Circulation. 1998;98:2219–2222. doi: 10.1161/01.cir.98.21.2219. [DOI] [PubMed] [Google Scholar]
- 55.Liao D, Carnethon M, Evans GW, Cascio WE, Heiss G. Lower heart rate variability is associated with the development of coronary heart disease in individuals with diabetes. Diabetes. 2002;51:3524–3531. doi: 10.2337/diabetes.51.12.3524. [DOI] [PubMed] [Google Scholar]
- 56.Strike PC, Perkins-Porras L, Whitehead DL, McEwan J, Steptoe A. Triggering of acute coronary syndromes by physical exertion and anger: clinical and sociodemographic characteristics. Heart. 2006;92:1035. doi: 10.1136/hrt.2005.077362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Steptoe A, Brydon L. Emotional triggering of cardiac events. Neurosci Biobehav Rev. 2009;33:63–70. doi: 10.1016/j.neubiorev.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 58.Blumenthal JA, Jiang W, Babyak MA, Krantz DS, Frid DJ, Coleman RE, Waugh R, Hanson M, Appelbaum M, O'Connor C, Morris JJ. Stress management and exercise training in cardiac patients with myocardial ischemia: effects on prognosis and evaluation of mechanisms. Arch Intern Med. 1997;157:2213. [PubMed] [Google Scholar]
- 59.Blumenthal JA, Jiang W, Waugh RA, Frid DJ, Morris JJ, Coleman RE, Hanson M, Babyak M, Thyrum ET, Krantz DS, O'Connor C. Mental stress-induced ischemia in the laboratory and ambulatory ischemia during daily life: association and hemodynamic features. Circulation. 1995;92:2102–2108. doi: 10.1161/01.cir.92.8.2102. [DOI] [PubMed] [Google Scholar]
- 60.Gabbay FH, Krantz DS, Kop WJ, Hedges SM, Klein J, Gottdiener JS, Rozanski A. Triggers of myocardial ischemia during daily life in patients with coronary artery disease: physical and mental activities, anger and smoking. J Am Coll Cardiol. 1996;27:585–592. doi: 10.1016/0735-1097(95)00510-2. [DOI] [PubMed] [Google Scholar]
- 61.Shimbo D, Child J, Davidson K, Geer E, Osende JI, Reddy S, Dronge A, Fuster V, Badimon JJ. Exaggerated serotonin-mediated platelet reactivity as a possible link in depression and acute coronary syndromes. Am J Cardiol. 2002;89:331. doi: 10.1016/s0002-9149(01)02236-6. [DOI] [PubMed] [Google Scholar]
- 62.Wilson PWF, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 63.Taggart P, Critchley H, Lambiase PD. Heart–brain interactions in cardiac arrhythmia. Heart. 2011;97:698–708. doi: 10.1136/hrt.2010.209304. [DOI] [PubMed] [Google Scholar]
- 64.Gussak I, Antzelevitch C. Early repolarization syndrome: clinical characteristics and possible cellular and ionic mechanisms. J Electrocardiol. 2000;33:299–309. doi: 10.1054/jelc.2000.18106. [DOI] [PubMed] [Google Scholar]
- 65.Bhattacharyya MR, Steptoe A. Emotional triggers of acute coronary syndromes: strength of evidence, biological processes, and clinical implications. Prog Cardiovasc Dis. 2007;49:353–365. doi: 10.1016/j.pcad.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 66.Matthews KA, Owens JF, Kuller LH, Sutton-Tyrrell K, Jansen-McWilliams L. Are hostility and anxiety associated with carotid atherosclerosis in healthy postmenopausal women? Psychosom Med. 1998;60:633–638. doi: 10.1097/00006842-199809000-00021. [DOI] [PubMed] [Google Scholar]
- 67.Joynt KE, O'Connor CM. Lessons from SADHART, ENRICHD, and other trials. Psychosom Med. 2005;67(Suppl. 1):S63–S66. doi: 10.1097/01.psy.0000163454.25036.fc. [DOI] [PubMed] [Google Scholar]