Abstract
Hematological malignancy patients not referred by their primary hematologist/medical oncologist suffer disparate access to allogeneic hematopoietic cell transplantation (HCT). However, investigation into physician, system and patient factors relevant to this decision making is lacking. We surveyed a national randomized sample of practicing hematologists/medical oncologists identified through the AMA (American Medical Association) masterfile. A modified Dillman approach was utilized to encourage survey response. From 1200 surveyed, a total of 113 physicians responded. In all, 68% were male, 62% identified as White/non-Hispanic, 79% practiced in non-academic settings and 80% reported spending 75–100% of their professional effort in clinical care. Using clinical vignettes, we detected significantly increased odds for HCT non-referral according to age (age 60 vs 30, odds ratio (OR) 8.3, 95% confidence interval (CI): 5.9–11.7, P<0.0001), insurance coverage (no coverage vs coverage, OR 6.9, 95% CI: 5.2–9.1, P<0.0001) and race (African–American vs Caucasian, OR 2.4, 95% CI: 1.9–2.9, P<0.0001). Physician (perception of HCT risks), system (insurance coverage) and patient (age, social support and co-morbid illness) factors were strongly endorsed by respondents as important determinants of their HCT referral practices. These data speak to important factors relevant to HCT referral practices, and highlight several opportunities for education and intervention to reduce current disparities.
Keywords: physician survey, health disparities, hematopoietic cell transplantation
INTRODUCTION
Important advances in allogeneic hematopoietic cell transplantation (HCT) have afforded improved outcomes. However, as these benefits have not been realized by all, the study of health disparities has relevance to the field.
Several areas of disparity have been previously reported. One important area of disparity is that of access to HCT. For patients without a matched sibling donor, the likelihood of finding a suitably matched unrelated donor varies according to race/ ethnicity.1 Other factors may determine access as well.2 Utilization of autologous and allogeneic HCT differs according to age, gender, race, education, insurance status, center factors and patient comorbidities.3–7 Disparities by race and socioeconomic status have also been documented in outcomes of HCT.8–11
In the continuum of care for patients with hematological malignancies, an important decision point involves the judgment of the patient’s primary hematologist/oncologist to consider referral to a blood and marrow transplant specialist. An individual patient’s opportunity to realize the benefits of this therapy is dependent on his/her access to this specialized service. However, systematic investigation into practice variation in HCT referral is lacking. Knowledge of factors involved in differential access to HCT would provide the first steps toward diminishing this disparity.
Accordingly, we conducted a national survey of hematologists/ oncologists to characterize practice variation in referral for HCT using a series of clinical vignettes, and to elucidate physician, system and patient factors, which inform these decisions.
MATERIALS AND METHODS
Development of survey instrument
A survey instrument was developed with content organized into three sections: (1) best–worst scaling of clinical vignettes describing patients by age, gender, race and insurance coverage; (2) examination of physician, system and patient factors relevant to decision making; and (3) respondent socio-demographic information. Modifications to the instrument were made based on input from semi-structured interviewing and focus group work conducted with HCT physicians, as well as academic and community hematologists/oncologists. Further modifications were made based on content validity, face validity and ability to complete the survey within the anticipated time. The final survey was reached by consensus among the investigators. Identical paper and web-based versions were produced (available upon request).
Survey structure
A cover page identified the study aims, investigators, provided participant’s rights and responsibilities, and described incentive for participation. An initial screening question excluded respondents who personally conduct HCT. In Section 1, best–worst scaling tasks were conducted for four disease conditions: AML in first CR (CR1); ALL in CR1; CML that failed tyrosine kinase inhibitor; and IPSS intermediate – 2 myelodysplastic syndrome. These were chosen, as literature supports HCT as an effective strategy. For each, four permutations in four binary factors including age (30 years vs 60 years), gender (male vs female), race (Caucasian vs African–American) and insurance coverage (HCT coverage vs no coverage), were presented. From each set, the respondent first identified the best case for HCT referral. From the remaining three cases, the respondent identified the worst case. The same three sets of four vignettes were asked for each of the four disease conditions (that is, a total of 12 best–worst scaling tasks).12
In section 2, respondents identified their endorsement for physician, system and patient factors’ contribution to their decision making in an ordinal scale ranging from strongly disagree to strongly agree. Physician factors included the following: prior experience with HCT outcomes; adequacy of prior training in HCT during hematology/oncology fellowship; knowledge of current HCT outcomes; perception regarding HCT associated morbidity/mortality; understanding of indications for HCT; perceived risk after unrelated vs sibling HCT; and decision to wait until relapse before recommending HCT. System factors included: access to HCT providers distance to closest HCT center and insurance coverage for HCT. Patient factors included: age; availability of sibling donor; primary language other than English; familial/social support system; history of medical non-compliance; education/understanding of medical conditions; co-morbid medical or psychiatric illness; and alcohol or substance abuse.
In section 3, respondents reported their own socio-demographic data (gender, race/ethnicity and duration of practice) and practice (academic/ not, urban/rural, distance to closest HCT center, % professional effort in clinical care, % of patients in practice with hematological malignancies) characteristics.
Survey distribution and data collection
We conducted a national survey of hematologists/oncologists practicing in the United States. This study was approved by the University of South Florida Institutional Review Board. An unbiased sample was obtained from the AMA (American Medical Association) masterfile. From a total 8676 (2515 Hematology and 6161 Oncology) providers, we obtained a nationally representative random sample of 1200 physicians, with oversampling of hematologists (3:1) over medical oncologists. As we expected no >25–30% response rate,13–15 we anticipated 300 respondents.
A modified Dillman approach (see Dillman, 197816) was utilized.15–18 Three waves of mailing were performed in February, March and April, 2011. Each mailing contained an introduction, instructions on how to complete the web-based electronic survey and a paper copy of the survey with postage-paid return envelope. The first contained a $5.00 gift card. All return correspondence (email to study investigator or returned survey materials) was tracked; reasons for non-participation were recorded.
On the basis of low-response rate, two additional waves were distributed in June and July of 2011 to the original 1200 physicians. In this revised mailing, the introductory page explained the prior low-response rate and promised a $20.00 incentive. As identifying information was not collected in the preceding waves, we could not determine if respondents had previously responded.
Statistical methods
While the primary intention of this survey was exploratory, we hypothesized that age, gender, race and insurance coverage influenced HCT referral and that this influence varies by disease condition (section 1). Using logistic regression with respondent-level clustering and STATA software, we estimated the odd ratios of no HCT referral by binary vignette attributes: age, gender, race and insurance coverage for HCT. As maximum likelihood logit coefficients are estimated on a log-odds scale, the odds ratio (OR) estimates represent geometric means and have asymmetric confidence intervals. Furthermore, we stratified the OR by disease condition and test the equivalence in log-odds across conditions using Wald tests.
Section 2 and 3 responses were summarized utilizing descriptive statistics. For the purpose of summarizing response to ordinal scale items in section 2, we defined ‘agree’ and ‘strongly agree’ as affirmative responses, ‘disagree’ and ‘strongly disagree’ as negative responses, and ‘neither agree or disagree’ as neutral. We determined association between response to items in section 2 and socio-demographic variables in section 3 with Cochran–Armitage trend test or γ-test.
RESULTS
Respondent characteristics
A total of 113 physicians completed the survey, including 91 paper and 22 web-based responses. Respondents after the first three waves were 16, 36 and 17; following the two additional waves, 31 and 13 responded. Socio-demographic and practice characteristics are described in Table 1. Of the 1200 physicians surveyed, a total of 34 actively declined participation. Reasons included the following: personally perform HCT (n=16); declined with no reason (n=8); do not see hematological malignancy patients (n=5); objected to survey based on questions on race (n=3); and not interested (n=2). One was returned undeliverable. A total of seven returned the gift card.
Table 1.
Socio-demographic and clinical practice characteristics of physician survey respondents
| Frequency | Percentage | |
|---|---|---|
| Practice type | ||
| Academic | 23 | 21% |
| Not academic | 89 | 79% |
| Practice setting | ||
| Urban | 87 | 78% |
| Rural | 24 | 22% |
| Distance to closest HCT center | ||
| At center | 16 | 14% |
| Within 10 miles | 25 | 22% |
| Within 25 miles | 20 | 18% |
| Within 50 miles | 11 | 10% |
| >50 miles | 40 | 36% |
| % Effort in clinical care | ||
| <25% | 6 | 5% |
| 25–49% | 4 | 4% |
| 50–74% | 12 | 11% |
| 75–100% | 90 | 80% |
| Proportion of patients with hematological malignancies | ||
| <25% | 62 | 57% |
| 25–49% | 39 | 36% |
| 50–74% | 2 | 2% |
| 75–100% | 6 | 6% |
| Years in practice since Hematology/Oncology fellowship training | ||
| <5 | 14 | 13% |
| 5–9 | 25 | 22% |
| 10–14 | 31 | 28% |
| 15–19 | 16 | 14% |
| ≥20 | 26 | 23% |
| Gender | ||
| Male | 74 | 68% |
| Female | 35 | 32% |
| Race/ethnicity | ||
| White, non-Hispanic | 68 | 62% |
| Hispanic | 7 | 6% |
| Black/African–American | 32 | 29% |
| Asian | 0 | 0% |
| Hawaiian/Pacific Islander | 0 | 0% |
| American Indian or Alaska native | 3 | 3% |
Abbreviation: HCT=hematopoietic cell transplantation.
OR of no HCT referral
Table 2 provides the OR of no HCT referral. Sixty-year-old patients and patients without HCT coverage were less likely to be referred than their younger, better-insured counterparts. African–American patients were less likely to be referred than Caucasian patients. These results did not differ when the study sample was restricted to exclude those respondents with <25% of their practice comprised of hematological malignancy patients.
Table 2.
OR for no HCT referralb
| ORa | 95% | CI | P value | |
|---|---|---|---|---|
| Age | ||||
| 60 years vs 30 years | 8.29 | 5.89 | 11.69 | <0.001 |
| Gender | ||||
| Female vs male | 0.83 | 0.69 | 0.99 | 0.042 |
| Race | ||||
| African–American vs Caucasian | 2.35 | 1.93 | 2.87 | <0.001 |
| Insurance: | ||||
| No HCT coverage vs HCT coverage | 6.95 | 5.32 | 9.07 | <0.001 |
Abbreviations: CI=confidence interval; HCT=hematopoietic cell transplantation; OR=odds ratio.
OR represents no HCT referral.
Additional analyses were conducted on the sub-sample of respondents reporting hematologic malignancy patients comprising >25% of their practice. Results were not affected (age: OR 10.5 (95% CI: 6.5–17.1), P<0.0001; gender: OR 0.88 (95% CI: 0.68–1.1), P=0.32; race OR 2.38 (95% CI: 1.78–3.2), P<0.0001; and insurance: OR 6.7 (95% CI: 4.84–9.3), P<0.0001).
Figure 1 illustrates condition-specific OR. All condition-specific OR are statistically significant at 0.05, except for gender among ALL and AML patients. The four attribute-specific Wald tests reject equivalence in OR across the four diseases at a P-value <0.05, indicating condition-specific variability.
Figure 1.
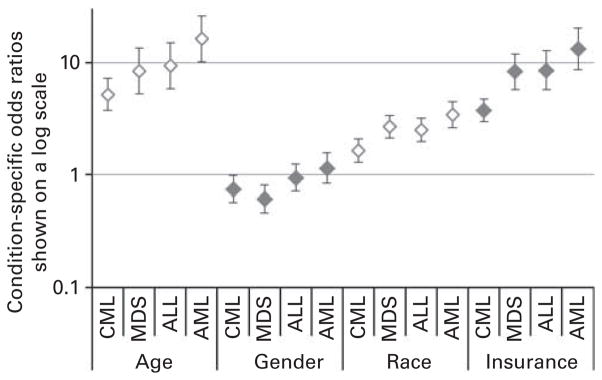
Condition-specific OR of no HCT referral.
Physician factors
Surveyed physicians largely reported confidence in their prior training, understanding of HCT indications and outcomes, and comfort in discussing these points with their patients. The majority (73%) indicated that they have had adequate HCT training in their fellowship; 88% indicated that they feel comfortable in knowing when to refer patients for HCT consultation; and 54% indicated that they feel comfortable discussing current HCT outcomes with patients. Previous experiences did not appear to adversely affect likelihood for HCT referral. The majority of physicians (77%) disagreed with the statement that ‘My patients have not done well with transplant, so I am reluctant to refer people for HCT consultation.’
Conversely, the majority of physicians indicated that they perceive the risks of HCT to be great and that this perceived risk influences their decision making in referral. The majority (51%) indicated that they agree with the statement, ‘I feel the risk (morbidity and mortality) after HCT is very high,’ most (57%) indicated that they ‘feel outcomes of unrelated donor HCT are much worse than matched sibling HCT.’ Interestingly, 32% agreed that, ‘Because of the high risks of allogeneic HCT, I refer only after failure of conventional chemotherapy.’
System factors
Physical access to HCT centers was not a major factor in decision making for surveyed physicians. The minority (11%) of surveyed physicians agreed that access to HCT physicians limits their referral of appropriate HCT candidates, and only 15% agreed that the physical distance to the closest HCT center influenced their decision making. Lack of insurance coverage, however, was perceived as an obstacle by 64%.
Patient factors
The majority (92%) indicated that patient age influences their decisions on HCT referral. The reported upper age limit in which physicians would consider referral for allogeneic HCT varied: age >75 (9%), 70–75 (8%), 65–70 (31%), 60–65 (32%), 55–60 (13%), 50–55 (5%), 45–50 (2%) and 35–40 (1%). Thirty-one percent indicated that they are less likely to refer for HCT consultation in those patients without siblings. Only 8% agreed that patients’ primary language, other than English, was important. Perceptions regarding patients’ environment, support and past behavior were endorsed as highly important: 57% indicated that they are less likely to refer patients without good social support, 77% were less likely to refer patients with medical non-compliance and 49% were less likely to refer patients with poor understanding of their medical conditions. As well, co-morbid issues factored strongly into physicians’ decision making: 48, 54 and 77% of physicians agreed that they were less likely to refer patients with co-morbid medical, psychiatric or alcohol and substance abuse issues. We did not observe any significant changes in the observed responses to these items dealing with physician, system and patient factors when we restricted the study sample to eliminate those respondents with <25% of their practice comprised of hematological malignancy patients.
Physicians’ perceptions on patient access to HCT
Interestingly, 64% responded ‘no’ to the question, ‘Do you feel that all patients have equal access to HCT consultation?’ Physicians were then asked, ‘If not, what do you think could be done to address this?’ Qualitative comments (n=57) provided in response brought even greater clarity to perceived barriers to HCT referral. The majority of these (n=29, or 60%) related to insurance coverage. Ten physicians (18%) indicated that greater education is needed on indications and timing for HCT referral. Four (7%) indicated that improvements are needed in HCT center outreach. Five (9%) described the need for support in addressing social/ support barriers. Two (4%) suggested improvements in patient education. The remainder (n=1 each) included ‘increased number of HCT centers,’ ‘increased published data demonstrating benefit of HCT over non-HCT therapies, particularly in MDS,’ ‘telephone or web-based consultation,’ ‘increased representation of racial/ethnic minorities in donor registries,’ ‘not sure,’ and ‘not an issue.’ One reported, ‘Nothing can be done. Disparities will always be there.’
Association between physician demographic/practice variables and response
Non-academic physicians were more likely to consider patient age (P=0.04) and to not refer those patients with poor support (P=0.009). Rural physicians were less likely to refer patients with co-morbid medical (P=0.009) or alcohol/substance issues (P=0.004). We could not detect significant association between proximity to closest HCT center and any of the studied physician, system or patient factors relevant to decision making. Physicians with a greater proportion of professional effort spent in clinical care were less likely to endorse insurance coverage as a barrier (P=0.002), less likely to consider non-English primary language in their decision making (P=0.04) and were less likely to endorse patients’ support system as important to referral (P=0.002). Physicians with a greater proportion of hematological malignancy patients in their practice were more likely to endorse adequate HCT training in hematology/oncology fellowship training (P=0.05), to be comfortable in discussing current HCT outcomes (P=0.0008), be comfortable in indications for HCT referral (P=0.04), to endorse distance to closest HCT center as a factor (P=0.03), to describe lack of insurance coverage as a barrier (P=0.02) and to consider perceived medical non-compliance as a deterrent (P=0.04). Physicians with a shorter duration of practice were more likely to report adequate HCT training in their hematology/oncology fellowship (P<0.0001) and were more likely to report that they felt comfortable in knowing HCT indications and timing of referral (P=0.02).
DISCUSSION
Proposing that practicing hematologists/oncologists act as gate-keepers to HCT access, we have conducted a national survey to directly understand what factors influence referral for HCT. A majority of respondents acknowledged biases against older, underinsured and African–American patients and that disparate access exists. These results identify several key areas for physician education and intervention.
Although most respondents reported adequate training, understanding appears to be undermined by the fact that 22 and 23% of respondents indicated that they either ‘neither agree or disagree’ or ‘disagree’ with the statement that they ‘feel comfortable discussing current HCT outcomes’ with their patients. As well, 18% of qualitative comments received argued for increased education of hematologists/medical oncologists in training about HCT referral indications. Finally, as 32% asserted HCT referral only after failure of conventional chemotherapy, these data indicate patients may miss the opportunity for appropriately timed HCT referral to maximize their chances of successful outcome. Thus, education on appropriate indications and timing for HCT referral is of utmost importance. Physicians with smaller numbers of hematological malignancy patients in their usual practice and those with greater durations of practice as completing fellowship training may be particularly suited for targeted education.
As well, perceptions regarding HCT risk appear to be another important area for targeted education. The majority agreed that ‘risks for morbidity and mortality following HCT are very high,’ and agreed that ‘outcomes of unrelated donor HCT are much worse than when an HLA-identical sibling is available.’ These data speak to the need for targeted education on current data demonstrating reduced mortality after HCT, as well as suggesting comparable outcomes between matched unrelated and sibling donor HCT.19–27
Access to HCT providers and distance to the closest HCT center did not emerge as major factors. These data should be interpreted with caution, as only 36% reported that the closest HCT center was >50 miles from their office. Despite this, a minority (15%) did report that distance to the closest HCT center was a deterrent in referral for HCT consultation. Importantly, it should be noted that Gratwohl et al.28 have previously demonstrated correlation between autologous and allogeneic HCT utilization and HCT team density in an analysis from the European Group for Blood and Marrow Transplantation. Comments provided by survey respondents here may suggest solutions: enhanced outreach from HCT centers, as well as remote consultation via alternative methods may facilitate access. The most consistent system-based factor at work in physician referral decisions, however, was lack of insurance coverage. This was clearly identified as a fundamental barrier throughout the relevant survey items and was the central theme addressed by physician comments.
Finally, these data suggest that a number of individual patient factors strongly influence physician decision making. The upper limit of age for HCT referral appears discordant with consensus among HCT providers. As peak incidence of many conditions appropriate for HCT referral occurs in these age ranges, patients may miss an opportunity to consider HCT as a therapeutic option. As evidence continues to mount that older patients can benefit from HCT, decisions about therapy would be best made in concert with a transplant specialist. Next, the data support the notion that physicians are less likely to refer African–American patients despite clear disease-based indications for HCT referral. As one respondent stated, ‘race has to do with availability of unrelated donors,’ perception of availability of a donor may dissuade physicians from considering HCT referral. Poor social support and limited understanding were deterrents for HCT referral. This practice may widen an existing gap in access such vulnerable patients. Finally, co-morbid medical, psychiatric and addiction issues were deterrents to HCT referral. These data are particularly noteworthy. In contrast to increased understanding among HCT providers in risk determination,29 these data suggest that hematologist/oncologists may consider co-morbid problems as more absolute barriers to HCT referral. Self-identified rural and non-academic physicians appear to be particularly suited to targeted education here.
Although these findings provide novel insights into factors at work in HCT referral decisions, we acknowledge limitations. First, despite established methods for enhancing response, the response rate was lower than anticipated. Although we have aimed to minimize bias through sampling of a geographically stratified, randomly selected, nationally representative study sample, we can not assure that the survey respondents do not differ in important ways from non-responders. Specific comparison of demographic information such as practice size and percent effort devoted to clinical care is not collected in the AMA database. As well, state and zip code of respondents’ address were not uniformly collected, rather only in the final waves of mailing to allow provision of the additional incentive. Comparison of state and zip code of residence of this subset of respondents (n=37) to that of the original AMA sample, however, did not demonstrate significant difference. Thus, this provides some assurance that survey respondents are comparable to the initial study sample. Next, as the survey was necessarily limited in terms of practical scope, we could not examine all potential clinical scenarios or investigate all possible factors at work in decision making.
In total, these data provided by practicing hematologists/ oncologists facilitate insight into factors relevant to HCT referral and suggest several educational and interventional means to reduce disparate access to HCT. With appropriate access to HCT consultation, patients would be better equipped to make informed decisions about their therapy.
Acknowledgments
The authors thank the staff in Dr Craig’s lab at Lee H Moffitt Cancer Center and Research Institute for their contributions to the research and creation of this paper: Shannon Hendrix-Buxton (best–worst scaling design) and Carol Templeton (copy editing). This study was supported by Interdisciplinary Health Disparities Pilot Research Grant (sponsored by USF/Moffitt Transdisciplinary Center to Address Cancer Health Disparities P20 MD003375-02, PI Richard Roetzheim, MD, MSPH): Practice variation in referral for hematopoietic cell transplantation. (PI: Pidala, J)
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest
References
- 1.Anasetti C, Hillgruber R, Nye V, Ayala E, Kharfan-Dabaja M, Fernandez H, et al. Patient ethnicity markedly affects the probability of finding an HLA-A, B, C, and DRB1 allele matched unrelated donor for hemopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16:S172. [Google Scholar]
- 2.Majhail NS, Omondi NA, Denzen E, Murphy EA, Rizzo JD. Access to hematopoietic cell transplantation in the United States. Biol Blood Marrow Transplant. 2010;16:1070–1075. doi: 10.1016/j.bbmt.2009.12.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho C. Factors affecting stem cell transplantation for leukemia and lymphoma. Available at http://hdl.handle.net/1961/3595.
- 4.Hwang JP, Lam TP, Cohen DS, Donato ML, Geraci JM. Hematopoietic stem cell transplantation among patients with leukemia of all ages in Texas. Cancer. 2004;101:2230–2238. doi: 10.1002/cncr.20628. [DOI] [PubMed] [Google Scholar]
- 5.Mehta P, Pollock BH, Nugent M, Horowitz M, Wingard JR. Access to stem cell transplantation: do women fare as well as men? Am J Hematol. 2003;72:99–102. doi: 10.1002/ajh.10273. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell JM, Meehan KR, Kong J, Schulman KA. Access to bone marrow transplantation for leukemia and lymphoma: the role of sociodemographic factors. J Clin Oncol. 1997;15:2644–2651. doi: 10.1200/JCO.1997.15.7.2644. [DOI] [PubMed] [Google Scholar]
- 7.Joshua T, Rizzo JD, Zhang MJ, Horowitz MM. Access to hematopoietic stem cell transplantation: effect of race and gender (abstract) Biol Blood Marrow Transplant. 2007;13(Suppl):22. [Google Scholar]
- 8.Baker KS, Davies SM, Majhail NS, Hassebroek A, Klein JP, Ballen KK, et al. Race and socioeconomic status influence outcomes of unrelated donor hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2009;15:1543–1554. doi: 10.1016/j.bbmt.2009.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker KS, Loberiza FR, Jr, Yu H, Cairo MS, Bolwell BJ, Bujan-Boza WA, et al. Outcome of ethnic minorities with acute or chronic leukemia treated with hematopoietic stem-cell transplantation in the United States. J Clin Oncol. 2005;23:7032–7042. doi: 10.1200/JCO.2005.01.7269. [DOI] [PubMed] [Google Scholar]
- 10.Serna DS, Lee SJ, Zhang MJ, Baker S, Eapen M, Horowitz MM, et al. Trends in survival rates after allogeneic hematopoietic stem-cell transplantation for acute and chronic leukemia by ethnicity in the United States and Canada. J Clin Oncol. 2003;21:3754–3760. doi: 10.1200/JCO.2003.03.133. [DOI] [PubMed] [Google Scholar]
- 11.Silla L, Fischer GB, Paz A, Daudt LE, Mitto I, Katz B, et al. Patient socioeconomic status as a prognostic factor for allo-SCT. Bone Marrow Transplant. 2009;43:571–577. doi: 10.1038/bmt.2008.358. [DOI] [PubMed] [Google Scholar]
- 12.Flynn TN, Louviere JJ, Peters TJ, Coast J. Best–worst scaling: what it can do for health care research and how to do it. J Health Econ. 2007;26:171–189. doi: 10.1016/j.jhealeco.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 14.McCloskey SA, Tao ML, Rose CM, Fink A, Amadeo AM. National survey of perspectives of palliative radiation therapy: role, barriers, and needs. Cancer J. 2007;13:130–137. doi: 10.1097/PPO.0b013e31804675d4. [DOI] [PubMed] [Google Scholar]
- 15.Thorpe C, Ryan B, McLean SL, Burt A, Stewart M, Brown JB, et al. How to obtain excellent response rates when surveying physicians. Fam Pract. 2009;26:65–68. doi: 10.1093/fampra/cmn097. [DOI] [PubMed] [Google Scholar]
- 16.Dillman DA. In: Mail and telephone surveys: the total design method. Sons JWa., editor. Wiley; New York: 1978. [Google Scholar]
- 17.Field TS, Cadoret CA, Brown ML, Ford M, Greene SM, Hill D, et al. Surveying physicians: do components of the ‘Total Design Approach’ to optimizing survey response rates apply to physicians? Med Care. 2002;40:596–605. doi: 10.1097/00005650-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev. 2007;2:MR000008. doi: 10.1002/14651858.MR000008.pub3. [DOI] [PubMed] [Google Scholar]
- 19.Arora M, Weisdorf DJ, Spellman SR, Haagenson MD, Klein JP, Hurley CK, et al. HLA-identical sibling compared with 8/8 matched and mismatched unrelated donor bone marrow transplant for chronic phase chronic myeloid leukemia. J Clin Oncol. 2009;27:1644–1652. doi: 10.1200/JCO.2008.18.7740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta V, Tallman MS, He W, Logan BR, Copelan E, Gale RP, et al. Comparable survival after HLA-well-matched unrelated or matched sibling donor transplantation for acute myeloid leukemia in first remission with unfavorable cytogenetics at diagnosis. Blood. 2010;116:1839–1848. doi: 10.1182/blood-2010-04-278317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hows JM, Passweg JR, Tichelli A, Locasciulli A, Szydlo R, Bacigalupo A, et al. Comparison of long-term outcomes after allogeneic hematopoietic stem cell transplantation from matched sibling and unrelated donors. Bone Marrow Transplant. 2006;38:799–805. doi: 10.1038/sj.bmt.1705531. [DOI] [PubMed] [Google Scholar]
- 22.Moore J, Nivison-Smith I, Goh K, Ma D, Bradstock K, Szer J, et al. Equivalent survival for sibling and unrelated donor allogeneic stem cell transplantation for acute myelogenous leukemia. Biol Blood Marrow Transplant. 2007;13:601–607. doi: 10.1016/j.bbmt.2007.01.073. [DOI] [PubMed] [Google Scholar]
- 23.Ringden O, Pavletic SZ, Anasetti C, Barrett AJ, Wang T, Wang D, et al. The graft-versus-leukemia effect using matched unrelated donors is not superior to HLA-identical siblings for hematopoietic stem cell transplantation. Blood. 2009;113:3110–3118. doi: 10.1182/blood-2008-07-163212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schetelig J, Bornhauser M, Schmid C, Hertenstein B, Schwerdtfeger R, Martin H, et al. Matched unrelated or matched sibling donors result in comparable survival after allogeneic stem-cell transplantation in elderly patients with acute myeloid leukemia: a report from the cooperative German Transplant Study Group. J Clin Oncol. 2008;26:5183–5191. doi: 10.1200/JCO.2007.15.5184. [DOI] [PubMed] [Google Scholar]
- 25.Walter RB, Pagel JM, Gooley TA, Petersdorf EW, Sorror ML, Woolfrey AE, et al. Comparison of matched unrelated and matched related donor myeloablative hematopoietic cell transplantation for adults with acute myeloid leukemia in first remission. Leukemia. 2010;24:1276–1282. doi: 10.1038/leu.2010.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weisdorf DJ, Anasetti C, Antin JH, Kernan NA, Kollman C, Snyder D, et al. Allogeneic bone marrow transplantation for chronic myelogenous leukemia: comparative analysis of unrelated versus matched sibling donor transplantation. Blood. 2002;99:1971–1977. doi: 10.1182/blood.v99.6.1971. [DOI] [PubMed] [Google Scholar]
- 27.Weisdorf DJ, Nelson G, Lee SJ, Haagenson M, Spellman S, Antin JH, et al. Sibling versus unrelated donor allogeneic hematopoietic cell transplantation for chronic myelogenous leukemia: refined HLA matching reveals more graft-versus- host disease but not less relapse. Biol Blood Marrow Transplant. 2009;15:1475–1478. doi: 10.1016/j.bbmt.2009.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gratwohl A, Schmid O, Baldomero H, Horisberger B, Urbano-Ispizua A. Haematopoietic stem cell transplantation (HSCT) in Europe 2002. Changes in indication and impact of team density. A report of the EBMT activity survey. Bone Marrow Transplant. 2004;34:855–875. doi: 10.1038/sj.bmt.1704653. [DOI] [PubMed] [Google Scholar]
- 29.Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–2919. doi: 10.1182/blood-2005-05-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]


