Abstract
Our objective was to assess how exposure to secondhand tobacco smoke occurs in Hungarian homes, particularly among non-smokers, and to examine the effectiveness of home smoking bans in eliminating exposure to secondhand smoke at home. In 2009, 2286 non-smokers and smokers aged 16–70 years, who were selected randomly from a nationally representative sample of 48 Hungarian settlements, completed paper-and-pencil self-administered questionnaires addressing tobacco-related attitudes, opinions and behaviors. Chi-square tests, one-way analysis of variance and multivariate logistic regression models were used to assess the effect of demographics, socio-economic characteristics and home smoking policies on the risk of exposure to secondhand tobacco smoke at home. Significantly higher risk of exposure was found among younger, lower educated and poorer people and among those having no or partial home smoking restrictions. There was a significant interaction between education level and home smoking policies: the effect of a smoking ban on exposure to secondhand tobacco smoke was stronger for the lower educated group than the higher educated group. The results suggest that Hungarians are making good progress in implementing home smoking bans, and that in the majority of population these bans are working. More can be done to promote the uptake of home smoking bans among poorer and less educated subpopulations.
Introduction
Studies published over the past decade substantiate the enormous health burden associated with secondhand tobacco smoke (SHS). SHS leads to a range of diseases in newborns (e.g. premature birth), in children (e.g. acute respiratory infections, middle ear disease) and in non-smoking adults (e.g. heart disease, lung cancer) [1–5]. A comprehensive analysis of morbidity and mortality data from 192 countries estimated that SHS caused 603 000 premature deaths and the loss of 10.9 million disability-adjusted life years in 2004 [6]. The same study estimated that 40% of children, 33% of male non-smokers and 35% of female non-smokers were exposed to SHS at work or home in 2004 [6]. SHS reduction is a global priority of the WHO and the European Union (EU) [7–9].
Exposure to SHS is particularly high in Central and Eastern Europe, especially Lithuania, Bulgaria, Romania, Poland, Hungary, Ukraine, Estonia and the Russian Federation [6, 10] are among the countries with the highest rates of smoking in Europe [8, 10]. In 2003, the smoking prevalence in Hungary was 35.0% (41.5% in males and 28.5% in females) [11]. Hungary also has relatively high levels of exposure to SHS: 20% of persons aged ≥15 years are regularly exposed to SHS at home, compared with 17% for European Union as a whole [10]. Over the past two decades, Hungary introduced national laws (e.g. Act XLII of 1999 on the Protection of Non-smokers and the Regulation of Tobacco Sales, Marketing and Use) that restrict smoking in indoor public places (e.g. designated smoking areas in work places, in restaurants, in closed public places, bans on smoking in public transport, in primary health care settings and pharmacies, in kindergartens and schools) [12]. In April 2011 the Hungarian Parliament amended the Act XLII of 1999 (Anti-Smoking Law) to regulate more strictly smoking in public places. The new law, which takes full effect in 2012, bans smoking completely in restaurants, workplaces, health care institutions and closed public places, as well as in specific outdoor public places, including bus stops and playgrounds [13]. As the new legislation is implemented and enforced, it is anticipated that major sources of SHS exposure will be eliminated. The primary remaining source of SHS exposure will be smoking in private homes. Smoking bans inside homes have been shown to reduce SHS exposure among children and adults, as well as to promote anti-smoking attitudes among youth [14, 15], decrease smoking and smoking uptake in teenagers [16] and increase quitting [17].
This study assesses how exposure to SHS occurs in homes within Hungary, particularly among non-smokers. We examine the effectiveness of home smoking bans in eliminating exposure to SHS at home. This involves two distinct questions: (i) How prevalent are home smoking bans? (ii) When home smoking bans are in place, how effective are they in eliminating exposure? This study also examines the relationship between SHS exposure and socio-economic status (SES). We hypothesize that lower SES people are more exposed by SHS at home, because lower SES households are less likely than higher SES households to adopt home smoking bans.
Methods
Study design and participants
The data reported here are from a survey of a large nationally representative sample of Hungarians conducted in 2009. This is the first wave of a longitudinal study, with the second wave conducted in 2011. A two-stage sampling method was used to select respondents. In the first stage, a nationally representative sample of 48 settlements (municipalities) from the seven geographical regions of Hungary was chosen. In the second stage the Central Office for Administrative and Electronic Public Services of Hungary extracted a random sample of residents aged 16–70 years within each of the 48 settlements. The age and gender distribution of each sample reflected the distribution of the respective population. A maximum of one person was selected from any given household.
Of the 4086 individuals selected for inclusion, the project staff were able to make contact with 3920 persons, and of these potential participants, 2286 completed the questionnaire (response rate of 55.1%; cooperation rate of 57.4%). We omitted 36 of the 2286 respondents from this study because of missing data on key demographic characteristics (age, sex or education), leaving a total sample of 2250.
The Regional and Institutional Human Medical Biological Research Ethics Committee of the University of Szeged approved the study protocol (No. 2431/2008). Informed written consent was obtained from adult respondents, and in the case of respondents aged <18 years, parental permission was sought to speak with the youth.
Study variables
A paper-and-pencil self-administered questionnaire was used to collect information on demographics, socio-economic status, smoking behavior, exposure to SHS, attitudes toward tobacco control policies and the rules about smoking in private homes.
Demographic variables included gender and age. Age was categorized as 16–24, 25–44, 45–64 or 65–70 years. Socio-economic status was indexed by educational level and financial difficulties. Educational level was categorized into three groups: low level (no more than primary school), medium level (trade school, grammar school, vocational secondary school) and high level (college, university). The evaluation of financial difficulties based on a question about the respondents’ ability to pay essential expenses (‘Did it happen in the last 12 month, that you couldn’t pay the heating/water/gas or lighting charges in time because of financial difficulties?’). Respondents saying ‘yes’ were classified as ‘poor’, whereas those indicating ‘no’ were classified as ‘non-poor’.
Smoking status of the respondents was measured according to WHO guidelines [18], and classified as current smokers and non-smokers (including former or never-smokers). A current smoker was defined as someone who smoked daily or occasionally in the past 30 days, regardless of the number of cigarettes smoked in his/her lifetime. Former smokers were those who smoked in the past—at least 100 cigarettes in one’s lifetime—but were not smoking for the preceding 30 days. Never-smokers were those who have never smoked or who smoked less than 100 cigarettes in their life.
The rules about smoking in the home were measured by one question: ‘Which statement best describes the rules about smoking inside your home?’ Response options were: smoking is not allowed anywhere inside the home, smoking is allowed in some places or at some times and smoking is allowed anywhere inside the home [19]. Exposure to SHS at home was assessed with the following question: ‘During the past 7 days, when you were at home, how many days were you exposed by other family members’ or visitors’ tobacco smoke?’
The reliability of survey items was evaluated in a pilot study involving test–retest examination. There were no significant differences in response choices in the 2-week test–retest study.
Statistical analysis
Simple descriptive statistics were applied to summarize the basic characteristics of the sample. Chi-square tests were used to assess whether home-smoking policies vary as a function of demographic and socio-economic factors, as well as by smoking status. Univariate and multivariate analyses were conducted to test whether exposure to SHS at home varies as a function of demographics, socio-economic characteristics and home smoking policies. The univariate analyses included a series of one-way analyses of variance to test whether the number of days exposed in the past week (0–7) varied as a function of each of the predictors, as well as a series of chi-squared tests to test whether the proportion who were exposed at all varied as a function of the predictors.
To assess the independent contribution that demographic characteristics, socio-economic factors and home smoking policies have on exposure to SHS at home, we conducted multivariate logistic regression analyses. Model 1 included gender, age, education and financial difficulties as independent variables. The respondents’ home smoking policy was added in Model 2. For the purpose of the logistic regression, this variable was treated as a dichotomous (‘total ban’ versus ‘no ban or partial ban’), because past studies have shown that a partial ban has the same practical effect as ‘no policy’ in predicting smoking behavior [20]. Model 3 included the interaction between financial difficulties and home smoking bans. Model 4 included the interaction between education and home smoking bans.
In each model, we calculated the odds ratio (OR) and 95% confidence interval (95% CI) for each predictor. Nagelkerke R2 values were used to compare the explanatory power of the models [21]. Statistical significance was set up at P < 0.05. Data analyses were performed using SPSS 17.0 for Windows.
Results
Characteristics of sample and smoking status
Table I shows the characteristics of respondents and the prevalence of home smoking policies among the entire sample of 2250 respondents. Of the total sample 53% are women. About 80% are between 25 and 64 years of age. Most respondents (62%) have a medium level of education (more than primary school but did not attend college or university), with the remainder split almost evenly between the low and high categories. Nearly one-third (31%) of the respondents reported that they had been unable to pay their utility bill in the past 12 months, and thus were classified as ‘poor’. The demographic profile of the total sample is consistent with that for the population of adults in Hungary [22]. Also in line with other studies of tobacco use in Hungary [23, 24], one-third of the sample reported that they are current smokers.
Table I.
Characteristics of the entire sample and of the non-smoker subsample
| All responders (n = 2250) | All non-smokers (n = 1502) | Non-smokers with non-missing data (n = 1371) | |
|---|---|---|---|
| Characteristics | n (%) | n (%) | n (%) |
| Gender | |||
| Male | 1053 (46.8) | 645 (42.9) | 591 (43.1) |
| Female | 1197 (53.2) | 857 (57.1) | 780 (56.9) |
| Age (years) | |||
| 16–24 | 314 (14.0) | 220 (14.6) | 203 (14.8) |
| 25–44 | 921 (40.9) | 579 (38.5) | 539 (39.3) |
| 45–64 | 862 (38.3) | 567 (37.7) | 504 (36.8) |
| 65–70 | 153 (6.8) | 136 (9.1) | 125 (9.1) |
| Educational level | |||
| Low | 418 (18.6) | 262 (17.4) | 213 (15.5) |
| Medium | 1390 (61.8) | 894 (59.5) | 829 (60.5) |
| High | 442 (19.6) | 346 (23.0) | 329 (24.0) |
| Financial difficulties | |||
| Poor | 694 (31.2) | 375 (25.0) | 339 (24.7) |
| Non-poor | 1530 (68.8) | 1108 (73.7) | 1032 (75.3) |
| Missing | 26 (1.2) | 19 (1.3) | 0 (0.0) |
| Smoking status | |||
| Current smoker | 748 (33.2) | 0 (0.0) | 0 (0.0) |
| Non-smoker or former smoker | 1502 (66.8) | 1502 (100.0) | 1371 (100.0) |
| Home smoking policies | |||
| No smoking restrictions | 167 (7.4) | 46 (3.1) | 45 (3.3) |
| Partial smoking restrictions | 699 (31.1) | 344 (22.9) | 317 (23.1) |
| Total smoking restrictions | 1334 (59.3) | 1073 (71.4) | 1009 (73.6) |
| Don’t know/missing | 50 (2.2) | 39 (2.6) | 0 (0.0) |
| Number of days in past week exposed to SHS at home | |||
| 0 | 1387 (61.6) | 1074 (71.5) | 1041 (75.9) |
| 1 | 104 (4.6) | 70 (4.7) | 68 (5.0) |
| 2 | 91 (4.2) | 58 (3.9) | 56 (4.1) |
| 3 | 45 (2.0) | 32 (2.1) | 32 (2.3) |
| 4 | 24 (1.1) | 19 (1.3) | 19 (1.4) |
| 5 | 29 (1.3) | 18 (1.2) | 18 (1.3) |
| 6 | 14 (0.6) | 6 (0.4) | 6 (0.4) |
| 7 | 408 (18.1) | 135 (9.0) | 131 (9.3) |
| Don’t know/missing | 145 (6.5) | 90 (6.0) | 0 (0.0) |
SHS: secondhand tobacco smoke.
Prevalence of home smoking bans
More than half (59.3%) of all the respondents reported that there was a total ban on smoking in their home, and another 31% reported having a partial ban (Table I). Only 7.4% of the sample reported that there were no restrictions on smoking at home. Home smoking policies were much more stringent among non-smokers than among current smokers: 71.4% of non-smokers reported that there was a total ban on smoking in their homes, compared with 34.9% of smokers (P < 0.001).
Home smoking policies also varied as a function of education and financial status (Table II). Higher educated respondents and respondents without financial difficulties were more likely to adopt home smoking bans. These differences were significant both for the entire sample and for the non-smoker subsample.
Table II.
Total smoking restrictions at home as a function of demographic variables
| Entire sample (n = 2250)a |
Non-smoker subsample (n = 1502)b |
|||
|---|---|---|---|---|
| Characteristics | Who have total restrictions at home (%) | P-valuec | Who have total restrictions at home (%) | P-valuec |
| Gender | <0.001 | 0.001 | ||
| Male | 56.2 | 68.6 | ||
| Female | 64.5 | 76.9 | ||
| Age (years) | <0.001 | 0.031 | ||
| 16–24 | 60.6 | 69.3 | ||
| 25–44 | 62.5 | 76.3 | ||
| 45–64 | 57.6 | 72.2 | ||
| 65–70 | 66.4 | 72.1 | ||
| Educational level | <0.001 | <0.001 | ||
| Low | 49.9 | 64.0 | ||
| Medium | 61.0 | 74.7 | ||
| High | 69.6 | 76.8 | ||
| Financial difficulties | <0.001 | 0.013 | ||
| Poor | 50.0 | 67.9 | ||
| Non-poor | 65.3 | 75.3 | ||
aMissing data range: 50–73.
bMissing data range: 39–55.
cBased on chi-square test.
Exposure to SHS at home
The primary outcome of interest for this study was exposure to SHS within one’s own home. Of all the respondents, 18% reported that they had been exposed to SHS in their ‘home every day within the past week’, with another 14% exposed ‘at least 1 day’ in the past week. In addition to the 32% who reported being exposed to SHS in their home at least 1 day in the previous week, another 6.5% reported they were not sure how many days they were exposed (Table I).
Given that smokers inherently expose themselves to environmental smoke, we were particularly interested in assessing how much exposure to SHS occurs among non-smokers. Of the 2250 respondents, 1502 were non-smokers. Among this group, 9% were exposed to SHS in their home every day in the past week, another 13.5% reported being exposed at least 1 day and another 6% were unsure of the number of days they were exposed (Table I).
The remaining analyses examined how exposure to SHS at home varied as a function of demographic factors, socio-economic status and home smoking policy. These analyses included only respondents with complete data. In total, ∼9% of the non-smoker subsample (n = 131) had missing data for either the financial difficulty variable, the home smoking ban variable, or the exposure to SHS variable. As shown in Table I, dropping these 131 respondents did not materially change the composition of the non-smoker subsample. For the 1371 non-smokers with complete data, 73.6% had total smoking restrictions at home, and 24.1% were exposed by SHS at least 1 day during the last week prior to the study.
Univariate analysis of factors effecting exposure to SHS
Table III shows how SHS exposure varies as a function of demographics, socio-economic factors and home smoking policies. Based on this univariate analysis, exposure was found to vary by age, education level and financial difficulties, but not by gender. In particular, SHS exposure was higher among respondents aged 16–24 years (37.9%) than among those aged ≥65 years (13.6%); higher in low educated (32.4%) than in high educated (14.9%) and higher among poor respondents (33.0%) than non-poor (21.1%).
Table III.
Exposure to secondhand tobacco smoke at home among non-smokers (n = 1371)
| Non-exposed | Exposed | ||
|---|---|---|---|
| Characteristics | n (%) | n (%) | P-valuea |
| Gender | 0.170 | ||
| Male | 438 (74.1) | 153 (25.9) | |
| Female | 603 (77.3) | 177 (22.7) | |
| Age (years) | <0.001 | ||
| 16–24 | 126 (62.1) | 77 (37.9) | |
| 25–44 | 399 (74.0) | 140 (26.0) | |
| 45–64 | 408 (81.0) | 96 (19.0) | |
| 65–70 | 108 (86.4) | 17 (13.6) | |
| Educational level | <0.001 | ||
| Low | 144 (67.6) | 69 (32.4) | |
| Medium | 617 (74.4) | 212 (25.6) | |
| High | 280 (85.1) | 49 (14.9) | |
| Financial difficulties | <0.001 | ||
| Poor | 227 (67.0) | 112 (33.0) | |
| Non-poor | 814 (78.9) | 218 (21.1) | |
| Home smoking policies | <0.001 | ||
| No smoking restrictions | 23 (51.1) | 22 (48.9) | |
| Partial smoking restrictions | 161 (50.8) | 156 (49.2) | |
| Total smoking restrictions | 857 (84.9) | 152 (15.1) | |
| Total | 1041 (75.9) | 330 (24.1) |
aResults of chi-square test.
As expected, exposure to SHS at home was much higher among respondents without any restrictions on smoking (48.9% exposed at least 1 day in the past week) than among respondents with a total ban (15.1% exposed at least 1 day). Among the respondents with partial restrictions, 49.2% were exposed at least 1 day, virtually the same rate as for the group with no restrictions. Similarly, the no-restriction group and partial-restriction group were roughly equivalent with regard to the average number of days exposed (2.64 versus 2.31).
Multivariate analysis of factors effecting exposure to SHS
The multivariate logistic regression models (Table IV) assessed the effect that various factors had on exposure to SHS at home among non-smokers, with exposure categorized as none versus any in the past week. Model 1 showed that age, education and financial status have independent effects on SHS exposure. The home smoking policy variable (categorized as total ban versus partial or no restrictions) was added in Model 2. Respondents without total smoking restrictions were much more likely to be exposed to SHS at home (OR 5.69). Age, education and financial difficulties remained significant in Model 2, but the ORs decreased in magnitude.
Table IV.
Multivariate logistic regression models of factors associated with exposure to secondhand tobacco smoke at home among non-smokers (n = 1371)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Variables | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Gender | ||||
| Male | 1.21 (0.93–1.56) | 1.04 (0.79–1.37) | 1.04 (0.78–1.37) | 1.05 (0.79–1.39) |
| Female | 1.00 | 1.00 | 1.00 | 1.00 |
| Age (years) | ||||
| 16–24 | 3.95 (2.18–7.17)*** | 4.52 (2.41–8.49)*** | 4.48 (2.39–8.42)*** | 4.59 (2.43–8.65)*** |
| 25–44 | 2.78 (1.57–4.91)*** | 3.26 (1.80–5.91)*** | 3.25 (1.79–5.90)*** | 3.22 (1.77–5.87)*** |
| 45–64 | 1.67 (0.94–2.96) | 1.70 (0.94–3.08) | 1.71 (0.94–3.10) | 1.71 (0.94–3.12) |
| 65–70 | 1.00 | 1.00 | 1.00 | 1.00 |
| Educational level | ||||
| Low | 2.86 (1.83–4.49)*** | 2.36 (1.46–3.81)*** | 2.34 (1.45–3.79)* | 1.83 (0.99–3.39) |
| Medium | 1.89 (1.33–2.69)*** | 1.96 (1.36–2.83)*** | 1.97 (1.36–2.84) | 1.32 (0.85–2.06) |
| High | 1.00 | 1.00 | 1.00 | 1.00 |
| Financial difficulties | ||||
| Poor | 1.70 (1.28–2.25)*** | 1.56 (1.15–2.11)** | 1.40 (0.94–2.08) | 1.59 (1.17–2.15)** |
| Non-poor | 1.00 | 1.00 | 1.00 | 1.00 |
| Home smoking policies | ||||
| No or partial smoking restrictions | 5.69 (4.28–7.57)*** | 5.27 (3.76–7.38)** | 2.61 (1.33–5.08)** | |
| Total smoking restrictions | 1.00 | 1.00 | 1.00 | |
| Financial difficulties by home smoking policies | ||||
| Poor by no or partial smoking restrictions | 1.31 (0.70–2.43) | |||
| Education by home smoking policies | ||||
| Low education by no or partial smoking restrictions | 1.98 (0.78–5.01) | |||
| Medium education by no or partial smoking restrictions | 2.83 (1.33–6.02)** | |||
| Nagelkerke R2 | 0.084 | 0.229 | 0.229 | 0.236 |
*P < 0.05; **P < 0.01; ***P < 0.001.
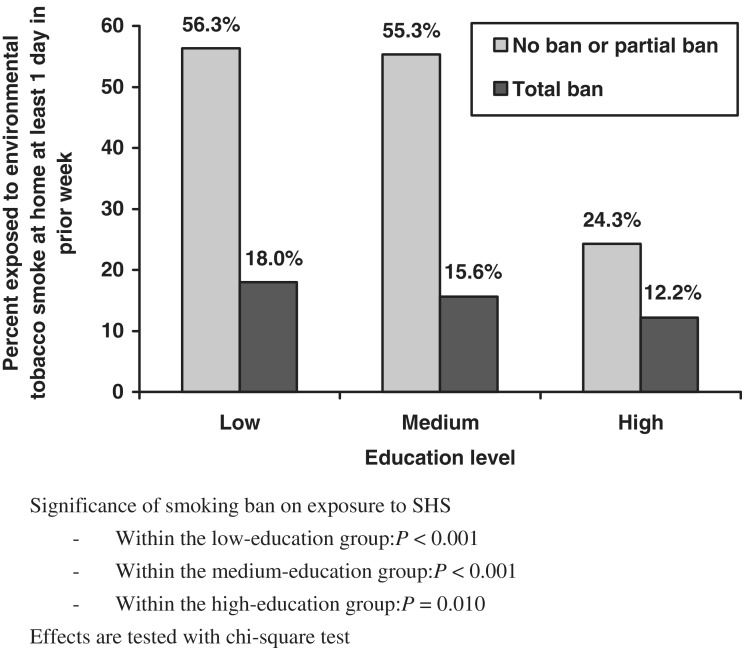
Models 3 and 4 add specific interaction terms that allowed us to test whether the effect of a home smoking ban might vary as a function of either financial difficulties (Model 3) or education (Model 4). The interaction between financial difficulties and home smoking policy was not significant (Model 3), but the interaction between education level and home smoking policy was significant at P < 0.01 (Model 4). The nature of this second interaction term is clear in Fig. 1. When respondents do not have a total home smoking ban, there is a large effect of education: the percentage of respondents exposed to SHS is >55% among the low and medium education groups, compared with 24% among the high education group. The effect of education is much more modest when respondents do have a total home smoking ban—between 12 and 18% in all three groups.
Fig. 1.
Exposure to environmental tobacco smoke as a function of education level and home-smoking ban.
Discussion
Given global experiences to date, there is every reason to expect that the national anti-tobacco legislation recently enacted in Hungary will succeed in limiting exposure to SHS in public places [8]. The current study indicates, however, that exposure to SHS in the home will continue to affect large numbers of Hungarians, including non-smokers. Within this nationally representative sample, approximately one-quarter of the 1502 non-smokers reported being exposed to SHS within their homes at least 1 day within the past week and 9% reported being exposed every day.
Lower education and being poor imposes an extra risk of being exposed to SHS. Nearly one-third (32.4%) of non-smokers with ≤8 years of education had been exposed to SHS at home in the prior week, compared with only 14.9% among non-smokers with at least 13 years of education. The rate of exposure among ‘poor’ respondents (i.e. those who had difficulty paying their utility bills) was similarly high: 33.0%.
A number of previous studies have found that smoke-free rules in homes and vehicles can reduce SHS exposure among children and non-smoking adults [16, 17, 25, 26], while also helping smokers to quit [17, 25] and reducing the risk of adolescents becoming smokers [16].
Although this study demonstrates that exposure to SHS at home is reduced significantly when a total ban is in place, having a total ban does not fully eliminate exposure to SHS at home. Of the respondents, 15% reporting a total ban were exposed to SHS at home at least on 1 day in the previous week. In other words, many home smoking bans are poorly enforced. Considerable attention has been paid to encouraging the adoption of home smoking policies. Additional effort is required to assist families in constructively confronting smokers who violate these policies.
Another important finding from this study relates to the ineffectiveness of ‘partial bans’. Respondents who reported that they had a policy limiting smoking to specific rooms were exposed to SHS at rates equivalent to those reported by respondents with no home SHS policy. Rainio and Rimpela [20] also found that partial or no home smoking bans versus total ban increased the likelihood of child smoking in Finland [20]. Our result reinforces the importance of a total ban on smoking in the home.
The 59.3% prevalence of smoke-free homes among participants in the current study is notably lower than in the rates reported in the United States and Australia, but considerably higher than what was found in one Chinese study. McMillen et al. [27] reported that 74% of US adults had household smoking bans in 2001, and the prevalence of smoke-free home rules reported by the CDC was 72.2% in 2003 (31.8% among households with at least one smoker and 83.5% among households with no smokers) [28]. Dunn et al. [29] found that 76.8% of the Australian respondents had smoking bans in their homes. In contrast, only 26% of the respondents reported having a complete home smoking ban in an urbanizing community in China [30].
Given the limited national promotion of home smoking policies, our results show that Hungarians are making relatively good progress in taking the initiative to implement smoking bans at home and that in the majority of cases these bans are working. On the other hand, much more can be done to educate Hungarians and promote the adoption of home smoking bans. A 59.3% prevalence for total bans implies that there is room for improvement in two of every five Hungarian households. Since only 35% of the smokers in our sample reported that there was a total ban on smoking in their home, it is specifically important to encourage total bans in households with smokers.
Efforts to encourage home smoking bans should target less-educated and poorer smokers and non-smokers. These subgroups are more likely to be exposed to SHS at home, and at the same time, less likely to have a total ban in place. We also found that having a ban in place proved to be much more valuable for respondents with a low or medium level of education than for highly educated respondents. Less than a quarter of highly educated respondents reported being exposed to SHS at home even when they did not have a ban in place, but this figure was >50% for the low and medium educated respondents.
Well-crafted communications and educational strategies are clearly important in increasing the adoption of home smoking bans [31]. In addition, it is important to recognize that the enactment of government policies that limit smoking in public places produces positive spin-off effects in encouraging households to adopt private policies regulating smoking in the home [32–34]. As noted above, the Hungarian national government passed comprehensive legislation in 2011 forbidding smoking in a variety of public places. Our study provides important baseline data for assessing whether home smoking bans will become more prevalent with the implementation and enforcement of these new bans in public places.
We also believe that health authorities in Hungary can do more to educate individuals about the dangers of SHS exposure in children and about the importance of the home as an environment of exposure, as well as to encourage them to make their homes smoke-free. Health professionals can play an important role in this regard, especially in reaching lower SES Hungarians. Medical care in Hungary is universally available to the entire population. Primary care providers (particularly, family physicians and pediatricians) should be encouraged to assess not only whether their patients smoke, but also whether others in the household smoke. When patients are found to be exposed to SHS, the provider should emphasize the importance of banning smoking within the home. Special attention should be placed on counseling economically disadvantaged and lower educated patients, since they are more likely to smoke and to be exposed to SHS at home.
The most effective messages for promoting home smoking bans include information on the harms of smoking in the home and positive benefits of having a smoke-free home (e.g. reduced likelihood that children will start smoking, having a cleaner home, and significantly less exposure to SHS and its health consequences) [35]. These messages should emphasize the effect of SHS on children as this has been found to motivate the adoption of home smoking bans [27, 36].
This study is based on a comprehensive in-home survey conducted among a large nationally representative sample of Hungarian adults. The response rate (55.1%) is slightly higher than is generally achieved for surveys of the general population. Against these strengths, we need to also acknowledge the study’s limitations. First, adults >70 years of age were not recruited. It is possible that the effect of education and financial status on exposure to SHS might be different in this older group than was observed in our sample. Second, ∼9% of the non-smokers in the sample had missing data on SHS exposure or home smoking policy and thus could not be included in the analysis. Third, data on exposure to SHS and home-smoking bans came from self-reports that may have been inaccurate in some instances. Finally, it is also possible that respondents over-report home smoking restrictions because of social desirability.
Despite these limitations, this study provides the first in-depth analysis of the degree to which Hungarians are exposed to SHS at home and the effect of home-smoking bans in limiting exposure. Prior to this study, little research had been conducted in Hungary on voluntary smoke-free policies and SHS exposure focusing on the non-smoker adult population. The findings support the development of future public health strategies of tobacco control. The implementation of home smoking bans should complement additional work to reduce smoking, especially among less educated and poorer Hungarians.
Funding
The Fogarty International Centre, the National Cancer Institute and the National Institutes on Drug Abuse, within the National Institutes of Health [1 R01 TW007927-01].
Conflict of interest statement
None declared.
Acknowledgements
The contribution of field workers and other study personnel is gratefully acknowledged. The contents are solely the responsibility of the authors and do not necessarily represent the official view of the National Institutes of Health.
References
- 1.U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Washington, DC: Department of Health and Human Services; 2006. Available at: http://www.surgeongeneral.gov/library/secondhandsmoke/. Accessed 18 October 2010. [Google Scholar]
- 2.U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. Available at: http://www.surgeongeneral.gov/library/tobaccosmoke/report/full_report.pdf. Accessed: 13 March 2011. [Google Scholar]
- 3.World Health Organization, International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Tobacco Smoke and Involuntary Smoking. Lyon: World Health Organization, International Agency for Research on Cancer; 2004. Available at: http://monographs.iarc.fr/ENG/Monographs/vol83/index.php. Accessed: 25 March 2011. [Google Scholar]
- 4.Sleiman M, Gundel LA, Pankow JF, et al. Formation of carcinogens indoors by surface-mediated reactions of nicotine with nitrous acid, leading to potential thirdhand smoke hazards. Proc Natl Acad Sci USA. 2010;15:6576–80. doi: 10.1073/pnas.0912820107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winickoff JP, Friebely J, Tanski SE, et al. Beliefs about the health effects of “thirdhand” smoke and home smoking bans. Pediatrics. 2009;123:e74–9. doi: 10.1542/peds.2008-2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Öberg M, Jaakkola MS, Woodward A, et al. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet. 2011;377:139–46. doi: 10.1016/S0140-6736(10)61388-8. [DOI] [PubMed] [Google Scholar]
- 7. World Health Organization. WHO Framework Convention on Tobacco Control. World Health Organization, 2003, Updated Reprint 2004, 2005. Geneva, Switzerland. Available at: http://whqlibdoc.who.int/publications/2003/9241591013.pdf. Accessed: 17 August 2010.
- 8. World Health Organization. WHO Report on the Global Tobacco Epidemic, 2009: Implementing Smoke-Free Environments. World Health Organization, 2009. Geneva, Switzerland. Available at: http://whqlibdoc.who.int/publications/2009/9789241563918_eng_full.pdf. Accessed: 11 May 2010.
- 9.Council Recommendation of 30 November 2009 on smoke-free environments (2009/C 296/02) Official Journal of the European Union. 5.12.2009;C 296:4–14. Available at: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:C:2009:296:0004:0014:EN:PDF. Accessed: 10 October 2010. [Google Scholar]
- 10.Survey on Tobacco – Analytical Report. Brussels: European Commission; 2009. (Flash Eurobarometer No. 253, The Gallup Organisation. Available at: http://ec.europa.eu/public_opinion/flash/fl_253_en.pdf/. Accessed: 13 April 2009. [Google Scholar]
- 11.National Health Interview Survey 2003, Hungary Executive Update. Budapest: Johan Béla National Center for Epidemiology; 2004. [Google Scholar]
- 12.Act XLII of 1999 on the Protection of Non-smokers and the Regulation of Tobacco Sales, Marketing and Use. Available at: http://net.jogtar.hu/jr/gen/hjegy_doc.cgi?docid=99900042.TV/. Accessed: 6 October 2010. [Google Scholar]
- 13.Act XLI of 2011 an amendment of Act XLII of 1999 on the Protection of Non-smokers and the Regulation of Tobacco Sales, Marketing and Use. Available at: http://www.kozlonyok.hu/nkonline/MKPDF/hiteles/MK11048.pdf. Accessed: 5 May 2011. [Google Scholar]
- 14.Albers AB, Biener L, Siegel M, et al. Household smoking bans and adolescent antismoking attitudes and smoking initiation: findings from a longitudinal study of a Massachusetts Youth Cohort. Am J Public Health. 2008;98:1886–93. doi: 10.2105/AJPH.2007.129320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schultz ASH, Nowatzki J, Dunn DA, et al. Effects of socialization in the household on youth susceptibility to smoking: a secondary analysis of the 2004/05 Canadian Youth Smoking Survey. Chron Dis Can. 2010;3:71–7. [PubMed] [Google Scholar]
- 16.Wakefield MA, Chaloupka FJ, Kaufman NJ, et al. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. BMJ. 2000;321:333–7. doi: 10.1136/bmj.321.7257.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shopland DR, Anderson CM, Burns DM. Association between home smoking restrictions and changes in smoking behaviour among employed women. J Epidemiol Community Health. 2006;60(Suppl 2):ii44–50. doi: 10.1136/jech.2006.045724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Guidelines for Controlling and Monitoring the Tobacco Epidemic. Geneva: WHO; 1998. Monitoring tobacco use. Available at: http://health21.hungary.globalink.org/koal_menu_elemei/WHO.DOC. Accessed: 2 January 2009. [Google Scholar]
- 19.Starr G, Rogers T, Schooley M, et al. Key Outcome Indicators for Evaluating Comprehensive Tobacco Control Programs. Atlanta, GA: Centers for Disease Control and Prevention; 2005. [Google Scholar]
- 20.Rainio SU, Rimpela AH. Home smoking bans in Finland and the association with child smoking. Eur J Public Health. 2008;18:306–11. doi: 10.1093/eurpub/ckm098. [DOI] [PubMed] [Google Scholar]
- 21.Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika. 1991;3:691–2. [Google Scholar]
- 22.Demographic Year Book, 2009. Budapest: Hungarian Central Statistical Office; 2010. [Google Scholar]
- 23. Boros J. Smoking. In: Boros J, Németh R, Vitrai J (eds). National Health Interview Survey 2000. Research Report. National Center for Epidemiology, 2002. Budapest, [In Hungarian] Available at: http://www.egeszsegmonitor.hu/dok/kutatasi_jelentes_OLEF2000.pdf. Accessed: 30 November 2011.
- 24.Tombor I, Paksi B, Urbán R, et al. Prevalence of smoking among the Hungarian adult population. Népegészségügy. 2010;2:131–6. [Google Scholar]
- 25.Farkas A, Gilpin EA, Disteefan JM, et al. The effects of household and workplace smoking restrictions on quitting behaviours. Tobacco Control. 1999;8:261–5. doi: 10.1136/tc.8.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cartmell KB, Miner C, Carpenter MJ, et al. Secondhand smoke exposure in young people and parental rules against smoking at home and in the car. Public Health Rep. 2011;126:575–82. doi: 10.1177/003335491112600414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McMillen RC, Winickoff JP, Klein JD, et al. US adult attitudes and practices regarding smoking restrictions and child exposure to environmental tobacco smoke: changes in the social climate from 2000-2001. Pediatrics. 2003;112:e55–60. doi: 10.1542/peds.112.1.e55. [DOI] [PubMed] [Google Scholar]
- 28.Trosclair A, Murphy-Hoefer R, Asman K, et al. State-specific prevalence of smoke-free home rules – United States, 1992-2003. MMWR. 2007;56:501–4. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5620a3.htm. Accessed: 30 November 2011. [PubMed] [Google Scholar]
- 29.Dunn J, Greenbank S, McDowell M, et al. Community knowledge, attitudes and behaviours about environmental tobacco smoke in homes and cars. Health Promot J Austr. 2008;19:113–7. doi: 10.1071/he08113. [DOI] [PubMed] [Google Scholar]
- 30.Ji M, Ding D, Hovell MF, et al. Home smoking bans in an urbanizing community in China. Am J Prev Med. 2009;37:132–6. doi: 10.1016/j.amepre.2009.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pizacani B, Laughter D, Menagh K, et al. Moving multiunit housing providers toward adoption of smoke-free policies. Prev Chronic Dis. 2011;8:A21. Available at: http://www.cdc.gov/pcd/issues/2011/jan/10_0015.htm. Accessed: 23 February 2012. [PMC free article] [PubMed] [Google Scholar]
- 32.Thomson G, Wilson N, Howden-Chapman P. Population level policy options for increasing the prevalence of smokefree homes. J Epidemiol Community Health. 2006;60:298–304. doi: 10.1136/jech.2005.038091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borland R, Yong H-H, Cummings KM, et al. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii42–50. doi: 10.1136/tc.2005.012492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mons U, Nagelhout GE, Allwright S, et al. Impact of national smoke-free legislation on home smoking bans: findings from the International Tobacco Control Policy Evaluation Project Europe Surveys. Tob Control. doi: 10.1136/tobaccocontrol-2011-050131. e-pub ahead of print, 13 February 2012; doi: 10.1136/tobaccocontrol-2011-050131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Escoffery C, Kegler MC, Butler S. Formative research on creating smoke-free homes in rural communities. Health Educ Res. 2009;1:76–86. doi: 10.1093/her/cym095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lund KE, Helgason ÁR. Environmental tobacco smoke in Norwegian homes, 1995 and 2001: changes in children’s exposure and parents attitudes and health risk awareness. Eur J Public Health. 2005;2:123–7. doi: 10.1093/eurpub/cki075. [DOI] [PubMed] [Google Scholar]