Motivational Interviewing (MI) is one intervention recommended in the U.S. Clinical Practice Guidelines for helping smokers become motivated to quit smoking (Fiore, 2008; Lancaster & Stead, 2005). MI is a client-centered counseling style for eliciting behavior change by helping clients to explore and resolve ambivalence (Miller & Rose, 2009). Meta-analyses have indicated that MI-based interventions are at least equivalent to other active treatments and superior to placebo controls for a wide variety of behavior change problems, including addictive behavior (drugs, alcohol, gambling) and health behaviors such as diet and exercise (Burke, Arkowitz, & Menchola, 2003; Burke, Dunn, Atkins, & Phelps, 2004; Hettema, Steele, & Miller, 2005; Rubak, Sandbaek, Lauritzen, & Christensen, 2005). Recent studies and meta-analyses suggest it is also effective for smoking cessation (Burke et al., 2003; Burke et al., 2004; Hettema et al., 2005; Lundahl, Brownwell, Tollefson & Burke. 2010; Rubak et al., 2005; Williams & Deci, 2001; Williams, Freedman, & Deci, 1998; Williams, Gagne, Ryan, & Deci, 2002; Williams, Grow, Freedman, Ryan, & Deci, 1996; Williams, McGregor, Sharp, Kouides et al., 2006a; Williams, McGregor, Sharp, Levesque et al., 2006b; Williams, Rodin, Ryan, Grolnick, & Deci, 1998). These studies documented that motivational interviewing can be effective even in brief encounters of only 15 minutes and that more than one encounter with a patient increases the likelihood of a positive effect. Another review examining 31 smoking cessation research trials using MI versus a control condition (9,485 individual participants) found a nearly 50% greater likelihood of cessation among those receiving MI (Heckman, 2010).
Despite the broad utilization of MI for smoking cessation, little is known about the mechanisms by which MI might promote cessation. To improve the effectiveness of interventions as well as the training of practitioners, it is important to establish the underlying mechanisms of action that account for MI’s effects. Miller and Rollnick (2002) initially suggested mechanisms such as cognitive dissonance and self-perception, but recent work has focused on the role of “change talk” (client statements that are consistent with behavior change) and “commitment language” (Amrhein, Miller, Yahne, Palmer, & Fulcher, 2003). Miller and Rose, (2009) recently proposed a theoretical model in which MI has its effects through increased change talk as well as interpersonal characteristics such as empathy and autonomy support. Other researchers have also suggested that a well-established theory of motivation, Self-Determination Theory (SDT) (Deci, Koestner, & Ryan, 1999; Ryan & Deci, 2000; Ryan, Kuhl, & Deci, 1997) may explain MI’s effects (Markland, Ryan, Tobin, & Rollnick, 2005; Vansteenkiste & Sheldon, 2006).
Although MI is not based on a specific theory, it is consistent with the principles of Self-Determination Theory (Deci et al., 1999; Ryan & Deci, 2000; Ryan et al., 1997). SDT proposes a continuum of human motivation with three distinct subtypes: amotivation, extrinsic motivation, and intrinsic motivation. Most relevant to health behavior change is the continuum within extrinsic motivation, the motivation to do activities that are not inherently interesting or enjoyable. Within extrinsic motivation, SDT differentiates between autonomous and controlled behavioral regulation. Behaviors are deemed autonomous when they result from a sense of choice or full volition and are personally relevant (“I am here to help you make the best decision for yourself. I am going to give you some facts about smoking, and you make the final decision what to do with your smoking”). Conversely, behaviors performed as a result of pressure or coercion, either by external or internal forces, are considered controlled, rather than self-regulated
According to SDT, behavioral regulation is more autonomous when it is internalized, as opposed to being regulated by external factors (e.g., doctor’s orders, or contingent rewards). Compared to external regulation, autonomous regulation is associated with increased self-efficacy, greater behavioral persistence, more long-term behavior change, and more positive health behaviors (Bandura, 1997). Studies have shown that physicians who counsel patients to quit smoking in an “autonomy supportive” style similar to MI, rather than in a “controlling” interpersonal style, are perceived as more “autonomy supportive” (Williams & Deci, 2001; Williams et al., 2002; Williams, McGregor, Sharp, Levesque et al., 2006). Their patients are more actively involved, use cessation medication more, and have higher self-efficacy and autonomous motivation, which are in turn, predictive of greater smoking cessation. In summary, self-determination theory posits that when counselors provide information and resources in a way that supports patients’ autonomy, patients internalize motivation for change, view themselves as competent to change, and are more likely to achieve lasting behavior change.
According to SDT proponents important elements of autonomy-supportive counseling include eliciting and listening carefully to patients perspectives, providing relevant information, inviting questions, respecting patients’ behavioral choices, supporting patient attempts at behavior change, and minimizing control (Williams et al., 2002). MI principles and methods are very consistent with these recommendations. MI is defined as a client-centered counseling approach which focuses on behavior change from the perspective of the client (Miller & Rollnick, 2002).The key tenets of the MI include using a collaborative style that elicits the patient’s perspective and reasons for change and supporting patient autonomy regarding behavior change. Internalization of health behavior change goals is likely fostered through these tenets as well as specific principles that include expressing empathy to communicate understanding of the patient’s perspective, “developing discrepancy” by exploring the health behavior change goal in relation to the patients broader life goals and values, and supporting self-efficacy.
Given the existing literature regarding the underlying processes of change involved in MI and the commonalities involved in the practice of MI and the principles of SDT, the present study examined the role of changes in motivation (controlled and autonomous) and self-efficacy from baseline to 6 months in predicting change in cigarettes per day at 12 months in the context of the KanQuit randomized clinical trial using different intensities of motivational interviewing counseling. We hypothesized that varying levels of MI (control group, moderate and high MI intensity) would independently predict change in cigarettes per day. Additionally, the effects of MI on smoking would be mediated through changes in self-efficacy and autonomous motivation, namely, that MI would enhance autonomous motivation and self-efficacy which would, in turn, result in increased likelihood of being quit at 12 months.
This is a secondary analysis of Kan Quit, an MI-based smoking cessation randomized trial which examined the effectiveness of a two-year disease management intervention for smoking cessation among rural smokers recruited through primary care practices (Ellerbeck et al., 2009). KanQuit provides an excellent opportunity for this analysis because motivation was measured over time and the intensity of MI varied across study condition. Specifying how an intervention impacts change in behavior by operating through its impact on mediating psychosocial variables (Baranowski, Cullen, & Baranowski, 1999; Baron & Kenny, 1986; Holmbeck, 1997) may help us further understand the process of MI and the role of psychosocial factors in smoking cessation.
METHODS
Kan Quit was a three-arm study examining cessation rate differences among participants receiving three levels of counseling intensity. In addition, all three groups received access to free pharmacotherapy (either bupropion or nicotine patch). At 12 months, groups who received MI had a greater cessation rates in the population who have not received treatment and smokers receiving standard care (High disease Management HDM: 23.9%; Moderate Disease Management MDM: 20.6%; no counseling: 15.6%, p=0.04; any counseling versus no counseling). The study design, recruiting, and detailed description of the intervention were reported elsewhere following CONSORT guidelines (Ellerbeck et al., 2009). The description of the intervention was consistent with the criteria for publication of an intervention study (Marks, 2010).
Trained medical students on preceptorships in 40 rural primary care clinics screened patients for their smoking status, identified eligible smokers, and obtained written informed consent. Participants’ contact information was forwarded to research staff who contacted participants via telephone, verified eligibility, and conducted the baseline survey. All groups received pharmacotherapy management consisting of offers of free pharmacotherapy (either nicotine patch or bupropion) at 6 month intervals accompanied by screening for potential contraindications and coordination of prescriptions with the patient’s physician (Cox et al., 2008). Participants were randomized to one of three intervention arms: 1) pharmacotherapy management only (PM – n=250); 2) PM plus moderate-intensity disease management (MDM – n=249); and 3) PM plus high-intensity disease management (HDM – n=251).
Both MDM and HDM coordinated smoking assessments and pharmacotherapy with the patient’s physician. Participants also completed a telephone survey every 6 months of the 2-year intervention. This study focused on data from the baseline, 6 month, and 12 month surveys since disparities in treatment across treatment groups was greatest at this point. This study was approved by the University of Kansas Medical Center Human Subjects Committee.
MI Counseling Intensities by Group
The intervention consisted of four 6 month cycles within each arm. The moderate-intensity disease management program (MDM) included up to 2 telephone counseling sessions and a physician progress report, while the high-intensity disease management program (HDM) included up to 6 telephone-based counseling sessions plus feedback of progress reports to the physician. The counseling protocol and instructions to participants were standardized, but were flexible. Participants who were abstinent at 6 month follow-up were offered one additional counseling session, for relapse prevention. Participants who were not abstinent were offered the maximum number of calls. Counselors were trained to offer additional counseling sessions to participants until the group standard for counseling sessions was reached (2 for moderate intensity, 6 for high intensity). However, counselors were instructed to schedule sessions but not attempt to persuade participants to take additional calls if participants declined to do so. We did this to remain within the spirit of MI. Participants who quit received only one additional relapse prevention while participants who did not quit received the maximum number of calls. The high intensity recipients completed an average of 3.2 call between months 0–6 and 1.8 calls between months 7–12, whereas the moderate-intensity recipients completed an average of 1.3 and 0.9 calls during these same time periods (Ellerbeck et al., 2009). The content of the counseling sessions were largely guided by Motivational Interviewing principles. Specifically, participants were guided through an exploration of their motivation and confidence to quit smoking, a discussion of the pros and cons of smoking and quitting, an examination of their values as they relate to smoking, and the development of a behavioral action plan (e.g., setting a quit date, strategies to succeed, etc.) using key principles of MI (e.g., expressing empathy, developing discrepancy, rolling with resistance, and supporting self-efficacy).
Counselors involved in this study were trained in a week-long training with certified and experienced MI trainers, as well as nationally renowned MI experts, where they were taught critical components of MI, encouraging autonomy support, and the MI protocol developed for this study. They also received ongoing counseling supervision based on case reports of sessions. Moreover, after each session, counselors were asked to complete a checklist asking about several of the key concepts of MI that served as process markers of appropriate MI delivery (e.g. rolling with resistance, making appropriate reflective statements, encouraging change talk) and a checklist asking about specific content that should have been covered per the MI protocol guiding the sessions (e.g., pros/cons of quitting, developing behavioral action plan). Counselors rated themselves and during supervision they were also rated using motivational interview markers.
Participants
Eligibility criteria included: (1) smoking ≥ 10 cigarettes per day; (2) smoking at least 25 of the last 30 days; (3) being at least 18 years of age; (4) not being pregnant or planning to become pregnant in the next two years; (5) not be planning on moving in the next two years; (6) having telephone access; and (7) considering one of the participating physicians as their regular doctor. Participants who completed the assessment at 6 months and 12 months were included in this analysis (N=612).
Measures
Participants completed a baseline telephone survey assessing demographic information and smoking history (i.e., number of cigarettes smoked per day, age at smoking initiation, number of previous quit attempts, length of longest quit attempt). The survey also included the following instruments assessed at baseline, 6 month and 12 month.
Smoking Self-Efficacy Questionnaire (SEQ-12)
The SEQ-12 (Etter, Bergman, Humair, & Perneger, 2000) is a two-dimensional 12-item scale measuring confidence in ability to refrain from smoking on a 5-point Likert scale (from 1 = “not at all sure” to 5 = “absolutely sure”). SEQ-12 scores range from 12 to 60 with higher scores indicating greater self-efficacy.
Treatment Self-Regulation Questionnaire (TSRQ)
The TSRQ for smoking (Williams, Ryan, & Deci, 2004) is a 15-item instrument that assesses one’s motivation to quit smoking using three subscales: autonomous motivation, controlled motivation, and amotivation. Autonomous motivation refers to motivation regulated by the process of choice and willingness to engage in a behavior (e.g., “because I feel I want to take responsibility for my own health,” “because it’s an important choice I really want to make”). Controlled motivation refers to motivation regulated by the process of compliance and one’s feelings that he or she has no choice (e.g., “because I feel pressure from others not to smoke,” “because I would feel guilty or ashamed of myself if I smoked”) (Berg et al., 2008). Amotivation refers to lack of motivation to quit (i.e., “I don’t really think about the [reasons for quitting],” “I don’t really know why [I would not smoke]”). Possible scores range from 6 to 42 for the autonomous motivation subscale and the controlled motivation subscale; possible scores range from 3 to 21 for the amotivation subscale. Higher scores indicate greater autonomous motivation, controlled motivation, or amotivation.
Smoking Outcome
Most smoking cessation studies use a binary variable, based on tobacco abstinence, for the main outcome. However, dichotomization reduces power to detect the effects of mediating variables (McCallum, 2002). For this reason we used cigarettes per day (CPD) as a continuous outcome variable. There was positive skew in the self-reported number of cigarettes smoked per day (CPD) at baseline (M=23.5, SD=10.4, Skew=1.7), 6 months (M=12.3, SD=10.7, Skew=1.3), and 12 months (M=11.8, SD=10.7, Skew=1.0). Further, normal quantile plots indicated lack of fit. Following log transformation, the skew reduced to 0.6, 0.1, and 0.1 respectively. Additionally, the transformed scale resulted in good fit for the normal quantile plot. The mean decline was statistically significant from a paired-test on transformed CPD from baseline to 6 months (t=27.4, df=611, p<.001) and 6 months to 12 months (t=2.2, df=611, p=.028)
Statistical Analysis
Before testing the main model, descriptive statistics for the observed variables were examined to identify extreme skewness. We identified skewness in the self-reported number of cigarettes smoked per day. We were concerned that the skewness induced on the raw data could inflate the effect size, so we conducted a log transformation. Thus, number of cigarettes smoked per day was transformed via ln(cigs+10) where “ln” is the natural log. Similar transformations—shifting by a constant—have been accomplished previously in order to adjust for skewness (Gajewski, 2004). Consequently, in our results we report standardized effect sizes rather than raw effect size.
Similar to the strategy employed by DiLorio et al. (2009), we fitted confirmatory factor analysis with Mplus 5.1 to test a measurement model for the baseline latent constructs (Brown, 2006). Note that four items is the minimum number needed to estimate a measurement having a single latent construct. Therefore, we used four items to estimate the latent constructs. This strategy was necessary in order to increase the ratio of the number of participants to model parameters; it conferred the additional benefit of making it easier to interpret the constructs. The fit for these measurement models were assessed using Root Mean Square Error of Approximation (RMSEA) and Comparative Fit Index (CFI) (Brown, 2006). An RMSEA<.08 and a CFI>0.90 were considered an adequate fit.
The results section of the SEM analysis is divided into baseline measurement model, final SEM, and alternative model considered. The baseline measurement model allowed construction of the latent variables that were parsimoniously measured by four items. Development of the final model was divided into two steps. First we allowed for testing of the relationship between different levels of MI on change in cigarettes per day. Second, we assessed mediation of behavioral latent variables at baseline and 6 months and their statistical role in predicting number of cigarettes smoked at 12 months. The alternative model tested the model stratified by baseline motivation to quit smoking. However, we had too few unmotivated smokers to deem an admissible model alternative to the final model choice. Once the measurement model was established, the final Structural Equation Model (SEM) was fitted using Mplus 5.1. We based our final model on the self-determination theory used for motivating tobacco cessation (Williams, McGregor, Sharp, Levesque et al., 2006). The main outcome was the log number of cigarettes per day at 12 months (logCIGS12). We assessed the direct effects of randomized clinical trial group category (PM, MDM, and HDM) to test the impact of different levels of motivational interviewing on outcome. We also assessed the direct effects of baseline log number of cigarettes (logCIGSb), self-efficacy, autonomous motivation, and controlled motivation as well as the indirect effects of these constructs through six-month mediating variables self-efficacy, autonomous motivation, and controlled motivation on outcome. Further, the model tested the direct effect of these six-month mediating constructs on number of cigarettes smoked at 12 months. Models were evaluated using the RMSEA and CFI criteria previously defined. To test mediation models for direct and indirect effects we conducted 10,000 bootstrap samples (Preacher & Hayes, 2008).
RESULTS
The majority of the participants included in this study were white (89.4%), under 50 years of age (58.7%), female (58.5%), who had completed high school or higher education (90%). The majority of our sample reported being ready to quit within the next 30 days at baseline (79%). Among the 612 participants included in the analysis, 23.2% had quit at 12 months and 66% requested smoking cessation medication at baseline. Numbers of cigarettes per day declined over time from 23.53 (SD=10.38) cigarettes per day at baseline to 12.31 (SD=10.69) and 11.75 (SD=10.75) at month 6 and month 12 respectively. The characteristics of the KanQuit participants were described in more detail elsewhere (Ellerbeck et al., 2009).
Baseline measurement model
Classical correlation measures (i.e., correlation of an item with a total score or a domain score where the item under study is omitted from the total score) guided item selection for behavioral latent constructs for the measurement models self-efficacy (SE), autonomous motivation (AM), and controlled motivation (CM) at baseline. Items chosen at baseline were also used for 6-month measures. Each construct originally had more than four items. Therefore, an initial set of item-total correlations were calculated and rank ordered. The top four correlations for each construct were preserved and tested for the final respective measurement model. Table 1 shows the items that were selected. SE, AM, and CM resulted in cronbach’s alpha=0.77, 0.85, and 0.81 respectively, which are above minimal standards of 0.70 (DeVellis, 2003). The item-total correlations ranged from 0.42 (‘When celebrating something’ -SE) to 0.70 (‘It is very important for many aspects of my life’ - AM); all above the recommended 0.30. Fitting an SEM simultaneously on all three of these constructs resulted in adequate goodness of fit (CFI=0.98, RMSEA=0.044).
Table 1.
Descriptive statistics of variables used to create constructs at baseline and 6 months (N=612)
| Variable | No. of items, Mean | Levels, SD | alpha | No. of items, Percent, Mean | Levels, SD | alpha |
|---|---|---|---|---|---|---|
|
| ||||||
| Baseline | 6 month | |||||
| Self-Efficacy: Baseline | 12 (4 items) | 1–5 | 0.77 | 0.84 | ||
| When I feel nervous | 2.43 | 1.24 | 0.60 | 2.81 | 1.41 | 0.74 |
| When I feel depressed | 2.68 | 1.32 | 0.63 | 2.99 | 1.42 | 0.71 |
| When I feel very anxious | 2.45 | 1.35 | 0.65 | 2.89 | 1.42 | 0.70 |
| When celebrating something | 3.22 | 1.45 | 0.42 | 3.62 | 1.37 | 0.55 |
| Autonomous Motivation: Baseline | 6 (4 items) | 1–7 | 0.85 | 0.85 | ||
| I believe it is the best thing for my health | 6.53 | 1.16 | 0.65 | 6.59 | 1.08 | 0.65 |
| It is very important for many aspects of my life | 6.33 | 1.38 | 0.70 | 6.37 | 1.22 | 0.73 |
| It is an important choice I want to make | 6.32 | 1.38 | 0.67 | 6.37 | 1.15 | 0.68 |
| Very important being as healthy as possible | 6.26 | 1.38 | 0.76 | 6.32 | 1.28 | 0.72 |
| Controlled Motivation: Baseline | 6 (4 items) | 1–7 | 0.81 | 1–7 | 0.82 | |
| Would feel guilty if I smoked | 3.47 | 2.19 | 0.65 | 3.70 | 2.20 | 0.70 |
| Others would be upset if I smoked | 3.72 | 2.30 | 0.62 | 3.72 | 2.36 | 0.63 |
| Would feel bad about myself if I smoked | 3.90 | 2.31 | 0.70 | 4.04 | 2.29 | 0.71 |
| I want others to approve of me | 2.86 | 2.23 | 0.51 | 2.74 | 2.11 | 0.56 |
Final SEM
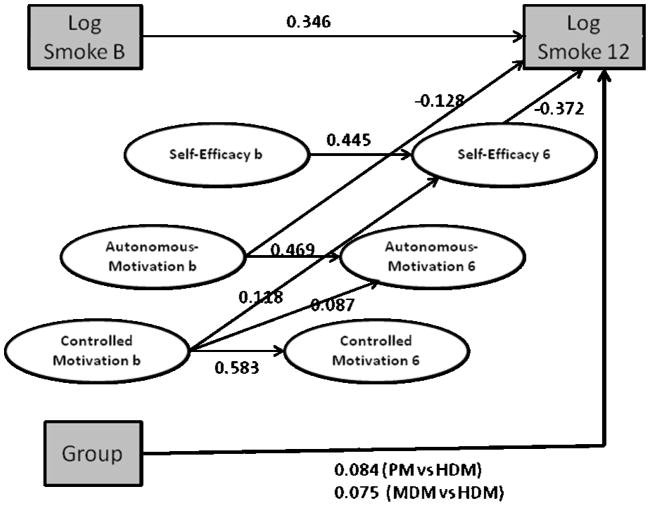
The final SEM was divided in two steps (see table 2). We included the log number of cigarettes at baseline (logCIGSb) and 12 months (logCIGS12), and clinical trial group category (PM, MDM, and HDM). The basic structure allowed logCIGS12 to be the main dependent variable with logCIGSb, group, and all behavioral latent constructs as predictors. Group category had a direct effect on logCIGS12, explaining 19% of the variance. Further, latent constructs at month 6 were multiple mediators for latent constructs at baseline. Therefore SEb, AMb, and CMb (baseline) were allowed to directly and indirectly impact logCIGS12 through mediating variables SE6, AM6, and CM6 (6 months). The overall fit of this model was adequate (CFI=0.94, RMSEA=0.045) and explained 31% of the variation in logCIGS12. The standardized path coefficients that were significant are displayed in Figure 1. For example, logCIGSb significantly predicted logCIGS12 (beta=0.346, p<.001). This indicates that for every one standard deviation increase in logCIGSb the logCIGS12 increases by 0.346 standard deviations. For treatment group difference, PM had significantly higher logCIGS12 compared to HDM (beta=0.084, p=.039) and MDM was marginally significantly higher than HDM (beta=0.075, p=.064). The results of the behavioral latent constructs can be categorized into direct effects and indirect effects. The constructs with significant direct effects on logCIGS12 were AMb (beta=−0.128, p=.007) and SE6 (beta=−0.372, p<.001). The psychosocial latent constructs also had significant direct effects between baseline and 6 months: SE6 & SEb (beta=0.445, p<.001), SE6 & CMb (beta=0.118, p=.008), AM6 & AMb (beta=0.469, p<.001), AM6 & CMb (beta=0.087, p=.039), and CM6 & CMb (beta=0.583, p<.001). All significant indirect effects on logCIGS12 went through mediator SE6. These indirect effects included CMb and SEb through mediator SE6. Multiplying respective standardized coefficients 0.118*(−0.372)= −0.044 and 0.445*(−0.372)= −0.166; indicating that SEb had the largest indirect effect (through SE6) on logCIGS12. Using the bootstrap approach, we tested baseline self-efficacy’s total direct effect on cigarettes per day at 12 months (Z=−6.5, p<.001) as well as its indirect effect (Z=−2.9, p<.004) through self-efficacy at 6-months” (Preacher & Hayes, 2008). Table 2 shows the bivariate correlation among latent variables, log smoking, and group, as other investigators may want to fit their own structural models in the future.
Table 2.
Bivariate correlations among latent variables with smoking and randomization and fit statistics for tested models
| Control group | MDM group | logSmoke B | logSmoke 12 | Self-efficacy B | Self-efficacy 6 | Autonomy B | Autonomy 6 | Controlled B | |
|---|---|---|---|---|---|---|---|---|---|
| Control Group | 1 | ||||||||
| MDM Group | 0.00 | 1 | |||||||
| logSmokeB | 0.05 | −0.08 | 1 | ||||||
| logSmoke12 mo | 0.18 | 0.13 | 0.42 | 1 | |||||
| Self-efficacy B | 0.02 | 0.03 | −0.04 | −0.15 | 1 | ||||
| Self-efficacy 6 | 0.02 | 0.07 | −0.03 | −0.41 | 0.460 | 1 | |||
| Autonomy B | 0.02 | −0.06 | −0.02 | −0.21 | 0.193 | 0.18 | 1 | ||
| Autonomy 6 | 0.01 | 0.04 | 0.02 | −0.17 | 0.103 | 0.23 | 0.64 | 1 | |
| Controlled B | 0.09 | 0.04 | −0.05 | −0.11 | 0.162 | 0.19 | 0.40 | 0.31 | 1 |
| Controlled 6 | 0.01 | 0.06 | −0.05 | −0.18 | 0.057 | 0.25 | 0.30 | 0.42 | 0.71 |
|
| |||||||||
| Model & fit statistics
| |||||||||
| Model | CFI>.9 RMSEA<.08 |
90% CI | |||||||
| Measure Baseline | 0.98 | 0.04 | (.03–.05) | ||||||
| FullModel +Meds | 0.94 | 0.04 | (.04–.05) | ||||||
| Full no Meds-Final | 0.94 | 0.05 | (.04–.05) | ||||||
Note: MDM group: moderate disease management group, logSmokeB=natural log transformation of smoking baseline + 10; logSmoke6= natural log transformation of smoking 6 months; logSmoke12= natural log transformation of smoking baseline 12 months; Self-efficacy B=Self Efficacy baseline; SE6=Self Efficacy 6 months; Autonomy B=Autonomous Motivation baseline; Autonomy 6 =Autonomous Motivation 6 months; Controlled B=Controlled Motivation baseline; Controlled 6=Controlled Motivation 6 months
Figure 1.
Structural equation model. Log SmokeB=natural log transformation of smoking baseline + 10; Log Smoke12=natural log transformation of smoking 12 months+ 10. Ovals are latent variables and rectangles are observed variables. Items associated with latent variables are not shown. Paths with statistically significant relations are shown (p<.05). All path coefficients are standardized except Group to Log Smoke 12. CFI=0.940 and RMSEA=0.045. The variance in Log igs 12 explained by the model using grey boxes only is R2=0.194; using all variables R2=0.306.
Alternative model considered: ‘readiness to quit.’
An alternative model was fitted after stratifying participants based on their baseline readiness to quit smoking in the next 30 days. Our hypothesis was that participants who were not ready to quit in the next 30 days benefit differently from motivational interview compared to participants who were ready to quit. This model was rejected because it had 612 participants with 196 parameters (3.1 participants per parameter). In order to preserve the model we would need at least five participants per parameter.
Discussion
This study examined the potential of self-determination theory to explain the mediating mechanisms by which MI counseling was associated with change in smoking behaviors during a 12 months intervention. In the final model MI intensity independently predicted change in cigarettes per day at 12 months. Unexpectedly, our findings indicated that the MI treatment group effect was not relate to autonomous motivation, controlled motivation, or self-efficacy at baseline and 6 months, the hypothesized mediators.
Interestingly, despite of the lack of an effect of MI treatment on the hypothesized mediators, mediator variables were related to change in smoking at 12 months in expected ways. Specifically, we found that: 1) higher self-efficacy at baseline predicted higher self-efficacy at 6 months, which in turn predicted quitting at 12 months (Maibach, Flora, & Nass, 1991; Warnecke et al., 2001); 2) higher autonomous motivation at baseline related directly to quitting at 12 months, which is consistent with a similar finding in the Williams et al.’s (2002) study; and 3) unexpectedly, higher controlled motivation at baseline predicted higher self-efficacy at 6 months, which in turn predicted quitting at 12 months.
As found in prior studies, change in self-efficacy was strongly associated with change in cigarettes smoked per day at 12 months (Maibach et al., 1991; Warnecke et al., 2001). Controlled motivation at baseline had an indirect impact on cigarettes smoked per day at 12 months mediated by self-efficacy. Despite a generally negative connotation of controlled motivation, our study suggests that baseline controlled motivation is significantly related to higher self-efficacy at 6 months as well as higher autonomous motivation at 6 months. External pressure to change (whether from environmental restriction or a request of someone considered important) changed behavior even though motivation to perform the behavior was not internalized initially. Taken together, it appears that some level of external pressure (i.e. controlled motivation) may have some benefit in initiating behavioral change (Berg et al., 2006; Strong & Huon, 1999). Although this appears to contradict SDT, it accords with the Theory of Planned Behavior, which posits subjective norms (i.e., perceived social pressure to perform or not perform certain behaviors) as one factor related to behavioral intention. However, participants were still in active counseling at our 12-month end point—controlled motivation may not be related to long-term abstinence. Future studies should explore if after treatment, controlled motivation remains as a significant predictor of cessation.
The finding that SDT variables did not mediate the relationship between different levels of MI on smoking are contrary to recent articles supporting the role of SDT variables on smoking among smokers recruited in primary care facilities (Williams & Deci, 2001; Williams et al., 2002). Most recently, Williams et al. (2006b) found that a 4-contact primary care based intervention MI consistent counseling based on SDT significantly improved 12 month quit rates compared to community care. Mediation analyses found that participants in the intervention group reported greater 1) autonomy support, 2) changes in reasons for using medications, 3) perceived competence for quitting, and 4) days on medications (Williams et al., 2006b). Among participants who elected to see a physician during the trial, autonomous motivation was even higher.
Methodological differences, including use of differing measures and intervention content, may explain possible contradictory findings. It could be that MI works via SDT, but KanQuit measures failed to detect it. First, in KanQuit, the SDT variable of perceived competence was measured by a proxy measure (i.e., the self-efficacy scale), whereas in the Williams et al. (2006b) study, it was measured by the perceived competence scale (PCS), which was developed specifically to measure a construct in SDT. Hence, self-efficacy may not measure perceived competence properly, as conceptualized in SDT, and KanQuit study measures may not have captured the effects of MI on perceived competence. Second, in the Williams et al. (2006b) study, the follow-up assessment of perceived competence and autonomy support was conducted one month after the program began, whereas the current study assessed these factors at baseline and month 6. This is an important distinction given that research has demonstrated that motivation and self-efficacy increase early in counseling (Irving et al., 2004; Snyder, Ilardi, Michael, & Cheavens, 2000). KanQuit may have measured mediators too late to detect the effects of MI on them.
Alternatively, it could be that MI, as delivered in KanQuit, did not have its impact through SDT mechanisms. In the Williams et al. (2006b) study, counseling sessions were delivered mostly face-to-face, while counseling sessions in KanQuit were delivered exclusively by phone. Although research has documented few differences in counseling modality (i.e., in person vs. via telephone) (Lemmens, Oenema, Knut, & Brug, 2008; Zaylor, 1999), it may be that important interpersonal aspects of MI were not optimally achieved in KanQuit due to the telephone-based delivery. The motivational-based counseling content in these two studies are significantly different. Differently from KanQuit, in Williams et al.’s (2006b) study, counseling content included perceived health risk about smoking and it also included information regarding participants’ 10-year-risk for developing cardiovascular disease (CVD), stating that quitting smoking would cut their risk by 50% reduction within 12 months. Last, we focused on measuring SDT variables, but there are other significant psycho-social mechanisms, such as relational factor, “commitment language”, and change talk (Miller & Rose, 2009) that may account for the effects of MI.
The study has a number of limitations. Because this sample was predominantly white, from rural areas, had access to regular health care, and smoked at least 10 cigarettes per day, it may not be representative of all smokers. We included in our analyses only those participants who responded to both the 6- and 12-month assessments. Thus, we cannot draw conclusions about those participants who did not complete these assessments. We could not add a measure of nicotine dependence in the model, because our dependent variable, number of cigarettes per day (which is an item within the nicotine dependence scale) is highly correlated with nicotine dependence. Adding both variables in the model would significantly increase the variance between both variables influencing the accuracy of estimates. While in the main outcome paper we report biochemical verification among participants who quit, in this manuscript we did not include biochemical validation of quitting status at 12 months. Last, due to the study design participants received different numbers of MI counseling sessions, which may have reduced our ability to detect mediation.
Another limitation is that we did not evaluate the fidelity of our MI delivery, that is, we did not comprehensively assess how it was actually delivered. However, we strongly supported appropriate delivery of MI, through several mechanisms (e.g., frequent and regular supervisions, in-depth training, self-evaluations after each session).
In addition, we did not measure all other psychosocial factors that might account for increases in self-efficacy outside of motivational interviewing, such as social support. As a result, we were not able to examine how these factors might influence the results of motivational interviewing. We did not assess participants’ perceptions of their counselors’ autonomy supportiveness in the context of the sessions. Last, we did not assess the role of medication use and adherence within the current trial. In this randomized trial a quit attempt was not a requirement to be in the study and using cessation medication was optional. For example, at baseline approximately 60% of participants received medication. Furthermore, participants who quit smoking could still be taking medication and participants who were still smoking could also be taking medication. Thus, at any single point of the study (baseline, 6mo, 12 mo) there are multiple possible combinations of smoking status and medication use. In this structural equation model we could not address the impact of psychological variables on medication utilization.
However, a few strengths of the study should be noted. Our sample included smokers at all stages of readiness to quit and therefore allows for a greater range in baseline motivation and self-efficacy than many previous studies. We also used SEM as a data analysis method that allowed us to investigate the direct and indirect effects of measured psycho-social variables related to smoking.
In conclusion, contrary to our hypothesis, the effect of different levels of MI counseling on smoking was not mediated by self-efficacy, autonomous and controlled motivation. However, changes in self-efficacy variables over time predicted positive smoking outcome. This study confirmed that the most significant psychosocial pathway to quitting smoking is through increased self-efficacy, and hence treatment should emphasize this psychosocial characteristic. Another practice implication is the need for counselors to strike a balance between promoting social norms that discourage smoking while also supporting the clients’ autonomy during treatment interactions. Further studies should assess the social pressures experienced by participants to quit smoking, and find ways to help participants capitalize on these pressures to change their own health behaviors.
Acknowledgments
This research was supported by grant number CA 1102390 from the National Cancer Institute at the National Institutes of Health and NCI-5K01CA136993-03.
References
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol. 2003;71(5):862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- Baranowski T, Cullen KW, Baranowski J. Psychosocial correlates of dietary intake: advancing dietary intervention. Annu Rev Nutr. 1999;19:17–40. doi: 10.1146/annurev.nutr.19.1.17. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Cox LS, Nazir N, Mussulman L, Ahluwalia JS, Ellerbeck EF. Correlates of home smoking restrictions among rural smokers. Nicotine and Tobacco Research. 2006;8(3):353–360. doi: 10.1080/14622200600670132. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Cox S, Lisa MDJ, Greiner KA, Ellerbeck EF. Correlates of Self-efficacy among Rural Smokers. J Health Psychol. 2008;13(3):416–421. doi: 10.1177/1359105307088144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA. Confirmatory Factor Analysis for Applied Research. Guilford Press; 2006. [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Burke BL, Dunn C, Atkins DC, Phelps JS. The Emerging Evidence Base for Motivational Interviewing: A Meta-Analytic and Qualitative Inquiry. Journal of Cognitive Psychotherapy: An International Quarterly. 2004;18(4):309–322. [Google Scholar]
- Cox LS, Cupertino AP, Mussulman LM, Nazir N, Greiner KA, Mahnken JD, et al. Design and baseline characteristics from the KAN-QUIT disease management intervention for rural smokers in primary care. Prev Med. 2008;47(2):200–205. doi: 10.1016/j.ypmed.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL, Koestner R, Ryan RM. A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychol Bull. 1999;125(6):627–668. doi: 10.1037/0033-2909.125.6.627. discussion 692–700. [DOI] [PubMed] [Google Scholar]
- DeVellis RF. Scale development: Theory and applications. 2. CA: Sage; 2003. [Google Scholar]
- DiLorio C, McCarty F, DePadilla L, Resnicow K, Holstad MM, Yeager K, Sharma SM, Morisky DE, Lundberg B. Adherence to antiretroviral medication regimens: a test of a psychosocial model. AIDS Behav. 2006;13(1):10–22. doi: 10.1007/s10461-007-9318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellerbeck EF, Mahnken JD, Cupertino AP, Cox LS, Greiner KA, Mussulman LM, et al. Effect of varying levels of disease management on smoking cessation: a randomized trial. Ann Intern Med. 2009;150(7):437–446. doi: 10.7326/0003-4819-150-7-200904070-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etter JF, Bergman MM, Humair JP, Perneger TV. Development and validation of a scale measuring self-efficacy of current and former smokers. Addiction. 2000;95(6):901–913. doi: 10.1046/j.1360-0443.2000.9569017.x. [DOI] [PubMed] [Google Scholar]
- Fiore M, Jaen CR, Baker TB. Treating Tobacco Use and Dependence: 2008 Update. May 2008. Rockville, MD: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Gajewski BJ. Correspondence estimation of the source profiles in receptor modeling. Environmetrics. 2004;15:613–634. [Google Scholar]
- Heckman CJ, Egleston BL, Hofmann MT. Efficacy of motivational interviewing for smoking cessation: a systematic review and meta-analysis. Tob Control. 2010;19(5):410–416. doi: 10.1136/tc.2009.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: examples from the child-clinical and pediatric psychology literatures. J Consult Clin Psychol. 1997;65(4):599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- Irving LM, Snyder CR, Cheavens J, Gravel L, Hanke J, Hillberg P, et al. The relationships between hope and outcomes at the pre-treatment, beginning, and later phases of psychotherapy. Journal of Psychotherapy Integration. 2004;14:419–443. [Google Scholar]
- Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005;(2):CD001292. doi: 10.1002/14651858.CD001292.pub2. [DOI] [PubMed] [Google Scholar]
- Lemmens V, Oenema A, Knut IK, Brug J. Effectiveness of smoking cessation interventions among adults: a systematic review of reviews. Eur J Cancer Prev. 2008;17(6):535–544. doi: 10.1097/CEJ.0b013e3282f75e48. [DOI] [PubMed] [Google Scholar]
- Lundahl BW, Kunz C, Brownwell C, Tollefson D, Burke BL. A Meta-Analysis of Motivational Interviewing: Twenty-Five Years of Empirical Studies. Research on Social Work Practice. 2010;20(2):137–160. [Google Scholar]
- Maibach E, Flora JA, Nass C. Changes in self-efficacy and health behavior in response to a minimal contact community health campaign. Hlth Comm. 1991;3(1):1–15. [Google Scholar]
- Markland D, Ryan RM, Tobin VJ, Rollnick S. Motivational interviewing and self-determination theory. J Soc Clin Pyschol. 2005;246:811–831. [Google Scholar]
- Marks D. Publication Guidelines for Intervention Studies in the Journal of Health Psychology. J Health Pyschol. 2010;15:5–78. [Google Scholar]
- McCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychological Methods. 2002;7:19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Kuhl J, Deci EL. Nature and autonomy: an organizational view of social and neurobiological aspects of self-regulation in behavior and development. Dev Psychopathol. 1997;9(4):701–728. doi: 10.1017/s0954579497001405. [DOI] [PubMed] [Google Scholar]
- Snyder CR, Ilardi SS, Michael ST, Cheavens J. Hope theory: Updating a commonprocess for psychological change. New York: John Wiley & Sons, Inc; 2000. [Google Scholar]
- Strong KG, Huon GF. Controlled motivation and the persistence of weight-loss dieting. European Eating Disorders Review. 1999;7(2):136–146. [Google Scholar]
- Vansteenkiste M, Sheldon KM. There’s nothing more practical than a good theory: integrating motivational interviewing and self-determination theory. Br J Clin Psychol. 2006;45(Pt 1):63–82. doi: 10.1348/014466505X34192. [DOI] [PubMed] [Google Scholar]
- Warnecke RB, Morera O, Turner L, Mermelstein R, Johnson TP, Parsons J, et al. Changes in self-efficacy and readiness for smoking cessation among women with high school or less education. J Health Soc Behav. 2001;42(1):97–110. [PubMed] [Google Scholar]
- Williams GC, Deci EL. Activating patients for smoking cessation through physician autonomy support. Medical Care. 2001;39:813–823. doi: 10.1097/00005650-200108000-00007. [DOI] [PubMed] [Google Scholar]
- Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21(10):1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- Williams GC, Gagne M, Ryan RM, Deci EL. Facilitating autonomous motivation for smoking cessation. Health Psychol. 2002;21:40–50. [PubMed] [Google Scholar]
- Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70(1):115–126. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- Williams GC, McGregor H, Sharp D, Kouides RW, Levesque CS, Ryan RM, et al. A Self-Determination Multiple Risk Intervention Trial to Improve Smokers’ Health. J Gen Intern Med. 2006a;21(12):1228–1294. doi: 10.1111/j.1525-1497.2006.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GC, McGregor HA, Sharp D, Levesque C, Kouides RW, Ryan RM, et al. Testing a self-determination theory intervention for motivating tobacco cessation: supporting autonomy and competence in a clinical trial. Health Psychol. 2006b;25(1):91–101. doi: 10.1037/0278-6133.25.1.91. [DOI] [PubMed] [Google Scholar]
- Williams GC, Rodin GC, Ryan RM, Grolnick WS, Deci EL. Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychol. 1998;17:269–276. doi: 10.1037//0278-6133.17.3.269. [DOI] [PubMed] [Google Scholar]
- Williams GC, Ryan RM, Deci EL. Health-Care, Self-Determination Theory Packet. 2004 Retrieved June 10, 2004, from http;// www.psych.rochester.edu/SDT./measures.html.
- Zaylor C. Clinical outcomes in telepsychiatry. J Telemed Telecare. 1999;5(Suppl 1):S59–60. doi: 10.1258/1357633991932577. [DOI] [PubMed] [Google Scholar]