Introduction
It is has long been appreciated that the presence of prominent anxiety in major depressive episodes is associated with a greater severity and persistence of depressive symptoms, whether that anxiety is manifest by the presence of panic attacks (1–4) or by more global dimensions of anxiety (5–8). Recent work has focused on the significance of anxiety in bipolar disorder and has yielded similar results. Bipolar subjects with high anxiety levels, or with coexisting DSM-IV anxiety disorders, appear to have higher likelihoods of rapid switching (9–11) and of suicidal behavior (12), shorter euthymic periods (12), poorer treatment response (13, 14) and, in the only large-scale follow-up on the topic, a longer time to remission from the index affective episode (15).
The following uses data from a long-term, high surveillance-intensity follow-up of subjects with type I or type II bipolar disorder to determine the effects of comorbid anxiety on subsequent affective morbidity. The analyses, in particular, address the following questions: 1) what is the effect of anxiety on the time spent in depressive or manic/hypomanic episodes, 2) what measure of anxiety best reflects this relationship, 3) how persistent is the relationship and, 4) does this effect vary by age, sex or index episode polarity (depressed, manic or polyphasic)?
Method
Subjects
The NIMH Collaborative Depression Study (CDS) recruited inpatients and outpatients who satisfied Research Diagnostic Criteria (RDC) (16) for major depressive disorder (MDD), manic disorder, or schizoaffective disorder, from the years 1978 to 1981. All were seeking treatment at one of five academic centers: Massachusetts General Hospital in Boston, New York State Psychiatric Institute and Columbia-Presbyterian Hospital in New York City, Rush Presbyterian Hospital in Chicago, Washington University in St. Louis and the University of Iowa Hospitals and Clinics in Iowa City. Inclusion criteria required participants to be at least 18 years old, not mentally retarded, English-speaking, Caucasian, and knowledgeable of their biological parents. All subjects were seeking treatment at the time of enrollment but inclusion did not specify the level or type of treatment received.
In the current analysis subjects with manic or hypomanic syndromes manifesting before intake, or at any time during follow-up, were designated as having bipolar disorder. Those with RDC schizoaffective disorder, other than the mainly-schizophrenic subtype, were included. The RDC mainly-schizophrenic subtype of schizoaffective disorder is equivalent to DSM-IV schizoaffective disorder but the remainder of RDC schizoaffective manic or depressed cases nearly all meet DSM-IV criteria for manic or major depressive disorder with mood-incongruent psychotic features.
Procedures
After subjects provided informed consent, professional raters conducted structured interviews using the Schedule for Affective Disorders and Schizophrenia (SADS) (17). Item ratings and the resulting diagnoses integrated information from the subject interview, from review of medical records, and from informants when available.
Follow-up assessments then took place semiannually for the subsequent five years, and annually thereafter. Raters used the Longitudinal Interval Follow-up Evaluation (LIFE) (18) and later variants, the LIFE-II and SLICE, to record descriptions of the clinical course and psychosocial outcome based on direct subject interview and on medical record review.
These instruments used LIFE Psychiatric Symptom Ratings (PSRs) to track all RDC syndromes that had been active at intake or that developed during follow-up. Interviewers helped subjects identify points at which symptom levels had changed and then quantified the levels present between those points. For major depression, manic disorder, schizoaffective depression and schizoaffective mania these symptom levels were assigned scores of “1” to “6.” A score of “1” indicated no symptoms, “2” indicated the presence of one to two symptoms to a mild degree, “5” indicated a full syndrome, and “6” a relatively severe, full syndrome. Individuals with scores of “3” and “4” had the continued presence of an episode with less than the number of symptoms necessary for an initial diagnosis. The end of an episode required eight consecutive weeks of PSR ratings no greater than “2” and a new episode required that the subject again met criteria for definite major depression, mania, or schizoaffective disorder.
Data Analytic Procedures
We selected the persistence of depressive episodes as the principal outcome measure because earlier analyses have shown that depression dominates the symptomatic course of the bipolar disorders (19, 20). This measure was quantified as the percent of follow-up weeks in episodes of major depression or schizoaffective depression as indicated by PSR ratings of 3 or more for either syndrome.
Because the presence or absence of cycling in an index episode, as well as its phase, have established prognostic importance (21–24) subjects were initially grouped according to the polarity of their intake episode at the time of the baseline assessment, as purely manic, purely depressed, cycling or mixed. Only eleven subjects were in mixed episodes and were therefore included with subjects who were cycling (Table 1). The three groups were compared by baseline demographic and clinical measures and by the principal outcome measure, the proportion of weeks of follow-up in major depressive or schizoaffective depression episodes, to determine whether these groups should be separated or combined in the analyses of outcome prediction.
Table 1.
Baseline Demographic and Clinical Measures by Type of Index Episode
| pure manic | pure depressed | cycling | |
|---|---|---|---|
| n | 96 | 169 | 168 |
| number (%) female 1 | 46 (47.9) | 109 (64.5) | 94 (56.0) |
| mean (SD) age | 36.5 (13.3) | 36.6 (14.4) | 35.9 (11.9) |
| number (%)2 | |||
| - bipolar I | 96 (100) | 70 (41.4) | 122 (72.6) |
| - bipolar II | 0 – | 99 (58.6) | 46 (27.4) |
| number (%) with lifetime | |||
| ASPD | 2 (2.1) | 5 (3.0) | 2 (1.2) |
| alcoholism | 28 (29.2) | 46 (27.2) | 45 (26.8) |
| drug dependence | 7 (7.3) | 18 (0.7) | 15 (8.9) |
| OCD | 2 (2.1) | 5 (3.0) | 4 (2.4) |
| phobic disorder | 3 (3.1) | 10 (5.9) | 10 (6.0) |
| panic disorder | 1 (1.0) | 9 (5.3) | 7 (4.2) |
| GAD | 1 (5.0) | 11 (55.0) | 8 (40.0) |
| number (%) with panic attacks in index episode 3 | 8 (8.3) | 51 (30.2) | 48 (28.6) |
| mean (SD) | |||
| somatic anxiety 4 | 1.3 (0.6) | 1.8 (0.9) | 1.7 (.9) |
| psychic anxiety 5 | 1.9 (1.3) | 4.0 (1.5) | 3.5 (1.6) |
| anxiety 6 | 3.6 (2.2) | 7.2 (2.3) | 6.3 (2.5) |
| mean (SD) weeks of follow-up | 809.3 (464.2) | 962.3 (401.9) | 907.1 (442.5) |
X2 = 7.16, df = 2, p = 0.028
X2 = 98.9, df = 2, p < 0.001
X2 = 17.9, df = 2, p < 0.001
F = 13.4, df = 2/430, p < 0.001; Dunnett T3 post-hoc: manic vs depressed, p < .001; manic vs cycling p < 0.001
F = 60.9, df = 2/430, p < 0.001; Dunnett T3 post-hoc: manic vs depressed, p < .001, manic vs cycling, p < .001, depressed vs cycling, p = 0.022
F = 75.1, df = 2/430, p < 0.001; Dunnett T3 post-hoc manic vs depressed p < 0.001, manic vs cycling, p < .001 depressed vs cycling p = 0.002
We likewise tested for significant relationships between percent time in depressive episodes and sex, age at intake, lifetime non-anxiety co-morbid diagnoses (alcoholism, drug dependence and antisocial personality disorder), bipolar type (I versus II), intake episode polarity (cycling, pure depressive or pure manic) and four measures of concurrent anxiety. These were the presence or absence of panic attacks within the index episode, the 6-point SADS ratings of somatic and of psychic anxiety (items #263 and #265), and the co-presence of any life-time RDC anxiety disorder: panic disorder, phobic disorder, obsessive-compulsive disorder (OCD), or generalized anxiety disorder (GAD). These anxiety measures were entered into an SPSS general linear model (GLM) to determine which added to the prediction of time depressed. Sex, age at intake, non-anxiety comorbid diagnoses, bipolar type or episode polarity was included in the model if univariate analysis had shown that factor to have a significant relationship to time depressed.
After selecting the most salient predictor of subsequent morbidity we next tested for the persistence of the relationship by considering depressive morbidity in each of four, five-year periods that comprised the follow-up period. These last analyses were restricted to subjects who completed the respective five-year follow-up period.
The above procedures were repeated for the prediction of proportion of weeks in episodes of mania, schizoaffective mania or hypomania. Two-tailed tests and an alpha of 0.05 were used throughout.
Results
Depressive Episodes
Neither sex, baseline age, the presence of antisocial personality disorder, alcoholism or drug dependence predicted the percent of weeks in depressive episodes during follow-up. The 284 with past or future manic episodes (bipolar I) were in depressive episodes for a lower percent of weeks during follow-up (mean = 36.6, SD = 27.7) than were the 145 with only episodes of hypomania (bipolar II) (mean = 36.5, SD = 27.7); (F = 10.3, p = 0.001). A strong relationship also existed between baseline episode polarity and subsequent time in depressive episodes; mean (SD) values were 24.3 (20.1) of follow-up weeks for those who entered the study with a pure manic episode and 37.7 (27.1), 33.0 (29.6) for those who entered with a pure depressive episode, and 22.6% (26.1) for those with a cycling episode (F = 25.8, df = 2/424, p < 0.000) Dunnett T3: manic versus depressed, p < 0.001, manic versus cycling, p < 0.001). Those in pure depressive episodes did not differ significantly from those who cycled, however (Dunnett t CI = −.018, .113, p = 0.188), and because baseline anxiety measures also separated the pure mania group from the other two, subsequent analyses condensed subject grouping to two polarity categories: pure mania and pure depression or cycling. When bipolar type and polarity category were entered together, polarity category was predictive (F = 37.6, p < .000) and diagnosis was not (F = 0.90, p = 0.034). Subsequent analyses therefore included only polarity category.
When tested individually, together with polarity category, neither the presence nor absence of panic attacks in the index episode (F = 2.2, p = 0.14), nor the presence or absence of any anxiety disorder (F = 2.4, p = 0.12) predicted subsequent time in depressive episodes but somatic (F = 7.9, p = 0.005) and psychic (F = 11.2, p = 0.001) anxiety did. With these two measures together psychic and anxiety remained highly significant (F = 7.0, p = 0.008) and somatic anxiety was of borderline significance (F = 3.8, p = 0.052). Because somatic anxiety appeared to add somewhat to the prediction of time depressed the two measures were combined into a single measure of “global anxiety” for further analyses. When this scale was, for graphic purposes, condensed from 12 to 6 points and plotted against the proportion of follow-up weeks in depressive episodes, a continuous relationship emerged with no prognostically meaningful threshold for the separation of anxious and non-anxious subjects (Figure 1).
Figure 1.
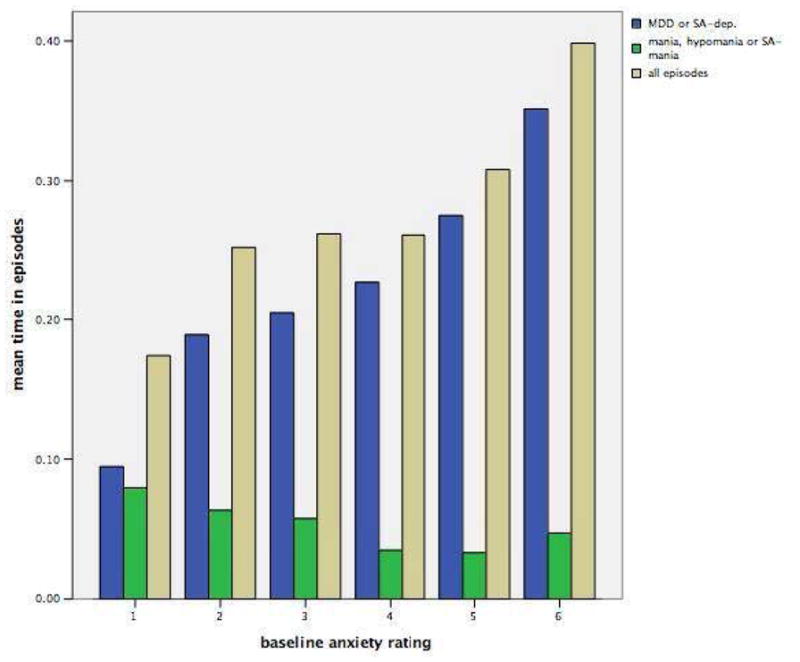
Baseline Global Anxiety Rating and Subsequent Time in Episodes among 433 Bipolar Subjects
Combinations of anxiety level and index episode polarity yielded large outcome differences. The subjects with purely manic index episodes and with a baseline global anxiety level below the median value of 6 spent only 12.3% (SD = 19.9) of the follow-up weeks in depressive episodes. The 237 subjects with depressed or cycling index episodes and with an above-median global anxiety measure baseline spent nearly three times as many weeks in depressive episodes, 37.8% (SD = 27.9).
A series of GLM analyses for each of the four, five-year follow-up periods showed that the relationship between the index episode polarity at intake and the proportion of follow-up time depressed faded after the first ten years while global anxiety continued to predict, though at modest or trend levels, throughout the twenty years (Table 2). Sex was not predictive in any of the four follow-up periods.
Table 2.
Relationships of Baseline Anxiety and Episode Type to Percent Time in Depressive Episodes by Follow-up Period 1
| 1 – 5 yrs, n = 401 | 6 – 10 yrs, n = 332 | 11–15 yrs, n = 302 | 16–20 yrs, n = 255 | |
|---|---|---|---|---|
| F (p) | F (p) | F (p) | F (p) | |
| % of weeks in major depressive or SA – D episodes | ||||
| - global anxiety2 | 5.0 (.026) | 2.0 (.153) | 5.6 (.019) | 3.7 (.055) |
| - episode polarity3 | 25.2 (.000) | 9.0 (.003) | 3.6 (.059) | 1.9 (.170) |
GLM analyses for subjects who completed each five-year period
combination of psychic and somatic anxiety measures
pure mania vs pure depression or cycling
Manic/hypomanic Episodes
Neither sex nor baseline age was associated with subsequent time in manic/hypomanic episodes, nor was the presence of alcoholism, drug abuse, ASPD, or of any anxiety disorder associated with subsequent manic/hypomanic morbidity. Both episode polarity and bipolar type predicted subsequent manic/hypomanic morbidity and, when both were included in a GLM model, bipolar type (I versus II) (F = 31.0, p < 0.001) but not episode polarity (F = 0.81, p = 0.368) was predictive. When the presence of any anxiety disorder, the presence of panic attacks, somatic anxiety and psychic anxiety were entered individually in GLM analyses, with bipolar type none were significantly predictive.
Discussion
Taken singly, two of the four baseline anxiety measures tested –somatic anxiety and psychic anxiety – were predictive of the proportion of weeks during follow-up spent in episodes of MDD or schizoaffective depression. The combination of these measures as “global anxiety” showed a continuous, step-wise dose-effect on subsequent depressive morbidity. This finding supports a dimensional over a categorical view of anxiety in bipolar disorder, at least for this important outcome.
The phase of index episode at the time of intake was also strongly associated with subsequent depressive morbidity such that subjects who had entered the study in a purely manic episode experienced substantially less depressive morbidity. This is consistent with a report early in the CDS follow-up that showed that recovery one year after intake was much more likely for those bipolar patients whose index episode was purely manic than for those whose index episode was depressed or mixed (25). The present findings suggest that the prognostic importance of episode polarity extends well beyond a year. Though episode polarity and global anxiety level were highly interrelated at intake, both were independently predictive of subsequent depressive morbidity. These two factors together can thus be considered a powerful prognostic formulation.
As with long-term follow-up studies generally, the CDS did not assign or control treatment. Though essentially all subjects were receiving some type of medication for affective disorder when they began the study, many were subsequently without somatic treatment for extended periods (23–28). Earlier analyses have shown that CDS subjects whose previous episodes have been more frequent or severe received more intensive somatotherapy and that, after control for these antecedent variables, the intensity of somatotherapy was associated with a higher likelihood of recovery from a given episode (27, 28). If higher anxiety levels, and a subsequently greater persistence of depressive symptoms, resulted in higher intensities of somatotherapy, the results of that treatment would have tended to lessen the apparent relationship between anxiety levels and later depressive morbidity. The results described here are therefore more likely to be an under-estimate than an over-estimate of the relationship between anxiety level and subsequent depressive morbidity.
The observation that the strength of the relationship between anxiety and depressive morbidity changed little over a twenty-year period suggests that anxiety levels mark a type, rather than a phase, of an individual’s bipolar illness. This is consistent with evidence from family studies that the coexistence of panic attacks and bipolar disorder in probands substantially increases the risk for this coexistence in family members (9, 29). Such comorbidity may thus help to identify phenotypes with unique genetic determinants. However, the identification of an optimal threshold for separating bipolar episodes with low and high levels of anxiety will present a challenge for such investigations.
Acknowledgments
Supported by NIH grant MH025416
Footnotes
Disclosures and Acknowledgements
Conducted with the current participation of the following investigators: M.B. Keller, M.D. (Chairperson, Providence, RI); W. Coryell, M.D. (Co-Chairperson, Iowa City, IA); D.A. Solomon, M.D. (Providence, RI); W. Scheftner, M.D. (Chicago, IL); J. Endicott, Ph.D., A.C. Leon, Ph.D., and J. Loth, M.S.W. (New York, NY); and J. Rice, Ph.D., (St. Louis, MO). Other current contributors include H.S. Akiskal, M.D., J. Fawcett, M.D., L.L. Judd, M.D., P.W. Lavori, Ph.D., J.D. Maser, Ph.D., and T. I. Mueller, M.D.
This manuscript has been reviewed by the Publication Committee of the Collaborative Depression Study and has its endorsement. The data for this manuscript came from the National Institute of Mental Health (NIMH) Collaborative Program on the Psychobiology of Depression -Clinical Studies. The Collaborative Program was initiated in 1975 to investigate nosologic, genetic, family, prognostic, and psychosocial issues of mood disorders, and is an ongoing, long-term multidisciplinary investigation of the course of mood and related affective disorders. The original principal and co-principal investigators were from five academic centers and included Gerald Klerman, M.D.* (Co-Chairperson), Martin Keller, M.D., Robert Shapiro, M.D.* (Massachusetts General Hospital, Harvard Medical School), Eli Robbins, M.D.*, Paula Clayton, M.D., Theodore Reich, M.D.,* Amos Wellner, M.D.,* (Washington University Medical School), Jean Endicott, Ph.D., Robert Spitzer, M.D., (Columbia University), Nancy Andreasen, M.D., Ph.D., William Coryell, M.D., George Winokur, M.D.* (University of Iowa), Jan Fawcett, M.D., William Scheftner, M.D., (Rush-Presbyterian-St. Luke’s Medical Center). The NIMH Clinical Research Branch was an active collaborator in the origin and development of the Collaborative Program with Martin M. Katz, Ph.D., Branch Chief as the Co-Chairperson and Robert Hirschfeld, M.D. as the Program Coordinator. Other past collaborators include J. Croughan, M.D., M.T. Shea, Ph.D., R. Gibbons, Ph.D., M.A. Young, Ph.D., D.C. Clark, Ph.D.
*deceased
Declaration of Interests: None
References
- 1.Coryell W, Endicott J, Andreasen NC, Keller MB, Clayton PJ, Hirschfeld RM, Scheftner WA, Winokur G. Depression and panic attacks: the significance of overlap as reflected in follow-up and family study data. Am J Psychiatry. 1988;145(3):293–300. doi: 10.1176/ajp.145.3.293. [DOI] [PubMed] [Google Scholar]
- 2.Grunhaus L, Pande AC, Brown MB, Greden JF. Clinical characteristics of patients with concurrent major depressive disorder and panic disorder. Am J Psychiatry. 1994;151(4):541–6. doi: 10.1176/ajp.151.4.541. [DOI] [PubMed] [Google Scholar]
- 3.Johnson J, Weissman MM, Klerman GL. Panic disorder, comorbidity, and suicide attempts. Arch Gen Psychiatry. 1990;47(9):805–8. doi: 10.1001/archpsyc.1990.01810210013002. [DOI] [PubMed] [Google Scholar]
- 4.VanValkenburg C, Akiskal HS, Puzantian V, Rosenthal T. Anxious depressions. Clinical, family history, and naturalistic outcome--comparisons with panic and major depressive disorders. J Affect Disord. 1984;6(1):67–82. doi: 10.1016/0165-0327(84)90009-0. [DOI] [PubMed] [Google Scholar]
- 5.Clayton PJ, Grove WM, Coryell W, Keller M, Hirschfeld R, Fawcett J. Follow-up and family study of anxious depression. Am J Psychiatry. 1991;148(11):1512–7. doi: 10.1176/ajp.148.11.1512. [DOI] [PubMed] [Google Scholar]
- 6.Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, Gibbons R. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147(9):1189–94. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- 7.Mykletun A, Bjerkeset O, Dewey M, Prince M, Overland S, Stewart R. Anxiety, depression, and cause-specific mortality: the HUNT study. Psychosom Med. 2007;69(4):323–31. doi: 10.1097/PSY.0b013e31803cb862. [DOI] [PubMed] [Google Scholar]
- 8.Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, Biggs MM, Zisook S, Leuchter A, Howland R, Warden D, Trivedi MH. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165(3):342–51. doi: 10.1176/appi.ajp.2007.06111868. [DOI] [PubMed] [Google Scholar]
- 9.MacKinnon DF, Zandi PP, Cooper J, Potash JB, Simpson SG, Gershon E, Nurnberger J, Reich T, DePaulo JR. Comorbid bipolar disorder and panic disorder in families with a high prevalence of bipolar disorder. Am J Psychiatry. 2002;159(1):30–5. doi: 10.1176/appi.ajp.159.1.30. [DOI] [PubMed] [Google Scholar]
- 10.MacKinnon DF, Zandi PP, Gershon E, Nurnberger JI, Jr, Reich T, DePaulo JR. Rapid switching of mood in families with multiple cases of bipolar disorder. Arch Gen Psychiatry. 2003;60(9):921–8. doi: 10.1001/archpsyc.60.9.921. [DOI] [PubMed] [Google Scholar]
- 11.Nwulia EA, Zandi PP, McInnis MG, DePaulo JR, Jr, MacKinnon DF. Rapid switching of mood in families with familial bipolar disorder. Bipolar Disord. 2008;10(5):597–606. doi: 10.1111/j.1399-5618.2008.00600.x. [DOI] [PubMed] [Google Scholar]
- 12.Simon NM, Otto MW, Wisniewski SR, Fossey M, Sagduyu K, Frank E, Sachs GS, Nierenberg AA, Thase ME, Pollack MH. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) Am J Psychiatry. 2004;161(12):2222–9. doi: 10.1176/appi.ajp.161.12.2222. [DOI] [PubMed] [Google Scholar]
- 13.Feske U, Frank E, Mallinger AG, Houck PR, Fagiolini A, Shear MK, Grochocinski VJ, Kupfer DJ. Anxiety as a correlate of response to the acute treatment of bipolar I disorder. Am J Psychiatry. 2000;157(6):956–62. doi: 10.1176/appi.ajp.157.6.956. [DOI] [PubMed] [Google Scholar]
- 14.Frank E, Cyranowski JM, Rucci P, Shear MK, Fagiolini A, Thase ME, Cassano GB, Grochocinski VJ, Kostelnik B, Kupfer DJ. Clinical significance of lifetime panic spectrum symptoms in the treatment of patients with bipolar I disorder. Arch Gen Psychiatry. 2002;59(10):905–11. doi: 10.1001/archpsyc.59.10.905. [DOI] [PubMed] [Google Scholar]
- 15.Otto MW, Simon NM, Wisniewski SR, Miklowitz DJ, Kogan JN, Reilly-Harrington NA, Frank E, Nierenberg AA, Marangell LB, Sagduyu K, Weiss RD, Miyahara S, Thas ME, Sachs GS, Pollack MH. Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry. 2006;189:20–5. doi: 10.1192/bjp.bp.104.007773. [DOI] [PubMed] [Google Scholar]
- 16.Spitzer RL, Endicott J, Robins E. Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry. 1978;35(6):773–82. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- 17.Endicott J, Spitzer RL. A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry. 1978;35(7):837–44. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- 18.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540–8. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 19.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, Leon AC, Rice JA, Keller MB. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59(6):530–7. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 20.Judd LL, Schettler PJ, Akiskal HS, Maser J, Coryell W, Solomon D, Endicott J, Keller M. Long-term symptomatic status of bipolar I vs. bipolar II disorders. Int J Neuropsychopharmacol. 2003;6(2):127–37. doi: 10.1017/S1461145703003341. [DOI] [PubMed] [Google Scholar]
- 21.Angst J, Gamma A, Pezawas L, Ajdacic-Gross V, Eich D, Rossler W, Altamura C. Parsing the clinical phenotype of depression: the need to integrate brief depressive episodes. Acta Psychiatr Scand. 2007;115(3):221–8. doi: 10.1111/j.1600-0447.2006.00893.x. [DOI] [PubMed] [Google Scholar]
- 22.Angst J, Gerber-Werder R, Zuberbuhler HU, Gamma A. Is bipolar I disorder heterogeneous? Eur Arch Psychiatry Clin Neurosci. 2004;254(2):82–91. doi: 10.1007/s00406-004-0501-6. [DOI] [PubMed] [Google Scholar]
- 23.Keller MB. The course of manic-depressive illness. J Clin Psychiatry. 1988;49 (Suppl):4–7. [PubMed] [Google Scholar]
- 24.Keller MB, Lavori PW, Coryell W, Andreasen NC, Endicott J, Clayton PJ, Klerman GL, Hirschfeld RM. Differential outcome of pure manic, mixed/cycling, and pure depressive episodes in patients with bipolar illness. JAMA. 1986;255(22):3138–42. [PubMed] [Google Scholar]
- 25.Keller MB, Lavori PW, Klerman GL, Andreasen NC, Endicott J, Coryell W, Fawcett J, Rice JP, Hirschfeld RM. Low levels and lack of predictors of somatotherapy and psychotherapy received by depressed patients. Arch Gen Psychiatry. 1986;43(5):458–66. doi: 10.1001/archpsyc.1986.01800050064007. [DOI] [PubMed] [Google Scholar]
- 26.Dawson R, Lavori PW, Coryell WH, Endicott J, Keller MB. Course of treatment received by depressed patients. J Psychiatr Res. 1999;33(3):233–42. doi: 10.1016/s0022-3956(98)00055-7. [DOI] [PubMed] [Google Scholar]
- 27.Leon AC, Solomon DA, Mueller TI, Endicott J, Rice JP, Maser JD, Coryell W, Keller MB. A 20-year longitudinal observational study of somatic antidepressant treatment effectiveness. Am J Psychiatry. 2003;160(4):727–33. doi: 10.1176/appi.ajp.160.4.727. [DOI] [PubMed] [Google Scholar]
- 28.Dawson R, Lavori PW, Coryell WH, Endicott J, Keller MB. Maintenance strategies for unipolar depression. an observational study of levels of treatment and recurrence. J Affect Disord. 1998;49(1):31–44. doi: 10.1016/s0165-0327(97)00181-x. [DOI] [PubMed] [Google Scholar]
- 29.Doughty CJ, Wells JE, Joyce PR, Olds RJ, Walsh AE. Bipolar-panic disorder comorbidity within bipolar disorder families: a study of siblings. Bipolar Disord. 2004;6(3):245–52. doi: 10.1111/j.1399-5618.2004.00120.x. [DOI] [PubMed] [Google Scholar]


