Abstract
Optical coherence tomography (OCT) is an imaging technology with the potential to provide high-resolution images of the skin non-invasively. With this device, it is possible to identify a host of skin structures including tumors. In this case report, we demonstrate the use of an OCT device in delineating a lateral tumor margin of an ill-defined basal cell carcinoma prior to Mohs micrographic surgery. Following surgery, the OCT images are compared to histologic sections to confirm their accuracy. OCT technology has the potential to be a vital tool for dermatologists and particularly Mohs surgeons in identifying tumor margins and potentially reducing the number of invasive procedures needed.
Key words: Optical coherence tomography, Mohs surgery, High-resolution imaging technology, Basal cell carcinoma
Background
Optical coherence tomography (OCT) is a non-invasive high-resolution imaging technology that has wide applications in medicine. The technology is analogous to ultrasound but does not require direct contact with the target source. It quickly provides lateral resolution of >7.5 µm with a depth of resolution extending to several millimeters depending on the tissue type.
OCT has a long established role in retinal imaging and ophthalmology [1]. The technology has also found uses in pulmonary medicine, cardiology, gastroenterology, neurology, and surgery, with emerging applications in many other fields [2, 3, 4, 5, 6].
In the late 1990s, OCT was introduced to dermatology. The high resolution of images allows excellent visualization of individual structures within the skin including the epidermis, the dermoepidermal junction, hair follicles, and superficial vessels. OCT has been studied in a variety of dermatologic conditions including inflammatory dermatoses, infections, bullous skin disease, vascular malformations, and malignancies [7].
OCT has a definite role in Mohs micrographic surgery where the delineation of tumor margins is paramount. The gold standard for determining tumor margins remains histology of frozen sections. However, if a surgeon can realize margins non-invasively prior to surgical extirpation, fewer invasive maneuvers would be required, improving the overall quality of care. By decreasing operating times, wound infection rates would presumably decrease and the cost to healthcare could be improved. Pomerantz et al. [8] reported a case of OCT's role in Mohs surgery. In their report, they showed an excellent correlation between a postoperative Mohs defect with OCT imaging. However, their tumor appeared relatively well-defined prior to surgery with margins that most would expect by visual inspection alone.
In this case report, we sought to assess the accuracy of a multi-beam OCT system in determining the lateral margins of an ill-defined tumor as compared to the gold standard of histology.
Case Report
A 72-year-old Caucasian male with a history of multiple non-melanoma skin cancers presented with an ill-defined pink plaque of the left helical rim, which had bled intermittently over the past couple of years. A biopsy report showed a basal cell carcinoma (BCC) with superficial and nodular components.
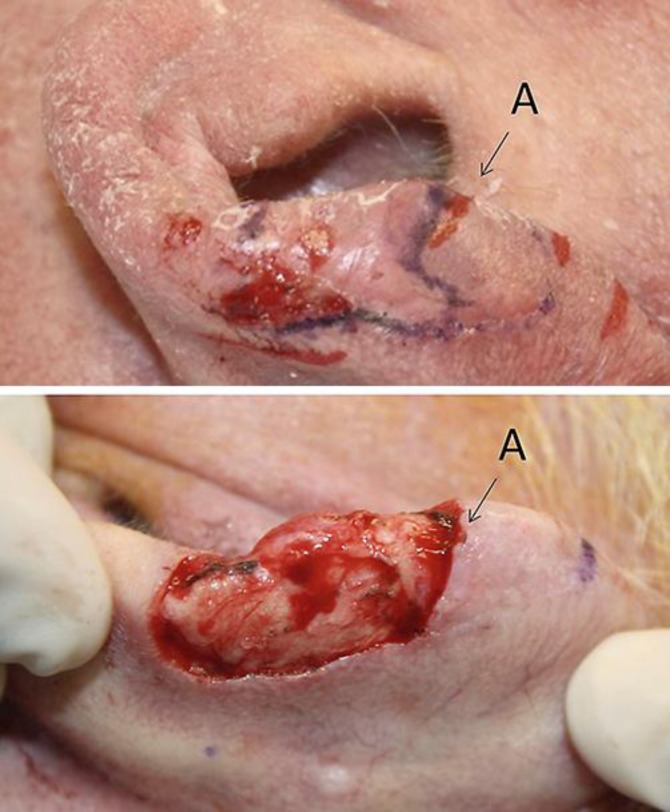
During the preoperative evaluation, the tumor was marked out with a purple marking pen, which is standard for all of our Mohs cases. Fig. 1 shows the appearance of the tumor prior to Mohs surgery. Following this, we used a commercially available FDA 510(k)-cleared OCT system (VivoSight; Michelson Diagnostics, Orpington, UK) to scan the tumor margins. For this case, we only scanned one margin (12 o'clock) with the OCT system, as this area had particularly unclear margins. The OCT device takes a series of 50 images every 0.1 mm and thus can scan 5 mm rapidly at once.
Fig. 1.
Tumor prior to Mohs micrographic surgery. The solid purple marking pen shows apparent tumor margins, as determined during the preoperative evaluation. Tthe dotted marking pen denotes a questionable secondary tumor margin.
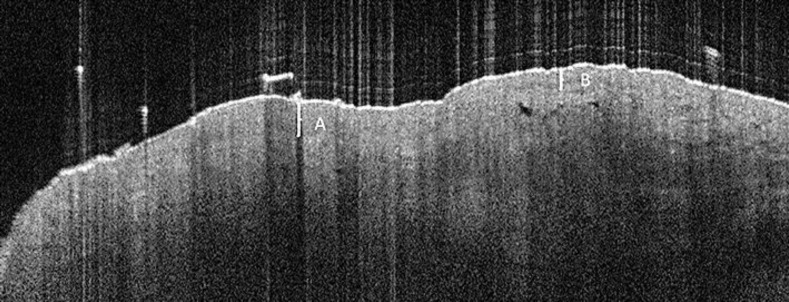
Fig. 2 shows the margins as determined by the OCT device. The red mark with the letter A shows the extent of the tumor. The imaging frame number was correlated with the placement of the hand piece to identify this border precisely. The red mark at B shows the extent of the scan, and no tumor was seen between marks B and A. Fig. 3 shows the first image at the 12 o'clock margin which revealed the tumor. When reviewing a complete set of OCT images, BCCs can be easily discerned from normal, uninvolved tissue. While there is a learning curve with the images, superficial BCCs appear as blurring of the dermoepidermal junction with apparent thickening of the epidermis. Nodular components within the dermis typically appear as hypodensities.
Fig. 2.
Margins as indicated by the OCT device. ‘A’ shows the extent of the tumor. ‘B’ indicates how far the scan was performed. There was no tumor seen between points ‘B’ and ‘A.’
Fig. 3.
OCT imaging shows the first slice where the BCC was appreciated. The BCC can be seen at area ‘A’ with thickening of the epidermis and blurring of the dermoepidermal junction. Area ‘B’ represents typical, uninvolved skin. This transition is more obvious when reviewing a complete OCT scan.
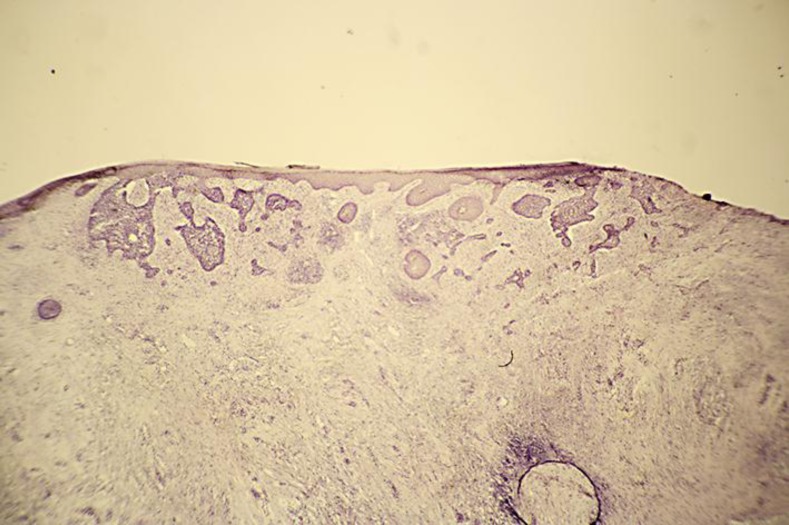
The Mohs procedure was performed as usual with no bias given to the OCT marked borders. Fig. 4 shows the representative BCC seen after the first Mohs stage, indicating tumor extension beyond what was appreciated visually during the preoperative evaluation. The tumor was cleared after three Mohs micrographic stages.
Fig. 4.
Histology from frozen section after the first stage showing extension of the BCC beyond the visually marked out margins.
Fig. 5 shows a comparison of the tumor margin mapped out by OCT preoperatively and the post-operative defect following Mohs surgery. There is excellent correlation with tumor extension between the two modalities.
Fig. 5.
Comparison of preoperative OCT tumor margins and the following clearance of tumor by Mohs micrographic surgery. ‘A’ indicates the tumor as shown by OCT.
Discussion
High-resolution imaging with a multi-beam OCT device can accurately predict tumor margins of a BCC prior to Mohs micrographic surgery. This case was particularly interesting as the margin that was mapped represented a very ill-defined area where tumor extended into almost normal appearing skin. The OCT device was able to effectively depict the tumor extension. While this report evaluated only one margin of one tumor, the potential applications of the technology are obvious. With any tumor, particularly ill-defined ones, the use of OCT could potentially reduce the number of stages required to clear the tumor leading to shorter operative times and reduction of cost.
Further studies supporting the accuracy and utility of OCT in identifying tumor margins are needed to validate its more widespread application. Currently, despite the excellent resolution of the images, significant subjectivity exists in their interpretation. Hopefully in the near future, OCT will be an important adjunct to aid our current methods of Mohs micrographic surgery.
References
- 1.Tadrous PJ. Methods for imaging the structure and function of living tissues and cells: 1. Optical coherence tomography. J Pathol. 2000;191:115–119. doi: 10.1002/(SICI)1096-9896(200006)191:2<115::AID-PATH589>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 2.Hou R, Le T, Murgu SD, Chen Z, Brenner M. Recent advances in optical coherence tomography for the diagnoses of lung disorders. Expert Rev Respir Med. 2011;5:711–724. doi: 10.1586/ers.11.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cahill RA, Mortensen NJ. Intraoperative augmented reality for laparoscopic colorectal surgery by intraoperative near-infrared fluorescence imaging and optical coherence tomography. Minerva Chir. 2010;65:451–462. [PubMed] [Google Scholar]
- 4.Chu CR, Izzo NJ, Irrgang JJ, Ferretti M, Studer RK. Clinical diagnosis of potentially treatable early articular cartilage degeneration using optical coherence tomography. J Biomed Opt. 2007;12:051703. doi: 10.1117/1.2789674. [DOI] [PubMed] [Google Scholar]
- 5.Lamirel C, Newman N, Biousse V. The use of optical coherence tomography in neurology. Rev Neurol Dis. 2009;6:E105–E120. [PubMed] [Google Scholar]
- 6.Gambichler T, Jaedicke V, Terras S. Optical coherence tomography in dermatology: technical and clinical aspects. Arch Dermatol Res. 2011;303:457–473. doi: 10.1007/s00403-011-1152-x. [DOI] [PubMed] [Google Scholar]
- 7.Mogensen M, Thrane L, Joergensen TM, Andersen PE, Jemec GB. Optical coherence tomography for imaging of skin and skin diseases. Semin Cutan Med Surg. 2009;28:196–202. doi: 10.1016/j.sder.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Pomerantz R, Zell D, McKenzie G, Siegel DM. Optical coherence tomography used as a modality to delineate basal cell carcinoma prior to Mohs micrographic surgery. Case Rep Dermatol. 2011;3:212–218. doi: 10.1159/000333000. [DOI] [PMC free article] [PubMed] [Google Scholar]