Abstract
Calcium artery calcium (CAC) scoring has become an integral part in the era of preventive cardiology, it has been extensively studied and been validated as a powerful tool for cardiovascular risk assessment in conjunction with other traditional well established scoring systems such as Framingham risk score. In addition, CAC testing has found its way into emergency department algorithms assessing low to intermediate risk patients presenting with chest pain, this strategy was recently adopted by the UK NICE guidelines, confidently ruling out cardiac origin of chest pain. Several studies have demonstrated that risk assessment using CAC was motivational to patients leading to better adherence to their preventive practices as well as to medications. Accordingly, this test has several recommendations for use by national and international guidelines.
Keywords: Coronary artery calcium, Coronary artery disease, Calcium score, Cardiovascular risk
Introduction
Coronary artery disease (CAD) remains the main cause of mortality in the US, and it is associated with a substantial functional impairment in survivors of acute cardiac events, imposing a very large economic burden. Many risk scoring tools have been used to help identify high risk patients who are most likely to benefit from therapeutic intervention. Unfortunately, most of these tools are not completely accurate. Coronary artery calcium (CAC) is a constituent of atherosclerosis detected almost exclusively in atherosclerotic arteries [1]. CAC pathophysiology and association with cardiovascular risk have been an area of intense investigation for several years. CAC detection has become an established method for cardiovascular risk assessment, and is particularly useful in asymptomatic intermediate risk individuals [2••]. The focus of this review is to present the most relevant literature on the use of CAC as a risk stratification tool of asymptomatic and symptomatic patients, different clinical applications as well as the utility of sequential CAC scanning to follow the evolution of coronary atherosclerosis.
Calcium Score Technical Aspects and Scoring Methods
Electron beam computed tomography (EBCT) and more recently, multidetector computed tomography (MDCT) have been used in quantification of CAC. Compared to EBCT, recent MDCT scanners have the advantage of higher spatial resolution and less noise, while EBCT has less motion artifacts and lower radiation. CAC is typically scanned in a prospectively ECG-triggered mode with 2.5–3.0 mm thick axial slices. The radiation dose is low, with a typical effective dose of approximately 1.0 mSv, which is about the same dose of radiation of 1.5 screening mammograms performed.
Agatston score is one of the most common methods used for CAC scoring that is calculated by multiplying the lesion area (mm2) by a density factor (between 1 and 4) [3] (Fig. 1). However, the increase in Agatston score over time might just represent an increase in plaque attenuation (density) rather than size over time. On the other hand, calcium volume score (CVS) represents an actual volume of CAC and reduces variability between scans [4]. The evaluation of coronary calcium has been proven to be feasible and the presence of calcification in addition to indicating the site of a plaque suggests its extension [5]. Of course only a small percentage of patients with coronary calcifications also have a coronary stenosis. According to the Mayo Clinic guidelines, the probability of the presence of a hemodynamically significant stenosis greater in patients with a calcium score (CS) >400 (Table 1) [6].
Fig. 1.
CAC scans showing progressively increasing Agatston score (from left to right)
Table 1.
Standardized categories for the CAC score
| Agatston score |
Calcium score categories |
Probability of significant CAD |
Cardiovascular risk |
Recommendations |
|---|---|---|---|---|
| 0 | Absent | Very unlikely (<5 %) | Very low | Reassure patient. General guidelines for primary prevention of CV diseases |
| 1–10 | Minimal | Very unlikely (<10 %) | Low | General guidelines for primary prevention of CV diseases |
| 11–100 | Mild | Mild or minimal coronary stenosis likely | Moderate | Counsel about risk factors modification, strict adherence with primary prevention goals. Daily ASA |
| 101–400 | Moderate | Non obstructive CAD, highly likely, obstructive CAD possible | Moderately high | Institute risk factor modification and secondary prevention goals. Consider exercise testing |
| >400 | Extensive | High likelihood of significant coronary stenosis (>90 %) | High | Institute very aggressive risk factor modification. Consider exercise or pharmacological nuclear stress testing for the detection o inducible ischemia |
CV cardiovascular; ASA acetylsalicylic acid
(Adapted from: Cademartiri F, Casolo G, Midiri M, eds: Calcium score and coronary plaque, In Clinical Applications of Cardiac CT. New York: Springer; 2012:121) [41]
Clinical Role and Applications of CAC
Cardiovascular Risk Assessment and Relation to Framingham Risk Score (FRS)
Cardiovascular disease (CVD) risk screening is performed by multiple methods relying on calculators derived from the Framingham study, other epidemiological studies or primary care records. However, it only identifies 70 % of individuals at risk for CVD events and there has been interest in adding other risk factors to improve its predictive capacity.
CAC score has been extensively validated as a marker for cardiovascular risk and currently regarded as a feasible surrogate marker for screening of coronary artery disease [7•]. In the 2010 ACCF/AHA practice guidelines, measurement of CAC was a Class IIa recommendation for assessment of cardiovascular risk in asymptomatic adults at intermediate risk (10–20 % 10-year) as well IIa in persons with diabetes, and a IIb recommendation for those persons at low-intermediate risk (6–10 % 10-year risk). Similarly, in the 2010 appropriateness criteria, CAC scoring was considered as appropriate for intermediate CHD risk patients, and for the specific subset of low-risk patients in whom a family history of premature CHD was present. However, in patients with low cardiovascular risk (< 6 %), CAC Score was judged as inappropriate for cardiovascular risk assessment [8••].
CAC score was studied in association with the traditional well established FRS system showing that the CAC score has been shown as an independent incremental value in prediction of CAD deaths or MIs in asymptomatic patients; Pooled analysis from six studies of 27,622 asymptomatic patients showed that about 43 % of subjects had CAC Score of 0, resulting in a low 3–5 year event rate of only 0.4 %. Subjects with positive CAC were further classified according to their scores into four groups; 1–99, 100–399, 400–999 and ≥1000 showing an incremental relationship where higher CAC scores were significantly associated with higher relative risk ratios and even rates; 1.9, 4.3, 7.2 and 10.8 respectively [9]. Moreover, CAC score helped reclassification of CAD risk categories, studies have shown that 60 % of coronary atherosclerotic events occur in patients in low or intermediate-Framingham risk categories [10]. Intermediate-risk patients with CACS >300 had a 2.8 % annual rate of cardiac death or MI (roughly equivalent to a 10- year rate of 28 %) that would put them in a high risk category [11]. In the Rotterdam study [12], cut-off values of 615 and 50 were suggested to reclassify elderly intermediate risk group population to either high or low risk groups respectively, and 52 % of intermediate risk patients were reclassified. A recent advanced analysis based on the Rotterdam study evaluated the change in the c-statistic and the overall net reclassification index (NRI) for multiple new risk markers. The maximum change in the c-statistic was observed for CAC score (increase, 0.05 [CI, 0.02 – 0.06]), followed by NT-proBNP level (increase, 0.02 [CI, 0.01 – 0.04]). The highest overall net percentage of persons correctly reclassified was also observed for CAC score (NRI, 19.3 % [CI, 12.5 – 26.2 %]), with a smaller NRI for NT-proBNP (7.6 % [CI, 2.8 – 12.5 %]). High sensitivity C reactive protein did not lead to net reclassification or improve the C statistic. Improvements in prediction with other markers were marginal [13].
CAC and Diagnostic Accuracy of Coronary CT Angiography (CCTA)
Severe calcification can limit lumen assessment due to blooming artifacts and yield false positive results decreasing the specificity of CCTA . In clinical practice, the decision whether or not to perform CCTA, if dependent on CAC score, is usually based on the total score and not on the distribution of calcified lesions [14]. For this reason, some study groups have limited CCTA to patients with CAC score below an arbitrary cut-off, with invasive coronary angiography being used for diagnostic purposes in those with higher score. To answer the question of whether a CAC score cut-off is needed to obtain good diagnostic accuracy in CCTA, a recent systematic review and meta-analysis of 27 studies (5203 participants) was conducted to assess the sensitivity and specificity of CCTA by MDCT for significant stenosis (≥50 %) at different degrees of coronary calcification. On a patient-basis, sensitivity of CCTA for significant stenosis was 95.8, 95.6, 97.6 and 99.0 % for CAC scores 0–100, 101–400, 401–1000 and >1000 respectively, while specificity was 91.2, 88.2, 80.6 and 84.0 % respectively. This study concluded that even in cases of severe coronary calcification, sensitivity and specificity of CCTA for significant stenosis are high and that the diagnostic accuracy of 64-MDCT and newer CT systems were significantly higher compared to the 16-slice MDCT indicating that a CAC score cutoff for performing CCTAs no longer seems necessary [15]. Even though, there are issues to keep in mind; if the CAC score is based on considerable calcification limited to a small area, there is a greater probability of artifacts and false positive results of CCTA, compared to a more even distribution of coronary calcification. Considering this, CCTA can be non-diagnostic for a certain coronary segment in case of a CS of 100, while CCTA in a patient with a CS of 1500 can have good diagnostic quality [16, 17].
Role of CAC Scoring in Evaluation of Patients with Chest Pain
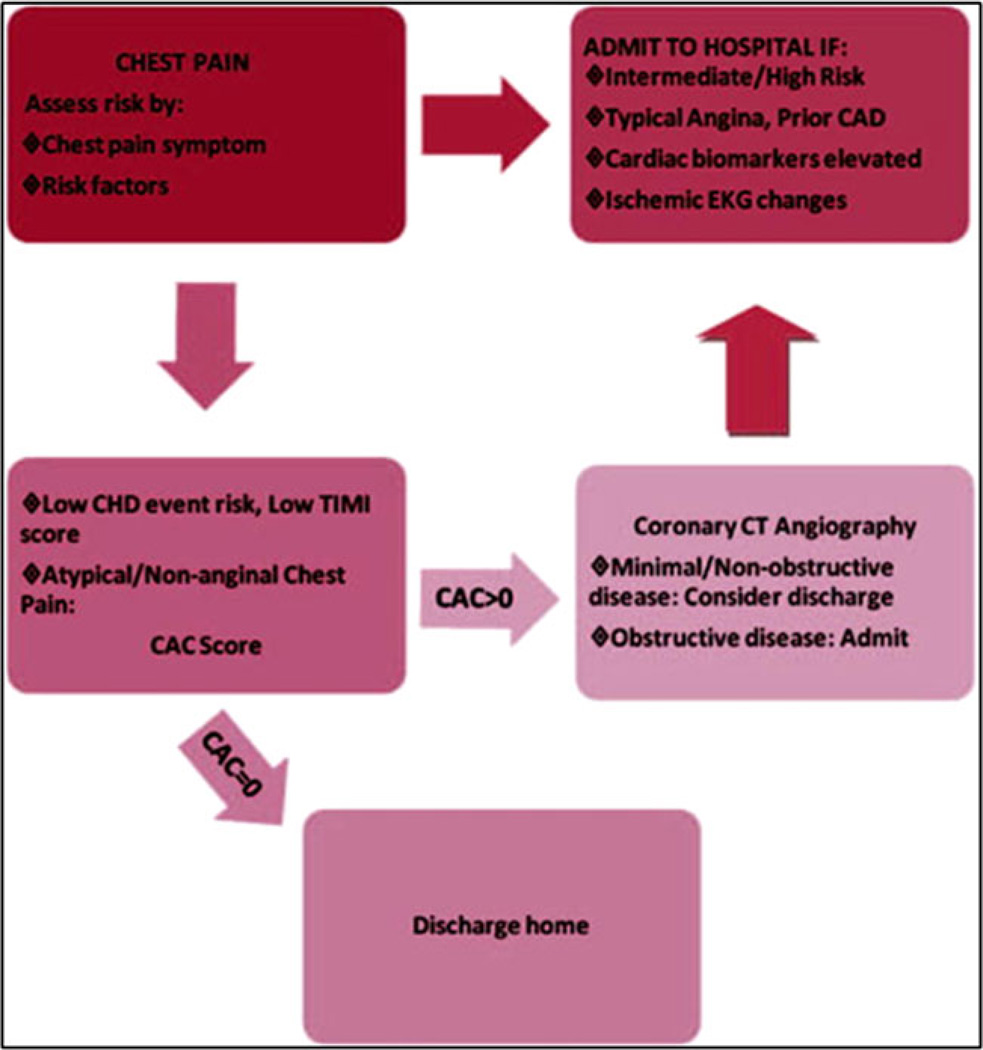
Various studies have shown that CAC score can be regarded as the gate keeper to CTA in diagnosis of significant CAD in patients presenting with chest pain. In those studies, zero calcium score was used as a negative test to identify cases with no obstructive disease with very high sensitivity (>95 %) and negative predictive value (99 %) highlighting its ability to rule out obstructive CAD. This has been reflected in the current recommendations where the 2010 appropriateness criteria considered CTA as appropriate indication in symptomatic patients with CAC score ≤400. In addition, the UK-based National Institute for Health and Clinical Excellence (NICE) guidelines for the management of patients with acute chest pain have recently endorsed CAC scoring as a first line test for symptomatic patients with a low pretest probability of obstructive CAD (10–29 %) [18]. CAC was used to confidently rule out cardiac pain in those with zero calcium score indicating no need for further imaging and to refer those with higher scores to invasive or non invasive coronary angiogram for further assessment of stenosis severity [18]. Similarly, in a recent meta-analysis paper, the authors proposed a hypothetical chest pain algorithm where initially patients are stratified by pretest likelihood of obstructive CAD based on risk factors for CHD events and the nature of chest pain. Once low-risk features are confirmed, CAC scoring can then be performed with further testing by CCTA with positive CAC (Fig. 2).
Fig. 2.
Proposed chest pain algorithm
There has been an ongoing heated debate with respect to the clinical implication of a zero CAC score in patients with chest pain syndrome. Nabi et al. studied 1031 patients in the ED with CAC and nuclear testing. Only two events occurred in 625 patients with a CACS of 0 (0.3 %). Both of these patients developed increased troponin levels during their index visit but had normal serial ECG and SPECT study results and no cardiac events at 6-month follow-up. A majority of patients (61 %) evaluated for chest pain of uncertain cardiac cause have a CACS of 0, which predicts both a normal SPECT result and an excellent short-term outcome. These results suggest that patients with a CACS of 0 can be discharged home, without further cardiac testing, strongly supporting the recent UK NICE guidelines [19]. Recently, Kim et al. has published a study of 1114 patients who presented with chest pain and zero calcium score with mean follow-up period of 2.8 years, early revascularization was done in 25 patients (2.2 %) and there were 14 major adverse cardiac events (1.3 %) [20]. Since there might be a theoretical concern that patients with zero CAC score may use that to justify an unhealthy lifestyle. There are two important messages that health care providers can give patients with a zero CAC score. First, the result is reassuring that an individual’s risk of a CHD event over the next 10 years is very low, <1 % [21]. Secondly, patients should also understand that the absence of CAC does not guarantee the absence of atherosclerosis because they may have exclusively non calcified plaque that is not identified by CAC testing. As a result, patients should still be encouraged to make appropriate therapeutic lifestyle changes to decrease their long-term risk.
Cost Effectiveness of CAC Scoring Approach in the ED
Three studies have exclusively explored the cost-effectiveness of integrating CAC scoring into an emergency room decision-making algorithm for patients with acute chest pain. Raggi et al. [22] allotted patients to either an “exercise treadmill test first” approach or to CAC scanning as the initial test of choice, followed by exercise stress testing for CAC >150. The economic analysis of these two approaches revealed a cost reduction of over 65 % when comparing the “CAC first” approach to that of exercise treadmill testing first ($599 vs. $1701, average savings $1102±123 [95 % CI $860–$1344]).
A more recent economic appraisal of chest pain algorithms compared CAC scanning and exercise stress electrocardiography at the Brighton and Sussex University Hospitals in the United Kingdom [23•]. In this study, performing a CAC scan first was more cost-effective than treadmill stress testing in patients with a pretest probability <30 % using the NICE guidelines. In addition, for patients with a pretest probability >30 %, proceeding directly to myocardial perfusion scintigraphy or invasive angiography was more cost-effective than either CAC scanning or exercise stress testing, suggesting that CAC scanning was more economically feasible in lower-risk patients. Branch et al. hypothesized that a CAC-based evaluation of ED patients at low to intermediate risk of ACS will be less expensive than the current standard of care involving stress testing, even when downstream costs of the CAC are considered. The authors studied 102 patients deemed to be low to intermediate risk on the basis of a mean TIMI risk score of 0.9, with a mean follow-up of 12 months. Mean patient costs for a CAC-based evaluation were significantly lower ($750, 24 %) than the standard of care testing ($2384 and $3134, respectively) [24].
Role of Zero Calcium Score in Asymptomatic Patients
In a recent meta-analysis involving more than 29,000 asymptomatic patients with a zero CAC score, with a mean follow-up period of 50 months, the annual event rate was only 0.12 % [25]. A zero CAC score was more predictive than a negative intima media thickness test or negative stress test of decreased cardiovascular events [26, 27]. Furthermore, diabetic patients who had a zero CAC score had a similar cardiovascular risk to those without diabetes [28].
CAC score retesting in asymptomatic subjects are subjects of debate. Obviously, if the patient becomes symptomatic, re-evaluation would be considered regardless of a previous zero calcium score. However, in those who remain symptom free, evidence suggests that the CAC score should not be repeated frequently [29]. In a recent study by Min et al. [30•], the cumulative rate of “conversion” from a zero CAC score to ≥1 CAC score was 15 % in the first 4 years and 25 % in the fifth year concluding that 4 years might be the ideal “warranty period” for a zero CAC score which is considerably longer that the warranty period that is offered by normal functional imaging tests (such as nuclear perfusion scans) which is considered to be around 1.5 to 2 years [31]. Budoff et al. studied 4609 consecutive asymptomatic individuals who underwent serial scanning and found that CAC progression added incremental value in predicting all-cause mortality over baseline score, time between scans, demographics, and cardiovascular risk factors. They concluded serial assessment may have clinical value in assessing plaque progression and future cardiovascular risk.
Role of Calcium Score in Women
CAC scoring was shown to be a good risk stratification tool for asymptomatic women over and above other traditional cardiovascular risk factors. The MESA study screened 2600 asymptomatic women with a median Agatston score of 0 (range, 0–26), CHD only occurred in 2 % of the studied population [32]. The area under the curve (AUC) for CHD increased significantly from 0.805 to 0.835 with the addition of CAC scanning. Similarly, in a study by Raggi et al., the ROC C-index for death estimation was 0.672 (95 % CI 5 0.622–0.722, p<0.0001) which significantly improved when calcification was added to this analysis from 0.672 to 0.75 (p<0.0001) [28].
Role of CAC Score in Promoting Patients Adherence to Treatment
CAC represents objective evidence of atherosclerosis and the way CAC results are conveyed is likely to serve as a powerful source of motivation for patients to adopt a healthier lifestyle and to adhere to both pharmacological and non pharmacological treatments, such as dietary changes and exercise. Kalia and colleagues studied 505 individuals treated with statins. Study investigators showed each participant sample images from their CT and described the degree of atherosclerosis as none, mild, moderate, or severe. After 3 years of follow-up, 44 % of individuals with a CAC score of 0 reported taking a statin, compared with 75% with a CAC score of 100–399 and 90 % with a CAC score of ≥400 [33].
In the Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research (EISNER) study, adults who underwent CAC testing met individually with a nurse to see sample images and receive counseling on risk factor modification. After 4 years of follow-up, adults with any CAC score achieved significantly greater reductions in systolic blood pressure (SBP) and low-density lipoprotein (LDL) cholesterol than adults with a CAC score of 0 [34••]. In a third study, Schwartz and colleagues evaluated the association of CAC testing with health behavior modification. After a mean of 6 years, those with a CAC score greater than 0 were more likely to increase their exercise (19 % vs 12 %, P<.01) and change their diet (33 % vs 21 %, P<.01) [35]. Although the association of CAC with medication adherence and behavior change is significant, further large randomized studies are warranted.
Another potentially useful tool is the arterial age calculator, found on the MESA Web http://www.mesa-nhlbi.org/Calcium/ArterialAge.aspx. Patients or providers can enter the CAC score to calculate an arterial age, which is the age at which the estimated CHD risk is the same as that for the observed CAC score. Arterial age can then be used to revise the estimated 10-year CHD risk. The missing piece of the puzzle in regards to scanning and compliance is whether undergoing a CAC scan results in better outcomes, which relies on the downstream treatment to make a change, not solely based on the performance of the scan itself.
Assessment of Coronary Artery Calcium Progression
A decade ago researchers started to investigate whether serial changes in CAC score were helpful in monitoring response to medical therapy. An important consideration as one sets up a sequential CT scanning program is the radiation dose provided with each cardiac CT that mandates that the benefit/risk ratio of repeat scanning be carefully weighed.
Progression of CAC is generally calculated as a percent or absolute change from the baseline score. In subjects at an average FRS, the annual CAC progression typically ranges from 20–25 % [36]. Factors that may significantly modify the rate of change include the patient’s baseline CAC score, gender, age, family history of premature CAD, ethnicity, diabetes and glycemic control, body mass index, hypertension, and renal insufficiency. Most patients will exhibit some increase in CAC scores over time [36] although a baseline score of 0 is usually associated with slow and delayed growth. Therefore, in patients with CAC score of 0 a CT scan should not be repeated prior to 5 years from the initial scan [29].
Some treatments (statins which will be discussed separately) have also been shown to slow CAC progression. In the Women’s Health Initiative (WHI), menopausal women between the ages of 50–59 years were randomized to treatment with conjugated estrogens or placebo [37]. In a sub-study of the WHI, 1064 women underwent CAC screening 8.7 years from trial initiation. Women receiving estrogens showed a lower CAC score compared to those receiving placebo (83.1 versus 123.1, p=0.02). Finally, several reports have noted that a rapid change in CAC score is associated with worse clinical outcomes, including incident MI [28, 38••]. It would appear that patients with baseline CAC scores ≥400 and those exhibiting significant CAC progression from their index scan (≥15%per year) have a shorter lag time to the development of acute MI compared to those with CAC scores ≤100 and a progression<15 % per year and. Thus, the baseline CAC score provides an insight into not only the expected rate of progression but also the timeline of conversion to symptomatic CAD.
Role of CAC Testing in Monitoring Response to Therapy
Clinical trial data suggest that the CAC score is relatively insensitive to statin therapy. In a study by Arad and colleagues, 1005 asymptomatic adults with CAC scores above the 80th percentile for age and sex were randomized to atorvastatin, 20 mg, versus placebo. After 4 years, there was no difference in CAC scores between the two arms, despite a 43 % reduction in LDL among those taking atorvastatin [39]. In a subsequent study, postmenopausal women with hyperlipidemia were randomized to atorvastatin, 80 mg, or pravastatin, 40 mg. Women in both arms experienced an approximately 20 % increase in CAC after 1 year, despite a 47 % reduction in mean LDL with atorvastatin and a 25 % reduction with pravastatin [40]. Therefore, it seems most appropriate to follow patients’ clinical response to therapy rather than repeat the CT scan. Accordingly, several factors might explain this conflicting data; (I) first CAC score might not be the best tool to monitor the treatment response, (II) longer follow up periods are needed or (III) statins might be improving the cardiovascular outcome through other pleiotropic effects rather than just mere lowering of the LDL-cholesterol or decreasing the CAC scores. As discussed earlier, CAC progression robustly predicts events, so further cost effectiveness and algorithms need to be developed for use of serial CAC scans to identify persons whose plaque is progressing despite therapies.
Conclusions and Future Directions
CAC scanning is a mature technology, and CT will become the modality of choice for risk stratification, particularly in intermediate risk patients, with selective application in the lower and higher risk groups. Screening of asymptomatic intermediate-risk patients for refinement of risk stratification and imaging in stable patients with chest discomfort to exclude obstructive CAD may constitute the best current indications. The role of zero calcium score in the management of patients with chest pain together with the treatment strategies on CAC progression rates are still controversial. Further developments will include decreasing radiation, and plaque characterization beyond calcification. CAC scores will not detect non-calcified plaques. CT angiography is better suited for the non-invasive detection of the non-calcified component of coronary atherosclerotic plaques, and will hopefully be instrumental in the classification of plaques along the spectrum of stable to vulnerable. It is important to educate the public and physicians as to the advantages and limitations for the most proper use of this powerful imaging tool.
Abbreviations
- CAC
Coronary artery calcium
- CAD
Coronary artery disease
- CCTA
Coronary CT angiography
- CHD
Coronary heart disease
- CVD
Cardiovascular disease
- CVS
Calcium volume score
- EBCT
Electron beam computed tomography
- ED
Emergency department
- FRS
Framingham risk score
- MDCT
Multidetector CT
Footnotes
This article is part of the Topical Collection on Cardiac PET, CT, and MRI
Disclosure No potential conflicts of interest relevant to this article were reported.
Contributor Information
George Youssef, Email: gyoussef@labiomed.org.
Matthew J. Budoff, Email: mbudoff@labiomed.org.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993;362:801–809. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- 2. Greenland P, Alpert JS, Beller GA, et al. ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122:2748–2764. doi: 10.1161/CIR.0b013e3182051bab. This article represents the most uptodate clinical expert consensus on the use of coronary artery calcium scoring in risk assessment of asymptomatic subjects.
- 3.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 4.Callister TQ, Cooil B, Raya SP, Lippolis NJ, Russo DJ, Raggi P. Coronary artery disease: improved reproducibility of calcium scoring with an electron-beam CT volumetric method. Radiology. 1998;208:807–814. doi: 10.1148/radiology.208.3.9722864. [DOI] [PubMed] [Google Scholar]
- 5.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157–2162. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 6.Rumberger JA, Brundage BH, Rader DJ, Kondos G. Electron beam computed tomographic coronary calcium scanning: a review and guidelines for use in asymptomatic persons. Mayo Clin Proc. 1999;74:243–252. doi: 10.4065/74.3.243. [DOI] [PubMed] [Google Scholar]
- 7. Youssef G, Budoff J. Coronary artery calcium scoring, what is answered and what questions remain. Cardiovasc Diagn Ther. 2012;2:94–105. doi: 10.3978/j.issn.2223-3652.2012.06.04. This review article shows the main controversies and debate regarding the clinical use of coronary artery score.
- 8. Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/ AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–1894. doi: 10.1016/j.jacc.2010.07.005. This is the most recent appropriatness criteria highlighting the most acceptable approach towards the use of coronary artery calcium scanning in clinical practice.
- 9.Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2007;49:378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Lauer MS. Primary prevention of atherosclerotic cardiovascular disease: the high public burden of low individual risk. JAMA. 2007;297:1376–1378. doi: 10.1001/jama.297.12.1376. [DOI] [PubMed] [Google Scholar]
- 11.Nasir K, Budoff MJ, Post WS, et al. Electron beam CT versus helical CT scans for assessing coronary calcification: current utility and future directions. Am Heart J. 2003;146:969–977. doi: 10.1016/S0002-8703(03)00450-2. [DOI] [PubMed] [Google Scholar]
- 12.Elias-Smale SE, Proenca RV, Koller MT, et al. Coronary calcium score improves classification of coronary heart disease risk in the elderly: the Rotterdam study. J Am Coll Cardiol. 2010;56:1407–1414. doi: 10.1016/j.jacc.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 13.Kavousi M, Elias-Smale S, Rutten JH, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med. 2012;156:438–444. doi: 10.7326/0003-4819-156-6-201203200-00006. [DOI] [PubMed] [Google Scholar]
- 14.Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/ AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–1894. doi: 10.1016/j.jacc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 15.den Dekker MA, de Smet K, de Bock GH, Tio RA, Oudkerk M, Vliegenthart R. Diagnostic performance of coronary CT angiography for stenosis detection according to calcium score: systematic review and meta-analysis. Eur Radiol. 22(12):2688–2698. doi: 10.1007/s00330-012-2551-x. [DOI] [PubMed] [Google Scholar]
- 16.Dey D, Lee CJ, Ohba M, et al. Image quality and artifacts in coronary CT angiography with dual-source CT: initial clinical experience. J Cardiovasc Comput Tomogr. 2008;2:105–114. doi: 10.1016/j.jcct.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 17.Sangiorgi G, Rumberger JA, Severson A, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998;31:126–133. doi: 10.1016/s0735-1097(97)00443-9. [DOI] [PubMed] [Google Scholar]
- 18.Smeeth L, Skinner JS, Ashcroft J, Hemingway H, Timmis A. NICE clinical guideline: chest pain of recent onset. Br J Gen Pract. 2010;60:607–610. doi: 10.3399/bjgp10X515124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nabi F, Chang SM, Pratt CM, et al. Coronary artery calcium scoring in the emergency department: identifying which patients with chest pain can be safely discharged home. Ann Emerg Med. 2010;56:220–229. doi: 10.1016/j.annemergmed.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Kim YJ, Hur J, Lee HJ, et al. Meaning of zero coronary calcium score in symptomatic patients referred for coronary computed tomographic angiography. Eur Heart J Cardiovasc Imag. 2012 doi: 10.1093/ehjci/jes060. [DOI] [PubMed] [Google Scholar]
- 21.Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–1870. doi: 10.1016/j.jacc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 22.Raggi P, Callister TQ, Cooil B, Russo DJ, Lippolis NJ, Patterson RE. Evaluation of chest pain in patients with low to intermediate pretest probability of coronary artery disease by electron beam computed tomography. Am J Cardiol. 2000;85:283–288. doi: 10.1016/s0002-9149(99)00733-x. [DOI] [PubMed] [Google Scholar]
- 23. Raman V, McWilliams ET, Holmberg SR, Miles K. Economic analysis of the use of coronary calcium scoring as an alternative to stress ECG in the non-invasive diagnosis of coronary artery disease. Eur Radiol. 2011;22:579–587. doi: 10.1007/s00330-011-2304-2. This study showed the economic benefit of endorsing coronary artery calcium scoring use in clinical practice protocols rather than other non-invasive modalities as an initial test to offer.
- 24.Branch KR, Bresnahan BW, Veenstra DL, et al. Economic outcome of cardiac CT-based evaluation and standard of care for suspected acute coronary syndrome in the emergency department: a decision analytic model. Acad Radiol. 2012;19:265–273. doi: 10.1016/j.acra.2011.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sarwar A, Shaw LJ, Shapiro MD, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imag. 2009;2:675–688. doi: 10.1016/j.jcmg.2008.12.031. [DOI] [PubMed] [Google Scholar]
- 26.Folsom AR, Kronmal RA, Detrano RC, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–1339. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gottlieb I, Sara L, Brinker JA, Lima JA, Rochitte CE. CT coronary calcification: What does a score of "0" mean? Curr Cardiol Rep. 2011;13:49–56. doi: 10.1007/s11886-010-0151-4. [DOI] [PubMed] [Google Scholar]
- 28.Raggi P, Shaw LJ, Berman DS, Callister TQ. Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol. 2004;43:1663–1669. doi: 10.1016/j.jacc.2003.09.068. [DOI] [PubMed] [Google Scholar]
- 29.Gopal A, Nasir K, Liu ST, Flores FR, Chen L, Budoff MJ. Coronary calcium progression rates with a zero initial score by electron beam tomography. Int J Cardiol. 2007;117:227–231. doi: 10.1016/j.ijcard.2006.04.081. [DOI] [PubMed] [Google Scholar]
- 30. Min JK, Lin FY, Gidseg DS, et al. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: what is the "warranty period" for remaining normal? J Am Coll Cardiol. 2010;55:1110–1117. doi: 10.1016/j.jacc.2009.08.088. This study showed prognostic value and warranty period of having zero CAC scores in long term clinical follow-up.
- 31.Hachamovitch R, Hayes S, Friedman JD, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan? J Am Coll Cardiol. 2003;41:1329–1340. doi: 10.1016/s0735-1097(03)00125-6. [DOI] [PubMed] [Google Scholar]
- 32.Lee J. Coronary artery calcium scoring and its impact on the clinical practice in the era of multidetector CT. Int J Cardiovasc Imag. 2011;27(Suppl 1):9–25. doi: 10.1007/s10554-011-9964-5. [DOI] [PubMed] [Google Scholar]
- 33.Kalia NK, Miller LG, Nasir K, Blumenthal RS, Agrawal N, Budoff MJ. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis. 2006;185:394–399. doi: 10.1016/j.atherosclerosis.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 34. Rozanski A, Gransar H, Shaw LJ, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol. 2011;57:1622–1632. doi: 10.1016/j.jacc.2011.01.019. This clinical trial revealed the impact of CAC scanning in motivating patients to comply and achieve better risk factors modification in a 4-year follow up study.
- 35.Schwartz J, Allison M, Wright CM. Health behavior modification after electron beam computed tomography and physician consultation. J Behav Med. 2011;34:148–155. doi: 10.1007/s10865-010-9294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raggi P, Cooil B, Shaw LJ, et al. Progression of coronary calcium on serial electron beam tomographic scanning is greater in patients with future myocardial infarction. Am J Cardiol. 2003;92:827–829. doi: 10.1016/s0002-9149(03)00892-0. [DOI] [PubMed] [Google Scholar]
- 37.Manson JE, Allison MA, Rossouw JE, et al. Estrogen therapy and coronary-artery calcification. N Engl J Med. 2007;356:2591–2602. doi: 10.1056/NEJMoa071513. [DOI] [PubMed] [Google Scholar]
- 38. Budoff MJ, Hokanson JE, Nasir K, et al. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovascular Imag. 2010;3:1229–1236. doi: 10.1016/j.jcmg.2010.08.018. This large size cohort study revealed prognostic value of CAC progression as an independent factor Identifying people with higher risk for all cause mortality.
- 39.Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol. 2005;46:166–172. doi: 10.1016/j.jacc.2005.02.089. [DOI] [PubMed] [Google Scholar]
- 40.Raggi P, Davidson M, Callister TQ, et al. Aggressive versus moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: Beyond Endorsed Lipid Lowering with EBT Scanning (BELLES) Circulation. 2005;112:563–571. doi: 10.1161/CIRCULATIONAHA.104.512681. [DOI] [PubMed] [Google Scholar]
- 41.Cademartiri F, Casolo G, Midiri M, editors. Clinical applications of cardiac CT. New York: Springer; 2012. Calcium score and coronary plaque; p. 121. [Google Scholar]