Abstract
Background:
Sentinel headache (SH) is a kind of secondary headache and is characterized as sudden, intense, and persistent, preceding spontaneous subarachnoid hemorrhage (SAH) by days or weeks.
Methods:
Eighty-nine consecutive patients with a diagnosis of spontaneous SAH were evaluated following admission to the Neurosurgical Service at Santa Casa Hospital, Belo Horizonte, between December 2009 and December 2010.
Results:
Out of the 89 patients, 64 (71.9%) were women. Mean age was 48.9 years (SD ± 13.4, ranging from 18 to 85 years). Twenty-four patients (27.0%) presented SH, which occurred, in average, 10.6 days (SD ± 13.5) before a SAH. No statistically significant differences were observed between the presence of SH and gender, arterial hypertension and migraine (P > 0.05), Glasgow Comma Scale (GCS) and World Federation of Neurological Surgeons (WFNS) scale at admission.
Conclusion:
The prevalence of SH was 27% in this study but no related factors were identified. Therefore, further clarification of this important entity is required so as to facilitate its recognition in emergency services and improve the prognosis of patients with cerebral aneurysms.
Keywords: Intracranial aneurysm, sentinel headache, subarachnoid hemorrhage
INTRODUCTION
Headache is one of the main complaints reported in medical practice, particularly by health professionals responsible for emergency services. Approximately 95% of young women and 91% of young men present at least one episode of headaches in any given 12-month period and only 18% of women and 15% of men seek medical care due to such complaint.[7] Headaches are symptoms commonly overlooked by patients and their relatives. When it appears as a single symptom, the patient can delay seeking medical care.[2,11]
Secondary headache represents a specific group in the international classification of headaches being characterized by the presence of structural alterations in the central nervous system and, therefore, having a broad list of possible causes for the pain and variable clinical status. Given the importance of secondary headaches, there are several risk factors that must be evaluated in order to assist diagnosis.
Sentinel headache (SH) is a kind of secondary headache that is characterized as sudden, intense, and persistent, preceding spontaneous subarachnoid hemorrhage (SAH) by days or weeks. It can occur in 15-60% of patients with spontaneous SAH and its pathophysiology has not been fully elucidated. The current consensus is that structural changes in the aneurysm wall or minor bleeding could be the factors responsible for the pain.[1,2,5,8,10–13]
Given this reality and knowing that the identification of SH is particularly relevant, since it can lead to the identification of an unruptured aneurysm, this study evaluates the prevalence of SH and try to identify factors associated with this clinical entity, besides the possible causes of the difficulty in its diagnoses in emergency care.
MATERIALS AND METHODS
The study was approved by the Research Ethics Committee of Santa Casa Hospital, Belo Horizonte, under protocol no. 054/2009.
Patients
Eighty-nine consecutive patients admitted to the Neurosurgery Service of Santa Casa de Belo Horizonte, between December 2009 and December 2010, with a diagnosis of SAH secondary to cerebral aneurysm, confirmed by computed tomography (CT) scan and cerebral arteriography, were evaluated.
It is important to mention that most of patients admitted at the neurosurgery service of our hospital are referred from other institutions, and so initial patient treatment is not standardized.
All the patients or their families were interviewed, and filled out a standardized questionnaire, which included the Glasgow Coma Scale (GCS), clinical scale of the World Federation of Neurological Surgeons (WFNS), and SH data.
Inclusion criteria were SAH due to ruptured aneurysm, with the possibility of gathering information from the patient or their relatives regarding SH.
A total of 94 patients were evaluated during the study period, but 4 were excluded: 2 patients presented SAH of nonaneurysmal origin and the other 2 patients were unable to provide information related to their clinical symptoms and we did not have contact with their family.
Definition of sentinel headache
SH was characterized as a severe headache with features different from the usual headache; or the worst headache ever reported by the patient previous to the day when the signs and symptoms that led to the diagnosis of spontaneous SAH were established.
Statistical analysis
The statistical analysis was performed using the SPSS software, version 9.0 (Statistical Package for the Social Sciences Base 9.0 for Windows, SPSS Inc. 1998, Chicago, IL, USA). The Mann – Whitney U test was used to calculate rank-ordered variables, the Chi square test was used for categorical variables, and the t tests was used for variables counted on an interval scale. Bivariate correlations were calculated by means of Pearson correlation coefficients.
RESULTS
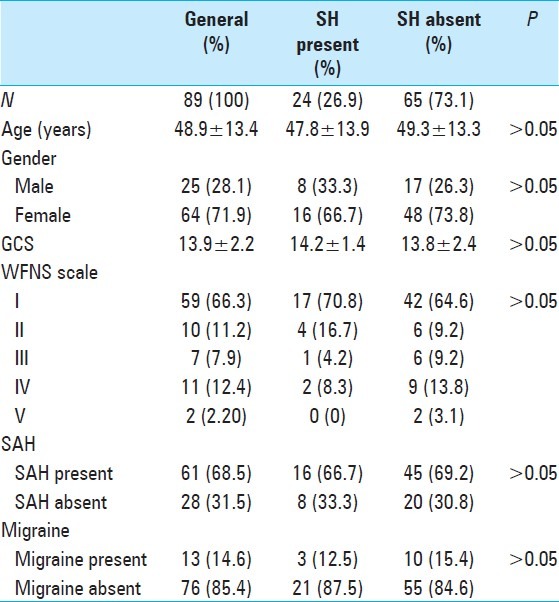
Of the 89 patients, 64 (71.9%) were women and 25 (28.1%) were men. Mean age was 48.9 years (SD ± 13.4, ranging from 18 to 85 years). Twenty-four patients (27.0%) presented SH. Demographic and clinical data are shown in Table 1.
Table 1.
Demographic and clinical data
Of the 24 patients with SH, 9 (37.5%) sought medical care due to SH and 6 of these patients (66.7%) were submitted to CT scan and lumbar puncture, which were normal. None of those patients underwent extended workup involving CT angiography (angio-CT) or magnetic resonance angiography (MR angiography). Interestingly, 62.5% (n = 15) of the patients presenting SH did not seek any medical care; they overlooked their symptoms, seeking help only at the time of the SAH [Figure 1].
Figure 1.
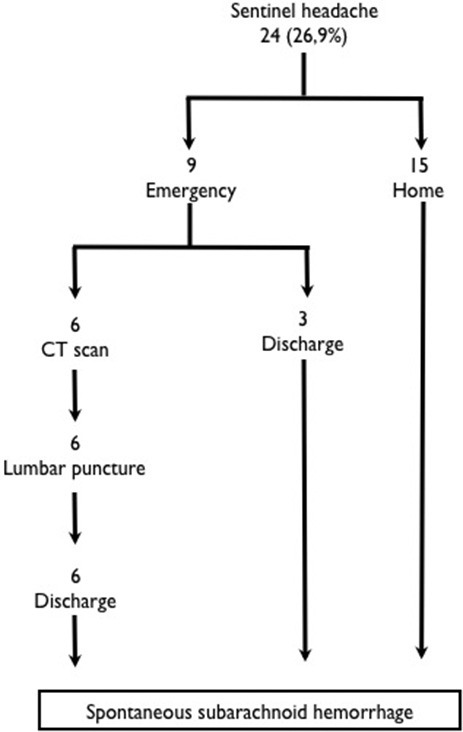
Flowchart of patients presenting sentinel headache
SH was described as a very intense headache in all patients. The pain was pulsatile in 54.2% by the patients, explosive in 41.6%, and heavy in 4.2%. Regarding the pain intensity of the SH compared with the spontaneous pain caused by the SAH, 18.7% of patients reported that the headache pain was greater in the case of SH, 18.7% reported it to be equal, and 62.5% reported it to be less painful than SAH-related headache.
On average, SH occurred 10.6 days (SD ± 13.5) before a SAH. Time delay between the SAH and the admission was in average 7.4 days (SD ± 6.6).
No statistically significant differences were observed between the presence of SH and gender, arterial hypertension and migraine, GCS and WFNS scale at admission (P > 0.05).
DISCUSSION
Headache is a common complaint in emergency services, accounting for approximately 1.2-4.5% of adult patient consultations and, out of them, between 4.3% and 6.4% being secondary headaches.[4,6,7,9,14]
SH is clinically similar to headaches that occur at the time of spontaneous SAH onset, developing rapidly, achieving maximum intensity in minutes and maybe lasting hours or days. However, it presents none of the classic signs of spontaneous SAH, such as altered levels of consciousness, neck stiffness, and focal neurological signs.[2,10,11]
Explosive headache is part of the differential diagnosis of SH and can be primary or secondary to cerebral venous thrombosis, arterial dissection, reversible cerebral vasospasm syndrome, vasculitis, or SAH.[15]
Early identification and surgical treatment of spontaneous SAH are good prognostic factors. In contrast, the high prevalence of headache in emergency service consultations combined with a lack of specialized care leads to under diagnosis of this entity.
One important aspect regarding our study is that only 37.5% of patients who reported SH sought emergency care [Figure 1]. Although most SH patients do not suffer from chronic headaches, an isolated headache seems to be regarded as a symptom of little relevance by the patients and their relatives, even when it presents a different pattern than usual.[3,4,14,15]
In this study, the presence of SH was identified in 27.0% of the patients and, although it was not statistically significant, it was more prevalent and predominant in females.[2,10,11]
Some studies have analyzed the incidence and epidemiological factors associated with SH, reporting a huge difference in its prevalence, varying from 9.5% to 42% of patients with spontaneous SAH.[2,10,11] Such difference could be attributed to different rates of misdiagnosis during emergency care, which varies from region to region, samples from different patients, and different methods of assessing and understanding the SH.
In the present study, the majority of the patients who presented SH (22 out of 24, 91.7%) did so within 30 days before the SAH. SH most commonly occurs within two weeks of spontaneous SAH. SH may be due to minor bleeding, distension or dissection of the aneurysm wall.[2,3,15]
Regarding the presence of primary headache, it is known that this is not a risk factor for cerebral aneurysm rupture. This study showed no increased prevalence of SH in patients with migraine (no statistical significance). Moreover, chronic headaches may have difficulty to diagnose in SH at emergency care.
SH is an important warning sign that remains underestimated when patients are seen at emergency services, but it should always be considered. The presence of SH should be investigated further, including MR angiography, angiotomography, or cerebral arteriography.
In this study, none of the patients were submitted to any cerebral blood vessels evaluation after SH. The diagnosis of cerebral aneurysm only occurred postrupture. There is no established protocol for handling suspected SH, making appropriate management difficult in a patient with a severe and potentially treatable disease. Normal CT scan and lumbar puncture should not be the only tests performed when suspicion of SH arises, rather we believe that this population should be submitted to tests that evaluate cerebral blood vessels, as angio-CT or magnetic resonance angiography (MRA).[3,14,15] In Figure 2, we suggest a flowchart to management of patients suspected to present SH, but it presents limitations related to cost and technology not available in many emergency departments.
Figure 2.
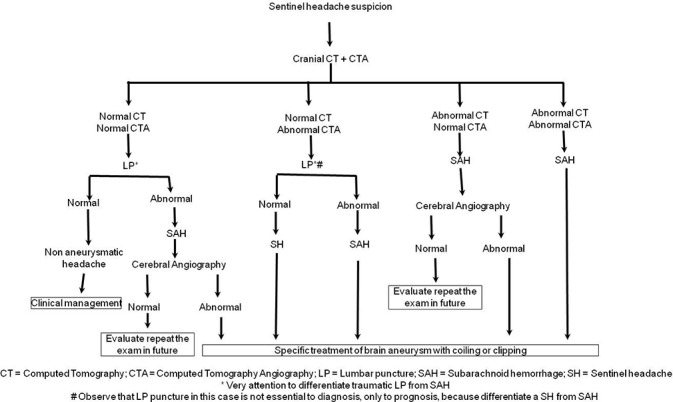
Flowchart to management of patients suspected to present sentinel headache
CONCLUSION
Further clarification of this important entity is required to facilitate its recognition in emergency services and improve the prognosis of patients with cerebral aneurysms. Establishing an appropriate protocol in cases of suspected SH is fundamental.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/162/105101
Contributor Information
Júlio Leonardo Barbosa Pereira, Email: juliommais@yahoo.com.br.
Lucas Alverne Freitas de Albuquerque, Email: lucasalverne@gmail.com.
Marcos Dellaretti, Email: mdellaretti@mac.com.
Gervásio Teles Cardoso de Carvalho, Email: gervasioteles@gmail.com.
Gerival Vieira Junior, Email: gerivaljr@yahoo.com.br.
Marcella Israel Rocha, Email: marcela_israel@yahoo.com.br.
Laize Luzia Andrade Loures, Email: laizeloures@hotmail.com.
Paulo Pereira Christo, Email: ppc@gold.com.br.
Atos Alves de Sousa, Email: sousatos@hotmail.com.
REFERENCES
- 1.Anderson C, Anderson N, Bonita R, Dunbabin D., Hankey G., Jamrozik K., et al. Epidemiology of aneurysmal subarachnoid hemorrhage in Australia and New Zealand: Incidence and case fatality from the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS) Stroke. 2000;31:1843–50. doi: 10.1161/01.str.31.8.1843. [DOI] [PubMed] [Google Scholar]
- 2.Asano AG, Silva WF, Valença MM. Cefaléia sentinela: Sinal de alerta da hemorragia subaracnoide. Migrâeas Cefaléias. 2008;11:78–83. [Google Scholar]
- 3.Edlow JA, Caplan LR. Avoiding pitfalls in the diagnosis of SAH. N Engl J Med. 2000;342:24–31. doi: 10.1056/NEJM200001063420106. [DOI] [PubMed] [Google Scholar]
- 4.Fridriksson S, Hillman J, Landtblom AM, Boive J. Education of referring doctors about sudden onset headache in subarachnoid hemorrhage: A prospective study. Acta Neurol Scand. 2001;103:238–42. [PubMed] [Google Scholar]
- 5.Inagawa T. What are the actual incidence and mortality rates of subarachnoid hemorrhage? Surg Neurol. 1997;47:47–52. doi: 10.1016/s0090-3019(96)00370-9. [DOI] [PubMed] [Google Scholar]
- 6.Kowalski RG, Claassen J, Kreiter KT, Bates JE, Ostapkovich ND, Connolly ES, et al. Initial misdiagnosis and outcome after subarachnoid hemorrhage. JAMA. 2004;291:866–9. doi: 10.1001/jama.291.7.866. [DOI] [PubMed] [Google Scholar]
- 7.Linet MS, Stewart WF, Celentano DD, Ziegler D, Sprecher M. An epidemiologic study of headache among adolescents and young adults. JAMA. 1989;261:2211–6. [PubMed] [Google Scholar]
- 8.Linn FH, Rinkel GJ, Algra A, van Gijn J. Incidence of subarachnoid hemorrhage: Role of region, year, and rate of computed tomography: A meta-analysis. Stroke. 1996;27:625–9. doi: 10.1161/01.str.27.4.625. [DOI] [PubMed] [Google Scholar]
- 9.Mayer PL, Awad IA, Todor R, Harbaugh K, Varnavas G, Lansen TA, et al. Misdiagnosis of symptomatic cerebral aneurysm: Prevalence and correlation with outcome at four institutions. Stroke. 1996;27:1558–63. doi: 10.1161/01.str.27.9.1558. [DOI] [PubMed] [Google Scholar]
- 10.Polmear A. Sentinel headaches in aneurysmal subarachnoid haemorrhage: What is the true incidence? A systematic review. Cephalalgia. 2003;23:935–41. doi: 10.1046/j.1468-2982.2003.00596.x. [DOI] [PubMed] [Google Scholar]
- 11.Schwedt TJ, Matharu MS, Dodick DW. Thunderclap headache. Lancet Neurol. 2006;5:621–31. doi: 10.1016/S1474-4422(06)70497-5. [DOI] [PubMed] [Google Scholar]
- 12.Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–96. doi: 10.1056/NEJMra052732. [DOI] [PubMed] [Google Scholar]
- 13.Van Gijn J, Rinkel GJ. Subarachnoid haemorrhage: Diagnosis, causes and management. Brain. 2001;124:249–78. doi: 10.1093/brain/124.2.249. [DOI] [PubMed] [Google Scholar]
- 14.Vannemreddy P, Nanda A, Kelley R, Baskaya MK. Delayed diagnosis of intracranial aneurysms: Confounding factors in clinical presentation and the influence of misdiagnosis on outcome. South Med J. 2001;94:1108–11. [PubMed] [Google Scholar]
- 15.Vermeulen MJ, Schull MJ. Missed diagnosis of subarachnoid haemorrhage in the emergency department. Stroke. 2007;38:1216–21. doi: 10.1161/01.STR.0000259661.05525.9a. [DOI] [PubMed] [Google Scholar]


