Abstract
Double balloon enteroscopy (DBE) is a revolutionary procedure in which the entire small bowel can be visualized endoscopically. DBE has the advantage of both diagnostic and therapeutic capabilities in the setting of small bowel neoplasms and vascular malformations. We present a unique case of a 76-year-old female who underwent small bowel DBE tattoo marking of a distal small bowel tumor complicated by development of severe abdominal pain postprocedure secondary to bowel air embolism into the mesenteric veins. Mesenteric air can be seen after other endoscopic procedures such as biopsy, mucosal clip placement and polypectomy, or following a colonoscopy. Mesenteric air embolism following small bowel tattooing procedure has not been previously reported in the literature. Mesenteric air when present may be attributed to mesenteric ischemia and can subject the patient to unnecessary surgical intervention if misdiagnosed. Thus, this report holds significance for the radiologist as computed tomography (CT) findings of mesenteric air embolism must be evaluated in the context of appropriate clinical history before treatment decisions are made.
Keywords: CT air embolism, mesenteric air embolism, small bowel tattoo
INTRODUCTION

Double balloon enteroscopy (DBE) consists of an enteroscope and an overtube with a balloon located at either distal end. With a success rate up to 89% and a low complication rate ranging from 0.8% to 4%, common therapeutic applications of DBE include biopsy and tattooing of small bowel lesions, hemostasis, polypectomy, balloon dilation, and foreign body retrieval.[1] DBE can be used in patients in whom capsule endoscopy is contraindicated for suspected bowel strictures and obstruction. Although DBE allows for deeper intubation of the small bowel, most complications arise following therapeutic procedure including electrocoagulation, polypectomy, and dilatation. Air embolism into the mesenteric venous system following a small bowel transmural tattooing procedure has not been previously described in the literature.
CASE REPORT
A 76-year-old female presented to the emergency department with acute abdominal pain and multiple episodes of melena. Initial laboratory workup revealed a guaiac positive stool test and hemoglobin of 6-7 g/dL. Upper and lower endoscopies were negative and capsule endoscopy revealed inconclusive results. A subsequent DBE showed a 3 cm ulcerated lesion in the mid-ileum and a mesenteric mass in the distal small bowel.
The location of the small bowel mass was subsequently marked with mucosal clips and the bowel was enteroscopically tattooed up to the serosal surface with India ink for intraoperative localization for the laparoscopic surgical team. Three hours following the DBE, the patient complained of severe abdominal pain. Concern for bowel perforation was raised and a contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis was ordered. The scan revealed a moderate amount of linear air tracking from the distal small bowel into the adjacent bowel venules and larger mesenteric veins. There was associated haziness surrounding the tumor location consistent with postprocedural edema [Figures 1a, b and 2]
Figure 1.
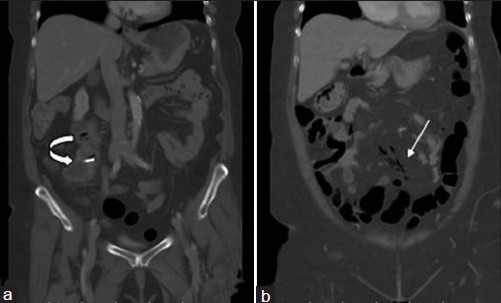
(a and b) Contrast-enhanced coronal CT images (lung window) demonstrate linear pockets of air tracking within small mesenteric veins (white arrow). Note the enteroscopically placed clip in the patient's distal ileal GIST, which was tattooed for the surgeon (curved arrow).
Figure 2.
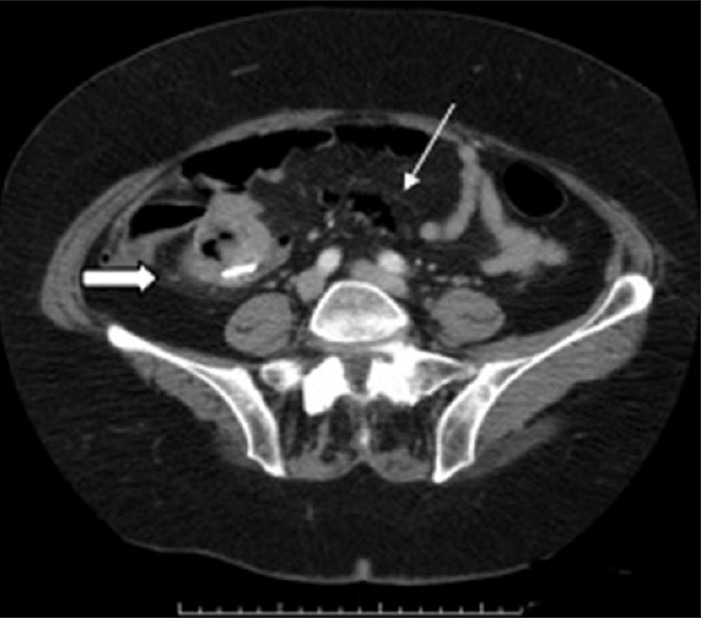
Contrast-enhanced axial CT image demonstrates linear branching pattern of air in the mesenteric veins due to air embolism (white arrow). Note the mild mesenteric stranding around the lesion, a common finding after enteroscopic procedure (thick arrow).
The presence of air in the mesenteric veins could not be attributed to disease pathology based on patient's clinical status and imaging. CT findings were correlated with location of enteroscopic tattoo and this led to the conclusion that bowel alterations from the tattoo procedure ultimately allowed for embolism of intraluminal bowel air into the adjacent mesenteric venous system. Due to this benign iatrogenic etiology of mesenteric venous gas, the patient's symptoms were managed conservatively and improved in a few hours. The patient subsequently underwent a successful laparoscopic small bowel resection for the mesenteric mass, which was confirmed by pathological examination to be a 4.5 × 2.5 × 2.5 cm gastrointestinal stromal tumor (GIST).
DISCUSSION
Since laparoscopic surgery plays a significant role in today's surgical landscape, accurate lesion localization after port placement is paramount since the surgeon does not have the ability to palpate a tumor/lesion in this setting. The serosal surface of bowel lesions is marked on enteroscopy with India ink for preoperative localization or subsequent endoscopic identification of lesions, with an accuracy ranging from 70% to 100%.[1] Endoscopic mucosal clips typically fall of on an average of 10 days and may also spontaneously migrate, making this technique unreliable for lesion localization. Optimal localization can be achieved with enteroscopic tattooing with India ink up to the serosal surface of the affected segment. When the lesion of interest is endoscopically located, the sclerotherapy needle deposits, approximately 0.2-0.5 ml of ink with each injection, through the bowel mucosa circumferentially around the lesion leaving a bluish-black marking visible from both the mucosal and serosal aspect [Figure 3].
Figure 3.

Mucosal surface of enteroscopically tattooed small bowel tumor with India ink. Note the bluish-black appearance of the deposited India ink
According to a large review of enteroscopic tattoo cases by Nizam et al.,[2] the clinical complication risk was only 0.22%. Case reports of adverse events following endoscopic tattoo include focal peritonitis, abscess/hematoma formation, idiopathic inflammatory bowel disease, dye spillage into peritoneal cavity, and tumor inoculation.[3–8] Our case is unique in that it is the first description of enteroscopic tattoo complicated by mesenteric air embolism from the tattooed bowel into adjacent mesenteric veins, presenting as acute abdominal pain.
Mesenteric ischemia is the most common and serious cause of mesenteric air for which surgical management is necessary in the majority of cases. Other causes of mesenteric venous air are associated with disease entities that cause ulceration of bowel mucosa and subsequent air embolism into the adjacent venous system. In iatrogenic cases of mesenteric air secondary to endoscopic procedures, the prognosis is favorable and rarely requires surgical intervention. In this report, the patient's history and presentation are incongruent with the common etiologies of mesenteric air and thus highlight the rarity of this case.
Gas in the great mesenteric veins is well visualized on contrast-enhanced CT scan and air in the small mesenteric veins appear as tubular or branched areas of low attenuation near the bowel margin. Mesenteric venous gas should not be confused with pneumoperitoneum or air in the appendix. Pneumoperitoneum does not have a tubular or branched appearance and can be found in the interface between the antimesenteric border of the bowel and the parietal peritoneum.[9]
CONCLUSION
To our knowledge, this is the first report in literature that describes mesenteric air embolism following an enteroscopic small bowel tattooing procedure, presenting as acute abdominal pain. Although mesenteric air due to bowel ischemia is a common setting, other nonemergent etiologies such as mesenteric venous gas secondary to invasive procedures need to be considered. Radiologists must recognize and differentiate iatrogenic causes of mesenteric air embolism to ensure appropriate clinical or surgical management.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/86/105270
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Trakarnsanga A, Akaraviputh T. Endoscopic tattooing of colorectal lesions: Is it a risk-free procedure? World J Gastrointest Endosc. 2011;3:256–60. doi: 10.4253/wjge.v3.i12.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nizam R, Siddiqi N, Landas SK, Kaplan DS, Holtzapple PG. Colonic tattooing with India ink: Benefits, risks, an alternatives. Am J Gastroenterol. 1996;91:1804–8. [PubMed] [Google Scholar]
- 3.Park SI, Genta RS, Romeo DP, Weesner RE. Colonic abscess and focal peritonitis secondary to india ink tattooing of the colon. Gastrointest Endosc. 1991;37:68–71. doi: 10.1016/s0016-5107(91)70627-5. [DOI] [PubMed] [Google Scholar]
- 4.Marques I, Lagos AC, Pinto A, Neves BC. Rectal intramural hematoma: A rare complication of endoscopic tattooing. Gastrointest Endosc. 2011;73:366–367. doi: 10.1016/j.gie.2010.07.027. [DOI] [PubMed] [Google Scholar]
- 5.Alba LM, Pandya PK, Clarkston WK. Rectus muscle abscess associated with endoscopic tattooing of the colon with India ink. Gastrointest Endosc. 2000;52:557–8. doi: 10.1067/mge.2000.108660. [DOI] [PubMed] [Google Scholar]
- 6.Coman E, Brandt LJ, Brenner S, Frank M, Sablay B, Bennett B. Fat necrosis and inflammatory pseudotumor due to endoscopic tattooing of the colon with India ink. Gastrointest Endosc. 1991;37:65–8. doi: 10.1016/s0016-5107(91)70626-3. [DOI] [PubMed] [Google Scholar]
- 7.Gopal DV, Morava-Protzner I, Miller HA, Hemphill DJ. Idiopathic inflammatory bowel disease associated with colonic tattooing with india ink preparation: Case report and review of literature. Gastrointest Endosc. 1999;49:636–39. doi: 10.1016/s0016-5107(99)70395-0. [DOI] [PubMed] [Google Scholar]
- 8.Tutticci N, Cameron D, Crosse J, Roche E. Peritoneal deposits with carbon pigmentation associated with endoscopic submucosal tattooing of a rectal cancer. Endoscopy. 2010;42:E136. doi: 10.1055/s-0029-1244049. [DOI] [PubMed] [Google Scholar]
- 9.Sebastia C, Quinoa S, Spin E, Boye R, Alvarex-Castells, Armengol M. Portomesenteric vein gas: Pathologic mechanisms, CT findings, and prognosis. Radiographics. 2001;20:1213–24. doi: 10.1148/radiographics.20.5.g00se011213. [DOI] [PubMed] [Google Scholar]


