Abstract
Background:
Experts advocate restructuring health care in the United States into a value-based system that maximizes positive health outcomes achieved per dollar spent. We describe how a value-based system implemented by the University of California, Los Angeles UCLA Section of Endocrine Surgery (SES) has optimized both quality and costs while increasing patient volume.
Methods:
Two SES clinical pathways were studied, one allocating patients to the most appropriate surgical care setting based on clinical complexity, and another standardizing initial management of papillary thyroid carcinoma (PTC). The mean cost per endocrine case performed from 2005 to 2010 was determined at each of three care settings: A tertiary care inpatient facility, a community inpatient facility, and an ambulatory facility. Blood tumor marker levels (thyroglobulin, Tg) and reoperation rates were compared between PTC patients who underwent routine central neck dissection (CND) and those who did not. Surgical patient volume and regional market share were analyzed over time.
Results:
The cost of care was substantially lower in both the community inpatient facility (14% cost savings) and the ambulatory facility (58% cost savings) in comparison with the tertiary care inpatient facility. Patients who underwent CND had lower Tg levels (6.6 vs 15.0 ng/mL; P = 0.024) and a reduced need for re-operation (1.5 vs 6.1%; P = 0.004) compared with those who did not undergo CND. UCLA maintained its position as the market leader in endocrine procedures while expanding its market share by 151% from 4.9% in 2003 to 7.4% in 2010.
Conclusions:
A value-driven health care delivery system can deliver improved clinical outcomes while reducing costs within a subspecialty surgical service. Broader application of these principles may contribute to resolving current dilemmas in the provision of care nationally.
Keywords: Cost, electronic health record, endocrine surgery, patient value
INTRODUCTION
Health care in the United States suffers from high costs, numerous inefficiencies, and less than optimal patient outcomes. Because providers lack information on the actual costs of delivering care, they are hard-pressed to identify opportunities for enhancing resource utilization and eliminating wasteful or nonvalue-added activities.[7] As a consequence, recent attempts at cost reduction, such as limiting services and minimizing the cost of each intervention, have been detrimental to the quality of care.[11] The failure of such efforts to meet national health care needs can be attributed to a narrow focus on cost rather than on the true goal, which is value. Porter and associates have thus advocated for the restructuring of the health care system into a more value-based system, with value defined as health outcomes achieved per dollar spent.[7,11,12]
The UCLA Section of Endocrine Surgery (SES) has sought to maximize value in health care delivery since its establishment in January 2006. One important tactic we have employed is the implementation of clinical pathways. Clinical pathways are evidence-based algorithms that help health care providers make decisions throughout the course of a care cycle, and they are increasingly being used with success to enhance patient outcomes and reduce errors, complications, and costs.[8] Herein we describe the effect of these clinical pathways on outcomes and costs within the broader scope of providing value-based care. We also assess longitudinal trends in patient volume and regional referral patterns as a reflection of the community's response to the level of service provided by the SES.
MATERIALS AND METHODS
Patients and cost data
Electronic records from 44,631 surgical patients admitted to the UCLA Westwood and Santa Monica hospitals from 2005 to 2011 were reviewed. Databases containing diagnoses, procedures, and demographic data were merged to create a master file linked to all associated costs and charges. Using appropriate ICD-9-CM procedure codes, patients who underwent unilateral thyroid lobectomy (codes 6.2, 6.31, and 6.39), total thyroidectomy (codes 6.4, 6.51, and 6.57), or parathyroidectomy (codes 6.81 and 6.89) were selected from the master file. Patients with renal hyperparathyroidism, those undergoing additional concurrent procedures, and those admitted emergently were excluded. Cost data were obtained from the UCLA Medical Center Financial Services department under appropriate institutional review board IRB approval. Patient-identifying information was masked in compliance with the Health Insurance Portability and Accountability Act. Patient comorbidities were quantified using the Deyo modification of the Charlson comorbidity index.[3]
Clinical pathway for allocation of patients to appropriate medical facility
This pathway was implemented in Fall of 2008 (first quarter of the 2009 fiscal year) in response to census pressures at the tertiary care inpatient facility. The criteria used for selecting the appropriate surgical venue for a given patient based on perioperative risk factors are shown in Table 1. Briefly, the pathway considers broad aspects of risk such as technical complexity, patient comorbid conditions (co-existing medical problems such as heart disease or obesity), a history of previous surgery in the same anatomic location thus requiring revision surgery, and adequacy of social supports. The tertiary care inpatient facility is reserved for high complexity cases, the community inpatient facility is utilized for intermediate complexity cases, and the outpatient facility is utilized for low complexity cases.
Table 1.
Surgical facility selection criteria based on perioperative risk stratification
Clinical pathway for initial papillary thyroid cancer management
This clinical pathway was applied to new patients presenting with biopsy-proven papillary thyroid carcinoma (PTC), the most common endocrine malignancy, as described previously.[10] Control patients had total thyroidectomy (TTx) alone, while patients managed according to the pathway had prophylactic central neck dissection (CND) in addition to TTx. Patients underwent long-term surveillance with serial measurements of thyroglobulin (Tg, a tumor marker) and periodic imaging. Tg levels and re-operation rates were compared between groups.
Longitudinal trends in patient volume and regional referral patterns
Demographic data collected included age, gender, race, ethnicity, health insurance, and five-digit zip code for primary residence. Regional market share was calculated using data from the California Office of Statewide Health Planning and Development. Choropleth maps were created using Microsoft MapPoint software.
Statistical analysis
Data were analyzed using STATA/SE version 12.1 (StataCorp, College Station, TX). For univariate analyses, 2-tailed Student's t-test, Chi-square, or one way analysis of variance (ANOVA) were applied, with alpha set to P < 0.05 level. The following nonparametric tests were applied: Wilcoxon rank-sum test, Kruskal – Wallis test, and contingency table tests. In accordance with recommended practices in the field of health economics, the log transformation was applied to all cost data prior to analysis.[6] Costs were adjusted for inflation using the Consumer Price Index and are reported in 2012 dollars.
RESULTS
Clinical pathway for allocation of patients to appropriate medical facility
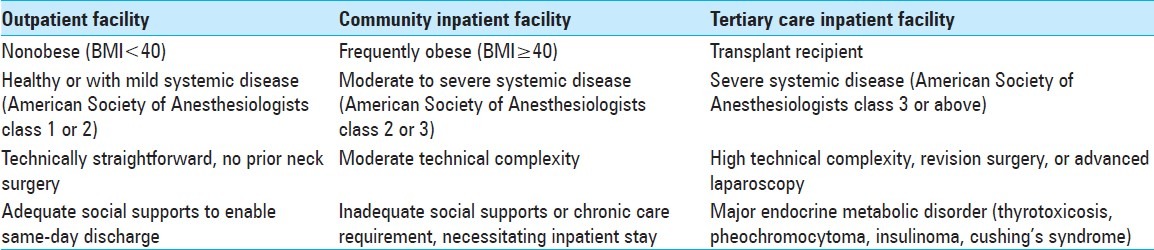
Quarterly case volume increased 39% from 2009 to 2012 [Figure 1]. This growth occurred entirely at the community inpatient facility and the outpatient facility, while case volume at the tertiary care inpatient facility declined by 25% as intermediate-and low-complexity cases were shifted out of the tertiary care facility to relieve inpatient census pressures there.
Figure 1.
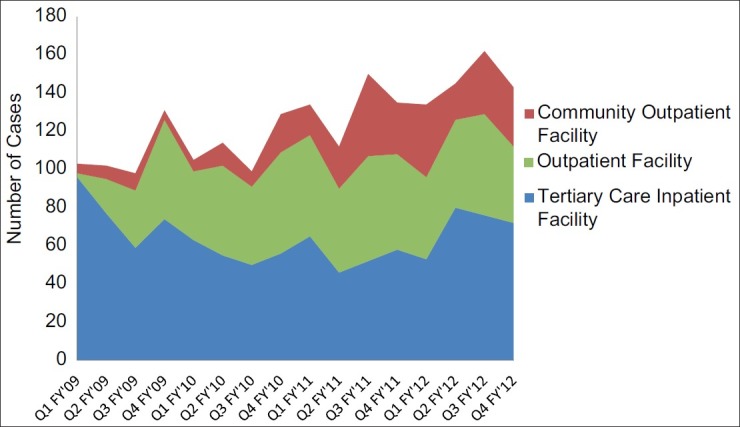
Growth in endocrine case volume in UCLA SES from 2009 to 2012
Figure 2 illustrates the relative mean cost per case of endocrine procedures in the three different surgical facilities (we are unable to report actual costs due to confidentiality agreements). For all endocrine cases combined, the mean cost per case in the community inpatient facility and in the outpatient facility was 85.3% and 41.6% of that in the tertiary care inpatient facility, respectively (P < 0.0001). The mean cost per thyroid lobectomy in the community inpatient and outpatient facilities was 81.86% and 46.68% the cost of same procedure in the tertiary care inpatient facility (P < 0.0001). The mean cost per TTx in the community inpatient and outpatient facilities was 70.59% and 48.60% of the cost of the same procedure in the tertiary care inpatient facility (P < 0.0001). The mean cost per parathyroidectomy in the community inpatient and outpatient facilities was 92.42% and 43.90% of the cost the same procedure in the tertiary care inpatient facility (P < 0.0001).
Figure 2.
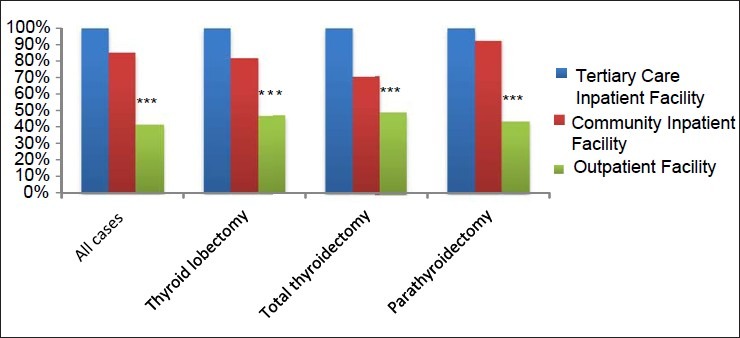
Relative mean cost per case in different UCLA SES facilities (2005-2010); *** P<0.0001
Clinical pathway for initial papillary thyroid cancer management
The full results of this study have been published elsewhere[10] and herein we present only an illustrative snapshot [Figure 3]. Stimulated Tg levels were measured prior to radioactive iodine ablation and therefore reflect the sole effect of initial surgical management. Patients who underwent TTX and CND had lower preablation Tg than those who underwent TTx alone (6.61 vs 15.01 ng/mL; P = 0.024). There was a trend toward lower Tg levels in patients undergoing TTx and CND at final follow-up, (1.9 vs 7.2 ng/mL; P = 0.11). Rates of central compartment re-operation were significantly lower in patients who underwent TTx and CND (1.5% vs 6.1%, P = 0.004). Mean follow up time was 42 months.
Figure 3.
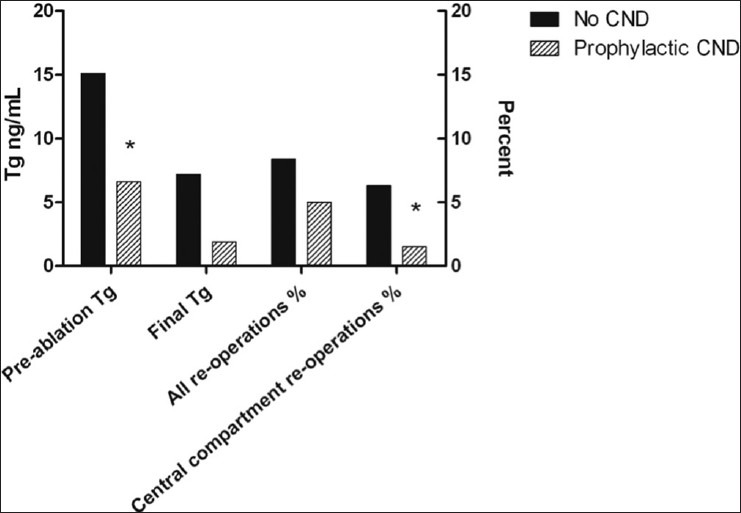
Influence of CND on Tg Levels and re-operation rates. *P<0.05. Adapted from: Popadich A, Levin O, Lee JC, Smooke-Praw S, Ro K, Fazel M, Arora A, Tolley NS, Palazzo F, Learoyd DL, Sidhu S, Delbridge L, Sywak M, Yeh MW. A multicenter cohort study of total thyroidectomy and routine central lymph node dissection for cN0 papillary thyroid cancer. Surgery. 2011 Dec;150(6):1048-57
Longitudinal trends in patient volume and regional referral patterns
Annual patient volume increased from 319 to 494 from 2006 to 2010. The majority of new patients resided within the eight-county region surrounding UCLA [Figure 4], which includes the following counties: Los Angeles, Orange, Riverside, San Bernandino, Ventura, Santa Barbra, Kern, and San Luis Obispo. The total number of zip codes from which at least 1 patient was treated at UCLA increased from 218 in 2006 to 308 in 2010, representing a 41% increase (P < 0.001). Additionally, the number of zip codes from which 4 or more patients were treated increased from 10 in 2006 to 33 in 2010, representing a 230% increase (P < 0.001). From 2003 to 2010, UCLA maintained its position as the market leader in endocrine procedures while expanding its market share by 151% from 4.9% to 7.4% [Figure 5]. During this time period, the annual number of endocrine procedures performed in the region grew 66%. The aggregate market share of the top eleven highest-volume hospitals increased from 25% to 42%, reflecting an overall trend toward case concentration in high-volume centers.
Figure 4.
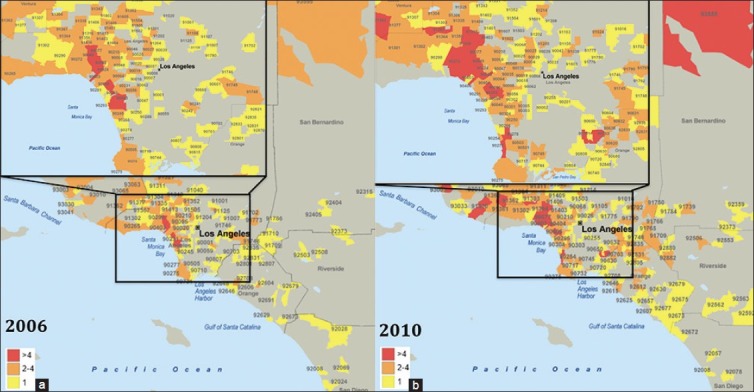
Choropleth maps illustrating distribution of ZIP code of origin for UCLA SES patients in 2006 (a) and 2010 (b)
Figure 5.
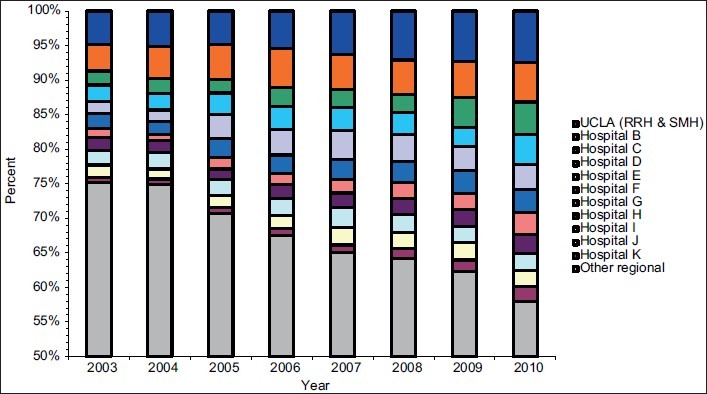
Distribution of market share for endocrine procedures, 8-county region (Los Angeles, Orange, Riverside, San Bernandino, Ventura, Santa Barbara, Kern, San Luis Obispo), fiscal years 2003-2010
DISCUSSION
The UCLA SES has embraced the concept of delivering value in health care since its inception. Our efforts, launched prior to any knowledge of Porter's work, were and are driven by what we consider ethical principles: Optimizing long-term patient outcomes, zero-tolerance for waste, and making world-class care affordable for all patients regardless of insurance status. We subsequently found our practices to be well aligned with the six points of Porter's strategic agenda, which will form the framework of our discussion:[11]
Organize care into integrated practice units around patient medical conditions
Measure outcomes and cost for every patient
Move to bundled prices for care cycles
Integrate care delivery across separate facilities
Expand areas of excellence
Create an enabling information technology platform
Organize care into integrated practice units around patient medical conditions
Currently, the health care system is organized into discrete services, reflecting traditional medical specialties or departments (radiology, anesthesiology, dermatology, etc.), which bear little relation to patient needs. The resulting care is fragmented, inefficient, and inconvenient for patients. The future of health care lies in moving to integrated practice units (IPUs), defined as multidisciplinary teams organized around a specific medical condition or group of conditions with common features. Ideally, IPUs are co-located in dedicated facilities under a unified administrative structure, where functional teams meet regularly. IPUs provide the full cycle of care for the condition(s) treated (everything required to restore the patient to health) and accept joint accountability for outcomes and costs. As a new endeavor, the UCLA SES benefitted from the absence of a structural legacy, permitting its creation as a multidisciplinary program from day one, incorporating team members from the following departments: Surgery, endocrinology, radiology, nuclear medicine, oncology, genetics, and pathology. Each team member devotes a substantial portion of his/her professional time to treating a focused set of conditions: Endocrine tumors (most commonly thyroid cancer), and diseases of endocrine hyperfunction (hormone excess). This arrangement supports the development of expertise.
At present, due to institutional resource limitations, we are not co-localized. Regular multidisciplinary meetings are held to discuss challenging cases, to provide feedback for quality improvement, and to develop and implement improved treatment methods and technologies. As illustrated in our results, the care cycle for these conditions stretches for years, generally obligating lifelong surveillance as thyroid cancer is associated with an excellent survival rate but a significant recurrence rate of 10% at 10 years that cannot be neglected.[1] We hold ourselves accountable for the surveillance process and for managing all recurrences. In providing full service for the aforementioned endocrine diseases, we do not hesitate to manage patients nonsurgically when indicated, thus avoiding unnecessary costs and risks. As we move toward a co-localized IPU we will thus phase out the term “surgery” to create an Endocrine Center, which will function alongside the affiliated Diabetes Center IPU.
Measure outcomes and cost for every patient
We have prospectively tracked patient outcomes in a dedicated endocrine surgery database since the establishment of the SES. Thyroid cancer outcomes are just one of many clinical endpoints that we continuously monitor. Through our long-term scrutiny of the effect of CND, we have demonstrated its beneficial impact with respect to Tg levels and re-operation rates. Though CND remains controversial,[2] the point we wish to drive home is that, regardless of one's position on a given therapeutic technique, systematic outcomes measurement is mandatory for all providers in order to enable quality improvement.
From the economic standpoint, we are assisted by a financial services and decision support department that accounts for costs in a relatively sophisticated manner in comparison to most other hospitals. Costs are subdivided into fixed and variable costs, and are attributed to individual cost centers within the hospital (bed costs, pharmacy costs, laboratory costs, etc.). These figures are considered separately from charges, which appear to bear little relation to costs. We have previously demonstrated cost savings associated with standardizing postoperative calcium management in patients undergoing thyroid surgery,[20] but this is the first time we have described cost differences attributable to different facilities within our organization. The considerable cost savings associated with outpatient endocrine surgery have motivated us to develop innovative methods enabling further shifting of cases to the outpatient setting to the extent possible without compromising patient safety. These methods include rapid parathyroid hormone (PTH) testing, preemptive analgesia to minimize postoperative pain and nausea, and pharmacy changes permitting prompt and/or anticipatory management of postoperative metabolic disturbances.
Move to bundled prices for care cycles
A current obstacle to the implementation of bundled pricing for the diseases we treat is the fact that reimbursement continues to occur at the department level rather than at the IPU level. In the case of the UCLA kidney transplant program, this obstacle was surmounted through a sophisticated cross-departmental financial agreement.[15] Perhaps the most important obstacle to bundled pricing is lack of motivation on the part of insurers, as the diseases we treat are less costly on the population level in comparison to attractive targets such as joint replacement.[13] However, because we accept that bundled prices would best serve our patients ultimately, we have started to develop cost-sharing strategies that will come to greater fruition when co-localization is achieved. This will serve to counteract the current distortion that certain aspects of care, namely procedures, are highly reimbursed while others, such as cognitive aspects of care, are poorly reimbursed.[14]
Our multidisciplinary team does bear a significant clinical and financial burden due to the perverse incentives and moral hazards arising from our nation's current failure to reimburse providers based on the entire care cycle. We currently devote one full day per week to caring for patients who have had failed initial surgery elsewhere, thus requiring revision surgery at our tertiary care facility. We note with dismay that an ineffective (or even unnecessary) operation generates revenue equivalent to that of an effective one, and are resigned to the fact that we will therefore receive a continuous stream of such cases until reimbursement is tied to outcome. Revision surgery is costly to the hospital and to society, and exposes us to significant liability in taking on these high-risk cases. We are financially penalized for providing definitive care in a single episode for the great majority of our patients, eliminating the need for further procedures as evidenced by the data on CND. Similarly, poorly reimbursed long-term surveillance care is generally provided at a loss.
Integrate care delivery across separate facilities
As part of his growth strategy, Dr. Delos Cosgrove, CEO of the Cleveland Clinic, aimed to have multispecialty teams use system-wide resources to deliver the right care at the right place for every patient, at the right time with the right cost.[16] In 2008, in response to seismic damage to the old UCLA Westwood Hospital, all inpatient care at the site was transferred to the new 480-bed Ronald Reagan Hospital (RRH), which was slightly smaller than the old one. The reduced capacity, coupled with the closure of several other hospitals in the region at that time, created a critical high census problem at RRH. The SES, then run as an entirely inpatient service, was thus confronted with the following dilemma: how could we expand a new clinical program without any beds for our patients?
The answer was to expand across facilities within our organization. The prerequisites were creation of the necessary physical environment (obtaining dedicated laboratory and imaging resources) and personnel environment (training of dedicated nursing staff) to support endocrine surgery at the community inpatient facility and outpatient facility. The result of this effort was substantial growth associated with a decrease in the tertiary care inpatient footprint of the service. Additional gains included >50% cost savings at the outpatient facility (largely attributable to reductions in length of stay, which are currently about 3 hours for our outpatient procedures compared with an average of 3 days nationally), improved financial margins, a reduced risk of nosocomial infections, improved patient satisfaction, and reduced patient out-of-pocket expenses. Traditionally, endocrine procedures have been performed in the inpatient setting for fear of complications arising that require inpatient facility resources, but an increasing number of centers are moving towards performing these procedures in the outpatient setting, with very low complication and readmission rates.[4,17,18,19] In our own experience, there have been no unplanned readmissions and no postoperative bleeding events associated with the outpatient setting. As outlined in Table 1, careful patient selection is paramount, as the outpatient care setting is essentially intolerant of any significant perioperative complications. Therefore, we do not recommend that outpatient endocrine surgery be attempted unless outcomes have already been optimized through systematic, experience-based, volume-driven performance improvement.
Expand areas of excellence
Within a relatively short period of time, the UCLA SES has experienced rapid expansion of its market share and geographic area of influence, thereby transforming regional referral patterns. Porter describes this trend toward regionalization as natural result of effective competition, which goes hand-in-hand with optimization of patient value through a self-reinforcing process he terms the “virtuous circle in health care delivery” [Figure 6]. High patient volumes are the principal motivator for care systematization using methods such as clinical pathways. Experience breeds the confidence and knowledge needed to increase efficiency. Experience enabled us to identify and eliminate unnecessary steps in care, resulting in the reduction of laboratory utilization by 70% and total cost by 60% by safely transitioning care to the outpatient setting.[8]
Figure 6.
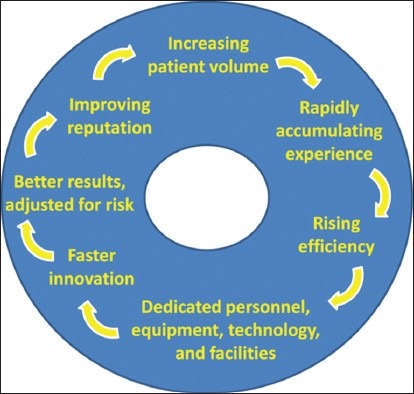
The virtuous circle in health care delivery. Adapted from: Porter ME, Teisberg EO. Redefining health care: creating value-based competition on results. Boston: Harvard Business School Press, 2006
An economy of scale generates adequate return on investment to justify dedicated personnel, facilities, and equipment incorporating expensive new technology. For example, we invested in the fastest platform for the measurement of intraoperative PTH levels (assay turnaround time 8 minutes) and a dedicated technician to run the assay. Other innovations, arising principally from multidisciplinary collaboration, implemented during the past six years include a new probabilistic strategy of interpreting intraoperative PTH values,[5] a new method of selective venous sampling,[9] the development of dynamic computed tomography (4D-CT) for parathyroid imaging, and a multi-level reflex algorithm for the molecular diagnosis of thyroid tumors. All of these factors contribute to the enhancement of the SES's reputation, resulting in increased patient volume and the continuation of the cycle.
Create an enabling information technology platform
In most health care systems, each patient encounter stands alone, and valuable information about the patient is not propagated to the next encounter. With the implementation of the enterprise-wide electronic health record (EHR) at UCLA on March 1, 2013, health care providers will share a single problem list, medication list, and past medical and surgical history list. As the patient passes though different encounters in the course of their treatment, the EHR will update the patient's medical record in a streamlined manner. Healthcare providers that have a longitudinal relationship with the patient (including outside providers such as referring physicians) can easily communicate with each other using the EHR, receive notifications involving patient data when appropriate, and truly function as members of a team in an integrated fashion. In addition, the patient will become part of this team by having real-time electronic access to their medical record thought the Internet.
From a quality standpoint, the EHR will collect structured data, in the form of discrete fields rather than free text, from all stages of the care cycle. It will allow detailed analysis of outcomes, costs, and ultimately value, which will be fed back to providers in a timely fashion to drive improvements in care.
CONCLUSIONS
The UCLA SES has demonstrated that a value-based health care delivery system can improve patient outcomes while reducing costs and growing volume within a subspecialty surgical service. Arguably, this is a relatively small-scale unit, treating a focused area of medical conditions, with motivated leadership and a manageably small number of key personnel and resources. Nonetheless, in seven years the SES has had a measurable impact in one of the largest metropolitan areas in the world, with a population of 15 million. We postulate that broader application of value-based principles may contribute to resolving current dilemmas in the provision of health care nationally.
ACKNOWLEDGMENTS
The authors are grateful to Nora Watson for her assistance with data acquisition and to Michael Pfeffer for his input regarding the electronic health record.
Disclosure statement: The authors have no conflicts of interest to disclose.
IRB approval: The study was approved by the UCLA Institutional Review Board, protocol # 11-000123-CR-00001.
Footnotes
Disclosure statement: The authors have no conflicts of interest to disclose
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/163/105102
IRB approval: The study was approved by the UCLA Institutional Review Board, protocol # 11-000123-CR-00001
Contributor Information
Amer G. Abdulla, Email: aabdulla@mednet.ucla.edu.
Philip H. G. Ituarte, Email: PItuarte@mednet.ucla.edu.
Randi Wiggins, Email: RWiggins@mednet.ucla.edu.
Elizabeth O. Teisberg, Email: TeisbergE@darden.virginia.edu.
Avital Harari, Email: AHarari@mednet.ucla.edu.
Michael W. Yeh, Email: MYeh@mednet.ucla.edu.
REFERENCES
- 1.Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg. 2007;246:375–84. doi: 10.1097/SLA.0b013e31814697d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carling T, Carty SE, Ciarleglio MM, Cooper DS, Gerard M, Kim LT, et al. American Thyroid Association (ATA)-Design and Feasibility of a Prospective Randomized Controlled Trial of Prophylactic Central Lymph Node Dissection for Papillary Thyroid Carcinoma. Thyroid. 2012;22:237–44. doi: 10.1089/thy.2011.0317. [DOI] [PubMed] [Google Scholar]
- 3.Deyo R, Cherkin D, Ciol M. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 4.Hessman C, Fields J, Schuman E. Outpatient thyroidectomy: Is it a safe and reasonable option? Am J Surg. 2011;201:565–8. doi: 10.1016/j.amjsurg.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Hwang RS, Morris LF, Ro K, Park S, Ituarte PHG, Hong JC, et al. A selective, Bayesian approach to intraoperative PTH monitoring. Ann Surg. 2010;251:1122–6. doi: 10.1097/SLA.0b013e3181dd4ee1. [DOI] [PubMed] [Google Scholar]
- 6.Jones A. Applied econometrics for health economists: A practical guide. Oxford: Radcliffe Publishing; 2007. The ordered probit model; p. 22. [Google Scholar]
- 7.Kaplan RS, Porter ME. How to solve the cost crisis in health care. (54,56-61 passim).Harv Bus Rev. 2011;89:46–52. [PubMed] [Google Scholar]
- 8.Kulkarni RP, Ituarte PH, Gunderson D, Yeh MW. Clinical pathways improve hospital resource use in endocrine surgery. J Am Coll Surg. 2011;212:35–41. doi: 10.1016/j.jamcollsurg.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 9.Morris LF, Loh C, Ro K, Wiseman JE, Gomes AS, Asandra A, et al. Non-super-selective venous sampling for persistent hyperparathyroidism using a systemic hypocalcemic challenge. J Vasc Interv Radiol. 2012;23:1191–9. doi: 10.1016/j.jvir.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Popadich A, Levin O, Lee JC, Smooke-Praw S, Ro K, Fazel M, et al. A multicenter cohort study of total thyroidectomy and routine central lymph node dissection for cN0 papillary thyroid cancer. Surgery. 2011;150:1048–57. doi: 10.1016/j.surg.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Porter ME. A strategy for health care reform-toward a value-based system. N Engl J Med. 2009;361:109–12. doi: 10.1056/NEJMp0904131. [DOI] [PubMed] [Google Scholar]
- 12.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–81. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 13.Porter ME. Value based health care delivery; bundled payment in practice hip and knee replacement in Stockholm. Sweden. Cambridge, MA, USA: Innovation in Healthcare Symposium; 2011. [Google Scholar]
- 14.Porter ME, Kaplan RS. Why Medical Bills are a Mystery. The New York Times. Opinion. 2012 [Google Scholar]
- 15.Porter ME, Baron JF, Chacko JM, Tang RJ. The UCLA Medical Center: Kidney Transplantation. Harvard Business School Case. 2012:711–410. [Google Scholar]
- 16.Porter ME, Teisberg EO. Cleveland Clinic: Growth Strategy 2012. Harvard Business School Case. 2012:709–473. [Google Scholar]
- 17.Seybt MW, Terris DJ. Outpatient thyroidectomy: experience in over 200 patients. Laryngoscope. 2010;120:959–63. doi: 10.1002/lary.20866. [DOI] [PubMed] [Google Scholar]
- 18.Snyder SK, Hamid KS, Roberson CR, Rai SS, Bossen AC, Luh JH, et al. Outpatient thyroidectomy is safe and reasonable: experience with more than 1,000 planned outpatient procedures. (582-4).J Am Coll Surg. 2010;210:575–82. doi: 10.1016/j.jamcollsurg.2009.12.037. [DOI] [PubMed] [Google Scholar]
- 19.Trottier DC, Barron P, Moonje V, Tadros S. Outpatient thyroid surgery: Should patients be discharged on the day of their procedures? Can J Surg. 2009;52:182–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Wiseman JE, Mossanen M, Ituarte PH, Bath JM, Yeh MW. An algorithm informed by the parathyroid hormone level reduces hypocalcemic complications of thyroidectomy. World J Surg. 2010;34:532–7. doi: 10.1007/s00268-009-0348-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


