Abstract
Several modes of telepathology exist including static (store-and-forward), dynamic (live video streaming or robotic microscopy), and hybrid technology involving whole slide imaging (WSI). Telepathology has been employed at the University of Pittsburgh Medical Center (UPMC) for over a decade at local, national, and international sites. All modes of telepathology have been successfully utilized to exploit our institutions subspecialty expertise and to compete for pathology services. This article discusses the experience garnered at UPMC with each of these teleconsultation methods. Static and WSI telepathology systems have been utilized for many years in transplant pathology using a private network and client-server architecture. Only minor clinically significant differences of opinion were documented. In hematopathology, the CellaVision® system is used to transmit, via email, static images of blood cells in peripheral blood smears for remote interpretation. While live video streaming has remained the mode of choice for providing immediate adequacy assessment of cytology specimens by telecytology, other methods such as robotic microscopy have been validated and shown to be effective. Robotic telepathology has been extensively used to remotely interpret intra-operative neuropathology consultations (frozen sections). Adoption of newer technology and increased pathologist experience has improved accuracy and deferral rates in teleneuropathology. A digital pathology consultation portal (https://pathconsult.upmc.com/) was recently created at our institution to facilitate digital pathology second opinion consults, especially for WSI. The success of this web-based tool is the ability to handle vendor agnostic, large image files of digitized slides, and ongoing user-friendly customization for clients and teleconsultants. It is evident that the practice of telepathology at our institution has evolved in concert with advances in technology and user experience. Early and continued adoption of telepathology has promoted additional digital pathology resources that are now being leveraged for other clinical, educational, and research purposes.
Keywords: Digital imaging, robotic, static, teleconsultation, telemicroscopy, telepathology, video microscopy, whole slide imaging
INTRODUCTION
Telepathology is defined as the practice of pathology at a distance, transmitting macroscopic and/or microscopic images via telecommunication links for (1) remote interpretations (telediagnosis), second opinions or consultations (teleconsultation), and educational purposes (teleconferencing).[1] With the widespread availability of imaging technology and telecommunication, access to global expert pathologists is no longer a limiting factor.[2] Telepathology has been shown to be applicable for: (i) Anatomical pathology including intra-operative consultation (frozen sections), surgical pathology (second opinions, immunostains), telecytology (e.g., on-site evaluation), and ultrastructural pathology, as well as (ii) Clinical pathology including telehematology, microbiology (e.g., parasitology), and chemistry (e.g., interpretation of gels).
There are three basic modes of telepathology. The first is static (store-and-forward) telepathology that involves the examination of pre-captured still images transmitted via e-mail or stored on a shared server. The second mode of telepathology involves dynamic (live) examination of images in real-time, employing video or robotic microscopy. Finally, hybrid technology involving whole slide imaging (WSI) has emerged that utilizes both dynamic viewing of a digitized (scanned) slide as well as viewing of selected areas of the saved image at higher magnification.
The University of Pittsburgh Medical Center (UPMC) health system operates 20 geographically diverse hospitals within and around the city of Pittsburgh, and also partners with hospitals located in distant states (e.g., Indianapolis, Indiana) and other countries (e.g., Italy, China). The Anatomical pathology department employs an academic Centers of Excellence (COE) subspecialty model, where pathologists in their respective specialty tend to all be located in the same hospital. With this infrastructure, telepathology has been employed at UPMC for over a decade to provide remote subspecialty expertise at local, national, and international sites. The aim of this article is to review the different modes of telepathology and share the experience garnered at UPMC with respect to each teleconsultation method as well as describe future aspects of practicing telepathology.
STATIC TELEPATHOLOGY
Static image telepathology involves capturing, storing, and forwarding individual digital images, or galleries of static images, for remote diagnosis. Advantages of this form of telepathology are the low cost involved, vendor independence, technical simplicity, the fact that the recipient does not require special software to view images, small manageable files are involved (easy to retrieve, send, review, store, and share), and that these systems are easy to maintain. However, disadvantages of static telepathology relate to the fact that the consulting telepathologist has no remote control of the microscope or imaging device/camera, their interpretation is limited to only captured field of views, the host capturing images needs to have some expertise, acquiring images is labor intensive and may cause sampling error if the incorrect images are captured, there is frequent lack of clarity with low power magnification images, and not all still images are in focus.
At UPMC, static telepathology was employed for many years in transplant pathology. Since 1999, consultations were received from ISMETT (Mediterranean Institute for Transplantation and High Specialization Therapies) located in Palermo, Italy. Transplant-related biopsies are usually challenging and hence best interpreted by experts in the field. Access to transplant pathologists is highly desirable for second opinions when dealing with difficult cases. Teleconsultation in this setting also needs to be performed in a timely manner, since rapid and accurate interpretation of allograft biopsies influences outcome after organ transplantation. Moreover, histopathologic interpretation determines whether a donor organ should be used for transplantation or disposed. The transplant telepathology system was, therefore, developed to support coverage 24 hours a day, 7 days a week. Initially, this employed static images run in a store-and-forward mode. Communication was limited to a private network using a thick client-server architecture between the host (e.g., Italy) and UPMC consulting pathologists. Analysis of early (14-month period) accrued data for 102 transmitted cases showed full agreement with the original diagnosis in 86% of cases.[3] For cases with disagreement (14%), 8 resulted in minor and 3 clinically significant differences in opinion. Subsequently, during the 12-year partnership between UPMC and ISMETT, approximately 3000 cases have been reviewed by telepathology. Teleconsultation using static images improved with respect to workflow with only infrequent discrepancies being noted. This first generation home-grown static telepathology system has since been replaced by second generation dynamic robotic microscopy (Nikon Coolscope streaming), third generation hybrid rapid virtual microscopy (Trestle live viewing), and most recently, in 2009, with fourth generation WSI ultra-rapid virtual microscopy (Mirax Midi) [Figure 1]. With better technology allowing pathologists to view entire slides at high resolution, the performance of telepathology has improved. However, we did not change to these newer technologies until these approaches were proven to be technically feasible. Although static images were quicker to read than robotic microscopy, being limited to specific field of views forced evolution. The evolution from static imaging to a WSI scanning system was necessitated due to the lag time required for robotic objective magnification changes and positional adjustments of the slide. With WSI scanning, these magnifications are digitally incorporated into the resultant image, as such the time required for biopsy interpretation was greatly reduced. Secondly, configuring the WSI system with a high numerical aperture (NA) objective (e.g., 40x, 95NA) enabled an image resolution that maximized image clarity (detail), therefore, reducing eye fatigue of the reviewing pathologist, enabling longer review sessions. Lower resolution imagery (e.g., 25 micron) forces the human eye to continually “focus” trying to pull out acute pathology details, which leads to fatigue. Lastly, high resolution scanning enabled subtle details pertaining to tissue rejection to be clearly identified, such as visual confirmation of splitting of the glomerular basement membranes. Combined, these advancements improved the performance of the system such that routine consultation was practical and efficient. Early and continued adoption of telepathology has provided invaluable experience with digital pathology, improved workflow, and accumulated resources (facilitated funding for equipment, IT infrastructure, and staffing) within the transplant pathology division. Today, digital pathology has evolved whereby multiplex-stained WSI is being used for microscopy and image analytics.[4] Multiplexing is defined as the application and analysis of multiple fluorescence markers (typically greater than 3) to a single histologically prepared section. These markers can then be analyzed in the tissue context, quantifying spatial relationships between multiple markers as related to surrounding morphology expression patterns.
Figure 1.
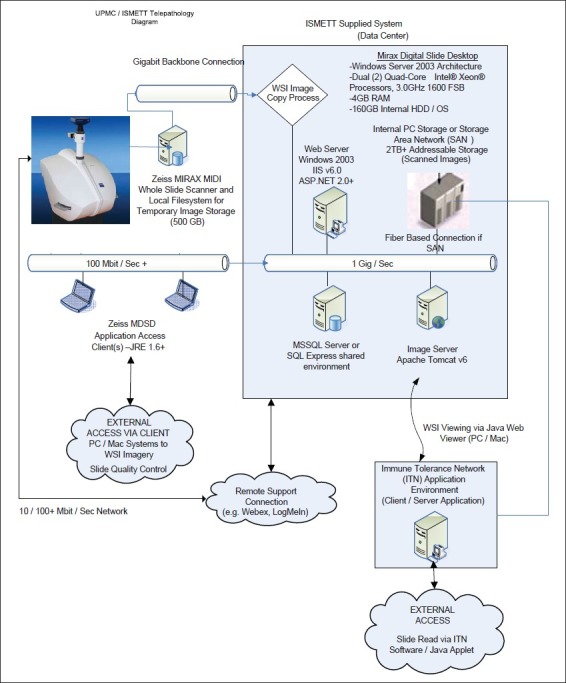
Diagram showing the information technology and server components for the UPMC/ISMETT telepathology platform. Cases are accessioned in the Mirax Digital Slide Desktop (MDSD) image repository (blue box), individual slides are then scanned on the Mirax MIDI WSI scanner and transferred via network file share to the MDSD repository. Access to the images is direct via secure (username/password) connection to the MDSD system from client PC/Mac using a java applet for viewing, or via affiliated/specific workflow applications for the purpose of transplant immunology assessment. The java applet viewer can be embedded in any website or client/server application for flexibility of workflow integration
The division of hematopathology at our institution is another area that employed static telepathology. In several of the academic hospitals, without a hematopathologist on site, telehematology has ensured that interpretation of peripheral blood smears and differentials continue to be performed rapidly and accurately. Expert hematopathologist interpretation is often required for difficult cases (e.g., blasts in leukemia). To accomplish this, the hematology laboratory relied on the CellaVision® automated digital system to digitize glass slides containing peripheral blood smears. The instrument was used to automatically locate and pre-classify digital images of white blood cells, red blood cells, and platelets. Using this system, a technologist in the laboratory was able to email static images of concerning blood cells to a hematopathologist for interpretation [Figure 2], while, in turn, the hematopathologist could access the system and the entire stored differential of a patient remotely from their office computer. Analysis of our experience has shown that this device correctly classified up to 94% of cells, with some reduced accuracy for immature granulocytes.[5] Telehematology has, therefore, allowed patient care at these different hospitals to be standardized. This will also allow clinicians to view digitized blood smears in real time, instead of having to come to the laboratory to physically review the blood smear.
Figure 2.
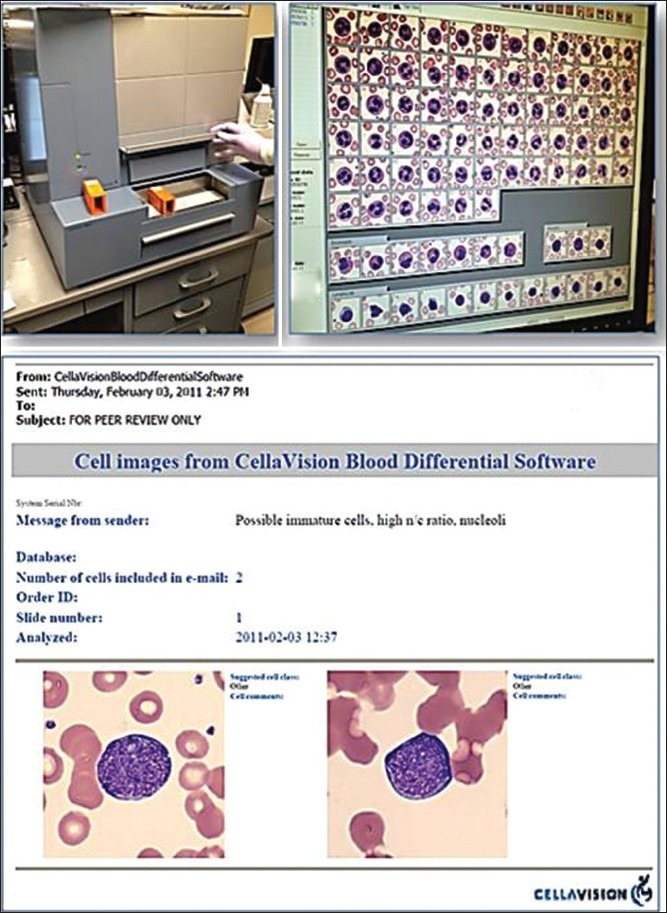
CellaVision® System. (a) CellaVision DM96 instrument; (b) Review monitor displaying captured images of different blood cells; (c) E-mail with embedded selected static images generated using the systems remote review software
DYNAMIC VIDEO MICROSCOPY
Video (or television) microscopy employs a video camera mounted on a microscope. The host “driving” (navigating and focusing) the slide on the microscope, to be viewed by a remote pathologist on a monitor, requires some expertise to perform this task. The remote consulting pathologist is usually in communication (e.g., via telephone or teleconferencing) with the host. However, in order to transmit the image over the Internet, the analog video signal needs to be converted (using an AD converter) to a digital signal. Analog video signals unfortunately are subject to noise and degradation, which may affect the image quality.
While many prior publications regarding telecytology have predominantly utilized static images, in practice, today, most cytology laboratories that use telecytology employ video streaming.[6] At UPMC, live video streaming has remained the mode of choice for providing immediate adequacy assessment of cytology specimens by telecytology. Other methods, such as robotic microscopy, have nevertheless been investigated and shown to be effective.[7] Validation studies conducted in our cytopathology division using web-based streaming have shown that adequacy assessment and diagnostic accuracy with telecytology are acceptable.[8] Nevertheless, cytopathologists found that the “quality” of these digital images were inferior to viewing these cases on a conventional light microscope [Figure 3]. Moreover, cytopathologists documented spending more time reviewing cases examined by telecytology [Figure 4]. These factors may explain, in part, why our cytopathologists only infrequently employ telecytology, despite the fact the necessary equipment to perform telepathology for immediate on-site evaluation of fine needle aspirations is available.
Figure 3.
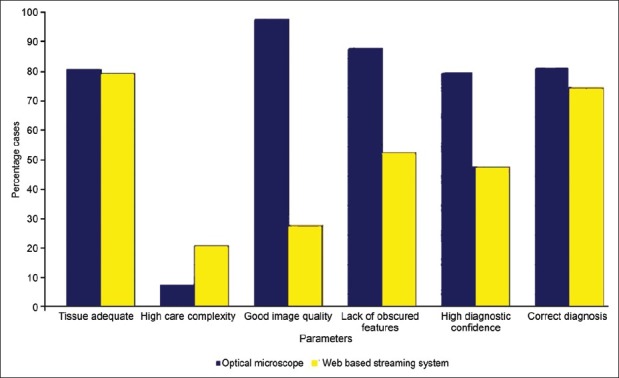
Comparison between glass and telecytology using video streaming. For remote evaluations of fine needle aspirations, cytopathologists demonstrated similar performance using a conventional microscope (blue bars) and the telecytology system (yellow bars) for providing tissue adequacy (far left bars) and the correct diagnosis (far right bars). However, the middle bars in this graph indicate that pathologists found reviewing cases remotely to appear more complex, with inferior image quality and more obscured features. Consequently, they were less confident with their telecytology diagnoses
Figure 4.
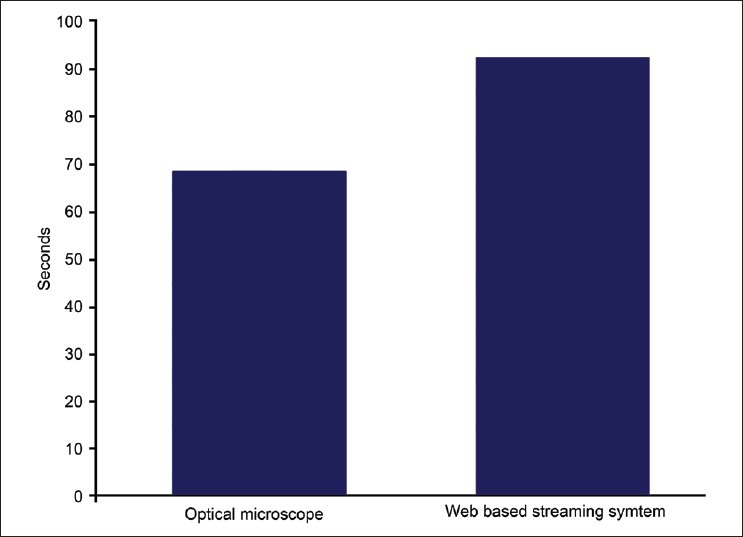
Average time (seconds) taken to review glass and telecytology cases. Cytopathologists took longer to review a cytology slide using telecytology (94 seconds) than they did when examining the same slide with a conventional light microscope (70 seconds)
ROBOTIC TELEPATHOLOGY
Robotic (real-time, dynamic) telepathology differs from video microscopy because the telepathologist (consultant) is now actively involved in selecting fields on the glass slide to be viewed. With a robotic telepathology system, the operator has remote control of critical motorized microscope functions, including glass slide movements in the X- and Y-axes on the motorized microscope stage, focus of the glass slide, and selection of various microscope objective lenses by a robotic turret. This provides the pathologist with access to the entire slide with good image quality. A trained host (e.g., pathology assistant) is still needed to prepare and load slides on the microscope. These devices are expensive and because of their point-to-point network connectivity requirements (i.e. not a web-based protocol) are often not desirable to implement within a hospital IT infrastructure. Additional disadvantages are the relatively slow scanning of slides (approximately 10 min/slide), the fact that both the host and recipient require integrated software, and a required high level of system maintenance for routine optimization, cleaning, and adjustment.
Robotic telepathology has been extensively used at UPMC to remotely interpret intra-operative neuropathology consultations (frozen sections). A considerable volume of neurosurgery is performed within our organization. However, in keeping with our COE model, neuropathologists are all housed at one hospital location. The steady demand for neuropathology frozen sections in different hospitals has been met by utilizing robotic telepathology [Figure 5]. Several Zeiss (previously Trestle) robotic microscopes have been strategically placed within frozen section rooms at the different facilities [Figure 6]. Pathology staff, including trainees, have received instruction on how to handle tissue received for frozen section and load prepared slides onto these microscopes. The importance of such training is a key element to the success of our teleneuropathology service and should not be overlooked. Since only small portions of brain/neural tissue are usually procured and entirely submitted for frozen section, in our experience, we found that a brief gross description of the tissues received to the remote neuropathologist over the telephone by a pathology resident or assistant was sufficient. At one site, a surgical pathologist does the sampling with guidance from a consulting neuropathologist. Nevertheless, a secure webcam in the frozen section room is available to facilitate gross telepathology if required. Also, investigations of newer technologies (e.g., high definition digital cameras and teleconferencing software) are underway in an attempt to improve our macroscopic teleneuropathology capabilities [Figure 7]. Software (MedMicroscopy and Mirax Navigator) to access scanned images and remotely control robotic microscopes has been made readily available on the Internet accessible from any workstation. The diagnostic outcome from 2002 to 2006 (comparing 1227 conventional frozen sections to 402 performed by telepathology) demonstrated that the telepathology deferral rate (19.7%) varied, and was higher than the deferral rate for conventional frozen section cases (10%).[9] However, with the adoption of newer technology (Trestle scanner replaced the Nikon Coolscope) and increased pathologist experience, in 2007 to 2008 (comparing 547 conventional frozen sections to 262 by telepathology), there was acceptable concordance (78.2%) between telepathology and conventional frozen sections.[10] In addition, discrepancy and deferral rate differences during this later time period were statistically insignificant. Intra-operative final discrepancies were uncommon, occurring in only 2.7% of these neuropathology cases. Discrepant events were more common in non-neoplastic (reactive) cases, lymphomas, and with rare tumors. On account of our neuropathology division's unique intra-institutional experience, they were able to successfully expand their teleconsultation practice across state lines (inter-institutional) with a financially separate medical center in Indianapolis, Indiana.[11] Implementation of technology during this venture proved to be easier than the accompanying administrative (e.g., contracts) and legal (e.g., licensing) issues involved.
Figure 5.
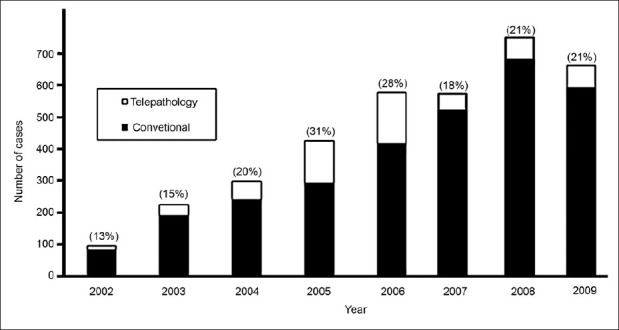
Neuropathology frozen section rate (updated from Horbinski et al. 2007)[9]
Figure 6.
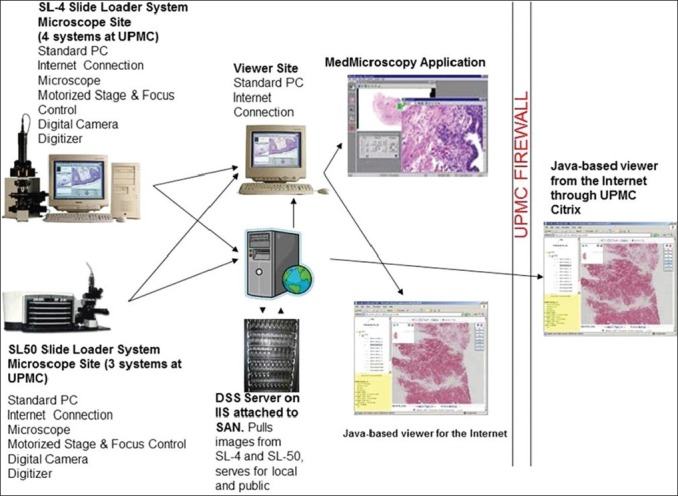
Information technology infrastructure used to support intra-institutional neuropathology frozen section telepathology
Figure 7.
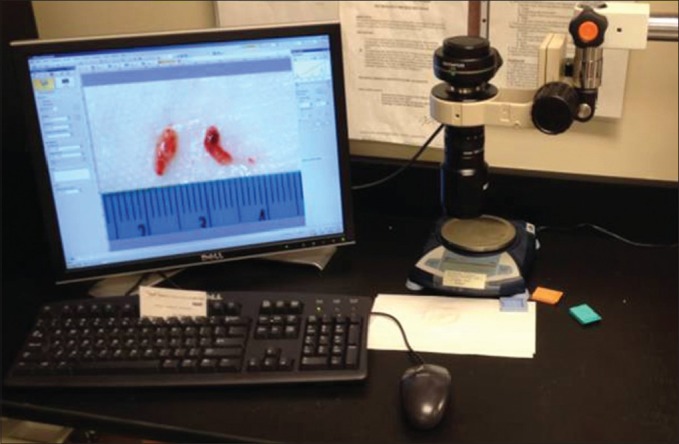
Gross teleneuropathology showing close-up views of two portions of tissue submitted for frozen section from a glioblastoma multiforme tumor
WSI TELEPATHOLOGY
WSI telepathology systems are being increasingly employed for clinical, education, and research applications. Efforts are underway at our institution to eventually replace older telepathology systems with WSI. WSI systems provide users with access to the entire case (including sets of slides), offers automated scanning, and rapidly produces high resolution images. WSI scanners often have added software available for teleconferencing, image management, and image analysis. However, current impediments to their widespread adoption are related to their high expense and limited vendor interoperability. Newer WSI scanners designed to hold one to four slides are smaller and less expensive. With WSI, there is a minor scan failure rate (2-5%).[4,12] Our scan failure rate is particularly low (below 1%),[13] probably because we train our staff to recognize problems before presenting images to pathologists. Furthermore, pathologists maintain a close working relationship with histology to optimize slides for scanning (e.g., care taken to avoid folds, bubbles, etc.). Our IT staff also adjusts scanning technique with the vendor to optimize scanner device settings. Such optimizations included vendor provided focus point algorithm changes to account for tissue artifact (edge effects, folds). Nevertheless, occasional difficulties can be experienced when scanning slides (e.g., misplaced cover slips and sticky wet slides). Small tissue fragments, faint tissue or material at the slide edge or even outside the coverslip may not be recognized. Users may also have to contend with long scan times, especially for thick tissue sections and if high-resolution images are desired (e.g., native high Numerical Aperture 40× scanning). All of these factors may impede the use of WSI for telepathology.
A digital pathology consultation portal (https://pathconsult.upmc.com/) was recently created at our institution.[14] This web-based tool was designed to facilitate digital pathology second opinion consults, especially for WSI. A general portal was developed to be used by all clients, and another that required customization for individual clients [Table 1].[15] With these portals, WSI can either be uploaded for transmission to UPMC consultants (general portal) or accessed on a specific client's server (client-specific portal) [Figure 8]. With the client-specific portal, we are able to avoid lengthy transfers of large WSI files over the Internet as well as automate the process for image association to cases. Despite distance, our viewer shows comparable performance to images viewed on a local server. However, with this client-specific model image files are largely outside our control, we cannot always quickly resolve problems with the client's image server, and any network/hardware changes on the client's side may cause unexpected instability. The general portal allows supported image file types (static and WSI formats of major vendors), as well as pertinent accompanying clinical information, to be uploaded. All clients are offered secure login to submit their patient's data and upload images, as well as to check on the status of their case and view or print second opinion reports. Using this tool, UPMC consultants are able to view digital images using a Java applet. They have the ability to annotate and capture static image snapshots to be embedded into their reports. Reporting has also been incorporated into this web-based application. Workflow is handled by managers who triage requests, monitor cases, and maintain personnel data. Streamlined workflow, as well as training of users, has ensured prompt turn-around time and buy-in by institute pathologists. Post-launch feedback from pathologists has resulted in customization to incorporate transcription services, peer-to-peer review for consultants, provision for issuing addenda and amendments, and improved WSI viewing experience. All cases received via the portal thus far have been surgical pathology cases. On average, 11 WSI per case have been received including H and E, histochemical and immunohistochemistry slides. The mean turnaround time for 22 consulting pathologists was 40 hours (range 2-152 hours). Delayed cases have been attributed mainly to network outage problems.
Table 1.
Different UPMC telepathology portals
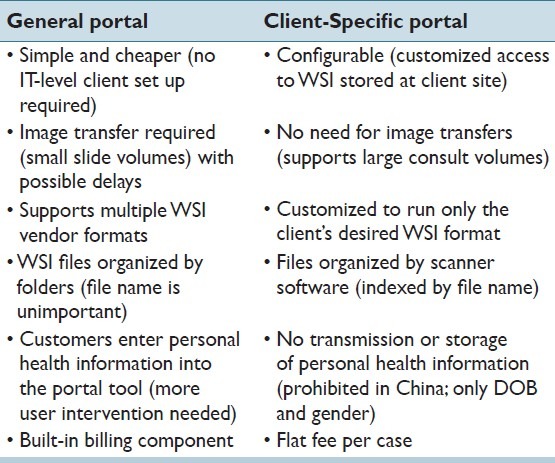
Figure 8.
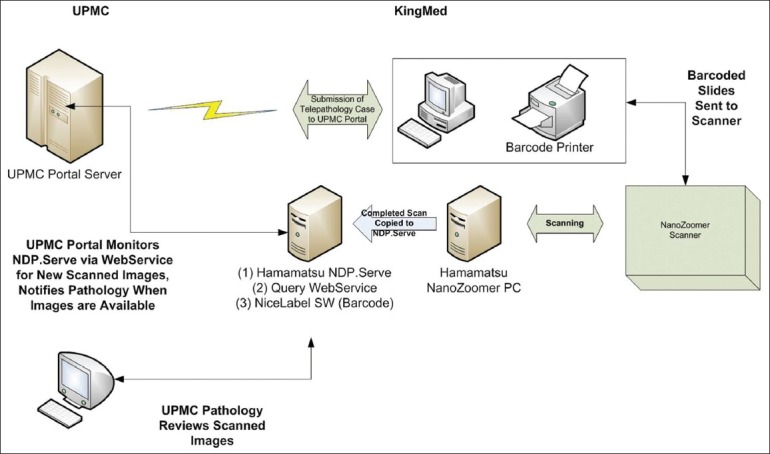
Data workflow with the UPMC Portal and one of their clients (KingMed in China). The data flow utilizes a web service (deployed on the NDP. Serve server) to monitor the NDP. Serve system for completed slide scans that can be associated with a telepathology case. As scans are transferred from the scanner to the NDP. Serve database, this system allows for automated notification of the UPMC assigned pathologist that the case is ready for consult. Perhaps more importantly, this automated system eliminates a person having to email or notify, which scan filenames are associated with a case, thereby removing the possibility of human error of assigning the wrong slide image to a case
CONCLUSIONS
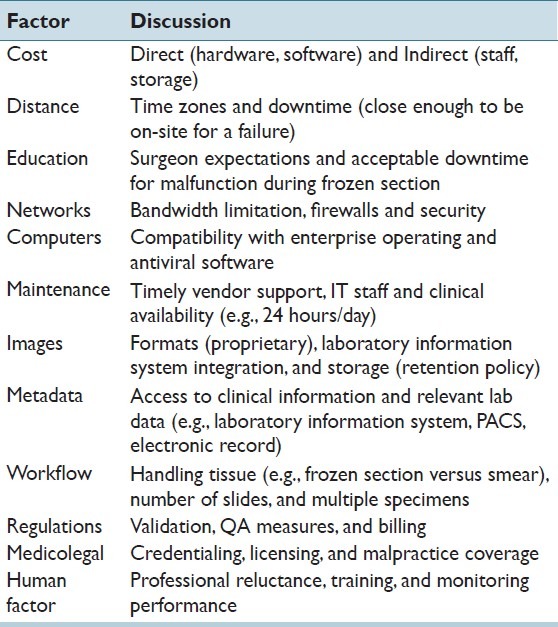
Digital pathology consultation at UPMC has spanned more than a decade. During this time, all modes of telepathology have been successfully utilized to exploit our subspecialty expertise and to compete for pathology services. The practice of telepathology at our institution has evolved in concert with advances in technology, which has become more cost-effective. Although several of the aforementioned modes of practicing telepathology may be outdated, we believe it is nevertheless important to share our experiences and point out that very often “technology” is not the limiting issue, but rather the people and processes involved. Of note, diagnostic accuracy and turnaround time have accordingly improved with advancing technology, as well as user experience. Telecytology has been accomplished largely using real-time video streaming, and for WSI of cytology slides, the low volume of cases received for teleconsultation have been interpretable without the need for scanning slides with Z-stacking. Early and continued adoption has promoted several digital pathology resources (e.g., facilitated funding for equipment, IT infrastructure, and staff) that are now being leveraged for other clinical, educational, and research purposes. We have come to realize that telepathology is not as easy as it looks. Comfort in use is acquired with hands-on practice. Table 2 lists many of the other factors that may need to be considered when practicing telepathology. A key aspect of a successful digital teleconsultation program is integration of digital images (including WSI) into the laboratory information system (LIS) and electronic health record. Such integration, for example, was one of the main objectives of the COST Action “Telepathology Network in Europe” (EURO-TELEPATH).[16] Efforts towards integrating the LIS with WSI are underway at our institution in partnership with Omnyx. Telepathology requirements are different for developed and developing countries. Based on our experience with China, some bottlenecks to telepathology included the high price of WSI devices and regulatory issues. Technological issues, however, are often easier to overcome than administrative, contractual, and legal challenges.
Table 2.
Practical considerations regarding telepathology
POTENTIAL FUTURE SOLUTIONS
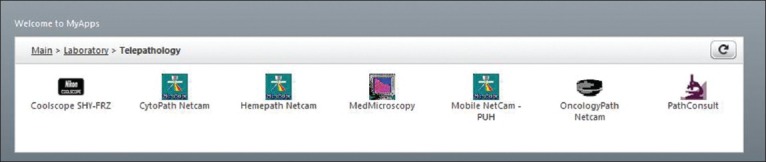
Our institution is currently evaluating newer approaches such as grid technology, open access forums, and mobile solutions to determine how they can be leveraged to enhance telepathology at our institution. Grid technology, which uses open standards to access distributed information, has been suggested by some authors as a way to improve quality in image-based diagnosis.[17] Cloud computing also has benefits for healthcare services.[18] For telepathology purposes, we have provided our pathologists with access to a suite of cloud-based applications through a web browser [Figure 9]. Since the computer programs that support these various telepathology devices are stored on servers at a remote location, the hardware and software demands placed on the end users are greatly diminished. Moreover, cloud computing allows our IT staff to better maintain these telepathology applications. While the use of commercial web conferencing systems (e.g., Skype) has been shown to be feasible for telepathology,[19] in our institutional setting, reliance on public servers raises potential security issues, which has proven to be a barrier for telepathology. More recently, the field of telepathology is witnessing the emergence of specific open access forums (e.g., Medical Electronic Expert Communication System [MECES] with embedded virtual slide technology).[20] These new generation forums, which employ browser-friendly W3C conform standards, offer additional benefits such as acoustic information transfer and assistance in image screening. Finally, taking advantage of mobile devices (e.g., cellular phones), which are almost ubiquitous today, provides another opportunity to perform telepathology almost anywhere and anytime.[21]
Figure 9.
Suite of current telepathology web-based applications available for pathologist use at UPMC
ACKNOWLEDGEMENT
This paper was presented in part as a talk at the Computational and Telepathology Symposium during the XXIX International Congress of the International Academy of Pathology (IAP) in Cape Town, South Africa, 2012. We thank Drs Gautam and Gaurav Sharma for their assistance with our telecytology streaming validation study. The authors are also indebted to our visionary leaders and many fellow pathologists who have embraced telepathology at our institution.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2012/3/1/45/104907
REFERENCES
- 1.Kaplan K, Weinstein RS, Pantanowitz L. Telepathology. In: Pantanowitz L, Balis UJ, Tuthill JM, editors. Pathology Informatics: Theory and Practice. Vol. 16. Chicago: ASCP Press; 2012. pp. 257–72. [Google Scholar]
- 2.Della Mea V. 25 years of telepathology research: A bibliometric analysis. Diagn Pathol. 2011;6(Suppl 1):S26. doi: 10.1186/1746-1596-6-S1-S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Minervini MI, Yagi Y, Marino IR, Lawson A, Nalesnik M, Randhawa P, et al. Development and experience with an integrated system for transplantation telepathology. Hum Pathol. 2001;32:1334–43. doi: 10.1053/hupa.2001.29655. [DOI] [PubMed] [Google Scholar]
- 4.Isse K, Lesniak A, Grama K, Roysam B, Minervini MI, Demetris AJ. Digital transplantation pathology: Combining whole slide imaging, multiplex staining and automated image analysis. Am J Transplant. 2012;12:27–37. doi: 10.1111/j.1600-6143.2011.03797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rollins-Raval MA, Raval JS, Contis L. Experience with CellaVision DM96 for peripheral blood differentials in a large multi-center academic hospital system. J Pathol Inform. 2012;3:29. doi: 10.4103/2153-3539.100154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thrall M, Pantanowitz L, Khalbuss WE. Telecytology: Clinical applications, current challenges and future benefits. J Pathol Inform. 2011;2:51. doi: 10.4103/2153-3539.91129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cai G, Teot LA, Khalbuss WE, Yu J, Monaco SE, Jukic DM, et al. Cytologic evaluation of image-guided fine needle aspiration biopsies via robotic microscopy: A validation study. J Pathol Inform. 2010;26:1. doi: 10.4103/2153-3539.63826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma G, Sharma G, Shah A, Monaco S, Khalbuss W, Parwani A, et al. Evaluation of web based streaming as a tool in telecytology. J Pathol Inform. 2011;2(43):S40–1. [Google Scholar]
- 9.Horbinski C, Fine JL, Medina-Flores R, Yagi Y, Wiley CA. Telepathology for intraoperative neuropathologic consultations at an academic medical center: A 5-year report. J Neuropathol Exp Neurol. 2007;66:750–9. doi: 10.1097/nen.0b013e318126c179. [DOI] [PubMed] [Google Scholar]
- 10.Horbinski C, Wiley CA. Comparison of telepathology systems in neuropathological intraoperative consultations. Neuropathology. 2009;29:655–63. doi: 10.1111/j.1440-1789.2009.01022.x. [DOI] [PubMed] [Google Scholar]
- 11.Wiley CA, Murdoch G, Parwani A, Cudahy T, Wilson D, Payner T, et al. Interinstitutional and interstate teleneuropathology. J Pathol Inform. 2011;2:21. doi: 10.4103/2153-3539.80717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yagi Y, Gilbertson JR. Digital pathology from past to the future. J eHealth Technol Appl. 2010;8:73–80. [Google Scholar]
- 13.Patel T, Park S, Duboy J, Parwani AV, Khalbuss WE, Pantanowitz L. Analysis of whole slide imaging (WSI) scan failures. J Pathol Inform. 2012;3(37):S31–2. [Google Scholar]
- 14.Cable W, Yousem SA, McHugh J, Lesniak A, Tseytlin E, Duboy J, et al. Development of a web-based digital pathology consultation portal (DPCP) for providing second opinion consultation services. J Pathol Inform. 2011;2(43):S29–30. [Google Scholar]
- 15.Roy S, Cable W, Tseytlin E, Lesniak A, McHugh J, Lauro GR, et al. Customization of a digital pathology consultation portal for clients. J Pathol Inform. 2012;3(37):S46–7. [Google Scholar]
- 16.Rojo MG, Castro AM, Gonçalves L. COST Action “EuroTelepath”: Digital pathology integration in electronic health record, including primary care centres. Diagn Pathol. 2011;30(6 Suppl 1):S6. doi: 10.1186/1746-1596-6-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Görtler J, Berghoff M, Kayser G, Kayser K. Grid technology in tissue-based diagnosis: Fundamentals and potential developments. Diagn Pathol. 2006;1:23. doi: 10.1186/1746-1596-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He C, Fan X, Li Y. Toward ubiquitous healthcare services with a novel efficient cloud platform. IEEE Trans Biomed Eng. 2012 Oct 5; doi: 10.1109/TBME.2012.2222404. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Kayser K, Borkenfeld S, Djenouni A, Kayser G. History and structures of telecommunication in pathology, focusing on open access platforms. Diagn Pathol. 2011;6:110. doi: 10.1186/1746-1596-6-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klock C, Gomes Rde P. Web conferencing systems: Skype and MSN in telepathology. Diagn Pathol. 2008;3(Suppl 1):S13. doi: 10.1186/1746-1596-3-S1-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park S, Parwani A, Satyanarayanan M, Pantanowitz L. Handheld computing in pathology. J Pathol Inform. 2012;3:15. doi: 10.4103/2153-3539.95127. [DOI] [PMC free article] [PubMed] [Google Scholar]


