Abstract
Black adolescents with mental health problems are less likely than non-Black adolescents with mental health problems to receive treatment, primarily for non-financial reasons including negative perceptions of services and providers, and self-stigma associated with experiencing mental health problems. To better understand these obstacles, 16 adolescents and 11 caregivers, recruited from two K-8th grade elementary-middle schools, participated in four focus groups guided by the unified theory of behavior to explore mental health help-seeking behaviors and perceptions of mental health services. In the focus groups, caregivers acknowledged more positive attitudes about seeking mental health services than adolescents, but both expected the experience of actually doing so to be negative. Adolescents and caregivers also acknowledged social norms that inhibit their mental health help-seeking. Therefore, we conclude that interventions targeting expectancies and social norms might increase the connection of urban, under-resourced Black adolescents and their families to mental health services, and be particularly important given the long-term consequences of untreated mental health problems for this group.
Keywords: Black adolescents, Mental health service use, Help-seeking, Behaviors, Caregivers, Schools
Introduction
Estimates indicate that 12–17 % (7.5–14 million) of youth in the United States have an emotional or behavioral disorder that impairs their functioning, yet only 20–50 % of these youth receive services (Costello et al. 2003; Merikangas et al. 2010). Given their disproportionate residence in resource-poor, urban environments that negatively influence their mental health (Cooley-Quille et al. 2001; Kodjo and Auinger 2004), urban, Black adolescents have particularly high mental health needs and especially limited mental health service use (dosReis et al. 2007). The problem of engaging and retaining ethnic minority youth and their families, especially low income Black adolescents and their families, in mental health treatment has been well documented (Cauce et al. 2002; Lindsey et al. 2006; McKay et al. 1996; USDHHS 2001), including that they face difficulties participating in mental health services because of psychosocial barriers and how they define their own mental health needs (Husky et al. 2011; Lindsey et al. 2006). Interventions to increase their connections to services, however, remain undeveloped (Hoagwood et al. 2007; Breland-Noble et al. 2006; Lindsey et al. 2010b). This is cause for additional concern given their elevated rate of suicidal behaviors (Joe et al. 2009) and participation in other high-risk activities (e.g. early sexual initiation/experimentation, substance abuse, school dropout; Brown et al. 2006; Glied and Daniel 2002; Kadivar et al. 2006).
Help-Seeking Behavior and Service Use Dilemmas Faced by Black Adolescents
Help-seeking by Black adolescents is intertwined with that of Black caregivers/adults in that beliefs and fears about help-seeking are likely shaped by caregivers and other adults in adolecents’ social networks (Lindsey et al. 2006). Extant research suggests that Black adolescents, like Black adults, have a general mistrust of mental health professionals (Molock et al. 2007). Past mistreatment of Blacks in the US mental health system contributes to current mistrust (Breland-Noble et al. 2006; Snowden 2001; Snowden 2003) through multi-generational transmission of these negative expectations (Lindsey et al. 2006). Black adults historically have exhibited greater reliance upon family and religious leaders, spiritual coping and other informal help sources over professional mental health services to address their mental health and psychosocial problems (Blank et al. 2002). Concurrently, people of color are far more likely than whites to use emergency services and African-Americans in particular seem to be at risk for involuntary commitment, the experience of which is likely to reinforce fears and mistrust (Chow et al. 2003). A similar trend can be seen among Black adolescents, whereby they also express mistrust of formal mental services and professionals (Molock et al. 2007). Black adolescents indicate a fear that mental health professionals will stereotype them, provide a misdiagnosis, and/or not understand their unique ethnic-related challenges (e.g. experiencing harassment from law enforcement officials, negative interactions with school personnel) if they present for mental health care (Lindsey 2010).
Barriers to engaging Black youth and families, in general, have often been conceptualized as structural (e.g. child care, time of day) or perceptual (e.g. parent believes child does not have a mental health problem or that mental health services are not helpful) (Kazdin and Wassell 2000; Owens et al. 2002; Vanderbleek 2004). These barriers are often assessed from the perspective of caregivers. Adolescents, however, face unique contingencies that facilitate or deter their positive connections to mental health services: (1) increased autonomy from parents regarding whether to participate in particular behaviors they might be view as problematic (e.g. whether to smoke cigarettes, drink alcohol or do drugs) (Smetana et al. 2004); and (2) adolescent and caregiver agreement/disagreement regarding mental health needs and whether formal mental health services are necessary to resolve observed problems (Williams et al. 2011).
School Mental Health Service Use
School-based mental health services provide the bulk of mental health services to children and adolescents (Farmer et al. 2003; Rones and Hoagwood 2000; Snowden and Yamada 2005; Stephan et al. 2007). As such, it is important to examine factors influencing help-seeking and service use among adolescents in this environment (Mills et al. 2006). The effectiveness of school-based mental health programs has been well-documented (Burns and Hoagwood 2004; Hoagwood and Burns 2005; Kazdin 2005; Stephan et al. 2007). School-based mental health services have been shown to enhance access to other services (Cappella et al. 2011; Weist et al. 1999), assist in reducing the stigma of seeking help from formal sources (Nabors and Reynolds 2000), promote generalization and maintenance of treatment gains (Evans 1999), improve school climate by increasing the perceptions of support available to students and teachers (Bruns et al. 2004; Walrath et al. 2004), and promote a natural, ecologically grounded approach to helping children and families (Atkins et al. 2003; Weist et al. 1999). However, despite the availability of mental health services in most schools, youth with mental health problems (especially ADHD, depression) still face difficulties in accessing them (Foster et al. 2005; Nabors and Reynolds 2000; USDHHS 2001). Identified obstacles for school-based mental health services echo those of other service settings: logistical barriers (e.g. lack of transportation, scheduling, and child care conflicts), perceptions of child mental health problems (e.g. denial of problem severity, belief that problems can be addressed without treatment), and negative perceptions of mental health services (e.g. mistrust of service providers, stigma regarding mental illness) (Lindsey et al. 2006; Owens et al. 2002; Vanderbleek 2004). These barriers may be particularly pronounced for Black adolescents in need of mental health treatment and their families given the structural and perceptual barriers to services faced by this group (Breland-Noble 2004; 2010; Breland-Noble et al. 2011; Owens et al. 2002).
Help-Seeking According to the Unified Theory of Behavior
Several seminal models of child mental health services help-seeking include components seeking to clarify the mechanisms by which families influence children’s mental health service use (Cauce et al. 2002; Costello et al. 1998; Logan and King 2001), often as downward extensions of theories of adult mental health service use to children and youth. While these models help researchers understand the social processes that influence help-seeking behaviors regarding formal service use, they are mainly oriented to adult service utilization without adequate appreciation for unique youth factors (e.g. attitudes, expectancies regarding service use, etc.) that influence youth engagement, satisfaction, and perceptions of service relevance. To our knowledge, a limited number of help-seeking models (c.f., Logan and King 2001) specifically consider adolescents’ attitudes about mental health services and the relation of these attitudes on parents’ attempts to seek formal or informal help for their child.
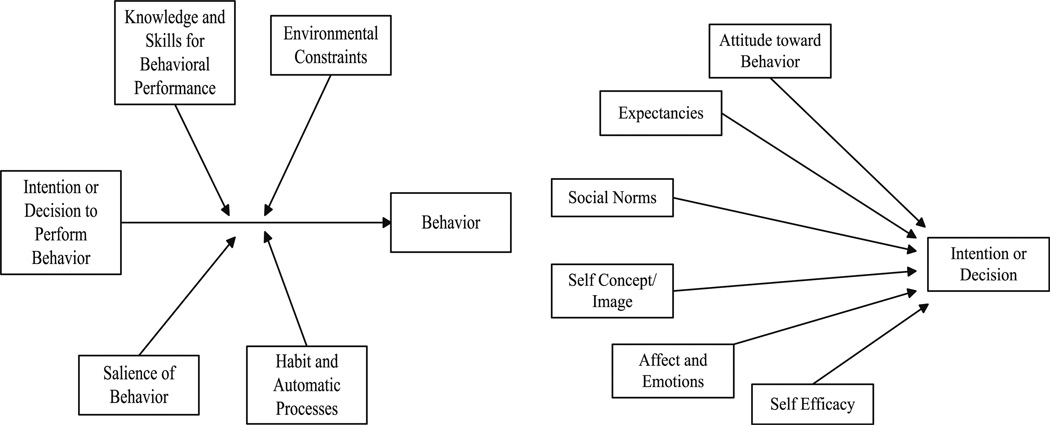
There is a need for greater understanding of both child- and caregiver-focused behavioral determinants of help-seeking, and the Unified Theory of Behavior (UTB) articulates the important behavioral determinants most amenable to change. The UTB (See Fig. 1) is a comprehensive, multivariate framework that incorporates micro- and macro-level constructs from several evidence-based theories of health behaviors and health-related decision-making (Breitkopf et al. 2004; Guilamo-Ramos et al. 2008; Jaccard et al. 2002). This framework emerged out of a week-long meeting convened by the National Institute of Mental Health (NIMH) in 1991 with leading human behavior theorists (Fishbein et al. 2001). The goal of this meeting was to summarize theories of social and developmental psychology under a unifying framework based on their core constructs. Although there was no consensus among the theorists, Jaccard and colleagues subsequently summarized a general framework, along with their specific modifications, into what is now the UTB. Specifically, UTB integrates Social Learning Theory (Bandura 1975), the Theory of Reasoned Action (Ajzen and Fishbein 1980; Fishbein and Ajzen 1975), versions of the Health Belief Model (Janz and Becker 1984; Rosenstock et al. 1988), the Theory of Subjective Culture (Triandis et al. 1972), and self-regulation theories (Kanfer 1987) into a unified theory of behavior decision-making and performance.
Fig. 1.
Unified theory of behavior: a framework for understanding mental health service use
The UTB posits that 11 different interrelated classes of constructs should be empirically examined when considering a given individual’s decision to engage in a target behavior. Specifically, one should first consider (1) the individual’s willingness or intention to perform the behavior in question, i.e. help-seeking via the use of formal mental health services to address a mental health problem, (2) whether the individual has the knowledge, skills and abilities to use mental health services, (3) the environmental constraints and facilitators operating to impede or facilitate mental health service utilization, (4) the salience of using mental health services and the presence of “cues to action” and (5) previous experiences with using mental health services, or what is commonly referred to as habitual and automatic processes (Jaccard et al. 2002).
The UTB then also posits that an individual’s decision to perform a behavior (e.g. one’s intention to utilize mental health services) will not necessarily translate into behavioral performance. However, it is a precursor to performance (Randall and Wolff 1994) and changing intentions has been found to predict changes in behavior (Webb and Sheeran 2006). Therefore, the second set of UTB variable categories are those that shape the likelihood of an intention to engage in actual behavioral performance, and in the case of mental health service use might be conceptualized as: (1) attitudes about mental health service utilization, (2) expectancies about the advantages and disadvantages of using mental health services, (3) normative pressures with respect to utilizing mental health services, (4) views of how utilizing mental health services will affect the image that they want to project, (5) emotional and affective reactions to the prospects of using mental health services, and (6) perceptions of their ability to utilize mental health services (Jaccard et al. 2002). Taken together, these 11 categories represent the proximal determinants of behavioral intentions and performance.
Among its many applications, the UTB offers a powerful framework for understanding behavioral determinants to help-seeking and formal mental health services use for both youth and their caregivers. The UTB does not elucidate specific cultural or environmental factors that influence mental health service use among Black adolescents and their caregivers. However, application of the UTB can facilitate the targeting of core processes and underlying behaviors regarding youth and family engagement, and other family contextual factors influencing service use, including relationships between families and clinicians, and families’ sense of self-efficacy, expectations, and attributions regarding mental health services.
The Current Study
There is a critical need to provide mental health services to Black adolescents with mental health problems. Although a large body of research has documented service need and barriers to treatment among Black adolescents and families (Garland et al. 2005; Owens et al. 2002; USDHHS 2001), less work has focused on factors that may promote treatment engagement, though research in this area is emerging (Breland-Noble 2012; Breland-Noble et al. 2011). In addition, while school mental health services that also involve family members may be an optimal context in which to reach Black adolescents, almost no research has identified the factors associated with successful engagement in school mental health services and that may be amenable to intervention. This study seeks to fill these voids by using qualitative methods (focus groups) to systematically examine help-seeking behaviors and underlying factors related to formal mental health treatment among urban, Black adolescents and their caregivers regarding school mental health services. The use of the UTB as the study’s guiding framework, informed by existing research on mental health need and service utilization of urban, Black adolescents and their families, will facilitate the identification of micro- and macro-level factors associated with help-seeking and perceptions of formal mental health service use that can inform future intervention development.
Method
Participants, Recruitment, and Consent
A total of 16 adolescents and 11 caregivers participated in four focus groups (two adolescent groups and two caregiver groups) during the spring of 2009. Participants were recruited at two elementary/middle schools in the local urban community where the focus groups were held, via flyers delivered to students by the school mental health clinician in their classrooms. Originally, the intention of the study was to recruit caregiver/adolescent dyads, but due to schedule conflicts, only six caregivers were matched with seven adolescents in the focus groups. Therefore, additional students who were interested in participating were enrolled (via consent forms signed by their parents/guardians, giving permission for their child participate in the study) even though their caregiver did not take part. Similarly, additional caregivers were recruited and consented who did not have children in grades 6–8 (a child eligibility criterion). All recruitment and study procedures were approved by University of Maryland Baltimore’s Internal Review Board prior to recruitment.
Final Participant Sample
All participants, including adolescents and caregivers, were African American. Adolescent participants ranged in age from 11 to 14 (mean age = 12.8 [SD = 1.01]), were in grades 6–8 (6.63 [.62]), and comprised 8 boys and 8 girls. Four adolescents self reported that they needed mental health services during the previous 6 months, five indicated having actually received school-based mental health services during the past 6 months, and seven had not received any mental health services in the past 6 months. Interestingly, two students reported not needing mental health counseling but had received counseling the previous 6 months, and one student indicated that they felt that they needed mental health counseling, but had not received it during this time period.
Caregiver participants ranged in age from 31 to 67 (40.75 [11.80]) and all but one were female. Four caregivers reported having attended at least some college, three had completed up to the eleventh grade in school and one reported having obtained a high school equivalency degree. Seven caregivers reported being Protestant (four Baptist and three Methodist), one reported being Catholic, and three did not respond (we did not independently solicit information regarding religious practices from the adolescent participants). Lastly, one caregiver indicated having both needed and received counseling services during the previous 6 months, all other parents reported that they did not need or receive any counseling services during this time period.
Procedures
Data were gathered using standard focus group methods (Krueger and Casey 2000). Focus groups were chosen because they would allow participants to broadly explore barriers and facilitators to help-seeking for mental health, and because the synergy created among participants would foster rich discussion of this content. The study team developed two related facilitator’s guides based on UTB (Jaccard et al. 2002), and the relevant literature summarized above: one for the two adolescent focus groups and one for the two caregiver focus groups. The adolescent groups focused on adolescents’ help-seeking experiences when faced with emotional challenges. Caregiver focus groups were framed by how they sought help for their children, particularly in times when their child struggled with an emotional or mental health-related concern. See Table 1 for sample questions. All focus group facilitators had at least a Master’s degree in psychology or social work, and two groups (1 adolescent and 1 caregiver) were facilitated by PhD-level social workers.
Table 1.
Sample UTB protocol questions
| Adolescent facilitator guide: sample questions | |
| Expectancies | Are there any advantages (or rewards)/disadvantages to using mental health services, i.e. seeing a counselor/therapist about feeling sad/down or hurt inside? |
| Are there any disadvantages (or drawbacks) to using mental health services, i.e. seeing a counselor/therapist about feeling sad/down or hurt inside? | |
| Are there any advantages (or rewards)/disadvantages to not using mental health services, i.e. seeing a counselor/therapist about feeling sad/down or hurt inside? | |
| Are there any disadvantages (or drawbacks) to not using mental health services, i.e. seeing a counselor/therapist about feeling sad/down or hurt inside? | |
| Social norms | Injunctive Norms: Who are the people who approve (or support) of you using school mental health (SMH services)? Note: If mothers approve, what is it about services that mothers approve? |
| Injunctive Norms: Who are the people who disapprove (don’t support) of you using SMH services? Note: If mothers don’t approve, what is it about services that mothers don’t approve? | |
| Descriptive Norms: How many people in your life are likely to influence your getting help from a SMH professional? For example, this might be a best friend, a close friend, someone in your class or a family member. How many of these people are actually using mental health services, whether in schools or in the community? | |
| Caregiver facilitator guide: sample questions | |
| Expectancies | What do you see as the advantages and disadvantages of using/not using SMH or community mental health services to address your child’s mental health issues? |
| Social norms | Injunctive Norms: Who approves or disapproves of your decision to use/not use SMH or community mental health services for your child? |
| Descriptive Norms: How many people in your life influence whether you get help SMH or community mental health services for your child? For example, this might be a best friend, close friend, family member, or neighbor. How many of these people are actually using mental health services of any form? | |
At the beginning of each focus group, a member of the research team reviewed the informed consent with adolescents and caregivers together to enable caregivers to give consent for themselves and their children to participate. For adolescents without a caregiver participating, informed (caregiver) consent and (adolescents’) assent were obtained at another occasion prior to the focus group.
Following consent, each focus group discussion was begun with a brief survey to assess participants’ demographics, asking participants’ age, race/ethnicity, and their highest level of education completed. Next, facilitators introduced the discussion using the facilitator’s guide. As an icebreaker question, adolescents were asked to think of the resources available to them in times of need at their school. The icebreaker question for caregivers concerned their perceptions of the number one challenge caregivers face in rearing their children. Facilitators asked open-ended questions based on constructs in the UTB, followed-up participants’ responses, sought clarification and elaboration as necessary and engaged all participants in discussion. Discussions lasted approximately one and a half hours. The focus groups were held in private offices within the adolescents’ school. All groups were audiotape recorded and then transcribed. Refreshments were provided to all participants during focus groups and one twenty-dollar gift card was raffled off randomly at each adolescent and caregiver group.
Data Analysis
Data were analyzed using template analysis, in which a set of a priori constructs is used to structure analysis of the data (Miller and Crabtree 1999). In this study those constructs were the elements of the UTB. Two Master’s level research staff trained in qualitative research methods independently coded the focus group transcripts for content and proposed categories using established UTB constructs (Miller and Crabtree 1999). First, the coders identified quotes from the group transcripts that linked to the constructs of the UTB and categorized these. The coders then reread the transcripts to identify codes not included within the UTB when content did not match or went beyond UTB constructs. This involved scrutinizing the data to discover recurrent patterns of similar and different meanings, expressions and practices, and tracing back to raw data to ensure data credibility and emergence of theme patterns (Miles and Huberman 1994). Each group’s transcript was then re-coded using this final common list of codes (UTB + other). In final independent coding, the two researchers agreed 95 % of the time. Disagreements were resolved through discussion until a mutually agreed upon code was decided.
In synthesizing themes in the data, we focused on points that demonstrate commonality across the two adolescent groups and the two caregiver groups, and selected transcript quotations to illustrate identified themes and categories. We took several steps to strengthen and corroborate study findings, a qualitative research concept similar to reliability and validity in quantitative research (Miles and Huberman 1994). These steps included using independent investigators to code transcripts, systematic checking of themes against supporting quotations by a second analyst, and an independent review of transcripts, categories, frequency tables, and themes by a third investigator.
Results
The UTB was chosen as our analytic framework because of the comprehensiveness it offers in assessing multiple proximal influences on behavioral performance, in this case school-based mental health services use. In keeping with our template analysis, themes were organized according to UTB constructs. Those that generated the most discussion among participants are presented below, accompanied by illustrative quotes from participants. We first present themes associated with behavioral intentions (e.g. attitudes, expectancies, etc.), followed by themes regarding constructs that shape the likelihood of actual behavioral performance (e.g. knowledge/skills). After these, we present themes that emerged as important in the focus groups but did not map onto a specific UTB construct. Importantly, not all UTB constructs generated themes (e.g. habitual and automatic processes—participants performing the behavior of seeking mental health services as a habit). Therefore, these UTB constructs were interpreted as not salient to the mental health help-seeking experiences for participants in this study.
UTB Construct: Attitudes about Mental Health Help-Seeking Behaviors
For the purposes of this study, the UTB construct “attitude toward target behavior” was defined as feelings of favorability or unfavorability toward seeking mental health treatment for their child (caregivers) or themselves (adolescents). Attitudes about seeking mental health services were primarily positive among caregivers with only a few caregivers relating negative sentiments. However, adolescents were mixed, voicing both positive and negative attitudes toward seeking mental health services. Dominant among the adolescents’ and caregivers’ positive attitudes was the belief that therapy can be supportive in solving personal problems:
…maybe you have a feeling in your body that hurts and you just want to get it out so badly and you finally have someone to tell that you know could help you (adolescent)
I’m glad that my grandson has someone he can come and talk to when things are not right with him. The support here [at school] for him has been really good… I don’t think he could have lasted this long if he did not have someone that he could talk to about how he felt.” (caregiver)
Further, multiple caregivers voiced that therapy would be a good place to obtain support if their child did not feel comfortable talking to family members or friends. For example, one participant said, “I’m happy ‘cause they getting it out; they got somebody to talk to if they feel like they can’t talk to me.”
Some adolescent participants felt that seeing a therapist and seeking help reflected positively on the help-seeker’s character. One said that someone who sought help would be described as “independent” and another called those who did not seek help when they needed it “selfish.” However, despite the general positive comments between the two groups, participants in one agreed unanimously that there were more negative aspects to going to a therapist than positive. These participants said that people who were in counseling were “weird” or “crazy” and one adolescent interjected that he “wouldn’t want any of these random people knowing his business.” This group may have been unique in that the majority of participants did not have prior mental health treatment experiences.
UTB Construct: Expectancies Regarding Mental Health Treatment
Adolescents and caregivers alike voiced many expectations regarding seeking mental health services. Caregivers were divided as to whether they thought therapy would provide positive results and many noted that this was the most important factor in whether they would agree with therapy.
if it’s gonna be positive, if it’s gonna work, I wouldn’t have a problem with sending my child to [a therapist] to get the help
This perspective suggests that caregivers might begin a course of mental health treatment for their child with apprehension about the potential advantages of treatment, which may be mitigated as they see its effects.
Part of caregivers’ expectations regarding the advantages/disadvantages of seeking mental health services also hinged on whether their child would feel comfortable with the therapist, and this played a big role in their ability to comply with the therapist’s recommendations.
…as long as your child is comfortable with that person, it’s easier for you to follow through with all the other plans that’s coming from the therapist
Illustrating how such expectations are often deeply shaped by past experiences, one mother expressed her frustration with being able to find a therapist that was a good fit for her daughter since her daughter had experienced so many therapists that did not work well with her. Among the adolescents, one noted it would be difficult to find therapist that would be a good match because “you might not know which one is good for you because [there are] a lot of good therapists and [there are] a lot of bad ones.”
Other factors shaping treatment expectations were mentioned less prominently. Generally, adolescents did not feel that their therapist’s race would be a disadvantage to seeking mental health treatment; however, a few participants indicated a gender preference for women over men and another felt that the therapist’s gender should match the client’s. Additionally, several adolescents raised the negative expectation of fear that their “parents might get taken away” if they tell a therapist that they were hurt or abused.
UTB Construct: Effect of Social Norms on Mental Health Help-Seeking Behaviors
Social norms (i.e. beliefs about what close family and friends feel one ought to do) regarding help-seeking were discussed in both adolescent and caregiver groups, often via participants’ reflections of hearing negative views about mental health treatment from those around them. These expressions of social stigma were the most prominent theme in this category across all groups. For example, one caregiver noted that family members criticized her sharing family information with any outside person and told her “Why you have my baby going to talk to all these people [mental health therapists]? Why are you putting all these people [mental health therapists] in your business?”
Adolescents were more concerned with being teased or gossiped about by their peers:
I think that it is good that you go to therapy, but not to tell a friend. Because maybe you tell a true friend and then that true friend tell another friend and that friend tell your friend not to hang with her [you]’ cause she’s stupid and all that; she going to therapy. (adolescent)
[A person] not gonna go [to therapy] because they know people gonna tease them saying they stupid and they don’t know nothing (adolescent)
One adolescent specifically related experiencing mental health treatment stigma and the perception that one is weak for using formal mental health services, stating that if “you tell a friend that you’re going to therapy, they gonna think [you] can’t handle that issue.”
Adolescent participants said they sometimes get conflicting messages from family members about where to go for help when troubled. On the one hand, some adolescents felt pressure from their family to get professional help for their issues,
they’re encouraging you to go [to a mental health professional] because they know that you should be there, that maybe those people could help you with your problem
On the other hand, adolescents also shared that family might also feel offended that they weren’t able to help or that they were a second choice. For example, one adolescent shared,
[Family members, friends] feel offended like they could probably help you, but you’re going to a [mental health therapist] because you don’t think that they can help you. [Family members, friends] might get offended because [they] might think that they can’t help you.
UTB Construct: Self-Concept/Image of a Person Goes to Mental Health Treatment
Self-concept was defined as how one perceives oneself or how one thinks others perceives one, in the context of having a child who needs treatment (caregiver) or as someone who is using professional treatment (adolescents). There was very little discussion of this area in the adolescents’ focus groups, although there was general agreement that a youth who needed help should get it—whether from family or mental health professionals. Caregivers, on the other hand, discussed their struggles with self-concept at length, specifically struggling with self-blame for their children’s problems and how their children’s problems reflected their competencies as a parent:
At first for me, when my daughter first started having problems, I took it personal like I wasn’t doing something that I was supposed to do… So I had to put my selfishness to the side and do what’s best for my child
Some caregivers felt that helping their child was more important than any qualms or fears they may have about working with a counselor: “…you know your child need the help, so you go get it for ‘em, I just see that as [being] a parent.” Upon being asked how they would view a parent that did not send their child to a counselor if the child was exhibiting emotional problems, a majority of caregivers in both groups felt that the caregiver was either in denial or lacked parental competency.
UTB Construct: Affect/Emotion Related to Using Mental Health Services
Discussions about affect or emotions regarding mental health service use were infrequent among both adolescents and caregivers. When discussed, caregivers expressed the importance of getting their children help when it is needed.
I feel very strongly about it, ‘cause I know my children need some help and I wanted them to get it. They need it.
One adolescent reported having feelings so intense he had trouble verbalizing them in order to get help.
I guess maybe the feeling that you have that you want to express…maybe that hurts so bad that you can’t get up to just go tell ‘em…you just gonna sit there and think about why you feel like that.
UTB Construct: Efficacy Regarding the Ability to Successfully Seek Help
Self-Efficacy was defined as the ability to do something effectively and its reflection on the self. During the focus groups, only caregivers endorsed feelings of self-efficacy pertaining to help-seeking—adolescents were mostly silent on this theme. Primarily, caregivers related concerns about not being competent to help their children.
…but when something happens like this and you don’t know how to deal with it, how to help them because you don’t want them to be depressed…
Another caregiver interjected that some parents may feel like failures because their children need mental health services, which may also be indicative of their self-concept.
UTB Construct: Knowledge/Skill about Seeking Mental Health Services
Reflections about knowledge of mental health problems and skills associated with obtaining services came primarily from caregivers. Most caregivers expressed uncertainty about the causes of their child’s mental health problems and about what happens in mental health treatment sessions, and resulting uncertainty or caution about services:
…the fact of the matter that we are here today [attending the focus group] is because sometimes as parents we don’t know. We hear about it [child’s mental health problems], but we just don’t know.
Responding to the follow-up probe of how might lack of knowledge influence treatment seeking, another caregiver reflected:
I know for a fact that some of them [caregivers] probably haven’t attended treatment so they wouldn’t know what it’s about.
Caregivers across both groups also expressed a lack of knowledge regarding the role that biology plays in the development of mental health problems. One caregiver, in particular, shared her concern about the role of heredity in the development of her grandson’s mental health problems:
And so his mother has been like this all this time and I’m wondering, you know, did she get it from me, or her father, and then it went on to my grandson like this. So in that perspective, I do think about how it came to be and if the problem, you know, came from my genes.
Caregivers’ comments also reflected incomplete information regarding the potential side effects of psychotropic medications. For example, responding to whether a caregiver would be right or wrong to refrain from putting their child on medication knowing the potential positive impact of the medications on attenuating negative behaviors versus dealing with the side effects the medications might cause, one caregiver reflected:
I wouldn’t say you are being selfish if you don’t want to go that route [psychotropic medications], cause I sure didn’t go that route. I didn’t want to slow my child down slower than what he is. I want him to learn, too. But, if he’s slow, why am I gonna put him on medication to make him slower than what he is? He just needs somebody to talk to.
On the other hand, for some caregivers, the knowledge they might gain from therapists in terms of helping them to understand how best to deal with their child’s emotional/psychological struggles was important. In this sense, they saw therapists as valuable but not always accessible sources of important information about their child. For example, one caregiver felt that it was difficult to extract the information she needed:
…if you don’t ask, nobody’s gonna tell you, because I know they [therapists, school personnel] know what you can do [to get help], but if you don’t ask the right questions, they won’t tell you.
In contrast, another mother related what she has learned working with a mental health counselor at her child’s school:
…when we go to group sessions with her, they give you different techniques and stuff to use; and then it turns around and winds up being helpful, then I can use them same techniques when it comes to different things
Overall, caregivers’ comments reflect a lack of knowledge about mental health services—what happens in a session, whether services are effective, the complexities of side effects—that shapes their expectations and affect regarding seeking and using services for their children. At the same time, at least some see mental health professionals as a potential source of this and other helpful mental health knowledge, but don’t see them as uniformly accessible.
UTB Construct: Environmental Constraints That Potentially Inhibit Mental Health Treatment
Caregivers and adolescents alike described external constraints that hinder their ability to access mental health services for their child or themselves. For example, one adolescent relayed the lack of services in the surrounding community where the school is located:
It’s only one place. There’re not a lot of places; the only place is the community center. That’s probably it.
Multiple caregivers reported financial difficulty:
It was just that he was being seen and medical assistance was canceled.
Maybe she’s focusing on keeping a roof over her head than she actually is on the mental health of the child.
Caregivers also felt that the school system is difficult to navigate when seeking help for a child:
I truly believe when you have so many sectors entering the school system, it’s not working.
It’s like a revolving door, it’s like you go through the chain of command, it’s like you’re spinning back around again… and it keeps going over and over.
You have teachers, but they was never taught how to deal with the different environments of what these children are going through.
UTB Construct: Salience of Mental Health Help-Seeking
Salience was defined as behavioral cues that prompt one to engage in help-seeking related to a mental health problem. First, caregivers in both focus groups cited their commitment to helping their children as a salient aspect of their help-seeking behaviors:
I do whatever it takes to help [my child], regardless of how I’m feeling. I didn’t feel like coming here today, but I did. I pushed myself to come for my child…I’m just a straightforward person. I mean, I didn’t want to, but whatever it takes to help him to get through what he’s going through, I’m there to help him.
Second, caregivers also expressed that their experiences with a mental health professional make help-seeking for mental health services more salient when:
They [mental health therapists] are interested in what’s going on, you know, and ask questions of the child or the parent. And, suggesting things and wait for a response from either one of them…sometimes you can go in the office, seem like they [mental health therapists] not even interested
For adolescents, the most salient, automatic behavior was to keep to oneself, prompted by the risks associated with telling someone your problem—that the person would not understand your circumstances, or they might tell someone else and cause you embarrassment. This was particularly the case among their peer networks. When asked what they do when they have feelings of sadness adolescent focus groups participants made comments such as:
[I] think about it by myself
I cry and write in my journal
I usually read a book
[I] talk to myself
I don’t think you need to share your problems with nobody else
Conversely, when not self-reliant, reliance on the family network became salient. That is, when asked who they go to for help, almost all of the adolescent participants in the focus groups said that they rely on their family members for help:
I go to my mother and my father
I could call my aunt
My godmother
My grandmother
My cousin
I might go to the barber shop where I can talk to my godfather
My brother and my niece
Themes Outside of the UTB
There were important several themes among the focus group discussions that did not map onto UTB constructs. Although we used the UTB to guide our analyses, these other themes are nonetheless potentially important for adding to our conceptualization of factors that influence behavioral performance related to help-seeking for emotional/psychological struggles and using formal mental health treatment as a source of help.
Non-UTB Construct: Difficulty Verbalizing Feelings about the Need for Help
Adolescents frequently discussed difficulty verbalizing emotions. When one adolescent focus group was asked how those close to them know something is wrong they described nonverbal as their main source of communicating. For example,
…she knows I’m sad when I sit down by myself on the floor or just cross my legs
Sometimes I might use my face to show, but sometimes I have to go deeper. Like I can just be looking sad and then I can keep going until they look. Sometimes I have to poke my lips out or go into that face.
My mom can tell because I stay to myself and I make a blank look
One adolescent described why he chooses nonverbal communication over verbal communication by saying,“…because I know that maybe if I do get their attention instead of just talking to them they might help me a little bit more; they might actually know what’s wrong and how to fix it.”
This quote is interesting because it suggests that words may not get people’s attention or be taken as seriously by family members, and that exhibiting non-verbal or behavioral signs of needing help may need to accompany the words to convey the seriousness of the issue. Caregivers concurred that their children often did not verbalize their needs and that it was often difficult to find out how their children were coping. One said, “I have to sort of drag it out of them, or make them tell me saying ‘I can see something’s wrong.” Another speculated that this might be because children are afraid to upset or anger their parents or other family members.
Adolescents’ difficulty verbalizing feeling sad or needing help also seems to go deeper than the points discussed above. During the focus groups, facilitators asked adolescents how sadness or depression felt to them and what actions they took when they felt that way. Only one adolescent mentioned seeking a counselor as a reaction to feeling sad. Many others said that they react angrily to sad or depressed feelings. One said that he “hit people,” while another said he “kicks stuff.” Others said that they would insult whoever is making them feel that way. In one adolescent group, the facilitator asked if feelings of anger were similar to feelings of sadness and adolescents unanimously agreed that this was the case. Making the link between them, when asked how it felt to be sad or hurt, one adolescent responded, “it feels like you’ve been disrespected…” Thus, externalizing behaviors seemed to accompany feelings of sadness or hurt, and these behaviors might be exhibited in lieu of talking about emotional difficulties with someone, i.e. a teacher, parent or therapist.
Non-UTB Construct: Strong Reliance on Spirituality as a Source of Help
Many caregivers from our focus groups indicated that they gain a great deal of strength from their spiritual beliefs and from fellow church members, and at times this may be done in lieu of seeking professional mental health services for their family or child. One caregiver said that he “has his pastor and church family” to count on in times of emotional need. Another mother felt that church served as a protective factor:
I think it’s good if you have religion in your life and you kind of keep in that guideline that you won’t go so far. I mean I came up in church myself; so that was sort of what kept me from going too far, you know, and getting into too much.
One grandmother emphasized the importance of church to her family:
I go to church; I take my grandson to church. He’s been in church since he was born. I have other grandchildren I brought up in church.
Non-UTB Construct: Reliance on School Staff in the Context of Providing Help
Since adolescents spend so many hours with their teachers, it is not surprising that caregivers rely on school staff to support them in parenting their children. This came up in the discussions regarding knowledge and skills associated with help-seeking, but was much broader. For example, one parent mentioned the importance of teachers as role models for her child. Another grandparent emphasized the need for parent-teacher communication:
[My Grandson] will go to his teachers [if he has a problem] and they will carry it a little further. They will call me and say he has a problem. Then we’ll sit and discuss it.
Many caregivers felt that the schools were short staffed and that more teachers were required to give more support to their children both academically and emotionally.
Discussion
This study used a template analysis based on the UTB to discern the mental health help-seeking behaviors and perceptions of mental health treatment that are salient to Black adolescents and their parents/caregivers. Use of the UTB in this manner is particularly apropos in that identifying the factors most germane to performing the desired behavior (e.g. use of mental health services) can enrich the development of intervention strategies to increase the behavior and to attenuate factors like negative expectancies of mental health services or social norms that potentially hinder it.
Our findings indicate that attitudes and expectancies were most the salient UTB constructs to both adolescent and caregivers in terms of their intentions to use mental health services. Generally, both adolescents and caregivers lauded the importance of seeking help to address a mental health concern (positive attitude about mental health helpseeking) in principle, but negative attitudes about treatment also resonated, especially among adolescents with no current or prior mental health treatment history. Both adolescents and caregivers also expected negative or difficult experiences in mental health treatment (e.g. finding a therapist that would be a good match in terms of their level of comfort with the therapist). Caregivers were also concerned about whether mental health treatment would produce positive results for their child. Adolescents expected emotional difficulty in seeking mental health treatment due to fears that what might be revealed to a therapist (e.g. allegations of abuse) could bring further unwanted scrutiny of the family, and fears that friends might stigmatize them for seeking services or family members might be offended if they sought professional rather than family support. Having these contextualized descriptions of participants’ specific concerns, fears, and gaps in knowledge will help us address them in tailored ways that are appealing to these young people and their families. For example, the discussion by adolescent focus group participants of their need for and use of non-verbal expressions of distress deserve even closer attention when we know that the caregiver participants remarked on their children’s silence but did not seem attuned to the non-verbal communications.
Our findings extend prior research (c.f. Brelenad-Noble et al. 2010; Lindsey et al. 2006) on Black adolescents’ attitudes regarding mental health help-seeking in several ways. First, there are only a limited number of studies that include both adolescents and their caregivers’ perspectives (Breland-Noble and Weller online). Including both adolescent and caregiver perspectives may facilitate the design of interventions that address both as they interact with each other. In particular, ambivalence as a motivational construct may be an important dimension of preparing adolescents and their caregivers to be positively engaged in mental health treatment (Brelenad-Noble et al. 2010).
Second, social norms also seemed to be influential regarding help-seeking perceptions and actual service use among both adolescents and their caregivers. Caregivers, reported limited support for mental health treatment among their social networks. Family members and friends of caregivers often expressed ideas that formal mental health services were irrelevant and that family matters, in this case a child’s mental health problems, should be kept within the family. This finding is consistent with a number of studies suggesting that Black families may be more inclined to rely on informal support for addressing emotional or psychological struggles (Blank et al. 2002; Chatters et al. 2011; Snowden 2001).
Additionally, consistent with previous studies of Black adolescents’ help-seeking (Brelenad-Noble et al. 2010; Lindsey et al. 2006), social normative influences among adolescents in this study were mostly related to their concerns about what others would think, say, and how they would respond to their use of mental health services. A related theme from this study that is consistent with prior research (c.f. Ofonedu et al. 2012) is the negative impact of these norms—adolescent participants (male and female) uniformly perceived that use of formal services may be considered a sign of weakness, signaling to others that the individual seeking treatment could not handle their own problems.
Importantly, our findings also include new emergent themes unrelated to the UTB that may be important for the health of Black adolescents and their caregivers. Of particular note is the complex way in which family members must identify an adolescent’s mental health problems. A consistent theme among adolescents was the tendency to not verbalize emotional or psychological struggles. Adolescents tended to want their problems discerned by family members, friends or teachers, behaviorally (body posture, hitting people), instead of expressing their distress verbally or acknowledging a need for help. There may be several explanations for this. As offered by one caregiver, adolescents may perceive that acknowledging mental health-related concerns may bring an added burden or matter of concern to their caregiver. Another explanation might be related to participants’ perceived need to “tough it out” and be self reliant as opposed to asking for help. For adolescents, like our sample, who live in impoverished communities, this may indeed be an important developmental perspective and resilient feature called for by living in an economically deprived or resource-poor circumstance (Anderson 1999).
Unlike Brelenad-Noble et al. (2010) who found that adolescents’ depressive symptoms may be demarcated along gender lines, we did not observe gender differences regarding the expression of anger and other forms of acting out (e.g. fighting, kicking things) as symptoms of sadness or emotional hurt. Both male and female participants described this as common. This finding is noteworthy in that such externalizing behavioral expressions may draw punitive instead of comforting or clinical responses from adults, particularly in a school setting. Therefore, adolescents who exhibit sadness and other forms of emotional pain in volatile, externalizing ways may risk having their problems identified as “bad behavior” and their internal emotional struggles overlooked. This in turn may lead to a greater disconnect from mental health treatment and possible referral to punitive treatments (e.g. detention, juvenile justice).
Finally, our findings reflect the important role teachers’ play in supporting caregivers, both via early identification of mental health and academic problems, and as role models for their children. The lack of resources and support, however, challenge many school districts, such as the one where this study took place. As noted elsewhere (Lindsey et al. 2010a), Black families in urban settings may see schools as an additional source of support, and are likely to support school-based over community-based mental health services. Thus, schools and teachers, in particular, have a great opportunity to bridge the gap between mental health need and treatment for children and families of color. However, this opportunity can be hard to take advantage of and may even become a burden in struggling school districts.
Our findings and the above implications should be viewed in light of the following limitations. First, given our sample size and methods employed, our findings are not generalizable to the larger population of Black adolescents. Rather they raise possibilities that need to be corroborated. Given the disproportionate underutilization of mental health services among Black adolescents (USDHHS 2001), and their higher susceptibility to stigma associated with mental health service use (Lindsey et al. 2010b; Rose et al. 2011), we need more such qualitative investigations to tease out the nuanced factors associated with mental health treatment for this population. Second, focus groups were chosen as the data collection strategy because interaction among participants enhanced their comfort level while participating and generated rich dialogue among them. A limitation of this strategy, however, is that participants may have provided social desirable responses. Third, we did not actively assess mental health symptoms, even while some participants were in school-based mental health treatment at the time focus groups were conducted or had previously received treatment. Thus, we cannot know whether our findings generalize to specific mental health disorders or are affected by the impact of current symptom expression on mental health help-seeking within this sample of Black adolescents and their caregivers. Finally, the UTB framework has been used to understand the salient features of behavioral determinants and to generate the content for closed-end format questionnaires using qualitative methods (Jaccard et al. 2002), and the questionnaire items can be further used to assess the relative weight of UTB constructs in relation to a phenomena, e.g. sexual risk-taking behaviors (Guilamo-Ramos et al. 2008). For our study, however, we only used the UTB framework to develop our facilitator guide and as the template for our analyses. Future research using the UTB to discern Black adolescent’ behavioral determinants to mental health help-seeking might build on this study and employ questionnaires developed from the UTB framework to determine the relative weight of UTB constructs on mental health seeking behaviors. For example such an investigation might ask whether expectancies are as salient to predicting mental health help-seeking behaviors as social norms?
Summary and Conclusions
The goal of this study was to explore factors that influence intentions to engage in mental health help-seeking and formal mental health treatment among urban, under-resourced Black youth. In applying the UTB to understand the phenomena of help-seeking for emotional struggles among this group, we were able to isolate key behavioral determinants that are likely to influence their help-seeking behaviors. In particular, we learned that negative expectancies and social norms regarding formal mental health treatment might potentially represent a major impediment to Black adolescents’ service use.
Our findings have important implications regarding the targeting of specific behavioral dimensions undergirding mental health help-seeking for Black adolescents and their caregivers. In particular, use of the UTB constructs as an analytic template indicated that attitudes, expectancies and social norms are behavioral intentions that resonate most for this group. Thus, treatment engagement strategies that target these behaviors might lead to stronger connections for formal mental health treatment among Black adolescents and their caregivers. For example, negative expectancies might be countered by targeted motivational enhancement strategies that address families’ emotional investment and commitment to change (Breland-Noble 2012; Miller and Rollnick 2002).
Educational strategies might also be employed to increase understanding of mental health symptoms and professional sources for mental health treatment. Even if adolescents and caregivers decided to seek formal treatment, it appeared that participants in our sample struggled with how to interpret early signs of mental health problems and what should be done to address the behaviors. Educational strategies might also target stigma regarding mental health services as one way to address perceptual barriers to care. Finally, educational strategies might also target parents’ negative perceptions of their parenting in the context of their child’s mental health problems. For example, caregivers in our study acknowledged their child’s mental health problems signified their failure as parents. Thus, education strategies might help parents to know their own limits in helping their children and clarify their misconceptions about the etiology of mental illness.
Acknowledgments
Dr. Lindsey was supported for his time in preparation of this manuscript by the University of Maryland Multidisciplinary Research Career Development Program—MCRDP (NIH K12RR023250; PI: Alan R. Shuldiner). Dr. Lindsey was awarded a personal competitive 5-year K12 scholar career development award as allocated under the institutional MCRDP K12 grant awarded to the University of Maryland.
Contributor Information
Michael A. Lindsey, Email: mlindsey@ssw.umaryland.edu, School of Social Work, University of Maryland, 525 W. Redwood Street, Baltimore, MD 21201, USA.
Kerri Chambers, School of Medicine, Department of Psychiatry, University of Maryland, Baltimore, MD 21201, USA.
Cara Pohle, School of Social Work, University of Southern California, Los Angeles, CA 90089-0411, USA.
Peggy Beall, School of Social Work, University of Maryland, 525 W. Redwood Street, Baltimore, MD 21201, USA.
Alicia Lucksted, School of Medicine, Department of Psychiatry, University of Maryland, Baltimore, MD 21201, USA.
References
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- Anderson E. Code of the street: Decency, violence and the moral life of the inner city. New York: W.W. Norton and Company; 1999. [Google Scholar]
- Atkins MS, Graczyk PA, Frazier SL, Abdul-Adil J. Toward a new model for promoting urban children’s mental health: Accessible, effective, and sustainable school-based mental health services. School Psychology Review. 2003;32(4):503–514. [Google Scholar]
- Bandura A. Social learning and personality development. New Jersey: Holt, Rinehart & Winston, INC; 1975. [Google Scholar]
- Blank M, Mahmood M, Fox J, Guterbock T. Alternative mental health services: The role of the black church in the south. American Journal of Public Health. 2002;92:1668–1672. doi: 10.2105/ajph.92.10.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitkopf C, Catero J, Jaccard J, Berenson A. Psychological and sociocultural perspectives on follow-up of abnormal papanicolaou results. Obstetrics and Gynecology. 2004;104:1347–1354. doi: 10.1097/01.AOG.0000143872.07081.84. [DOI] [PubMed] [Google Scholar]
- Breland-Noble AM. Mental healthcare disparities affect treatment of Black adolescents. Psychiatric Annals. 2004;34:534–541. doi: 10.3928/0048-5713-20040701-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breland-Noble AM. Community and treatment engagement for depressed African American youth: The AAKOMA FLOA pilot. Journal of Clinical Psychology in Medical Settings. 2012;19(1):41–48. doi: 10.1007/s10880-011-9281-0. [DOI] [PubMed] [Google Scholar]
- Breland-Noble AM, Weller B. Examining African American adolescent depression in a community sample: The impact of parent/child agreement. Journal of Child and Family Studies. (Online First). [Google Scholar]
- Breland-Noble AM, Burriss A, Bell CC The AAKOMA Project Adult Advisory Board. “Mama just won’t accept this”: Adult perspectives on engaging depressed African American Teens in clinical research and treatment. Journal of Clinical Psychology in Medical Settings. 2011;18(3):225–234. doi: 10.1007/s10880-011-9235-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breland-Noble AM, Bell C, Nicolas G. Family first: The development of an evidence-based family intervention for increasing participation in psychiatric clinical care and research in depressed African American adolescents. Fam Proc. 2006;45:153–169. doi: 10.1111/j.1545-5300.2006.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brelenad-Noble AM, Burris A, Poole HK. Engaging depressed African American adolescents in treatment: Lessons from the AAKOMA project. Journal of Clinical Psychology: In Session. 2010;68(8):868–879. doi: 10.1002/jclp.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Tolou-Shams M, Lescano C, Houck C, Zeidman J, Pugatch D, Oourie KJ Project SHIELD Study Group. Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. Journal of Adolescent Health. 2006;39:e1–e8. doi: 10.1016/j.jadohealth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Bruns EJ, Walrath C, Glass-Siegel M, Weist MD. Association with school climate and special education referrals. Behavior Modification. 2004;28:491–512. doi: 10.1177/0145445503259524. [DOI] [PubMed] [Google Scholar]
- Burns BJ, Hoagwood K. Evidence-based practice, Part I: Research update. Child and Adolescent Psychiatric Clinics of North America. 2004;13:xi–xiii. doi: 10.1016/j.chc.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Cappella E, Jackson DR, Bilal C, Hamre BK, Soulé C. Bridging mental health and education in urban elementary schools: Participatory research to inform intervention development. School Psychology Review. 2011;40(4):486–508. [Google Scholar]
- Cauce AM, Domenech-Rodríguez M, Paradise M, Cochran BN, Shea JM, Srebnik D, et al. Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology. 2002;70(1):44. doi: 10.1037//0022-006x.70.1.44. [DOI] [PubMed] [Google Scholar]
- Chatters LM, Mattis JS, Woodward AT, Taylor RJ, Neighbors HW, Grayman NA. Use of ministers for a serious personal problem among African Americans: Findings from the national survey of American life. American Journal of Orthopsychiatry. 2011;81(1):118–127. doi: 10.1111/j.1939-0025.2010.01079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow GC, Jaffee K, Snowden L. Racial/ethnic disparities use of mental health services in poverty areas. American Journal of Public Health. 2003;93:792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooley-Quille M, Boyd RC, Frantz E, Walsh J. Emotional and behavioral impact of exposure to community violence in inner-city adolescents. Journal of Clinical Child Psychology. 2001;30:199–206. doi: 10.1207/S15374424JCCP3002_7. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Pescosolido BA, Angold A, Burns BJ. A family network-based model of access to child mental health services. Research in Community and Mental Health. 1998;9:165–190. [Google Scholar]
- dosReis S, Mychailyszyn MP, Myers M, Riley AW. Coming to terms with ADHD: How urban African-American families come to seek care for their children. Psychiatric Services. 2007;58:636–641. doi: 10.1176/ps.2007.58.5.636. [DOI] [PubMed] [Google Scholar]
- Evans SW. Mental health services in schools: Utilization, effectiveness and consent. Clinical Psychology Review. 1999;19:165–178. doi: 10.1016/s0272-7358(98)00069-5. [DOI] [PubMed] [Google Scholar]
- Farmer EMZ, Burns BJ, Phillips SD, Angold A, Costello E. Pathways into and through mental health services for children and adolescents. Psychiatric Services. 2003;54:60–66. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Fishbein M, Trandis H, Kanfer F, Becker M, Middlestadt S, Eichler A. Factors influencing behavior and behavior change. In: Baum A, Revenson T, Singer J, editors. Handbook of health psychology. Mahwah, NJ: Lawrence Erlbaum; 2001. [Google Scholar]
- Foster S, Rollefson M, Doksum T, Noonan D, Robinson G, Teich J. School mental health services in the United States 2002–2003. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; 2005. DHHS Pub. No. (SMA) 05-4068. [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. American Journal of Psychiatry. 2005;162:1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- Glied SP, Daniel S. Consequences and correlates of adolescent depression. Archives Pediatric Adolescent Medicine. 2002;156:1009–1014. doi: 10.1001/archpedi.156.10.1009. [DOI] [PubMed] [Google Scholar]
- Guilamo-Ramos V, Jaccard J, Dittus P, Gonzalez B, Bouris A. A conceptual framework for the analysis of risk and problem behaviors: The case of adolescent sexual behavior. Social Work Research. 2008;32(1):30–45. [Google Scholar]
- Hoagwood KE, Burns BJ. Evidence-based practice, part II: Effecting change. Child and Adolescent Psychiatric Clinics of North America. 2005;14:xv–xvii. doi: 10.1016/j.chc.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Hoagwood KE, Olin SS, Kerker BD, Kratochwill TR, Crowe M, Saka N. Empirically based school interventions targeted at academic and mental health functioning. Journal of Emotional and Behavioral Disorders. 2007;15:66–92. [Google Scholar]
- Husky MM, Kaplan A, McGuire L, Flynn L, Chrostowski C, Olfson M. Identifying adolescents at risk through voluntary school-base mental health screening. Journal of Adolescents. 2011;34:505–511. doi: 10.1016/j.adolescence.2010.05.018. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Dodge T, Dittus P. Parent-adolescent communication about sex and birth control: A conceptual framework. In: Feldman S, Rosenthal DA, Damon W, editors. Talking sexuality: Parent-adolescent communication. San Francisco: Jossey-Bass; 2002. New Directions in Child and Adolescent Development. Series Editor. [DOI] [PubMed] [Google Scholar]
- Janz NK, Becker MH. The health belief model: A decade later. Health Education Quaterly. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Joe S, Baser RS, Neighbors HW, Caldwell CH, Jackson JS. 12-month and lifetime prevalence of suicide attempts among black adolescents in the national survey of American life. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:271–282. doi: 10.1097/CHI.0b013e318195bccf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadivar H, Garvie PA, Sinnock C, Heston JD, Flynn PM. Psychosocial profile of HIV-infected adolescents in a southern US urban cohort. AIDS Care. 2006;18:544–549. doi: 10.1080/13548500500228763. [DOI] [PubMed] [Google Scholar]
- Kanfer R. Task-specific motivation: An integrative approach to issues of measurement, mechanisms, processes, and determinants. Journal of Social and Clinical Psychology. 1987;5:237–264. [Google Scholar]
- Kazdin AE. Evidence-based assessment for children and adolescents: Issues in measurement development and clinical application. Journal of Clinical Child and Adolescent Psychology. 2005;34:548–558. doi: 10.1207/s15374424jccp3403_10. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Wassell G. Predictors of barriers to treatment and therapeutic change in outpatient therapy for antisocial children and their families. Mental Health Services Research. 2000;2:27–40. doi: 10.1023/a:1010191807861. [DOI] [PubMed] [Google Scholar]
- Kodjo CM, Auinger P. Predictors for emotionally distressed adolescents to receive mental health care. Journal of Adolescent Health. 2004;35:368. doi: 10.1016/j.jadohealth.2003.12.005. [DOI] [PubMed] [Google Scholar]
- Krueger RA, Casey MA. Focus groups: A practical guide for applied research. Thousand Oaks, CA: Sage Publications, Inc.; 2000. [Google Scholar]
- Lindsey MA. What are depressed African American adolescents males saying about mental health services and providers? In: Johnson WE, editor. Social work with African American males—health, mental health, and social policy. New York, NY: Oxford University Press; 2010. pp. 161–178. [Google Scholar]
- Lindsey MA, Barksdale C, Lambert SF, Ialongo N. Social network influences on service use among urban, African American youth with mental health problems. Journal of Adolescent Health. 2010a;47(4):367–373. doi: 10.1016/j.jadohealth.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey MA, Joe S, Nebbitt V. Family matters: The role of mental health stigma and social support on depressive symptoms and subsequent help seeking among African American boys. Journal of Black Psychology. 2010b;36:458–482. doi: 10.1177/0095798409355796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey MA, Korr WS, Broitman M, Bone L, Green A, Leaf PJ. Help-seeking behaviors and depression among African American adolescent boys. Social Work. 2006;51:49–58. doi: 10.1093/sw/51.1.49. [DOI] [PubMed] [Google Scholar]
- Logan DE, King CA. Parental facilitation of adolescent mental health services utilization: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2001;8(3):319–333. [Google Scholar]
- McKay M, Nudelman R, McCadam K. Involving innercity families in mental health services: First interview engagement skills. Research on Social Work Practice. 1996;6:462–472. [Google Scholar]
- Merikangas KR, He J-P, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010;125:75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles MB, Huberman A. Qualitative data analysis: An expanded sourcebook. 2nd ed. Thousand Oaks, CA: SAGE Publications Ltd.; 1994. [Google Scholar]
- Miller WL, Crabtree BJ. The dance of interpretation. In: Miller WL, Crabtree BJ, editors. Doing qualitative research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999. pp. 127–143. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford Press; 2002. [Google Scholar]
- Mills C, Stephan SH, Moore E, Weist MD, Daly BP, Edwards M. The president’s new freedom commission: Capitalizing on opportunities to advance school-based mental health services. Clinical Child and Family Psychology Review. 2006;9(3/4):149–161. doi: 10.1007/s10567-006-0003-3. [DOI] [PubMed] [Google Scholar]
- Molock SD, Barksdale C, Matlin S, Puri R, Cammack N, Spann M. Qualitative study of suicidality and help-seeking behaviors in African American adolescents. American Journal of Community Psychology. 2007;40:52–63. doi: 10.1007/s10464-007-9122-3. [DOI] [PubMed] [Google Scholar]
- Nabors LA, Reynolds MW. Program evaluation activities: Outcomes related to treatment for adolescents receiving school-based mental health services. Children’s Services: Social Policy, Research, and Practice. 2000;3:175–189. [Google Scholar]
- Ofonedu M, Percy W, Harris-Britt A, Belcher H. Depression in inner city African American youth: A phenomenological study. Journal of Child and Family Studies. 2012;1 [Google Scholar]
- Owens PL, Hoagwood K, Horwitz SM, Leaf PJ, Poduska JM, Kellam SG, et al. Barriers to children’s mental health services. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(6):731–738. doi: 10.1097/00004583-200206000-00013. [DOI] [PubMed] [Google Scholar]
- Randall DM, Wolff JA. The time interval in the intention-behavior relationship: Meta-analysis. British Journal of Social Psychology. 1994;33:405–418. [Google Scholar]
- Rones M, Hoagwood K. School-based mental health services: A research review. Clinical Child and Family Psychology Review. 2000;3:223–241. doi: 10.1023/a:1026425104386. [DOI] [PubMed] [Google Scholar]
- Rose T, Joe S, Lindsey M. Perceived stigma and depression among black adolescents in outpatient treatment. Children and Youth Services Review. 2011;33:161–166. doi: 10.1016/j.childyouth.2010.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM, Stretcher VJ, Becker MH. Social learning theory and the health belief model. Health Education Quarterly. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Smetana JG, Campione-Barr N, Daddis D. Longitudinal development of family decision making: Defining healthy behavioral autonomy for middle-class African American adolescents. Child Development. 2004;75(5):1418–1434. doi: 10.1111/j.1467-8624.2004.00749.x. [DOI] [PubMed] [Google Scholar]
- Snowden LR. Barriers to effective mental health services for African Americans. Mental Health Services Research. 2001;3:181–187. doi: 10.1023/a:1013172913880. [DOI] [PubMed] [Google Scholar]
- Snowden LR. Bias in mental health assessment and intervention: Theory and evidence. American Journal of Public Health. 2003;93(2):239–243. doi: 10.2105/ajph.93.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden LR, Yamada A. Cultural differences in access to care. Annual Review of Clinical Psychology. 2005;1:143–166. doi: 10.1146/annurev.clinpsy.1.102803.143846. [DOI] [PubMed] [Google Scholar]
- Stephan SH, Weist M, Kataoka SH, Adelsheim S, Mills C. Transformation of children’s mental health services: The role of school mental health. Psychiatric Services. 2007;58:1330–1338. doi: 10.1176/ps.2007.58.10.1330. [DOI] [PubMed] [Google Scholar]
- Triandis HC, Vassiliou V, Vassiliou G, Tanaka Y, Shanmugam AV. The analysis of subjective culture. New York: Wiley; 1972. [Google Scholar]
- US Department of Health and Human Services. Mental health: Culture, race, and ethnicity—a supplement to mental health: A report of the surgeon general. Rockville, MD: Author; 2001. [PubMed] [Google Scholar]
- Vanderbleek LM. Engaging families in school-based mental health treatment. Journal Mental Health Counseling. 2004;26:211–224. [Google Scholar]
- Walrath C, Bruns EJ, Glass-Siegel M, Anderson K, Weist MD. Understanding expanded school mental health services in Baltimore City. Behavior Modification. 2004;28:472–490. doi: 10.1177/0145445503259501. [DOI] [PubMed] [Google Scholar]
- Webb T, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin. 2006;132(2):249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- Weist MD, Myers CP, Hastings E, Ghuman H, Han Y. Psychosocial functioning of youth receiving mental health services in the schools vs. community mental health centers. Community Mental Health Journal. 1999;35(5):69–81. doi: 10.1023/a:1018700126364. [DOI] [PubMed] [Google Scholar]
- Williams CD, Lindsey M, Joe S. Parent-adolescent concordance on perceived need for mental health services and its impact on service use. Children and Youth Services Review. 2011;33:2253–2260. doi: 10.1016/j.childyouth.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]