Abstract
Background
Methamphetamine (METH) use, especially in females, has become a growing public health concern in China. In this study, we aimed to characterize the factors that contributed to drug craving in female METH users under isolated compulsory detoxification. We characterized factors contributing to craving such as duration of detoxification, history of drug use and self-reported mood state.
Methods
Subjects (N=113) undergoing a 1- to 3-year METH detoxification program were recruited from the Zhejiang Compulsory Detoxification Center for Women. The Questionnaire of METH-use Urge (QMU) was used to evaluate the level of craving for METH. The Abbreviate Profile of Mood States (A-POMS) was applied as an assessment for the negative mood disturbances.
Results
The participants were at a mean age of 25.2, primarily lowly educated and unemployed, and single. Smoking was the only route of METH administration at an average dose of 0.5 g/day, and 4 times/week. The reported craving level was positively correlated with the negative mood disturbances and the weekly dose of METH, but independent of the duration of detoxification. Furthermore, all five aspects of negative mood disturbances, including fatigue, bewilderment, anxiety, depression and hostility, were shown to positively correlate to the self-reported craving level after controlling for weekly dose of METH.
Conclusions
The data demonstrate a robust correlation between mood distress and craving for METH. Our results call for close evaluation of mood distress in treatment of METH users in China.
Keywords: Methamphetamine, Addiction, Craving, Mood distress, Detoxification
Background
Amphetamine-type stimulant (ATS) use is rapidly increasing worldwide. It is estimated that 3.4–20.7 million people have used ATS in East and South-East Asia, which is approximately 1.4% of the population aged 15–64 years [1]. The number of methamphetamine (METH) users has increased dramatically in China in recent years [2]. In 2001, there were approximately 160,000 registered ATS users a , which consisted of 17.3% of the total registered illicit drug addicts in China [3]. However, by the end of 2010, the number of registered ATS users had increased to approximately 430,000, which consisted of 31.0% of all registered drug users [4].
The evidences have shown that the females can sometimes have worse outcomes than the males in relation to METH use. For example, one study has suggested that women are more likely to become dependent on METH than men [5]. Similar vulnerability to METH has been implicated in several species of rodents. For instance, female Wistar rats are more vulnerable to the acquisition of METH self-administration [6]. Meanwhile, female C57BL/6J mice exhibit a more potent METH-induced conditioned place preference than the male mice, and these gender differences may be facilitated by estradiol [7]. A number of studies have also shown that female METH users exhibit more severe psychiatric symptoms [8-11]. Researchers in Taiwan have found that 43.4% of female METH users suffer from psychiatric problems, 35.9% demonstrate suicidal behavior, and 11.0% are diagnosed with mood disorders [8]. In contrast, only about 31.1% men have psychiatric problems, and 5.6% and 8.9% of them are diagnosed with suicidal behavior and mood disorders, respectively [8]. Similarly, one study in San Diego have shown the high prevalence of depressive symptoms among female METH users, with severe depressive symptoms observed in 60% of them [9] A study focused on adolescents has also found the more symptoms in female METH users by Symptom Checklist-90R, with enhanced cortisol secretion following a social stressor [12]. Taken together, probably vulnerability to METH use in women suggests the necessity for a focus on the female METH users, with attention to the mood states.
In China, drug addicts with confirmed relapses are required to receive isolated compulsory detoxification for 1–3 years [13], where the confirmed relapse means registered drug users being caught abusing drugs repeatedly more than twice. In Zhejiang province, approximately 8.0% of registered drug users were considered as relapsed users, and were enrolled in the detoxification program. During the program, participants were isolated from the communities for at least one year, and evaluated by behavioral improvement. Usually, they receive physical training for the first three months. And in the following months, they get paid work in the working days, and receive education on the weekends regarding drug control law, virtue, and occupational skills. Individuals with severe depressive symptoms or stress are able to receive personal psychological counseling. However, not any forms of cognitive behavioral therapies have yet been introduced into the system. The effect of such compulsory treatment has not been fully evaluated among METH users.
Drug craving is a critical component of addiction, and serves to elicit relapse in psychostimulant users [14,15]. Current data show that craving for METH decreases within two months after abstinence [16]. However, the longer-term effect of abstinence on craving for METH has not been studied. The high rate of relapse suggests that craving might persist or reemerge after a long period of abstinence. Moreover, mood distress is known to increase the craving for nicotine [17-21], alcohol [22,23] and heroin [24] in drug abstinence subjects. However, it is not known whether mood distress also increases the craving for METH.
The purpose of the present study was to determine the factors that contributed to METH craving in the women under isolated compulsory detoxification, who might be expected to have more salient mood problems than their male partners. We focused on the time-dependent effect of the detoxification program and self-reported mood states in female METH users We hypothesized that craving might recur after a longer period of detoxification, and it might be affected by negative moods states.
Methods
Participants
The investigation protocols have been approved by the Institutional Review Board of the Ningbo Addiction Research and Treatment Center according to the Declaration of Helsinki (No. 2010–01). Female METH users, who only or primarily used METH in the last year prior to enroll, were recruited from the Compulsory Detoxification Center for Women in Zhejiang Province. During the detoxification program, subjects were isolated from the community, and spot checks of the urine tests were done every three months to ensure the abstinence. No positive urine test for any of the illicit drugs (e.g. morphine, amphetamine or cocaine) was found in the center during the past two years before our investigation.
Criteria of inclusion were meeting the diagnosis of METH abuse or dependence by DSM-IV, while subjects with diagnosis of abuse or dependence of other substances were excluded. The diagnosis of METH dependence or abuse was made upon self-reports of METH use during the last month when participants had free access to the drug. Voluntary participation was required and subjects received stationery gifts, upon request, for participating. Personal information collected from participants was kept confidential, and the personal data collected were used only for this study. The interviews were undertaken under a separated room, and the officers of the detoxification center were not allowed to stand by or listen to the interviews. Participants gave written informed consent after a full explanation of the study had been provided, and each subject completed the survey under the direction of the trained researchers. This investigation was conducted in Mandarin, and took approximately 30 minutes for each participant to complete.
Questionnaires
A battery of questionnaires was designed and discussed by the researchers. One month before the investigation, researchers discussed the questionnaires item-by-item to exclude any ambiguity that might be introduced in the investigation. Investigators were also taught to express with more understandable oral language which the drug users commonly used. For most of the items, choices were provided to facilitate the investigation, expected for the questions that needed numerical answers. Subjects were allowed to choose multiple-choices answers or to provide their own answers.
Demographic variables included age, ethnicity, education level, occupation, marital status and children. Characteristics of METH use included the onset age of METH use, total duration of METH use (years), frequency (times/week), dose (gram/day), route of administration, environment of METH use in the 12 months prior to incarceration, and the duration of present detoxification.
The Questionnaire of METH-use Urge (QMU) was modified from the Questionnaire of Smoking Urge-brief [25] by replacing the word “smoking” with “using METH”. The Chinese version of Questionnaire of Smoking Urge-brief had been used in a previous study on nicotine craving [26]. The QMU contains 10 items. Participants were asked to indicate how strongly they currently agreed or disagreed with each item using a Likert scale from 1 (strongly disagree) to 7 (strongly agree). The participant responses were classified by two factors. Factor 1 addresses the “intention/desire to use METH” (items 1 and 6), and factor 2 (items 4, 8, and 9) addresses the “anticipation of relief of negative effect/urgent desire to use METH”. It is moderately to highly correlated with the Visual Analog Scale for METH Craving (VASC) (coefficient for QMU factor 1 and VASC: 0.78; for factor 2 and VASC: 0.69, for total scores and VASC: 0.77).
The Abbreviate Profile of Mood States (A-POMS) [27] used in this study is a revision of an earlier version of the Profile of Mood States, and has been modified and translated into Chinese [28]. It contains 40 items rated on a 5-point scale from 0 (not at all) to 4 (extremely). Subscales include 5 negative mood factors (tension-anxiety, depression, anger-hostility, fatigue, and confusion-bewilderment) and 2 positive mood factors (vigor-activity and self-esteem). Total mood disturbance (TMD) was calculated as the sum of negative mood factors minus the positive mood factors, vigor and self-esteem. Higher scores of negative moods indicate a greater degree of mood disturbance. These data are based on mood states experienced and reported ‘during the past week, including today’. The POMS is a well-developed, highly reliable method to assess mood disturbance [29]. It is moderately to highly correlated with other scales, including the Visual Analog Mood Scales, the State-Trait Anxiety Inventory, and the Beck Depression Inventory, with coefficients ranging from 0.72 to 0.79 [30].
Data analyses
The data were tested for normality using the Shapiro-Wilk method and had a skewed distribution. Therefore, the data were analyzed by two-tailed Mann–Whitney U-test and Kruskal-Wallis H test. Categorical variables were analyzed by two-tailed chi-square or Fisher’s exact test. A Spearman correlation was used to determine the relationship between craving, mood, characteristics of drug use, and participant demographics. A Spearman partial correlation was used to investigate the independent factors related to METH craving. The data were analyzed using SPSS for Windows (version 16.0, SPSS, Chicago, IL, USA), and significance was set at p < 0.05.
Results
General information
A total of 113 females were included in this study. Participant demographics and characteristics of METH use are reported in Table 1. Every participant self-administered METH via smoking. Self-report of multiple substances of abuse were present in 40.7% (45/112) of subjects. Other types of ATSs, such as Magu, a methamphetamine-caffeine mixture, were used by 38.9% of the participants, and Ecstasy was used by 12.4%. The top three frequently used non-ATSs were ketamine (28.6%), cannabis (15.2%), and heroin (8.9%).
Table 1.
Participant Demographics and Characteristics of Meth Use (N=113)
| Demographic factors | Mean ± SD/Number (percentage) |
|---|---|
| Age (years) |
25.2 ± 6.9 |
| Education Illiterate |
3 (2.7%) |
| Primary school |
34 (30.1%) |
| Middle school |
60 (53.1%) |
| High school /tech school |
14 (12.4%) |
| College |
2 (1.8%) |
| Occupation Unemployed |
58 (55.2%) |
| Employed |
28 (26.7%) |
| Self-employed |
19 (18.1%) |
| Marital status Not married |
90 (80.4%) |
| Married |
11 (9.8%) |
| Divorced |
11 (9.8%) |
| Children None |
91 (81.3%) |
| One |
20 (17.9%) |
| More than one |
1 (0.9%) |
|
Characteristics of METH use |
|
| Age beginning meth usage |
22.7 ± 6.7 |
| Years of meth use |
2.0 ± 1.4 |
| Dose (g/day) |
0.6 ± 0.6 |
| Frequency (times/week) |
4.8 ± 4.1 |
| Duration of detoxification (months) | 8.7 ± 4.8 |
Based on the criteria of DSM-IV, 101 participants met the diagnosis of METH dependence, and 12 were METH abusers. Subjects with METH dependence had longer durations (z = 2.312, p < 0.05), more frequent use patterns (z=3.742, p <0.001), and larger daily doses (z = 2.730, p <0.01) of METH use, and higher scores of QMU factor 2 (z = 1.976, p < 0.05). No significant differences of QMU factor 1 (z=1.848 p=0.065), QMU total scores (z=1.541, p=0.123), and negative mood states (TMD) (z=1.537, p=0.124) were found between the two groups.
As shown in Figure 1, the craving level for METH and the TMD in 3-month intervals according to the duration that each individual had been enrolled in the program. After combining the neighboring groups with comparable craving levels, Kruskal Wallis tests were performed in subjects at detoxification durations of 1–3 months, 4–9 months, 10–15 months, and more than 15 months. It was found that the QMU total scores were higher in subjects who were abstinent for 4–9 months and 10–15 months (Chi-square =9.26, p <0.05). However, no significant difference was observed in the QMU factor 1, 2 and TMD.
Figure 1.
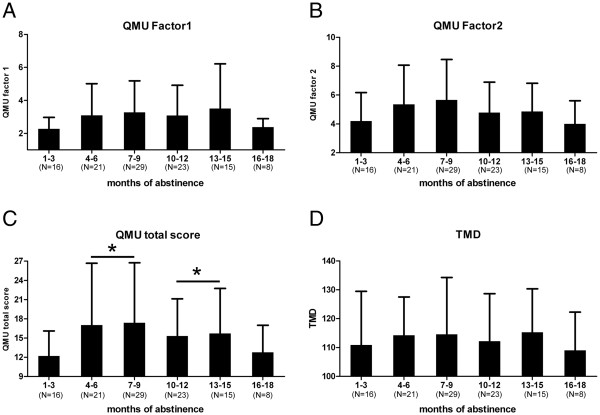
The distribution of QMU scores and negative mood states in the participants following the different durations of abstinence. QMU, Questionnaire of METH-use Urge. Factor 1 addresses “intention/desire to use meth” and factor 2 addresses “anticipation of relief of negative effect/urgent desire to use meth”. TMD: Total Mood Disturbance. *: QMU total scores were higher in subjects who were abstinent for 4–9 months and 10–15 months, compared to those are abstinent for 1–3 months (Kruskal Wallis tests, p<0.05).
Mood distress and former drug use independently affect craving level
Factors related to the increased craving were screened by Spearman coefficient analysis. As shown in Figure 2, significant correlations were found between QMU factors and negative mood states, as well as the weekly METH dose. Other characteristics of the participants, such as age, education level, marital status, work experience, the age of first METH use, and the duration of METH use were not significantly correlated with the current craving level. TMD can be decomposed into five negative mood ingredients including fatigue, bewilderment, anxiety, depression and hostility, minus two positive mood factors of vigor-activity and self-esteem. Statistical analysis showed that all the five negative mood factors, but not the two positive mood factors, were closely related to the QMU score (Table 2).
Figure 2.
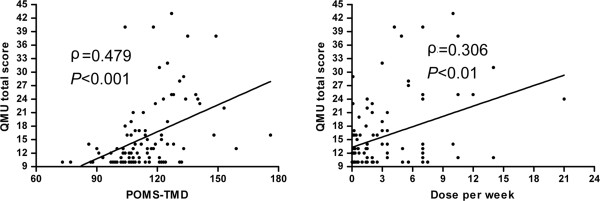
Craving levels were positively correlated to total mood disturbance (left) and the weekly dose of former METH use (right). POMS, Profile of Mood State. TMD, Total Mood Disturbance. QMU, Questionnaire of METH-use Urge.
Table 2.
The Spearman correlation coefficients between ratings of POMS and scores of Questionnaires of METH-use Urge (QMU)
| Spearman coefficients | |||
|---|---|---|---|
|
A-POMS |
QMU factor 1 |
QMU factor 2 |
QMU total score |
| Fatigue |
0.275** |
0.330** |
0.341*** |
| Confusion-bewilderment |
0.236* |
0.332** |
0.342*** |
| Tension-anxiety |
0.291** |
0.382*** |
0.346*** |
| Depression |
0.263** |
0.444*** |
0.391*** |
| Anger-hostility |
0.277** |
0.402*** |
0.404*** |
| Vigor-activity |
−0.028 |
−0.065 |
−0.050 |
| Self-esteem |
−0.046 |
−0.033 |
−0.025 |
| Total mood disturbance (TMD) | 0.355*** | 0.503*** | 0.479*** |
*p< 0.05, **p< 0.01, ***p< 0.001.
Partial correlation analysis (Table 3) was used to determine the independent factors that related to the increased QMU scores. After controlling for overall mood distress, the weekly dose of METH use was significantly related to the total score of QMU and QMU factor 2, but not QMU factor 1. TMD had a significant correlation with QMU scores after controlling for weekly dose, duration of METH dose, or duration of detoxification. Moreover, each of the five negative mood factors including fatigue, bewilderment, anxiety, depression and hostility, were related to all QMU scores (total score of QMU, QMU factor 1 and 2) after controlling for weekly dose of meth.
Table 3.
The Spearman Partial Correlations with Questionnaires of METH-use Urge (QMU) Scores
| Spearman partial coefficients | |||
|---|---|---|---|
| Models |
QMU Factor 1 |
QMU Factor 2 |
QMU Total score |
| 1: Dose per week controlled for TMD |
0.177 |
0.236* |
0.261* |
| 2. Fatigue controlled for weekly dose |
0.260* |
0.314** |
0.326** |
| 3. Confusion controlled for weekly dose |
0.214* |
0.310** |
0.320** |
| 4. Tension-anxiety controlled for weekly dose |
0.268** |
0.359*** |
0.320** |
| 5. Depression controlled for weekly dose |
0.245* |
0.432*** |
0.376*** |
| 6. Anger-hostility controlled for weekly dose |
0.273** |
0.405*** |
0.408*** |
| 7. TMD controlled for dose of meth |
0.331** |
0.481*** |
0.455*** |
| 8. TMD controlled for duration of meth use |
0.330** |
0.493*** |
0.467*** |
| 9. TMD controlled for duration of detoxification |
0.353*** |
0.504*** |
0.477*** |
| 10. 7+8 |
0.314** |
0.477*** |
0.450*** |
| 11. 7+8+9 | 0.314** | 0.479*** | 0.450*** |
*p< 0.05, **p< 0.01, ***p< 0.001.
Discussion
The primary finding of present study was that the craving ratings increased, but the ratings of total mood disturbance did not change following the abstinence in the female METH users. The data demonstrated the impact of mood distress on craving level in female METH users. All of the five ingredients of negative moods, including hostility, depression, anxiety, bewilderment, and fatigue, showed an positive relationship to increased craving level. The weekly dose of METH use was the only one among historical factors that related to METH craving, and the effect of higher-dose METH use history on craving was primarily independent of the present negative mood states.
The present data were consistent with the previous studies that mood distress increases the craving for nicotine [17-21], alcohol [22,23] and heroin [24] in drug abstinence subjects. METH abusers who also have mood problems are more vulnerable to psychiatric diseases. For example, it has been shown that relapse of METH psychosis can be evoked by stress [31,32]. In addition, major depression and suicidal ideation is commonly observed in patients seeking treatment, especially in females [11]. Proper psychosocial therapy can not only lower the degree of craving and drug use [33,34], but also help to prevent relapse and exacerbation of psychiatric diseases [35,36]. The ultimate goal of compulsory detoxification is to prevent relapse among METH users who will be released in 1–3 years. Our results suggest that negative mood distress should be carefully evaluated during the mandatory treatment. Therefore, providing the suitable treatment for the mood disorders should be a key component of the compulsory detoxification program.
Although some literature suggests that craving for METH may greatly decreases within the first two months of abstinence [16], our study implicated a persistence of desire to use the drug, which might be easily promoted by mood disturbance. A progressive elevation of cue-induced craving over an extended period of abstinence was first suggested in 1986 in cocaine users [37]. This phenomenon was lately named as incubation of drug craving, and repeatedly confirmed in rodents with different substances of abuse [38]. In fact, the present data showed the more craving in the female METH users who exposed to the higher doses of METH. Therefore, acquiring a full history of METH use for each individual would be necessary to anticipate the increased METH craving for women enrolled in treatment.
Biological basis of the long lasting craving has been indicated in many studies. For instance, imaging studies have shown reduced dopamine transporter density and reduced dopamine D2 receptors in the stratum [39,40], and reduced glutamate in prefrontal gray matter [41] in abstinent psychostimulant users and non-human primate. These persistent corticolimblic dysregulation can cause increased baseline levels of stress [42] and deficits in inhibitory control [43]. And drug-seeking behavior recurs once drug cue or stressful environment is presented. Meanwhile, the long- term craving has been suggested as a result of the formation of GluA2-lacking AMPARs in the nucleus accumbens [38]. The incubation of craving has also been linked with the increased neuronal activity in the ventral medial prefrontal cortex, nucleus accumbens core, and central amygdale [38]. Taken together, the persistent craving may result from the neural deficits caused by the drugs, as well as neural adaption to the drugs. The detailed mechanisms need to be clarified in further studies.
Environmental context of incarceration may also contribute to the elevated craving. Studies have shown that rodents exhibit enhanced incubation of craving when put in an isolated environment [44] or with the no access of exercise [45]. Similarly, mandatory treatment with subjects isolated from the community may confront the same problem as the experimental animals. Thus, the efficacy of the treatment might be weakened when subjects lived in the relatively close environment. Although the total ratings of mood distress of female METH users did not change following the abstinence in the isolated detoxification Center, introduction of the more activities in a more open environment for female METH users is therefore suggested.
As in all studies, this data should be carefully interpreted. This is a cross-sectional study. Therefore, the data generated from subjects with different duration of compulsory detoxification program may not necessarily represent the time course of mood changes and cravings in individuals in the program. Moreover, our data cannot be applied to describe the time courses of cravings in women who are not in the compulsory detoxification program but remain abstinent from METH. Future longitudinal studies are necessary to understand the course of chronic withdrawal symptoms for each patient as well as patient outcomes once they return to their communities. Additionally, the data collected on the characteristics of drug use, mood state, and craving level are based on participant self-reports, but because patients were guaranteed confidentiality, we concluded that the data are reliable and valid.
Conclusions
This study is the first to demonstrate a correlation between mood distress and craving for METH. It is also the first study that focuses on the isolated compulsory detoxification program in China. Our results call for appropriate psychosocial therapies to offer coping skills and to alleviate mood disorders in women with METH dependence in detoxification treatment.
Endnotes
a. In P.R.China, individuals with records of using illicit drugs in the local police station are registered in the Narcotics Control Bureau of the Ministry of Public Security, and they are called registered drug users. After registration, they are asked to report to the local police office regularly, and underwent the urine test for illicit drugs randomly. If the records of drug use for the individual were clean for three years, then the individual is considered as recovered and is removed from the registration list. The list helps the government to understand the prevalence of drug use, as well as to treat the drug users.
Abbreviations
A-POMS: The Abbreviate Profile of Mood States; ATS: Amphetamine-type stimulant; METH: Methamphetamine; QMU: Questionnaire of Meth-use Urge-belief; TMD: Total mood disturbance.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
WS participated in the interviewing, recorded the data, performed the data analysis, and drafted the manuscript. YL designed the questionnaires, participated in the interviewing, and revised the manuscript. LL helped to design to questionnaires, and participated in interviewing. YZ designed to questionnaires and participated in interviewing. WZ conceived of the study, participated in the coordination and made the final manuscript. All authors read and approved the final manuscript.
Contributor Information
Wenwen Shen, Email: ww-shen@163.com.
Yu Liu, Email: liuyu@nbu.edu.cn.
Longhui Li, Email: llh8630@163.com.
Yisheng Zhang, Email: doctorzhangys@163.com.
Wenhua Zhou, Email: whzhou@vip.163.com.
Acknowledgements
The authors thank Dr. Wei Cui for his comments, and Yongqing Yao for providing interviewing rooms and the access to the participants.
This work was supported by National Key Technology R&D Program in the 12th Five-Year Plan of China (2012BAI01B07), Nature Science Foundation of China (U1132602;81071077) and sponsored by K.C. Wong Magna Fund in Ningbo University.
References
- United Nations Office on Drugs and Crime. World Drug Report 2010. Vienna: United Nations Publications; 2010. [Google Scholar]
- Liu Z, Cao J, Lu X, Mu Y, Lian Z. Epidemiological study of central stimulants and other related psychoactive substance abuse. Chin J Drug Depend. 2002;11:286–293. [Google Scholar]
- Office of the National Narcotics Control Commission. Annual report on drug control in China. Beijing: Ministry of Public Security of China; 2001. [Google Scholar]
- Office of the National Narcotics Control Commission. Annual report on drug control in China. Beijing: Ministry of Public Security of China; 2011. [Google Scholar]
- Brecht ML, O’Brien A, von Mayrhauser C, Anglin MD. Methamphetamine use behaviors and gender differences. Addict Behav. 2004;29:89–106. doi: 10.1016/S0306-4603(03)00082-0. [DOI] [PubMed] [Google Scholar]
- Roth ME, Carroll ME. Sex differences in the acquisition of IV methamphetamine self-administration and subsequent maintenance under a progressive ratio schedule in rats. Psychopharmacology (Berl) 2004;172:443–449. doi: 10.1007/s00213-003-1670-0. [DOI] [PubMed] [Google Scholar]
- Chen HH, Yang YK, Yeh TL, Cherng CF, Hsu HC, Hsiao SY, Yu L. Methamphetamine-induced conditioned place preference is facilitated by estradiol pretreatment in female mice. Chin J Physiol. 2003;46:169–174. [PubMed] [Google Scholar]
- Lin SK, Ball D, Hsiao CC, Chiang YL, Ree SC, Chen CK. Psychiatric comorbidity and gender differences of persons incarcerated for methamphetamine abuse in Taiwan. Psychiatry Clin Neurosci. 2004;58:206–212. doi: 10.1111/j.1440-1819.2003.01218.x. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Zians J, Strathdee SA, Patterson TL. Psychosocial and behavioral correlates of depressed mood among female methamphetamine users. J Psychoactive Drugs. 2007;Suppl 4:353–366. doi: 10.1080/02791072.2007.10399897. [DOI] [PubMed] [Google Scholar]
- King G, Alicata D, Cloak C, Chang L. Psychiatric Symptoms and HPA Axis Function in Adolescent Methamphetamine Users. J Neuroimmune Pharmacol. 2010;5:582–91. doi: 10.1007/s11481-010-9206-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Torok M, McKetin R, Kaye S, Ross J. Patterns of psychological distress related to regular methamphetamine and opioid use. Addiction Res Theor. 2011;19:121–127. doi: 10.3109/16066351003695631. [DOI] [Google Scholar]
- King G, Alicata D, Cloak C, Chang L. Psychiatric symptoms and HPA axis function in adolescent methamphetamine users. J Neuroimmune Pharmacol. 2010;5:582–591. doi: 10.1007/s11481-010-9206-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Liang J, Zhao C, Zhou W. Looking for a solution for drug addiction in China: exploring the challenges and opportunities in the way of China’s new Drug Control Law. Int J Drug Policy. 2010;21:149–154. doi: 10.1016/j.drugpo.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Martin RA, Eaton CA, Monti PM. Cocaine craving as a predictor of treatment attrition and outcomes after residential treatment for cocaine dependence. J Stud Alcohol Drugs. 2007;68:641–648. doi: 10.15288/jsad.2007.68.641. [DOI] [PubMed] [Google Scholar]
- Galloway GP, Singleton EG. How long does craving predict use of methamphetamine? Assessment of use one to seven weeks after the assessment of craving: Craving and ongoing methamphetamine use. Subst Abuse. 2009;1:63–79. [PMC free article] [PubMed] [Google Scholar]
- 3rd Urschel HC, Hanselka LL, Gromov I, White L, Baron M. Open-label study of a proprietary treatment program targeting type A gamma-aminobutyric acid receptor dysregulation in methamphetamine dependence. Mayo Clin Proc. 2007;82:1170–1178. doi: 10.4065/82.10.1170. [DOI] [PubMed] [Google Scholar]
- Cordovil De Sousa Uva M, Luminet O, Cortesi M, Constant E, Derely M, De Timary P. Distinct effects of protracted withdrawal on affect, craving, selective attention and executive functions among alcohol-dependent patients. Alcohol Alcohol. 2010;45:241–246. doi: 10.1093/alcalc/agq012. [DOI] [PubMed] [Google Scholar]
- Fucito LM, Juliano LM. Depression moderates smoking behavior in response to a sad mood induction. Psychol Addict Behav. 2009;23:546–551. doi: 10.1037/a0016529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter BL, Lam CY, Robinson JD, Paris MM, Waters AJ, Wetter DW, Cinciripini PM. Real-time craving and mood assessments before and after smoking. Nicotine Tob Res. 2008;10:1165–1169. doi: 10.1080/14622200802163084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blalock JA, Robinson JD, Wetter DW, Schreindorfer LS, Cinciripini PM. Nicotine withdrawal in smokers with current depressive disorders undergoing intensive smoking cessation treatment. Psychol Addict Behav. 2008;22:122–128. doi: 10.1037/0893-164X.22.1.122. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Carr SB, Bongard S. Anger and psychobiological changes during smoking abstinence and in response to acute stress: prediction of smoking relapse. Int J Psychophysiol. 2007;66:109–115. doi: 10.1016/j.ijpsycho.2007.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz KM. Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology. 2009;34:1198–1208. doi: 10.1038/npp.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Castro V, Fong T, Rosenthal RJ, Tavares H. A comparison of craving and emotional states between pathological gamblers and alcoholics. Addict Behav. 2007;32:1555–1564. doi: 10.1016/j.addbeh.2006.11.014. [DOI] [PubMed] [Google Scholar]
- Epstein DH, Willner-Reid J, Vahabzadeh M, Mezghanni M, Lin JL, Preston KL. Real-time electronic diary reports of cue exposure and mood in the hours before cocaine and heroin craving and use. Arch Gen Psychiatry. 2009;66:88–94. doi: 10.1001/archgenpsychiatry.2008.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toll BA, Katulak NA, McKee SA. Investigating the factor structure of the Questionnaire on Smoking Urges-Brief (QSU-Brief) Addict Behav. 2006;31:1231–1239. doi: 10.1016/j.addbeh.2005.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Sun HQ, Bao YP, Li SX, Beveridge TJ, Di XL, Yang FD, Lu L. Subjective, cognitive/psychomotor, and physiological effects of aripiprazole in Chinese light and heavy smokers. Drug Alcohol Depend. 2009;101:42–52. doi: 10.1016/j.drugalcdep.2008.10.024. [DOI] [PubMed] [Google Scholar]
- Grove JR, Prapavessie H. Preliminary evidence for the reliability and validity of an abbreviated Profile of Mood States. Int J Sport Psychol. 1992;23:93–109. [Google Scholar]
- Zhu BL. Brief introduction of POMS scale and its model for China. Journal of Tianjin University of Sport. 1995;10:35–37. [Google Scholar]
- Cranford JA, Shrout PE, Iida M, Rafaeli E, Yip T, Bolger N. A procedure for evaluating sensitivity to within-person change: can mood measures in diary studies detect change reliably? Pers Soc Psychol Bull. 2006;32:917–929. doi: 10.1177/0146167206287721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyenhuis DL, Yamamoto C, Luchetta T, Terrien A, Parmentier A. Adult and geriatric normative data and validation of the profile of mood states. J Clin Psychol. 1999;55:79–86. doi: 10.1002/(SICI)1097-4679(199901)55:1<79::AID-JCLP8>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Yui K, Goto K, Ikemoto S, Nishijima K, Yoshino T, Ishiguro T. Susceptibility to subsequent episodes of spontaneous recurrence of methamphetamine psychosis. Drug Alcohol Depend. 2001;64:133–142. doi: 10.1016/S0376-8716(00)00240-4. [DOI] [PubMed] [Google Scholar]
- Yui K, Goto K, Ikemoto S, Ishiguro T. Stress induced spontaneous recurrence of methamphetamine psychosis: the relation between stressful experiences and sensitivity to stress. Drug Alcohol Depend. 2000;58:67–75. doi: 10.1016/S0376-8716(99)00060-5. [DOI] [PubMed] [Google Scholar]
- Grasing K, Mathur D, Desouza C. Written emotional expression during recovery from cocaine dependence: group and individual differences in craving intensity. Subst Use Misuse. 2010;45:1201–1215. doi: 10.3109/10826080903474003. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol. 2010;78:362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C, Wolff J, Uhl K. Cognitive-behavioral therapy for adolescent depression and suicidality. Child Adolesc Psychiatr Clin N Am. 2011;20:191–204. doi: 10.1016/j.chc.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penn DL, Mueser KT, Tarrier N, Gloege A, Cather C, Serrano D, Otto MW. Supportive therapy for schizophrenia: possible mechanisms and implications for adjunctive psychosocial treatments. Schizophr Bull. 2004;30:101–112. doi: 10.1093/oxfordjournals.schbul.a007055. [DOI] [PubMed] [Google Scholar]
- Gawin FH, Kleber HD. Abstinence symptomatology and psychiatric diagnosis in cocaine abusers. Clinical observations. Arch Gen Psychiatry. 1986;43:107–113. doi: 10.1001/archpsyc.1986.01800020013003. [DOI] [PubMed] [Google Scholar]
- Pickens CL, Airavaara M, Theberge F, Fanous S, Hope BT, Shaham Y. Neurobiology of the incubation of drug craving. Trends Neurosci. 2011;34:411–420. doi: 10.1016/j.tins.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nader MA, Daunais JB, Moore T, Nader SH, Moore RJ, Smith HR, Friedman DP, Porrino LJ. Effects of cocaine self-administration on striatal dopamine systems in rhesus monkeys: initial and chronic exposure. Neuropsychopharmacology. 2002;27:35–46. doi: 10.1016/S0893-133X(01)00427-4. [DOI] [PubMed] [Google Scholar]
- Chang L, Alicata D, Ernst T, Volkow N. Structural and metabolic brain changes in the striatum associated with methamphetamine abuse. Addiction. 2007;102(Suppl 1):16–32. doi: 10.1111/j.1360-0443.2006.01782.x. [DOI] [PubMed] [Google Scholar]
- Ernst T, Chang L. Adaptation of brain glutamate plus glutamine during abstinence from chronic methamphetamine use. J Neuroimmune Pharmacol. 2008;3:165–172. doi: 10.1007/s11481-008-9108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164:1149–1159. doi: 10.1176/appi.ajp.2007.05030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicy K, London ED. Corticolimbic dysregulation and chronic methamphetamine abuse. Addiction. 2007;102(Suppl 1):5–15. doi: 10.1111/j.1360-0443.2006.01777.x. [DOI] [PubMed] [Google Scholar]
- Chauvet C, Lardeux V, Goldberg SR, Jaber M, Solinas M. Environmental enrichment reduces cocaine seeking and reinstatement induced by cues and stress but not by cocaine. Neuropsychopharmacology. 2009;34:2767–2778. doi: 10.1038/npp.2009.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch WJ, Piehl KB, Acosta G, Peterson AB, Hemby SE. Aerobic exercise attenuates reinstatement of cocaine-seeking behavior and associated neuroadaptations in the prefrontal cortex. Biol Psychiatry. 2010;68:774–777. doi: 10.1016/j.biopsych.2010.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]


