Abstract
When I heard about the concept of immunotherapeutics, I immediately loved it. Everything I had learned about medicine, cancer biology, genetics and oncology indicated to me that this was a potent approach, and at the time, completely untapped. I figured that since we had been unable to cure most metastatic solid tumors, something completely different needed to be employed. Realistically, “magic bullets” are not easy to find and therefore something that can be combined with other therapies, for enhanced synergy without overlapping adverse events, would be appealing.
Keywords: adenovirus, cancer, gene therapy, immunotherapy, oncolytic virus
Oncolytic viruses kill cancer cells by replicating in them. Normal cells are spared since the virus is modified so that the virus doesn’t amplify in them. Oncolysis is highly immunogenic and in fact results in a personalized cancer vaccine for each patient. I love the pragmatism of thisapproach: whichever epitopes (features of the tumor cell) are most relevant immunologically for each tumor, will be released by oncolysis. For immunity, as opposed to tolerance, a “danger signal” is important, and adenoviral oncolysis excels in this regard.
How did I get involved in cancer research ? I still remember the moment in the second year of medical school when I realized that the biggest unmet clinical need in medicine is metastatic cancer. I’m an incurable passionate optimist and a sucker for good-versus-evil stories. Cancer is the most devious imaginable enemy and oncolytic viruses the unlikely young hero from out of town. The hero struggles initially but eventually comes of age and wins the day. Along the way there are epic battles, love-and-loss, betrayal, even despair. I guess I had been searching for a mission and now I had discovered it. Initially, I thought understanding cancer genetics would be key for curing the disease and therefore that was what I did for my PhD. However, I realized that genetics was only a first step, and that it needed to be applied in a more pragmatic approach to help patients.
My plan became to use oncolytic viruses to cure cancer. Maybe not every patient but at least some. Later on I came up with a more concrete goal: since we can’t eradicate cancer as a disease, as it is a side effect of evolution (mutations in genes allow evolution, and they can also give rise to cancer), and since all of us must die one day, lets at least try to make sure no one under 65 dies of cancer. I realized this was unrealistic but perhaps having an ambitious goal would allow some concrete, if more modest, actual steps forward.
After completing medical school and a concurrent PhD, and recuperating from the associated burnout, I was ready for the next step. I considered my post-doc group carefully and decided on David Curiel’s group in Birmingham, Alabama. I liked his focus on adenovirus, which I thought was the most promising cancer gene therapy agent, and the fact that there were about 80 people there, giving critical mass and indicating sufficient funding. Also, Birmingham is a great city for a lover of music, food and the outdoors.
Since my goal was taking the approach to humans, the fact that there were trials ongoing there was intriguing. However, I would learn that trials are in fact incredibly difficult to make happen. To a lay-man it seems obvious that if there is an unmet clinical need, and a promising technology, it should be taken from the laboratory to patients. There is little point in preclinical research unless it leads to clinical application. Regulatory bodies are sometimes blamed for thwarting progress but this seems a bit unfair since they are just doing what we as society have mandate them with. Nevertheless, at the same time we are unhappy with both the slowness of clinical translation and the cost of new drugs. As if it weren’t logical that the more expensive and slow each trial is, the costs will have to be compensated in the prices of the few drugs that make it through all trial phases into products. Pharmaceutical companies are viewed as greedy but at the same time regulation has made sure that only companies can do trials. This is painfully obvious in the EU where the clinical trials directive was written by the “Enterprise and Industry” directorate of the Commission, instead of for example “Health and Consumers” or “Research and Innovation”.
In Birmingham we made swift progress in building and analyzing a new generation of oncolytic adenoviruses in the laboratory. There is a wonderful National Cancer Institute (NCI) mechanism which funds for the Good Manufacturing Practices (GMP) quality production, toxicity and biodistribution testing of novel therapeutics. We were fortunate to obtain several of these awards while in Birmingham and eventually three clinical trials resulted.
After 3 years in the US, I was becoming almost more American than Finnish so I had to make a choice. At the time Finland was a great country to do trials, but I also wanted to give clinical work a try since I had realized that to make a real clinical impact, I had to have a specialty. In Finland I could get both medical and radiation oncology in a combined specialty in five years. Thus, I moved back and embarked on specialization, while at the same time setting up my laboratory at the University.
We were doing preclinical work but all the time the goal was getting into humans. Unfortunately, clinical translation became significantly more difficult with the EU clinical trials directive (2001/20/EC) in 2004. The directive attempted to harmonize trial regulations by raising the bar throughout, so that all trials now had the same requirements as multicenter transnational phase 3 trials. While this might sound like a good idea, it made academic, investigator initiated early-stage trials practically impossible, especially when they involved new treatment agents. With regard to oncolytic viruses, production became a nearly unsurmountable obstacle since industrial manufacturing was required even for phase 1 trials. Since preclinical models are poorly predictive (“useless”, a sceptic would say) of patient data for many human-specific agents including oncolytic adenoviruses, fast development would require a flexible bench-to-bedside-and-back process, which is not possible if every trial needs to employ and industrial production process.
The tightened regulatory environment became excruciatingly clear when I tried to get an oncolytic vaccinia virus trial approved in Finland in 2005. The product had already been approved by the US FDA for phase 1 trials but the Finnish FDA (currently known as FIMEA) did not think production quality was sufficient and after 2 years of discussions they gave a final rejection.
The NCI mechanism that we had employed in the US is not restricted to American investigators and I was able to get a virus produced for a trial in Finland. However, it became clear that the production level applied in the US for phase 1 academic trials (some people call it “GMP light”) would not be sufficient in Finland. The FDA (but not FIMEA) differentiates between trials likely to be part of the bench-to-bedside-and-back process and industry trials which usually aim at proceeding to phase 3 trials. With regard to the former, developing an industrial production process would be prohibitively expensive, while for the latter having this in place early on can help the company proceed faster.
It is unfortunate how rarely patients are considered in discussions about clinical trial rules. Regulators view trials as something which is in the interest of companies while researchers are interested in meticulously forwarding the science. However, patients with incurable disease would need something today, not after ten years. The fewer trials are out there, the fewer patients have access to experimental therapeutics.
Although our NCI award covered the most expensive aspects of a phase 1 trial, it did not cover the actual treatments, since in the US clinicians are often able to get NIH grants for trials. However, in Finland no such mechanisms exist and I was only able to collect about 10% of the required amount through Finnish grants. In one EU application a reviewer pointed out that it would be a waste of money to fund a trial since they are within the realm of companies.
Through my frequent interactions with regulators I learned of the Advanced therapies directive (EC/1394/2007), which defines the “hospital exemption”, allowing, or even encouraging, individualized patient-by-patient treatment with gene therapy and stem cells. In essence the exemption determines that patients can be treated outside of clinical trials under the sole responsibility of the physician. Nevertheless, national bodies are required to oversee these treatments by regulating production and by requiring adverse event reporting. I started discussing with authorities, lawyers and ethics bodies the possibility of treating patients in what we called the Advanced Therapy Access Program (ATAP). In fact the approach was initially suggested by a department chief at FIMEA, who pointed out that the World Medical Association Declaration of Helsinki (the globally accepted ethical framework for clinical research) article 35 basically requires physicians to look beyond routine therapies when the patient’s disease cannot be cured with available modalities.
We set up a production suite at the University and the first patient was treated in November 2007. Having established safety with the first virus, we next moved to enhance efficacy. It had become evident that pure oncolysis was unlikely to eradicate advanced tumor because of intratumoral complexities such as high pressure, necrotic areas and non-tumoral (stromal) areas within tumors, all of which would compromise intratumoral viral dissemination. One way to overcome this is arming of the virus with an immunostimulatory molecule; an immune response against the tumor would help in eradicating non-infected malignant cells both locally and also at metastatic sites. I knew enough of immunology to figure that adenovirus was a perfect immunological agent due to its innate immunogenicity and co-stimulatory activity.
The first virus in this family coded for granulocyte-macrophage colony stimulating factor (GMCSF) which had been effective in cancer vaccine studies. The virus proved to be safe and there were several striking examples of efficacy, including complete disappearance of all disease in some patients. Another transgene we employed was CD40L, a molecule which has several properties appealing for cancer immunotherapy. This virus also provided a striking example of the power of ATAP in full swing. It took a mere 10 months from the day when we started making the virus to the first patient treated.
One of the most useful aspects of ATAP was the rapid learning curve. If we learned something important in a patient or at a scientific meeting, we could apply this knowledge with the very next patient. ATAP had begun as an academic endeavor but the University wasn’t actually too happy about it. Many colleagues felt that production, patient treatments and clinical research should not be done at the University. Also, with the safety and efficacy data mounting in ATAP, it was becoming clear that we needed to move to clinical trials. ATAP is in no way a replacement for trials and only through the latter can we gain formal evidence of safety and efficacy, and only through developing a product can we give a larger number of patients access to the technology.
Based on my earlier experiences, I knew for a fact that a trial could not be done in Finland with public money and thus the only solution was companies. For corporations to have an interest, the intellectual property needs to be protected, so that they can get their money back in case their investment proves successful. With this in mind we submitted our first patent in 2005 and tried to get companies interested but without success. I was told by many people that I should found my own company. I had nothing against that except that one person’s resources are limited, regardless of how hard he works, and therefore I needed a partner. Eventually, Pekka Simula was suggested by a mutual friend, resulting in plans for Oncos Therapeutics Ltd being drawn up rapidly. Oncos raised 4 million euros from HealthCap in 2010 and the Finnish government matched it through TEKES. This may seem like a lot of money but in fact is barely sufficient to treat about 20 patients in phase 1 trials.
ATAP was transferred from the University to Oncos but its end was already nearing. The Directive that had inspired ATAP was finally integrated into Finnish law and FIMEA regulations. Production requirements were discussed in the Social Affairs and Health Committee in Finnish parliament, as the directive in fact makes a clear distinction between industrial and non-industrial production. Patients had heard about the possible impact of full GMP on ATAP and they had collected 8,000 names in a petition to keep the treatments going. There were several programs on TV featuring patients who had benefited from ATAP. The committee asked to see me and I gave them a short presentation flowed by lively discussion.
Oncos and FIMEA communicated closely for a production license but eventually no virus was produced according to the new standard as the amount of money spent subventing treatments would simply not justify the information gained. Oncos is a small company and all of its resources were needed for getting clinical trials started. For a while we were able to use our earlier production lots but this temporary permission ended in Spring 2012. Keeping in mind that we had been using 10 different viruses, and the whole idea in ATAP was personalized therapy, production of a single lot of virus would not have allowed ATAP to continue. Also, it can be discussed how many patients can be treated with one virus under the hospital exemption for it to still remain patient-by-patient. Thus, oncolytic viruses and other forms of viral gene therapy may not be compatible with the exemption unless production requirements can be relaxed.
Thus, in Spring 2012 ATAP was closed but three clinical trials had been initiated by Oncos. My own future prospects probably involve a need to make some choices. Running the research group, helping Oncos set up trials, seeing patients and trying to be a father to three children is clearly too many things. If I knew which one of my three jobs is the best way to help the young hero to beat the enemy, I would surely choose that path. (Fig. 1)
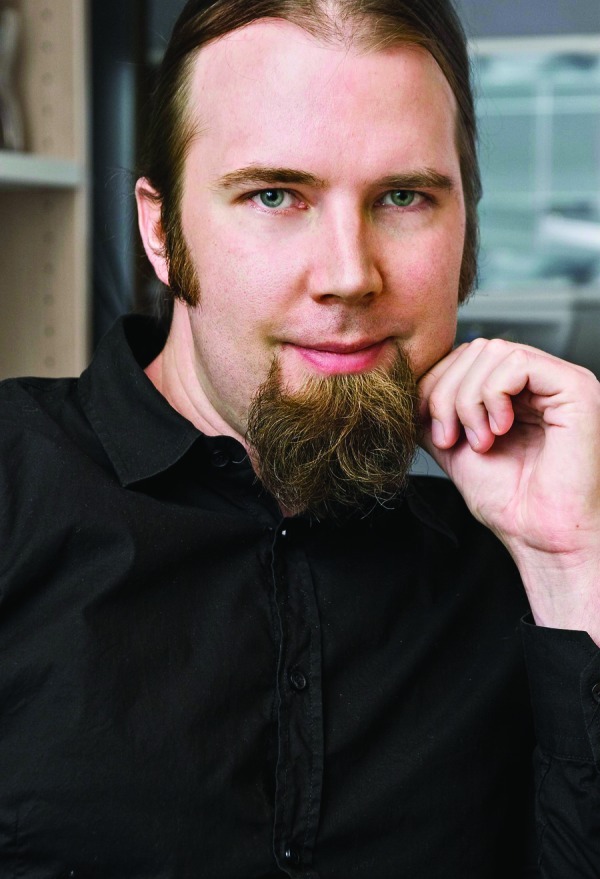
Figure 1. About Dr Hemminki: Dr Akseli Eetu Hemminki studied Medicine and Medical Science at the University of Helsinki (Finland), where he completed his MD and PhD in 1999. He performed postdoctoral studies at the Department of Genetics at the University of Helsinki and in the Division of Human Gene Therapy at the University of Alabama at Birmingham (AL, USA), where he held positions as Research Assistant Professor, Director of Clinical Trials and Group Leader of Ovarian Cancer in the Division of Human Gene Therapy. In 2002 Dr. Hemminki returned to Finland as Group Leader of the Cancer Gene Therapy Group at the University of Helsinki, a position he still holds. He is also Docent of Cancer Biology and University Lecturer at the Haartman Institute at Helsinki University, as well as K Albin Johansson Research Professor at the Finnish Cancer Institute. In 2007 he completed the oncology specialization program at the University of Helsinki. Besides his research, Dr Hemminki has been working as senior physician at Helsinki University Central Hospital and Oncologist at International Cancer Center Docrates, Helsinki. Dr Hemminki is an active member of many professional societies and a regular speaker at national and international conferences in the fields of oncology and cancer immunotherapy. His research resulted in over 180 publications in peer-reviewed scientific journals, ten scientific books and book chapters, and several patents on viral vectors for immunotherapy. The research of the world-class Cancer Gene Therapy Group, headed by Dr Hemminki, was also the basis for his cofounding the biotech company Oncos Therapeutics in 2008. The company develops novel cancer immunotherapies and was awarded the BioFinland prize from Finnish Bioindustries in 2011. In addition, Dr Hemminki has received numerous awards and honors such as the Outstanding Young Investigator Award of the American Society of Gene Therapy in 2007 or the American Society of Clinical Oncology career development award in 2010.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/21699


