Abstract
Jumping and cutting activities are investigated in many laboratories attempting to better understand the biomechanics associated with non-contact ACL injury. Optical motion capture is widely used; however, it is subject to soft tissue artifact (STA). Biplanar videoradiography offers a unique approach to collecting skeletal motion without STA. The goal of this study was to compare how STA affects the six-degree-of-freedom motion of the femur and tibia during a jump-cut maneuver associated with non-contact ACL injury. Ten volunteers performed a jump-cut maneuver while their landing leg was imaged using optical motion capture (OMC) and biplanar videoradiography. The within-bone motion differences were compared using anatomical coordinate systems for the femur and tibia, respectively. The knee joint kinematic measurements were compared during two periods: before and after ground contact. Over the entire activity, the within-bone motion differences between the two motion capture techniques were significantly lower for the tibia than the femur for two of the rotational axes (flexion/extension, internal/external) and the origin. The OMC and biplanar videoradiography knee joint kinematics were in best agreement before landing. Kinematic deviations between the two techniques increased significantly after contact. This study provides information on the kinematic discrepancies between OMC and biplanar videoradiography that can be used to optimize methods employing both technologies for studying dynamic in vivo knee kinematics and kinetics during a jump-cut maneuver.
Keywords: knee, biomechanics, soft tissue artifact, x-ray, in vivo
1. Introduction
Activities involving jumping, landing, and cutting are commonly associated with non-contact anterior cruciate ligament (ACL) injuries (Griffin et al., 2006; Gianotti et al., 2009). Non-contact ACL injuries are those sustained without contact with another athlete. They account for ~70% of the estimated 400,000 ACL injuries sustained in the United States each year (McNair et al., 1990; Junkin et al., 2009). The mechanisms associated with non-contact ACL injury are not well understood and most likely occur from a combination of risk factors including environmental, anatomical, hormonal, and biomechanical (Griffin et al., 2006). Understanding the biomechanics of activities associated with non-contact ACL injury would provide insight into injury mechanisms and may provide evidence in support of specialized training and rehabilitation techniques to minimize injury and optimize treatment (McNair et al., 1990; Boden et al., 2000).
Optical motion capture (OMC) technologies have been used to non-invasively quantify 3-D joint kinematics, including jumping and cutting (Ford et al., 2005). The field-of-view (FOV) of OMC systems is large enough to capture the motion of multiple joints over an entire jumping and cutting movement. When combined with ground reaction forces and a biomechanical model, OMC is a powerful tool for providing insight into the biomechanics of the knee during these high speed maneuvers.
However, OMC is sensitive to soft tissue artifact (STA), where motion of skin mounted markers move relative to the underlying bones, particularly during the landing and support phases of a movement (Cappozzo et al., 1996; Reinschmidt, van den Bogert, et al., 1997). STA limits the accuracy of joint metrics at the level of the ligaments and articulating surfaces. Cluster based motion capture techniques have been developed to mitigate the effect of STA (Andriacchi et al., 1998). While these techniques improve segment tracking they do not eliminate STA. Attempts to eliminate STA using percutaneous bone fixtures have been successful; however, these methods are highly invasive and likely alter joint motion, especially during jumping and cutting maneuvers (Lafortune et al., 1992; Cappozzo et al., 1996; Holden et al., 1997). Elucidating how joint arthrokinematics (e.g. joint translation, joint space, contact regions) may contribute to a sports injury remains challenging without an accurate, non-invasive method for understanding the bone-bone kinematics during landing and cutting.
High-speed biplanar videoradiography motion capture techniques allow investigators to accurately quantify 3-D bone motion during dynamic activities without STA (Tashman and Anderst, 2003; Brainerd et al., 2010; Miranda et al., 2011; Torry et al., 2011). Currently, biplanar videoradiography systems are capable of capturing 3-D kinematics of a single joint within a basketball sized FOV. It would be advantageous to capture an entire jump-cut maneuver with OMC while using biplanar videoradiography to focus on knee joint kinematics at the level of the articulating surfaces during impact with the ground. This would provide highly accurate bone kinematics during an important phase of the maneuver while quantifying the kinematics of the surrounding joints throughout the entire movement.
Recently, Myers et al. (2011) and Taylor et al. (2011) make use of both biplanar videoradiography and OMC to study tibiofemoral kinematics during drop and jump landings. While these studies provide a foundation for combining the two motion capture techniques, comparing the respective kinematic outcomes was beyond their scope. Understanding how STA affects each body segment (e.g. thigh and shank) during different periods of an activity will strengthen the interpretation of kinematic outcomes associated with high demand activities. Moreover, by better understanding the limitations of a combined technique, kinetic outcomes may be estimated by effectively expanding the FOV using OMC. In order to optimize a combined OMC and biplanar videoradiography technique, their measurement differences during landing activities (i.e. those which are more susceptible to STA) must be quantified.
The goal of this study was to compare how STA affects the six-degree-of-freedom motion of the femur and tibia during a jump-cut maneuver. For this assessment, we (1) quantified the within-bone motion differences as measured by OMC and biplanar videoradiography; and (2) evaluated how these within-bone motion differences affected the clinically relevant knee joint kinematics (tibia with respect to the femur) before and after ground contact. It has previously been shown that soft tissue surrounding the femur affects kinematic measurements more significantly than the soft tissue surrounding the tibia during knee flexion, axial hip rotation, and stair-ascent (Garling et al., 2007; Akbarshahi et al., 2010; Tsai et al., 2011). Additionally, Garling et al. has reported an increase in STA after ground contact during stair-ascent (2007). Based on these data, we hypothesized that the soft tissue surrounding the femur would have a greater effect on the kinematic measurements than the soft tissue surrounding the tibia during the jump-cut maneuver. Moreover, we hypothesized that STA would significantly influence the OMC joint kinematic measurements after ground contact during the jump-cut maneuver when compared to the biplanar videoradiography measurements.
2. Methods
2.1 Subjects
All experimental procedures were approved by the Institutional Review Board. Ten recreational athletes (5 males, 5 females; age 25±3.3years; height 1.73±0.10m; weight 73.17±10.15kg) were enrolled in this study. The inclusion criteria were: (1) no neurological disease(s); (2) no pregnancy; (3) no history of lower extremity injury; and (4) a Tegner activity score of five or greater (Tegner and Lysholm, 1985). After granting their informed consent, each subject was outfitted with two marker clusters containing five retro-reflective markers. These marker clusters were placed on the thigh and shank to track the six degree-of-freedom motions of the femur and tibia using OMC. This marker set was chosen because it is a subset of a larger marker set commonly used to track segment motion using OMC (Buczek et al., 2010). The outfitted leg was chosen randomly (6L and 4R).
2.2 Jump-Cut Maneuver
Volunteers performed a jump-cut maneuver, originally described by Ford et al, that was designed to mimic maneuvers associated with non-contact ACL injury (Ford et al., 2005). Three targets were placed on the floor within the testing environment: a jump-landing target on the center of the force plate and two targets placed two meters beyond the jump-landing target at an angle of ~45°. These two targets provided a reference for the subject to cut toward and jog past after landing. Before beginning the maneuver, the subject was asked to stand approximately one meter from the force plate with their knees bent at ~45°. A verbal prompt was used to cue the subject to jump upward and forward toward the landing target. A visual directional prompt (L or R) cued the subject to perform a sidestep cut toward and jog past one of the angled targets. For example, when a subject began their jump and were signaled to cut to the left, they landed and pushed off with their right foot and led with their left (Figure 1A). Ten trials (five in each direction) were performed. The subject was unaware of the directional prompt prior to each trial.
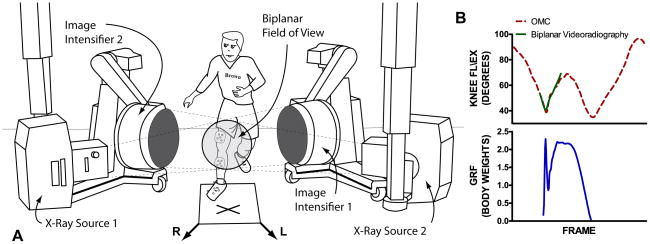
Figure 1.
A, experimental set-up including image intensifiers and x-ray sources. The optical motion capture cameras are not shown. The subject is performing the jump-cut maneuver. In this example they were cued to cut to their left upon landing on the force plate. The ‘X’ marks the landing location and the arrows represent the left (L) and right (R) cut directions. B, the OMC (dotted red) and biplanar videoradiography (solid green) knee flexion/extension and GRF (solid blue) for the entire jump-cut activity including the flight phase, landing, rotation, cut, and toe-off. The field of view for the biplanar videoradiography limits its ability to collect kinematic data for the entire jump-cut activity. However, it can be tailored to measure motion for specific periods of an activity where OMC is more sensitive to soft tissue artifact.
2.3 Data Collection and Processing
All biomechanical data were collected in the W.M. Keck Foundation X-Ray Reconstruction of Moving Morphology (XROMM) Facility at Brown University, (www.xromm.org). OMC data was collected at 250Hz using a 4 camera Qualisys Oqus 5-series system (Gothenburg, Sweden). GRF data were time-synchronized with the OMC system and collected at 5,000Hz using a Kistler model 9281B force plate (Amherst, NY).
Biplanar videoradiography data were time-synchronized with the OMC system using an electrical trigger and collected at 250Hz during three of the jump-cut trials where the subject landed and cut with their outfitted leg. The biplanar videoradiography system has been previously described in detail (Miranda et al., 2011). X-rays were generated using an exposure of 70kVp and 100mA. Digital radiographs were captured using shutter speeds of 400–800μs. The x-ray sources were positioned at 120° with a source to image distance of 165cm. Image de-distortion and 3-D space calibration (XrayProject; http://www.xromm.org) was performed using previously described methods (Brainerd et al., 2010).
Clinical CT scans (Lightspeed; GE, Piscataway, NJ) for each subject’s outfitted knee were acquired in the axial plane at 80kVp, using GE’s SMART mA and Bone Plus reconstruction algorithm. The voxel resolution was <0.381×0.381×0.625mm3. For each scan, the femur and tibia were isolated from the entire volume using threshold and segmentation tools available in Mimics v14 (Materialise, Ann Arbor, MI).
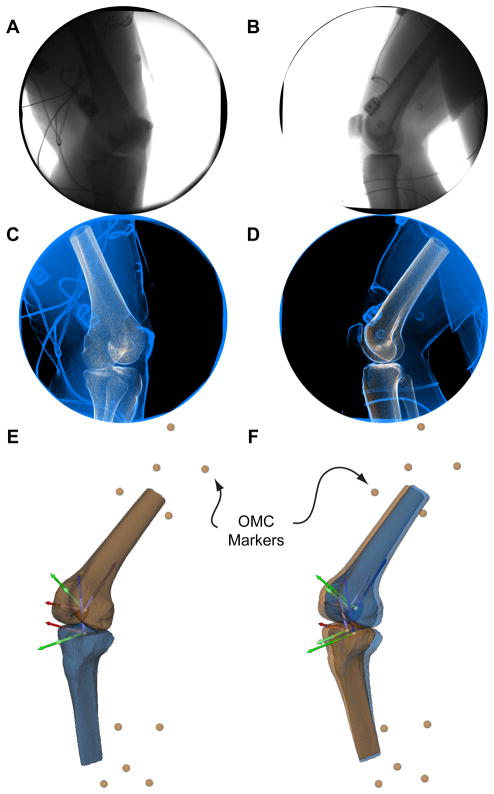
The biplanar videoradiography data were processed using custom markerless tracking software (Autoscoper; http://www.xromm.org) detailed previously (Miranda et al., 2011). Briefly, the CT volumes for the femur and tibia were registered with the biplanar videoradiography data and the bones were tracked across all captured frames using the Autoscoper software (Figure 2A–D). These techniques track in vivo bone motion within 0.25mm and 0.25° (Miranda et al., 2011). The knee joint kinematics of the tibia with respect to the femur were described using a pair of anatomical coordinate systems (ACSs) created from the 3-D CT bone models of the femur and tibia using previously described methods (Figure 2E) (Miranda et al., 2010). This pair of ACSs was used to interpret knee joint kinematics for both OMC and biplanar videoradiography.
Figure 2.
Panels A and B represent a single frame of the biplanar videoradiography data for source 1 and 2, respectively. Panels C and D represent the same frame of the biplanar videoradiography data (blue) after image processing. Contrast and edge detection is used to enhance the images. Additionally, the digitally reconstructed radiographs generated from the CT volume are displayed in tan and are superimposed on the blue and black biplanar videoradiography data. The images represent the outcome of the Autoscoper software after bone tracking is completed for the current frame. The 3-D models of the tibia and femur driven by optical motion capture (tan) and biplanar motion capture (blue) are shown in panels E and F. All four independently tracked anatomical coordinate systems are also shown. The short and lighter coordinate systems are being driven by OMC and the long and darker coordinate systems are being driven by biplanar videoradiography. The external markers for the thigh and shank are also shown in tan. Panel E represents the initial frame, where OMC and biplanar videoradiography are perfectly aligned. Panel F represents a frame where soft tissue artifact is affecting the OMC driven bones and coordinate systems.
In order to use the same ACSs for both imaging modalities, the global coordinate spaces of the OMC and biplanar videoradiography systems were registered using a rigid lattice that consisted of 11 radio-opaque, spherical markers outfitted with retroreflective tape (3M, St. Paul, MN). The OMC and biplanar videoradiography systems simultaneously captured a static position of the lattice and the transformation matrix for co-registration of each global coordinate space was computed (Söderkvist and Wedin, 1993; Challis, 1995) and applied to the respective kinematic data sets.
2.3 Data Analysis
In order to compare the within-bone motion differences, the CT-based ACSs were independently driven by the OMC and biplanar videoradiography systems. This resulted in the motion of the CT-based femoral and tibial ACSs as determined by the biplanar videoradiography system and as determined by the OMC system (Figure 2F). The biplanar videoradiography ACSs were compared to the OMC ACSs by determining the axes (Rx, Ry, and Rz) and origin (T) differences at each frame. The range (max-min) of axes and origin differences were calculated for each trial across all subjects and these data were described using sample means and standard deviations. The range differences of the femoral ACS were compared to the range differences of the tibial ACS using a paired t-test. Additionally, the overall median and maximum range differences of the femoral and tibial ACSs were computed for all subject trials.
Knee joint kinematics were compared for each trial across all subjects using both sets of ACSs. Joint rotations in flexion/extension (FL/EX), adduction/abduction (AD/AB), and internal/external (IN/EX) rotations of the tibia relative to the femur were interpreted using Grood and Suntay’s method (1983). Joint translations in medial/lateral (ME/LA), anterior/posterior (AN/PO), and compression/distraction (CO/DI) displacements of the tibia relative to the femur were determined by a vector originating at the origin of the femoral ACS and terminating at the origin of the tibial ACS (Deneweth et al., 2010). All kinematic measurements were processed using Visual3D (C-Motion; Germantown, MD).
The joint rotations and translations were separated into two periods: (A) flight phase to contact, and (B) following contact. Period A began and period B ended when the femur and tibia entered and exited the FOV of the biplanar videoradiography system. For each period, the differences in kinematic excursions (max-min) between OMC and biplanar videoradiography were calculated for each trial. The absolute differences in kinematic excursions were described using sample means and standard deviations. A paired t-test was used to determine if the differences in values among periods A and B were greater than would be expected by chance. Additionally, the overall median and maximum differences in knee joint rotational and translational excursions were computed for both periods across all subject trials.
3. Results
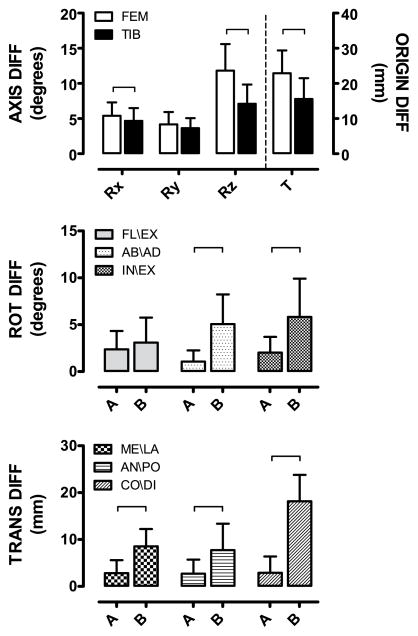
The ranges of femoral ACS axes (Rx, Ry, Rz) and origin (T) differences between OMC and biplanar videoradiography were higher than the range of tibial ACS axes and origin differences (Figure 3 Top). The ranges of femoral differences were only significantly higher for Rx, Rz, and T; however, the p-value for Ry was 0.19. The maximum range of axes differences for the femoral and tibial ACSs were as high as 18° and 13°, respectively (Table 1). The maximum range of origin differences for the femoral and tibial ACSs were as high as 34mm and 29mm, respectively (Table 1).
Figure 3.
Top, the difference between OMC and biplanar videoradiography for the three rotational axes (Rx, Ry, and Rz) and origin (T) of the independently driven femoral and tibial ACSs. Middle, the rotation difference (FL\EX, AB\AD, IN\EX) between OMC and biplanar videoradiography. Bottom, the translational difference (ME\LA, AN\PO, CO\DI) between OMC and biplanar videoradiography. For all knee joint rotational and translational differences, the data is displayed for the period before contact (A) and the period after contact (B). For each graph, the data is summarized using means plus standard deviations and the brackets represent significant differences (p ≤ 0.05) between groups.
Table 1.
Top, overall median and maximum range differences of the femoral and tibial ACS axes (Rx, Ry, and Rz) and origin (T). Bottom, overall median and maximum difference in knee joint rotational and translational excursion for periods A and B.
| ANATOMICAL COORDINATE SYSTEM DIFFERENCES | ||||||||
|---|---|---|---|---|---|---|---|---|
| FEMUR | TIBIA | |||||||
|
| ||||||||
| Rx (°) | Ry (°) | Rz (°) | T (mm) | Rx (°) | Ry (°) | Rz (°) | T (mm) | |
|
| ||||||||
| MAX | 10.23 | 8.88 | 18.18 | 33.70 | 9.25 | 7.47 | 13.43 | 29.11 |
|
| ||||||||
| MEDIAN | 5.07 | 3.67 | 11.97 | 24.91 | 4.24 | 3.60 | 7.48 | 14.18 |
| KNEE JOINT KINEMATIC DIFFERENCES | ||||||
|---|---|---|---|---|---|---|
| JOINT ROTATIONS | JOINT TRANSLATIONS | |||||
|
| ||||||
| FL\EX (°) | AD\AB (°) | IN\EX (°) | ME\LA (mm) | AN\PO (mm) | CO\DI (mm) | |
|
| ||||||
| PERIOD A | ||||||
| MAX | 7.08 | 5.12 | 6.34 | 9.31 | 10.71 | 10.66 |
|
| ||||||
| MEDIAN | 0.51 | 0.02 | 0.06 | 1.70 | 1.21 | 0.68 |
|
| ||||||
| PERIOD B | ||||||
| MAX | 9.28 | 11.80 | 14.76 | 16.84 | 21.62 | 27.60 |
|
| ||||||
| MEDIAN | 2.21 | 5.52 | 5.04 | 8.61 | 6.74 | 18.72 |
The joint excursion differences between OMC and biplanar videoradiography were larger after contact (period B) for all knee joint parameters (Figure 3 Middle: FL/EX, AD/AB, IN/EX; Figure 3 Bottom: ME/LA, AN/PO, and CO/DI). The FL/EX excursion differences were not found to be statistically significant between period A and B (p=0.13). For AD/AB and IN/EX, the increase in excursion difference between OMC and biplanar videoradiography was more striking. These increases were statistically significant (p<0.0001). The maximum excursion differences for joint rotations were as high as 7° for periods A and 15° for period B (Table 1).
For ME/LA, AN/PO, and CO/DI, excursion differences between OMC and biplanar videoradiography increased from period A to period B. These increases were all statistically significant (p<0.001). The maximum excursion differences for joint translations were as high as 11mm and 28mm for periods A and B, respectively (Table 1).
4. Discussion
We compared the kinematic measurements obtained from OMC and biplanar videoradiography during a jump-cut maneuver. The results support our first hypothesis that the soft tissue surrounding the femur would have a greater effect on the kinematic measurements than the soft tissue surrounding the tibia during a jump-cut maneuver. The results also support our second hypothesis that that STA would significantly influence the OMC joint kinematic measurements after ground contact (period B) during a jump-cut manuever.
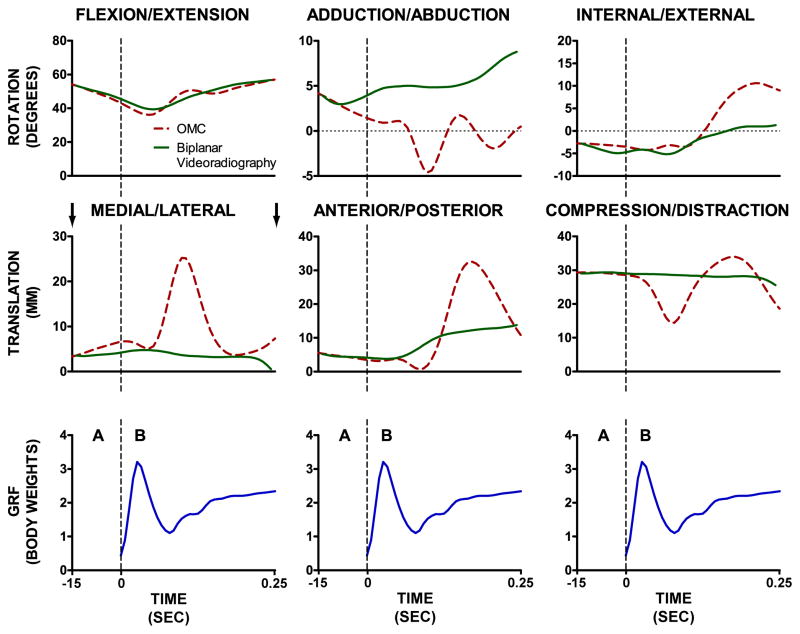
Peak OMC joint rotations and translations were observed to differ as much as 15° and 28mm (Table 1), which is consistent with previous studies that report deviations of 2–20° and 10–30mm (Cappozzo et al., 1996; Holden et al., 1997; Reinschmidt, van den Bogert, et al., 1997; Garling et al., 2007; Tsai et al., 2011). Herein, the majority of deviations occur during the period after contact (period B), where the skin and muscle is reacting to the landing in an oscillatory manner (Figure 4). The OMC kinematic measurements followed the biplanar videoradiography measurements more closely during the period before contact (period A).
Figure 4.
Example OMC (dotted red) and biplanar videoradiography (solid green) knee flexion angle and ground reaction force (solid blue) data versus time. The dotted vertical lines represent the contact event. The period before contact is period A and the period after contact is period B. Period A began and period B ended when the femur and tibia entered and exited the FOV of the biplanar videoradiography system. Thus, the arrows shown above the ME/LA translation graph denote the time point where the knee entered and exited the field of view of the biplanar videoradiography system, respectively.
The overall distribution of OMC differences, as compared to biplanar videoradiography, was of similar magnitude within each period for all joint rotations and translations. For example, the FL/EX differences during period B were similar to the AB/AD and IN/EX differences during period B. These findings are especially important when evaluating secondary rotational motions such as AB/AD or IN/EX rotation, because the total range of motion is significantly less than FL/EX. This leads to OMC deviations of 100% and above for the secondary rotational motions as well as the three translational components. This amount of kinematic deviation will introduce errors in joint kinetics, determined through inverse dynamics. A study performed by Tsai et al. (2011) comparing single-plane videoradiography motion capture to OMC during slow stair ascent reported significant deviations in joint moments at the knee (>12%), particularly the knee extensor moment. The effect OMC had on the abduction and internal rotational moment at the knee may have been mitigated by the restrictions of both single-plane videoradiography and the shank marker set used for OMC, which make out of plane knee kinematics difficult to elucidate. Additionally, the stair ascent activity studied may not produce impacts large enough to produce influential STA. We expect these kinetic parameters to be significantly affected, especially in high demand landing conditions such as jumping and cutting.
Currently, biplanar videoradiography is limited in its FOV and typically allows only a single joint to be imaged. Thus, a union between OMC and biplanar videoradiography is required for extracting 3-D kinetics at the knee during jumping and cutting. The data presented herein show that the soft tissue surrounding the femur affects joint kinematics more significantly than the soft tissue surrounding the tibia, which aligns with the results presented by Garling et al. (2007) and Reinschmidt et al. (1997). This makes intuitive sense because the soft tissue mass surrounding the femur is more than twice that of the tibia (Cheng et al., 2000). Moreover, work from Okita et al. (2009) and Reinschmidt et al. (1997) support the expectation that motion artifact associated with surface markers rigidly affixed to the bony prominences of the ankle malioli and to the foot segment would be small. By using a calibration lattice for co-registration of OMC and biplanar videoradiography, we avoid using heavier radio-opaque markers on the surface of the skin and facilitate full body OMC modeling. The combined technique presented herein allows investigators to collect femur and tibia motion without STA while collecting OMC data for the foot and ankle to preserve the kinematic chain required for calculating inverse dynamics. These results highlight the importance of reporting knee joint kinetics in the tibial coordinate system to mitigate the effect of STA when using OMC alone.
Furthermore, an entire maneuver involving jumping and cutting will include kinematic outcomes before and after landing and beginning a cut (Figure 1B). These parts of the maneuver are more easily captured using OMC because the FOV is significantly larger. The combination of both OMC and biplanar videoradiography becomes advantageous in assessing the entire maneuver from start to finish. Based on the reported results, OMC can sufficiently measure the sagittal plane kinematics and kinetics before and after landing while biplanar videoradiography allows investigators to focus in on the knee during landing, where the bones, cartilage, and ligamentous structures are under the most stress.
The limitations of biplanar videoradiography have been thoroughly documented (Tashman and Anderst, 2003). Specifically, biplanar videoradiography is not as readily available as traditional OMC and the x-ray exposure increases the risk to subjects, albeit the total dose applied in this study was low (<15mrem). Furthermore, the relatively small imaging volume limits the range of activities that can be studied. Other potential study limitations include the placement of the OMC markers to optimize for the least squares technique and not the point cluster technique, and only a single jump-cut activity was tested. Results for walking, running, or other activities may be vastly different. Additionally, our subject population was relatively small and consisted of healthy recreational athletes with similar height and weight demographics. This excluded the possibility of directly correlating STA with body mass index (BMI). However, it would be expected that higher BMI would correlate with higher STA based on the results presented herein. Finally, the lack of a common and independent static calibration frame required that we co-register the two imaging modalities using a frame during the flight phase. This may produce a shift in the data along the y-axis of the Cartesian plane; however, any affects of this shift are eliminated using the excursion (max-min) analysis executed herein.
In this study, we captured an entire jump-cut maneuver with OMC while using biplanar videoradiography to focus on knee joint kinematics during impact with the ground. To our knowledge, this is the first use of biplanar videoradiography to assess six degree-of-freedom STA in the knee during a jump-cut maneuver. This study is a significant step toward understanding the ways OMC and biplanar videoradiography can be used together for answering questions about the biomechanics of the joint, especially during rapid movements and direction changes that are associated with injury. Additionally, this study provides a foundation for creating methods for modeling soft tissue motion in order to mitigate its affect on kinematic outcome measures. The results presented in this study should be considered when interpreting knee mechanics from OMC at and directly after impact during a jump-cut manuever, specifically those associated with joint translations and secondary rotations (AB/AD and IN/EX). Additionally, we recommend the interpretation of all knee kinetics in the tibial coordinate system based on the lower STA observed for the shank. It is our hope that a combination of OMC and bi-planar videoradiography motion capture can be used to investigate entire jumping and cutting activities in order to better understand the kinematic and kinetic factors associated with non-contact ACL injury.
Acknowledgments
This publication was made possible by The W.M. Keck Foundation and Grant Numbers P20-GM104937 (COBRE), and R01-AR047910 from NIAMS/NIH. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIAMS and NIH.
Footnotes
Conflict of Interest Statement
The authors have no financial or personal relationships that could bias this work.
References
- Akbarshahi M, Schache AG, Fernandez JW, Baker R, Banks S, Pandy MG. Non-invasive assessment of soft-tissue artifact and its effect on knee joint kinematics during functional activity. Journal of Biomechics. 2010;43:1292–1301. doi: 10.1016/j.jbiomech.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. Journal of Biomechanical Engineering. 1998;120:743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- Brainerd EL, Baier DB, Gatesy SM, Hedrick TL, Metzger KA, Gilbert SL, Crisco JJ. X-ray reconstruction of moving morphology (XROMM): precision, accuracy and applications in comparative biomechanics research. Journal of Experimental Zoology Part A, Ecological Genetics and Physiology. 2010;313:262–279. doi: 10.1002/jez.589. [DOI] [PubMed] [Google Scholar]
- Buczek FL, Rainbow MJ, Cooney KM, Walker MR, Sanders JO. Implications of using hierarchical and six degree-of-freedom models for normal gait analyses. Gait & Posture. 2010;31:57–63. doi: 10.1016/j.gaitpost.2009.08.245. [DOI] [PubMed] [Google Scholar]
- Cappozzo A, Catani F, Leardini A, Benedetti M, Della Croce U. Position and orientation in space of bones during movement: experimental artefacts. Clinical Biomechanics. 1996;11:90–100. doi: 10.1016/0268-0033(95)00046-1. [DOI] [PubMed] [Google Scholar]
- Challis JH. A procedure for determining rigid body transformation parameters. Journal of Biomechanics. 1995;28:733–737. doi: 10.1016/0021-9290(94)00116-l. [DOI] [PubMed] [Google Scholar]
- Cheng CK, Chen HH, Chen CS, Lee CL, Chen CY. Segment inertial properties of Chinese adults determined from magnetic resonance imaging. Clinical Biomechanics. 2000;15:559–566. doi: 10.1016/s0268-0033(00)00016-4. [DOI] [PubMed] [Google Scholar]
- Deneweth JM, Bey MJ, McLean SG, Lock TR, Kolowich PA, Tashman S. Tibiofemoral joint kinematics of the anterior cruciate ligament-reconstructed knee during a single-legged hop landing. American Journal of Sports Medicine. 2010;38:1820–1828. doi: 10.1177/0363546510365531. [DOI] [PubMed] [Google Scholar]
- Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes. Medicine and Science in Sports and Exercise. 2005;37:124–129. [PubMed] [Google Scholar]
- Garling EH, Kaptein BL, Mertens B, Barendregt W, Veeger HEJ, Nelissen RGHH, Valstar ER. Soft-tissue artefact assessment during step-up using fluoroscopy and skin-mounted markers. Journal of Biomechanics. 2007;40:S18–S24. doi: 10.1016/j.jbiomech.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. Journal of Science and Medicine in Sport/Sports Medicine Australia. 2009;12:622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE, Hannafin JA, Hewett TE, Huston LJ, Ireland ML, Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, Myklebust G, Noyes FR, Powers C, Shields C, Shultz SJ, Silvers H, Slauterbeck J, Taylor DC, Teitz CC, Wojtys EM, Yu B. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. American Journal of Sports Medicine. 2006;34:1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. Journal of Biomechanical Engineering. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- Holden JP, Orsini JA, Siegel KL, Kepple TM, Gerber LH, Stanhope SJ. Surface movement errors in shank kinematics and knee kinetics during gait. Gait & Posture. 1997;5:217–227. [Google Scholar]
- Junkin DM, Johnson DJ, Fu FH, Mark MD, Willenborn M, Fanelli GC, Wascher DW. Orthopaedic Knowledge Update: Sports Medicine. Vol. 4. American Academy of Orthopaedic Surgeons; 2009. Knee Ligament Injuries; pp. 135–153. [Google Scholar]
- Lafortune MA, Cavanagh PR, Sommer HJ, Kalenak A. Three-dimensional kinematics of the human knee during walking. Journal of Biomechanics. 1992;25:347–357. doi: 10.1016/0021-9290(92)90254-x. [DOI] [PubMed] [Google Scholar]
- McNair PJ, Marshall RN, Matheson JA. Important features associated with acute anterior cruciate ligament injury. The New Zealand Medical Journal. 1990;103:537–539. [PubMed] [Google Scholar]
- Miranda DL, Rainbow MJ, Leventhal EL, Crisco JJ, Fleming BC. Automatic determination of anatomical coordinate systems for three-dimensional bone models of the isolated human knee. Journal of Biomechanics. 2010;43:1623–1626. doi: 10.1016/j.jbiomech.2010.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda DL, Schwartz JB, Loomis AC, Brainerd EL, Fleming BC, Crisco JJ. Static and Dynamic Error of a Biplanar Videoradiography System Using Marker-Based and Markerless Tracking Techniques. Journal of Biomechanical Engineering. 2011;133:121002. doi: 10.1115/1.4005471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers CA, Torry MR, Peterson DS, Shelburne KB, Giphart JE, Krong JP, Woo SLY, Steadman JR. Measurements of Tibiofemoral Kinematics During Soft and Stiff Drop Landings Using Biplane Fluoroscopy. American Journal of Sports Medicine. 2011 doi: 10.1177/0363546511404922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okita N, Meyers SA, Challis JH, Sharkey NA. An objective evaluation of a segmented foot model. Gait & Posture. 2009;30:27–34. doi: 10.1016/j.gaitpost.2009.02.010. [DOI] [PubMed] [Google Scholar]
- Reinschmidt C, van Den Bogert AJ, Murphy N, Lundberg A, Nigg BM. Tibiocalcaneal motion during running, measured with external and bone markers. Clinical Biomechanics (Bristol, Avon) 1997;12:8–16. doi: 10.1016/s0268-0033(96)00046-0. [DOI] [PubMed] [Google Scholar]
- Reinschmidt C, van den Bogert AJ, Nigg BM, Lundberg A, Murphy N. Effect of skin movement on the analysis of skeletal knee joint motion during running. Journal of Biomechanics. 1997;30:729–732. doi: 10.1016/s0021-9290(97)00001-8. [DOI] [PubMed] [Google Scholar]
- Söderkvist I, Wedin PA. Determining the movements of the skeleton using well-configured markers. Journal of Biomechanics. 1993;26:1473–1477. doi: 10.1016/0021-9290(93)90098-y. [DOI] [PubMed] [Google Scholar]
- Tashman S, Anderst W. In-vivo measurement of dynamic joint motion using high speed biplane radiography and CT: application to canine ACL deficiency. Journal of Biomechanical Engineering. 2003;125:238–245. doi: 10.1115/1.1559896. [DOI] [PubMed] [Google Scholar]
- Taylor KA, Terry ME, Utturkar GM, Spritzer CE, Queen RM, Irribarra LA, Garrett WE, DeFrate LE. Measurement of in vivo anterior cruciate ligament strain during dynamic jump landing. Journal of Biomechanics. 2011;44:365–371. doi: 10.1016/j.jbiomech.2010.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clinical Orthopaedics and Related Research. 1985:43–49. [PubMed] [Google Scholar]
- Torry MR, Shelburne KB, Peterson DS, Giphart JE, Krong JP, Myers C, Steadman JR, Woo SLY. Knee kinematic profiles during drop landings: a biplane fluoroscopy study. Medicine and Science in Sports and Exercise. 2011;43:533–541. doi: 10.1249/MSS.0b013e3181f1e491. [DOI] [PubMed] [Google Scholar]
- Tsai TY, Lu TW, Kuo MY, Lin CC. Effects of soft tissue artifacts on the calculated kinematics and kinetics of the knee during stair-ascent. Journal of Biomechanics. 2011;44:1182–1188. doi: 10.1016/j.jbiomech.2011.01.009. [DOI] [PubMed] [Google Scholar]