Abstract
Analysis of lipid storage in postmortem brains of patients with amaurotic idiocy led to the recognition of five lysosomal ganglioside storage diseases and identification of their inherited metabolic blocks. Purification of lysosomal acid sphingomyelinase and ceramidase and analysis of their gene structures were the prerequisites for the clarification of Niemann-Pick and Farber disease. For lipid catabolism, intraendosomal vesicles are formed during the endocytotic pathway. They are subjected to lipid sorting processes and were identified as luminal platforms for cellular lipid and membrane degradation. Lipid binding glycoproteins solubilize lipids from these cholesterol poor membranes and present them to water-soluble hydrolases for digestion. Biosynthesis and intracellular trafficking of lysosomal hydrolases (hexosaminidases, acid sphingomyelinase and ceramidase) and lipid binding and transfer proteins (GM2 activator, saposins) were analyzed to identify the molecular and metabolic basis of several sphingolipidoses. Studies on the biosynthesis of glycosphingolipids yielded the scheme of Combinatorial Ganglioside Biosynthesis involving promiscuous glycosyltransferases. Their defects in mutagenized mice impair brain development and function.
Keywords: endocytosis of membrane lipids, lysosomal digestion, lipids regulate endolysosomal proteins, lipid storage diseases, lipid binding proteins, ganglioside metabolism
1. Lipid analysis of post-mortem brain tissues with infantile amaurotic idiocy and the discovery of GM1 gangliosidosis
As a student my special areas of interest were natural sciences and mathematics. In the early 1960s, I studied chemistry at the Ludwig-Maximilians-University in Munich. For a training in neurosciences I joined the neurochemical group of Prof. Horst Jatzkewitz at the Max-Planck-Institute of Psychiatry, who was developing analytical methods for the separation and analysis of sphingolipids and the study of metachromatic leukodystrophy.1–3) Unfortunately, my original thesis project failed, but I was saved by a lucky coincidence. In June 1962, acetone-fixed post-mortem brain tissue from a patient with infantile amaurotic idiocy (IAI) arrived at the laboratory. This case opened a new research field to me for many years to come. My lipid analysis revealed two storage compounds (A’ (GM2) and B’ (GA2)) (Fig. 1), an observation which was supported by the analysis of 11 additional formalin fixed post-mortem brains with IAI. However, a 12th case did not store these lipids but accumulated enormous amounts of related compounds, ganglioside A (now named ganglioside GM1) and its sialic acid-free residue (GA1).4–6) They were much less abundant in control brain samples kept comparably proving that both were original storage compounds and not merely generated by formalin fixation. This was the first description of GM1 gangliosidosis.4–6)
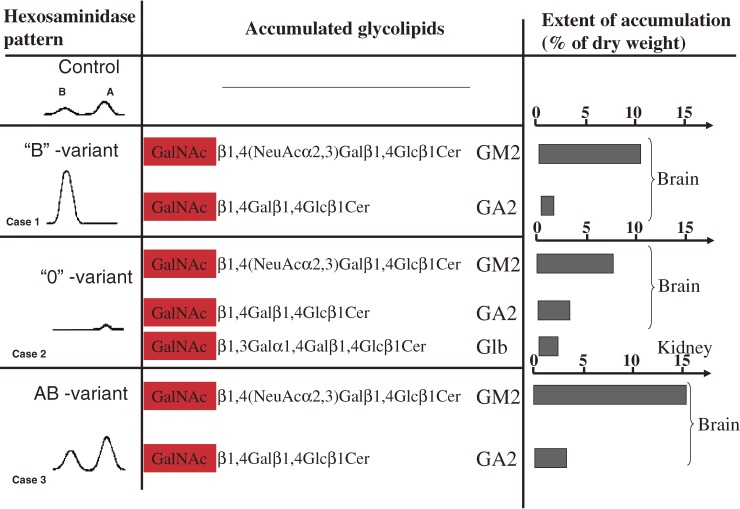
Figure 1.
Biochemical analysis of brains with infantile amaurotic idiocy. Lipid and hexosaminidase analysis in the brain tissue of the three first cases revealed puzzling results in 1967 and spring of 1968 (summarized in: ref. 249).
- The tissue of case 1 with TSD (called “B”-variant) was deficient in HexA activity and had increased HexB activity, a finding which was confirmed in 1968 by an additional case250) and the observation by Okada and O’Brian.251)
- Brain and visceral organs of case 2 –characterized by the additional storage of globoside (Glb) in visceral tissues– was completely deficient in both major hexosaminidases, A and B, and was left with a minor activity of HexS.26,250,252,253) This one we named “0”-variant of GM2-gangliosidosis and it was later called Sandhoff disease.
- Apparently contradicting the above findings, the brain tissue of case 3 contained both, HexA and HexB activity, even at elevated levels despite a huge accumulation of GM2 and GA2 (later called AB-variant after the defect of a cofactor –GM2AP– was discovered, see below).
At that time, amaurotic idiocy was described as an inherited disease characterized by the accumulation of lipid-containing cells in the viscera and in the nervous system, mental retardation and impaired vision or blindness. The classical infantile form of amaurotic idiocy had been known as Tay-Sachs disease (TSD). There had been little progress in its understanding until the development of chemical, biochemical and refined ultrastructural means of investigations. In the late 1930s, the biochemist Ernst Klenk7,8) from the University of Cologne, detected a new group of acid glycosphingolipids as storage material in the brain of TSD patients. They were also abundant in normal ganglion cells,9,10) and named “Ganglioside” (gangliosides). The first ganglioside structure, that of ganglioside G1 (GM1), was elucidated by Kuhn and Wiegandt,11) the main storage compound in TSD was identified by Svennerholm,12) and its structure elucidated by Makita and Yamakawa13) and Ledeen and Salsman.14) In the electron microscope, Terry and co-workers15–17) observed storage granules (membranous cytoplasmic bodies) in the cytoplasm of the distended neurons that resemble pathologically modified lysosomes incapable of degrading their storage material.
2. Search for the metabolic defects in Tay-Sachs and related diseases
In the early 1960s, I collected post-mortem tissues of several cases of IAI with neuronal storage of ganglioside GM2 and its sialic acid free derivative GA2. Storage compounds were isolated and radiolabeled for enzymatic studies by catalytic reduction of the double bond in the sphingoid base. Since 1966, I also obtained fresh and deep-frozen autopsy material from several cases with IAI, suitable for metabolic studies to search for the defective enzymatic step causing the pathological lipid storage in the patients. Different from all cases of TSD studied so far, one of them contained an additional accumulation of globoside in its visceral organs. Most importantly, all three storage compounds –GM2, GA2 and globoside– had a structural feature in common, a terminal β-glycosidically linked N-acetylgalactosamine residue (Fig. 1). This observation suggested a β-N-acetylgalactosaminidase deficiency in the patients’ tissues, blocking the catabolism of the storage compounds. At that time, however, no N-acetylgalactosaminidase was known in human tissues, only N-acetylglucosaminidases. Studies on the purification and substrate specificities of human N-acetylglucosaminidases proved that they also hydrolyze N-acetyl-β-galactosaminids though with different kinetic constants,18) and that their two major forms, the hexosaminidases A and B, could easily be separated by ion exchange chromatography19) and isoelectric focussing.20) Indeed, the case with an additional storage of globoside in the visceral organs exhibited complete deficiencies of hexosaminidases A and B (0-variant), another case a deficiency of hexosaminidase A (B-variant), and a third case no hexosaminidase deficiency at all (AB-variant) (Fig. 1).
3. Structure and function of the lysosomal hexosaminidases
In order to clarify the stunning and apparently contradictory findings on the first three cases of IAI described above, we purified the human hexosaminidases A (HexA) and B (HexB), and later also S (HexS) to apparent homogeneity for closer characterization. A historical view is given in.21) Here, some major observations are presented.
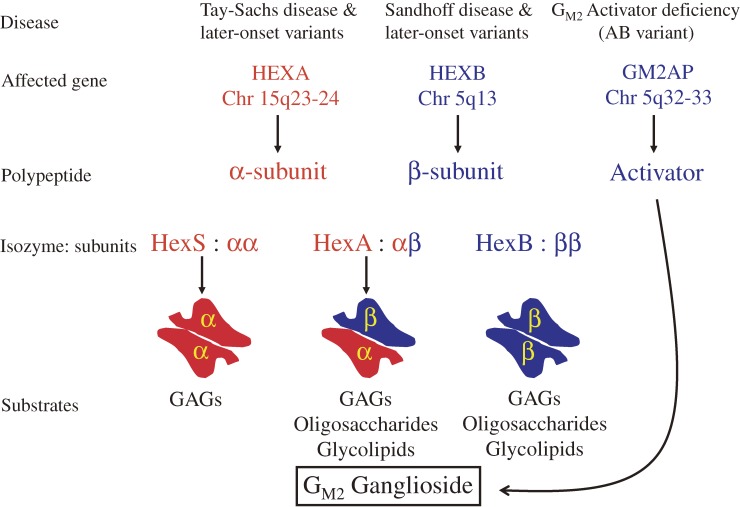
Both isoenzymes hydrolyzed the radiolabeled neutral storage compounds, GA2 and globoside, and released their terminal N-acetylgalactosamine residues in a detergent based assay using a crude sodium taurocholate preparation. On the other hand, only HexA had a minor but significant activity on the anionic storage compound, the radiolabeled ganglioside GM2 releasing its terminal N-acetylgalactosamine residue.18,22) Heating of HexA under appropriate conditions generated HexB,23) an observation which was explained by the finding of Srivastava and Beutler,24) that both isoenzymes had a subunit in common, HexA being a heteropolymer (αβ)n and HexB a homopolymer (ββ)n. This view was substantiated and refined by several groups (for review see21,25)) and was eventually proven by the observation that mutations in the β-subunit gene caused the loss of HexA and HexB activity in variant 0 of GM2-Gangliosidoses (Sandhoff disease), whereas mutations in α-subunit gen caused the loss of HexA and HexS activity in TSD (Fig. 2).
Figure 2.
The GM2 Gangliosidoses and the β-hexosaminidase system (modified after ref. 25). Three polypeptides, each encoded in a different gene, are needed for the degradation of ganglioside GM2: the α- and β-subunit of the A isoenzyme and the activator protein which binds the ganglioside and presents it to the enzyme. GAGs, glycosaminoglycans.
The minor and labile HexS26) has a specificity similar to that of HexA. It hydrolyzes anionic and neutral substrates, oligosaccharides and glycosphingolipids including the sulfated SM2 and ganglioside GM2.27)
4. Search for the missing cofactor in AB variant of GM2 gangliosidoses
HexA and B purified from the brain tissue of our first case with AB variant (Fig. 1) exhibited normal activities and specificities against water-soluble synthetic substrates and hydrolyzed also the neutral storage compound GA2 in the presence of detergents.28) Also the main storage compound GM2 was hydrolyzed by a HexA preparation from the patient’s liver in the presence of detergents.28) It remained an enigma why the patient’s tissues stored glycolipids in the presence of their functional catabolic enzyme. Therefore, we looked for a missing factor in human tissues that might substitute for the detergent in the in vitro assay and stimulate the HexA catalyzed hydrolysis of radiolabeled ganglioside GM2. Such a protein factor, now named GM2 activator protein, GM2AP, was found by Ernst Conzelmann29) and purified to homogeneity.30) Its activity was completely missing in AB variant tissues and its cellular uptake restored the catabolism of ganglioside GM2 in AB variant fibroblasts.31)
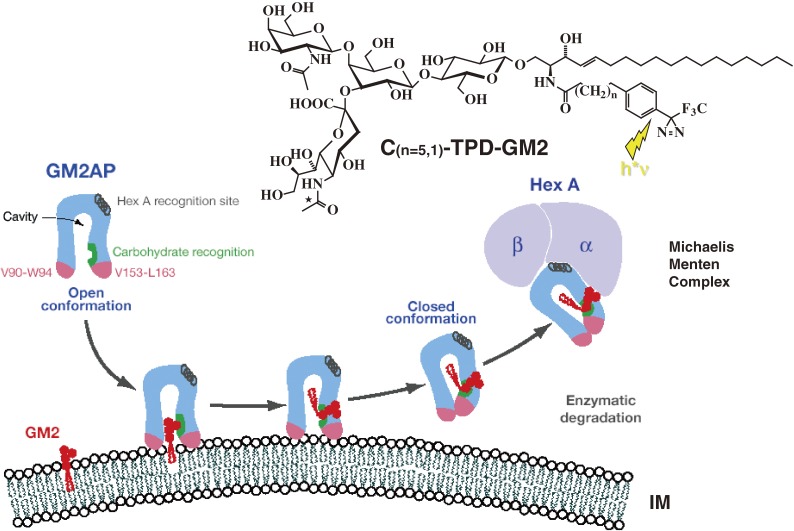
The GM2AP is a small glycolipid binding protein which can form water-soluble stochiometric complexes (1:1) with ganglioside GM230,32) and presents the lipid substrate to the water soluble HexA. In the presence of GM2AP, nice Michaelis-Menten kinetics were obtained for the hydrolysis of GM2 and GA2 by HexA (Fig. 3), whereas detergent assays always suffered from nonlinearities and poor reproducibility.
Figure 3.
Mechanism of GM2AP-Liftase. Model for the interaction of GM2-activator protein with luminal lysosomal membranes in the degradation of ganglioside GM2 (modified after ref. 36). GM2AP interacts with the membrane by dipping the two exposed hydrophobic loops, V90-W94 and V153-L163, into the apolar part of the membrane. Ganglioside GM2 is recognized by specific sites at the rim of the cavity. In the open protein conformation, the large hydrophobic area reaching from the apolar phase of the membrane to the activator’s cavity lowers the energy barrier for lipids leaving the membrane in an upward direction. After the ceramide tail has moved inside the activator’s cavity, the inward pointing orientation for the hydrophobic loop V153-L163 is favoured and the conformation changes to the closed form.254) This folding in of the hydrophobic loop leaves a more polar patch close to the membrane. The activator is then anchored only by the loop V90-W94. It may now rotate slightly upwards to expose all polar patches more fully to the solvent, and it may also leave the membrane and interact with the degrading enzyme. The photoaffinity label analogues C(n=5,1)-TPD-GM2 were photoincorporated specifically into the region V153-L163.
The mature GM2AP is a small glycoprotein of about 20 kDa generated from a precursor protein in the endolysosomal compartment of the cell.33) It carries an N-glycosylation site and contains eight cysteins that form four disulfide bonds34). Its crystal structure shows a unique spacious hydrophobic β-cup for binding of the ceramide moiety.35)
A flexible hydrophobic loop adjacent to the cavity is supposed to interact with membranes and allows the extraction of the lipid at acidic pH values.36) A HexA binding region of the GM2AP facilitates the formation of the Michaelis-Menten complex37) (Fig. 3).
In vitro and in vivo data obtained until 2000 suggested that GM2AP might be quite specific for binding and solubilizing glycolipids like GM2 and GM1 from micells and lipid vesicles, and transferring them to other membranes or enzymes like HexA,38) and β-galactosidase, respectively.39) However, expression of recombinant human GM2AP in insect cells revealed that it also recognizes phospholipids40) and fuses lipid vesicles at acidic pH values.41)
5. Variant B1 of GM2 gangliosidoses
In 1980, two cases with apparent variant AB of GM2 gangliosidosis were described.42) In one of them, however, Li and co-workers could not find an activator protein deficiency.43) They suggested that the patient might have a structural gene mutation rendering HexA nonresponsive to stimulation by the GM2 activator for the hydrolysis of GM2 ganglioside.44) To clarify this point, we studied the substrate specificity of human hexosaminidases. Competition experiments between different substrates showed that normal human HexA carries two active sites to hydrolyze both, anionic and neutral substrates, respectively, whereas HexB hydrolyzes neutral substrates only.45) Then Kytzia analyzed two patients with clinical TSD and extensive neuronal storage of GM2, still having apparently both, HexA and GM2 activator protein activity. HexA of both patients cleaved neutral N-acetylglucosaminides and -galactosaminides with almost normal kinetics, but were almost inactive to hydrolyze an anionic sulphated and water soluble glucosaminide (MUGlcNAc-6-S, a newly described substrate for HexA,46)) and ganglioside GM2 in the presence of the GM2 activator protein.45,47) The new form of the disease was named variant B1 of GM2 gangliosidoses since their HexA was still active against neutral substrates but had lost its capacity to cleave anionic substrates such as GM2.
Cellular hybridization experiments between patient fibroblasts demonstrated variant B1 being allelic to variant B.48) They indicated that the α-subunit of HexA contributes to the hydrolysis of anionic substrates, MUGlcNAc-6-S and GM2 (as well as GA2) in the presence of the GM2AP and that this function is inactivated by mutations in the α-subunit in patients with variant B1. Kinetic experiments showed furthermore that the free GM2 activator competes with the sulphated substrate MUGlcNAc-6-S for the α-dependent site of HexA and HexS.45) Indeed, GM2AP recognizes the α-subunit,37) an observation that is in line with an earlier finding30) that glycolipids GM2, GA2 and globoside in the presence of the GM2 activator protein were almost exclusively degraded by HexA and not by HexB. Even the precursor, proHexA degrades GM2 in the presence of the GM2 activator protein.49)
6. Threshold theory and the development of different clinical forms of GM2 gangliosidoses
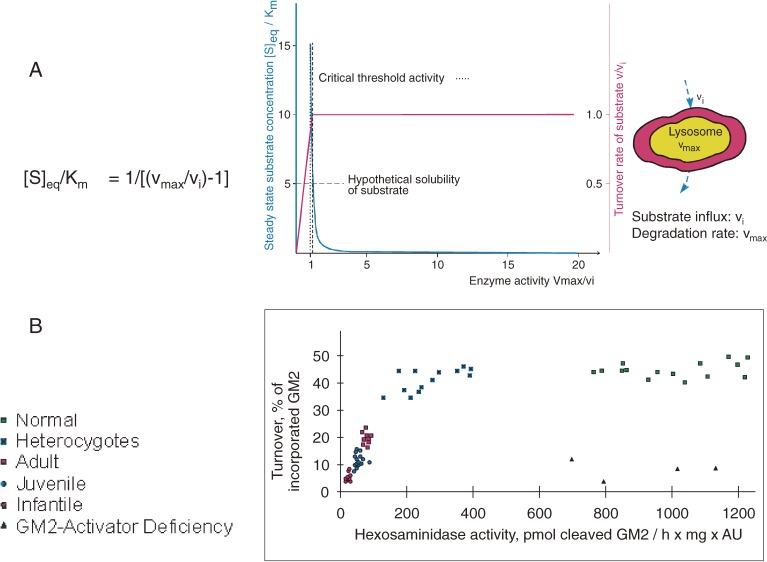
Deficiencies of hexosaminidase activities of various extent caused by allelic mutations of the α- and β-subunits, respectively, have been observed in a variety of patients with different clinical forms (infantile, juvenile, adult and chronic) of GM2 gangliosidoses representing a wide range of clinical symptomatology.25) Whereas the infantile forms show a very uniform clinical picture, that of juvenile and adult forms is quite variable and ranges from spinocerebellar degeneration, muscular atrophy- and amyotrophic lateral sclerosis-like syndromes, to psychiatric symptomatology which hardly resembles that of the infantile form of the disease. At the biochemical level, this heterogeneity is paralleled by a variation of the extent and pattern of the glycolipid accumulation in different regions of the brain. Whereas infantile forms show an excessive and ubiquitous neuronal storage, late-onset forms have a less pronounced accumulation which is restricted to specific brain regions.16,50) Obviously, different allelic mutations in one gene locus can lead to extremely different clinical syndromes and neuropathic forms. A crucial difference observed between various clinical forms, e.g. of GM2 gangliosidosis, is the occurrence of different residual activities of the variant HexA in cultured fibroblasts against its natural substrate.51–53) Ganglioside GM2 cleaving activities were almost absent in fibroblasts of infantile patients, and significantly higher in fibroblasts of juvenile and adult patients (Fig. 4). Residual activities in the range of 10–20% of the control value already appear to be compatible with normal life. Similar findings in fibroblasts from patients with variant 054) and arylsulfatase A activity in fibroblasts of patients with MLD revealed the importance of small variations of the low residual enzyme activities for the development of different clinical syndromes of a disease.53)
Figure 4.
Residual catabolic activity correlates with clinical forms of GM2 gangliosidoses (modified after ref. 53). A) Steady-state substrate concentration as a function of enzyme concentration and activity.51) The model underlying this theoretical calculation assumes influx of the substrate into the lysosomal compartment at a constant rate (vi) and its subsequent utilization by the catabolic enzyme (for details see text). Blue line = [S]eq steady-state substrate concentration; ……… = theoretical threshold of enzyme activity; - - - - - - - = critical threshold value, taking limited solubility of substrate into account; red line = turnover rate of substrate (flux rate). B) In order to experimentally verify the basic assumptions on which this model rests, studies were performed in cell culture.53) The radiolabeled substrate ganglioside GM2 was added to cultures of skin fibroblasts with different activities of beta-hexosaminidase A and its uptake and turnover measured. The correlation between residual enzyme activity and the turnover rate of the substrate was essentially as predicted: degradation rate of ganglioside GM2 increased steeply with residual activity, to reach the control level at a residual activity of approximately 10–15% of normal. All cells with an activity above this critical threshold had a normal turnover. Comparison of the results of these feeding studies with the clinical status of the donor of each cell line basically confirmed our notions but also revealed the limitations of the cell culture approach.
Also in Gaucher disease and in acid sphingomyelinase-deficient Niemann-Pick disease, the severity of the clinical symptoms correlates inversely with the residual activities of the deficient enzymes.55–57)
These observations can be understood qualitatively on the basis of a greatly simplified kinetic model51–53). Considering an influx rate (vi) of the substrate (e.g. ganglioside) into the lysosomal compartment of an individual cell, the steady-state substrate concentrations [Seq] and the turnover rate were simply calculated as a function of the residual catabolic enzyme activity (Fig. 4).
Since the degradative capacity (Vmax) in normal control cells exceeds the influx rate vi severalfold (for the GM2-degrading system a factor of about 20-fold was estimated), [S]eq will be far below the KM value of the degrading enzyme. As discussed before,21) substantial reductions of the probands’ degrading enzyme activity ν to values still above νi will lead to a moderate increase of [Seq] and not to an irreversible accumulation, since the remaining enzyme activity is still sufficient to cope with the substrate’s influx rate. However, when the residual activity of the patients’ variant enzyme falls below a critical threshold the turnover of the substrate will be reduced and it will accumulate. The rate of accumulation will be proportional to the difference between threshold activity of the catabolic step and its smaller actual residual activity in the patient’s lysosome.
Rates of ganglioside biosynthesis (corresponding to influx rates) and degrading enzyme activities (HexA in the presence of GM2 activator) may vary with organs and cell types, and even between individual neurons. Therefore, the consequence of an incomplete enzyme deficiency may be different for different cell types and organs. Cells with a high rate of substrate biosynthesis (corresponding to a high influx rate) and a low level of residual degrading enzyme activity should store first during development of the disease. This means that a certain subset of neurons should be affected preferentially by the storage process, e.g. in the adult form of GM2 gangliosidosis. Thus, in contrast to infantile forms, in which all neurons are affected, in late-onset forms function and viability of a subset of neurons should be affected preferentially, causing different clinical symptomatology.
Of course, the simple kinetic model is only one of several factors involved in the pathogenesis of the disease.21) Other parameters involved include intracellular transport of substrates, regulation of enzyme activities, formation of lytic and toxic compounds,58,59) mechanical distortion of the cells, depletion of precursor pools, and alterations of composition and functions of membranes by the storage process. Formation of meganeurites and the increase in synaptic spines may disturb the connectivity of the brain.60)
7. Sphingolipid activator proteins and the lipid phase problem
The in vitro analysis of enzymatic sphingolipid degradation revealed early on that water-soluble lysosomal hydrolases can cleave their sphingolipid substrates effectively only in the presence of appropriate detergents.22,61,62) The search for in vivo factors substituting for detergents resulted in the discovery of sphingolipid activator proteins, small glycoproteins that bind and solubilize lipids. The first activator protein was discovered in the early 60s by Horst Jatzkewitz when his co-workers purified arylsulfatase A.62) Its deficiency causes sulfatide storage in MLD.1,62–64) Saposin B (Sap-B) is a small glycoprotein forming water soluble stochiometric complexes with sulfatides presenting them to the water soluble enzyme. Its inherited deficiency causes different clinical forms of MLD depending on the mutational profile.64–67)
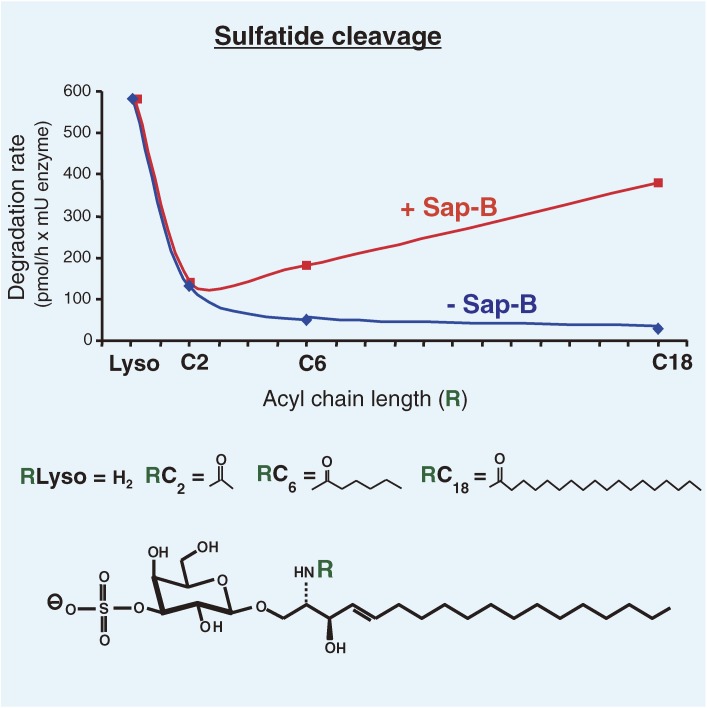
In the absence of detergents or Sap-B, arylsulfatase A (ASA) has almost no activity on its lipophilic substrates, sulfatide and seminolipid. To clarify the mystery we synthesized years later sulfatides with fatty acid residues of different chain lengths and studied their hydrolysis by arylsulfatase A in the absence and presence of Sap-B.68)
As shown in Fig. 5, the water-soluble short chain sulfatides were readily hydrolyzed by ASA in the absence of any detergent or activator protein. Even more, the addition of Sap-B did not stimulate the hydrolysis of soluble short chain sulfatide analogs. However, to achieve substantial cleavage rates of the less soluble, lipophilic sulfatides with long acyl chains, the addition of Sap-B was needed. Similar studies were performed with soluble and less soluble lipophilic analogs of ganglioside GM1 and GM2. The hydrolysis of ganglioside GM1 micelles by β-galactosidase was achieved only by the addition of detergents, or GM2AP or Sap-B. However, the more soluble short acyl chain analogs of GM1 were readily hydrolyzed by β-galactosidase, even in the absence of these additions.39,68–70)
Figure 5.
Sap-B stimulates the enzymatic hydrolysis of micellar sulfatides with long acyl chains. Derivates of sulfatide were hydrolyzed by human arylsulfatase A in the absence or presence of Sap-B (0.1 nmol) in a total incubation volume of 50 µl. The degradation rates given are means from six experiments. Experimental values were all within a range of 20 per cent of the mean. Sulfatides contain different acyl residues in their ceramide moieties: C18-stearoyl, C8-octanoyl, C6-hexanoyl and C2-acetyl-residues.68)
The GM2AP is an essential cofactor for the hydrolysis of GM2 ganglioside by HexA, but not for its more water-soluble analogs with short acyl chains.71) It is also not needed to cleave off the terminal N-acetyl-galactosamine residue from the extended and more exposed oligosaccharide chain of membrane-bound ganglioside GD1a-GalNAc.71)
These experiments showed that the soluble enzymes used can cleave water soluble substrates readily, but hardly recognize insoluble substrates forming micelles in aqueous solution or being components of liposomes or biological membranes. Glycosphingolipids with short oligosaccharide chains (four or less sugars) have to be complexed, lifted from their membranes or solubilized by SAPs to be efficiently degraded by water-soluble lysosomal hydrolases. This view is supported by in vivo findings in SAP deficient mice and human patients. The catabolism of all GSL with short oligosaccharide chains requires the action of SAPs.67) Their inherited deficiency causes fatal storage diseases.
8. The complex cellular functions of SAPs
Sap-B and GM2AP were discovered as essential cofactors for the catabolism of few glycolipids. Their inherited defects cause fatal sphingolipidoses with a rather limited number of storage compounds.67) Based on these observations and early biochemical tests,67) I expected rather limited lipid binding specificities of these proteins. The first surprise came during an attempt to identify further cofactors involved in GSL-catabolism. Sap-B turned out to be quite unspecific as a lipid binding protein and enhanced the catabolism of several GSLs. Sap-B not only stimulated the hydrolysis of sulfatides by ASA,62,72) but also that of globotriaoscylceramide by α-galactosidase,73) ganglioside GM1 by β-galactosidase,68,69) lactosylceramide by β-galactosidase70) and others. Li and co-workers74) even used the human Sap-B successfully to stimulate the hydrolysis of several bacterial glycolipids by bacterial hydrolases.
GM2AP, which is specifically needed for the catabolism of the GSLs, GM2 and GA2, also effectively stimulates the degradation of ganglioside GM1 by β-galactosidase39,71) and binds in its hydrophobic cavity a bunch of unspecific phospholipids.36,75) The identification of inherited SAP deficiencies causing variant forms of known sphingolipidoses and corresponding knock-out mice models (for review see: refs. 21, 67, 76–80) triggered a more detailed analysis of their formation and functions (for review see refs. 67, 81–85).
Unexpected was the finding of Werner Fürst, that the precursor of the sulfatide activator protein, now called saposin B, codes for a big polyprotein and is processed to at least 4 different proteins,86) including the well-known activators Sap-B, and -C. The galley proof of our paper was mailed to three authors of a later Science paper87) 4 months before they published a conceptually similar finding. No reference was given to our work.
A great help for the following studies on the genomic structures, the expression of recombinant proteins and the identification of mutations in patients, was the collaboration between our laboratory and that of Kunihiko Suzuki who also stayed in Bonn for several periods in the late 80s and early 90s.77,88–101)
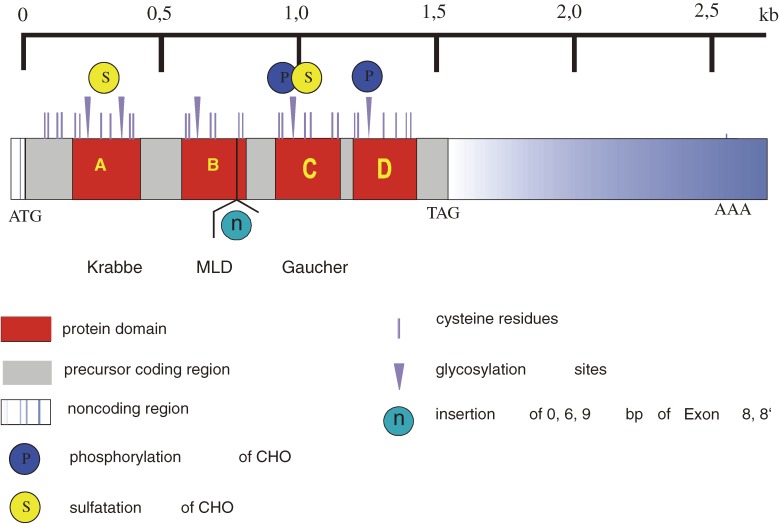
The analysis of the precursor protein, prosaposin,94) revealed that it is generated as a complex glycoprotein and transported from the ER through the Golgi and TGN to the endolysosomal compartment where it is proteolytically processed to four homologous saposins (A, B, C and D) of about 80 amino acids each.90,102)
Each of their sequences contain a conserved N-glycosylation site (Sap-A contains two) and six conserved cysteins forming disulfide bonds.103,104) Inherited defects (Fig. 6) of individual saposins85) and constitutionally generated knockout mice (for review see refs. 67, 79, 80, 105) demonstrated the essential life supporting functions of these lipid binding and activator proteins and helped to determine their in vivo functions which are still a matter of debate.
Figure 6.
Human Prosaposin. The cDNA of human prosaposin codes for a sequence of 524 (or 527) amino acids including a signal peptide of 16 amino acids.92,94) The precursor is proteolytically processed in the endolysosomal compartment to 4 domains, saposin A, B, C and D.102) Cystein residues are marked by vertical bars, N-glycosylation sites by arrow heads. Disease causing mutations affecting human Sap-A,255) Sap-B,64,65) Sap-C256) and prosaposin67,96,257) have been described. Murine models of prosaposin deficiency77) and deficiencies of individual saposins have been investigated: Sap-A,78,80,258) Sap-B,76) Sap-C79) and Sap-D.80,105,259)
A key observation was the discovery of a patient with a total deficiency of prosaposin and therefore also of all four saposins A-D96,106) caused by a homoallelic mutation in the start codon of the prosaposin gene. Patients with this perinatally fatal disease store all those sphingolipids which need a saposin cofactor for their catabolism (ceramide, glucosylceramide, lactosylceramide, sulfatides, ganglioside GM3, globotriaosylceramide etc.) and most importantly they accumulate them together with intraendolysosomal vesicular membranes. A mouse model substantiated these findings.77) Storage of multiple sphingolipids and accumulation of internal membranes (IMs) in the endolysosomal organelles could be reversed in cultured prosaposin deficient fibroblasts by a receptor mediated cellular uptake of the missing prosaposin from the culture medium.107) The prosaposin deficiency turned out to be a “proof of principle” experiment by nature supporting our hypothesis on the cell biology of sphingolipid catabolism in mammalian cells.108) Luminal vesicles are formed within the endolysosomal compartment as platforms for the degradation of sphingolipids and membranes.
Saposins A, B, C and D are essential for the sphingolipid- and membrane degradation at inner lysosomal membranes.83) They bind lipids and transfer them as water-soluble complexes from vesicular membranes to catabolising enzymes or acceptor membranes. GM2AP forms a soluble 1:1 stochiometric complex with ganglioside GM2 which is recognized by HexA as real Michaelis-Menten complex.32) The dimer of saposin B also binds and solubilizes sulfatides (and other lipids) stochiometrically, presenting them to catabolic hydrolases as substrates.109)
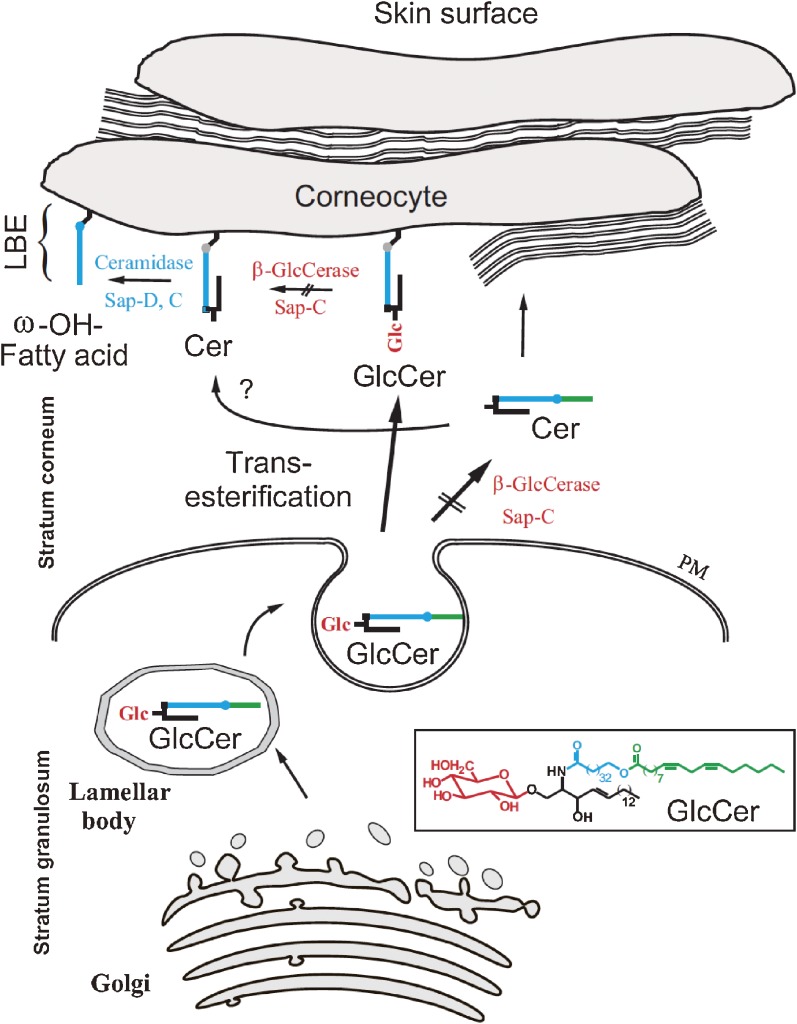
In plasmon resonance studies, saposins A and B were even able to solubilize most of the membrane lipids –including cholesterol and PC– from BMP (bis[monoacylglycero]phosphate) rich and cholesterol poor vesicles at acidic pH values efficiently within few minutes.110,111) Saposin C even transfers bacterial lipids to the CD1b immuno-receptors of the lysosomal membrane.112) Unexpectedly, membrane fusion assays identified GM2AP and the saposins A, C and D –the latter stimulates the hydrolysis of ceramides by acid ceramidase93,113)– also as fusogens for lipid vesicles at lysosomal pH values.114) Saposins are also essential for the generation and maintenance of the water permeability barrier in the skin of land dwelling mammals. Two different phenotypes occur in prosaposin knock-out mice, a neonatally fatal one, and another one with later onset surviving up to about 5 weeks. The latter one shows a complex pathology featuring ichtyosiform dermatitis.77) Prosaposin knock-out mice fail to generate a proper water permeability barrier in the skin.115,116) Detailed analysis uncovered the formation of glucosylceramides with very long acyl chains of 30 up to 36 C-atoms, ω-hydroxylated and esterified with linoleic acid, in mice and in human keratinocytes. With linoleic acid as leaving group, these glucosylceramides can be covalently bound to surface proteins of the keratinocytes in the stratum corneum of the epidermis85) (Fig. 7).
Figure 7.
Extracellular metabolism of glucosylceramide (GlcCer) and formation of the lipid-bound envelope (LBE) (modified after ref. 260). PM: plasma membrane, Cer: ceramide, consisting of sphingosine (black) and long-chain ω-hydroxyl fatty acid (blue). Linoleic acid (green) is found esterified to the ω-hydroxyl moiety. Catabolic blocks in β-glucocerebrosidase- and SAP-C deficiency are indicated by the arrows with slashes through them.
After removal of their terminal glucose residue by lysosomal β-glucocerebrosidase in cooperation with saposin C, they form a hydrophobic protein-bound surface layer of ceramides which is essential for the generation of extracellular lipid stacks (mainly composed of long chain ceramides, fatty acids and cholesterol) forming the water permeability barrier of the skin. Mutagenized mice deficient in prosaposin or in β-glucocerebrosidase cannot remove the terminal glucose residue properly and fail to complete the permeability barrier in the skin. They die soon after birth due to a permanent water loss. This observation also explains instant death of so called Collodion babies117) who suffer from a complete loss of β-glucocerebrosidase activity.
9. Topology of endocytosis and lysosomal digestion of membrane lipids
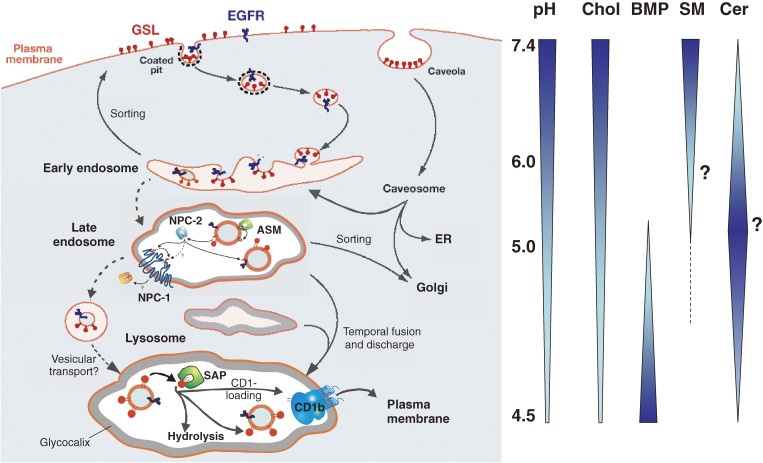
Macromolecules and membrane components reach the lysosomal compartment for digestion by endocytotic pathways, by autophagy118) and by phagocytosis.119,120) They are degraded by lysosomal enzymes at acidic pH values. Their components (amino acids, fatty acids, monosaccharides, sphingoid bases and others) are released to the cytosol and reused for biosynthetic pathways and/or cellular energy production. Complex lipids and proteins of the plasma membrane reach the lysosomal compartment mainly by a vesicular membrane flow through early and late endosomes.121) In cultured fibroblasts, up to 5% of the endocytosed gangliosides GM1 and GM2 are diverted to the Golgi membranes and are used directly for the biosynthesis of more complex gangliosides.122) The original view that the majority of the endocytosed membrane lipids will become part of the limiting lysosomal membranes poses a severe topological problem for their degradation and the stability of the lysosomal perimeter membrane. Newly endocytosed components reaching the limiting lysosomal membrane should be selectively degraded without endangering its essential permeability barrier. This was a quite unlikely hypothesis. Therefore, we proposed108) an alternative pathway based on the formation of multivesicular bodies in normal cultured cells123–125) and the deposition of storage material in form of lamellar arrays within the lysosomal lumen in sphingolipidoses.126)
A key observation for our hypothesis was the accumulation of intralysosomal vesicles and inner membranes (IMs) in patients with an inherited prosaposin deficiency96,106) and in its mouse model.77) Since the accumulation of luminal vesicles and IMs could be reversed by feeding the missing prosaposin at nanomolar concentrations to the patients’ cultured fibroblasts, they were identified as transient platforms for membrane- and lipid degradation.107) Cellular uptake and lysosomal delivery of prosaposin are efficiently facilitated, e.g. by LRP (low density lipoprotein receptor-related protein).127)
Immunoelectron microscopy revealed that lipids of the plasma membrane, e.g. biotinylated ganglioside GM1 indeed reach the IMs of the lysosomal compartment128) as a transient pool for degradation of sphingolipids and other membrane components. The major part of lipid degradation was supposed to take place at their surface with the help of lipid binding and transfer proteins, the SAPs.
Our present view on the topology of lysosomal digestion is given schematically in Fig. 8. During endocytosis, transient IMs are formed by successive steps of vesicle budding and fission controlled by ESCRT proteins129) along the endocytotic pathways. They are prepared for digestion by a lipid sorting process beginning at the level of endosomes.82,130)
Figure 8.
Principles of lysosomal sphingolipid catabolism and membrane digestion. Proposed topology of endocytosis and lysosomal degradation.130) A section of the plasma membrane is internalized by way of coated pits or caveolae. These membrane patches include glycosphingolipids (GSL, red) and receptors such as EGFR (epidermal growth factor receptor, blue). These vesicles fuse with the early endosomes which mature to late endosomes. Endosomal perimeter membranes form invaginations, controlled by ESCRT proteins,129) which bud off, forming intra-endosomal vesicles. Lipid sorting occurs at this stage. The pH of the lumen is at about 5. At this pH, acid sphingomyelinase is active and degrades sphingomyelin of the intra-endosomal vesicles to ceramide, whereas the perimeter membrane is protected against the action of ASM by the glycocalix facing the lumen. This reduction of the sphingomyelin level, coupled with the increase in ceramide, facilitates the binding of cholesterol to NPC-2 and its transport to the perimeter membrane of the late endosome where it is transferred to NPC-1.261) This protein enables the export of cholesterol through the glycocalix, eventually reaching cholesterol binding proteins in the cytosol. Ultimately, late endosomes fuse with lysosomes. The GSLs are in intra-lysosomal vesicles facing the lumen of the lysosome and are degraded by hydrolases with the assistance of LLBPs. The products of this degradation are exported to the cytosol or loaded on CD1b immunoreceptors and exported to the plasma membrane for antigen presentation. Gradients of pH in the lysosol, and intra-endo-lysosomal vesicle content of cholesterol (Chol), BMP, sphingomyelin (SM, hypothetical) and ceramide (Cer; hypothetical) are shown (modified after ref. 83).
Plasma membrane stabilizing lipids are removed from the luminal vesicles. The egress of cholesterol is mediated by two sterol binding proteins, NPC-2 and NPC-1 (summarized in 114), and sphingomyelin is degraded by acid sphingomyelinase (ASM) (Breiden et al., 2012, in preparation).
Anionic BMP stimulating most of the catabolic processes in the lysosome is exclusively formed in the IMs,82,130,131) but not in the lysosomal perimeter membrane, which seems to be quite resistant against lysosomal digestion. It is protected by a thick glycocalix132–136) on its luminal leaflet from the attack by membrane degrading enzymes present in the lumen of the lysosome. The glycocalix is formed by membrane proteins which are highly glycosylated with polylactosamine units highly resistant toward lysosomal digestion. As most biological membranes, the lysosomal perimeter membrane is supposed to have a lateral pressure of at least 31 mN/m, too high to be attacked by GM2AP.137) The lysosomes are also stabilized by HSP70.138)
Indeed, ganglioside GM3 of the limiting lysosomal membrane is in a stable pool protected from degradation,136) whereas it is rapidly degraded during the constitutive process of membrane turnover.139) The major part of membrane degradation has to proceed on the surfaces of these transient IM structures.82) During endocytosis, there is a lipid sorting process to prepare IMs as platforms for sphingolipid and membrane degradation (see section 12). Apparently, acid sphingomyelinase plays a major role in the maturation of IMs for lysosomal digestion.
10. Acid sphingomyelinase and Niemann-Pick disease, type A and type B
Until recently, three main clinical forms of NPD were distinguished,140–142) the infantile neuropathic form type A, the non-neuropathic form type B and the rather variable form type C. As an early hallmark of the disease Ernst Klenk discovered an accumulation of the membrane lipid sphingomyelin,143) known later on to be caused in type A and B patients by a deficiency of its catabolic enzyme, the lysosomal acid sphingomyelinase (ASM).144) ASM is very special among the many soluble sphingolipid degrading enzymes of the lysosome, since it does not need an activator protein for the physiological turnover of sphingomyelin. The inherited defect of prosaposin and its splice variants (Fig. 6) does not cause a substantial SM accumulation. Purification of human ASM turned out to be rather difficult and attempts failed in many laboratories including ours. A breakthrough was achieved by Lothar Quintern in his thesis work when he realized that the urine from patients with peritonitis or severe organ trauma was a rich source of the enzyme.145,146) The enzyme was purified 25000 fold before peptide sequencing, the search for its cDNA and its sequencing were possible in collaboration with Edward Schuchman.147,148) This allowed us to early identify the molecular basis of acid sphingomyelinase deficiency in a patient with NPD type A149) in parallel to Levran et al.150) and also in patients with type B.101) The generation of ASM deficient knockout mice151) paved the way to study the molecular and cellular pathology of NPD type A and the development of therapeutic approaches for NPD type B.152)
Studies on biosynthesis and intracellular processing of the lysosomal ASM153) identified several molecular forms including secreted proforms with high enzyme activity.88) Functional characterization of its N-glycosylation sites154) and protein domains155,156) revealed that it carries a saposin like domain, binds at acidic pH values to anionic surfaces of BMP containing vesicular membranes and catabolizes membrane bound SM to ceramide and phosphorylcholine,155) even in the absence of SAPs.
In the presence of detergents, it also exhibits some phospholipase C activity cleaving PG and PC,145) an observation which became important for recent studies, using detergent free assay systems with liposomal vesicles carrying the radio labelled SM substrate (or other lipid substrates) as a model of the IM of the late endosomes.157) It became clear that ASM is a nonspecific phospholipase C and that its lipid specificity and enzyme activity are regulated by membrane lipids of the vesicular surface (see section 12). ASM is a very active but labile enzyme having a fast turnover in the lysosomal compartment,153) which is tremendously increased by cationic CADs (cationic amphiphilic drugs) like desipramine.158) In vitro studies at endolysosomal pH values show a strong electrostatic binding of cationic ASM to negatively charged vesicles doped with BMP.159) Desipramine is endocytosed by cultured cells and compensates the negative surface charge of IMs, reducing the electrostatic binding of proteins to the vesicular surfaces. ASM is released and proteolytically degraded.156,158) In general, CADs will weaken the electrostatic interaction between lysosomal proteins and luminal lysosomal vesicles and thereby induce a phospholipidosis.160,161)
11. Lysosomal acid ceramidase and Farber disease
The last big protein contamination, which was separated by Lothar Quintern from ASM during its purification, turned out to be acid ceramidase (AC)145). This allowed purification, structural analysis and characterization of AC,162) the cloning of its cDNA and for the first time the identification of the molecular defect in a patient with Farber disease.162–164) The enzyme appears to be rather slow and cleaves ceramide to sphingosine and fatty acid at the surface of lipid vesicles mimicking IMs of the lysosomes. The surface reaction is reversible164,165) and interfacially regulated by membrane lipids and saposins.113) The cloning of the cDNA and genomic sequences encoding the murine AC166) allowed its insertional mutagenesis of mouse AC.167) It led to early embryonic lethality, demonstrating the importance of AC for embryonic development. At that time, we already knew that sphingosine is not an intermediate in de novo sphingolipid biosynthesis.168,169) Mammalian cells generate ceramide by dehydrogenation of dihydroceramide which is formed by de novo biosynthesis at the ER. After lysosomal degradation of sphingolipids to ceramide, the latter is hydrolyzed by AC to fatty acid and free sphingosine. The latter is the direct precursor of sphingosine-1-phosphate, an important regulator and stimulator of cellular growth, mobility and survival (reviewed in ref. 170). It may well be that a deficiency of sphingosine-1-phosphate contributes to the early embryonic lethality observed in AC deficient mice embryos.167)
12. NPC and an emerging role of ASM in endosomal lipid sorting
Niemann-Pick disease type C (NPC) is a complex neurodegenerative lipid storage disease characterized in systemic tissues by the accumulation of unesterified cholesterol, sphingomyelin, some glycolipids and a broad range of other lipids in the late endolysosomal compartment.171) The disease is caused by mutations in either of the genes of the cholesterol binding proteins, NPC-1 or NPC-2, which lead to impaired cholesterol transport out of the late endosomes. Cells can take up cholesterolester e.g. as components of low-density lipoprotein (LDL) via receptor mediated endocytosis. In the endosomal compartments, they are hydrolyzed to fatty acid and cholesterol.172) Since cholesterol cannot be degraded in the lysosome, it is rapidly transported out of the late endosome to induce homeostatic responses by downward regulation of the de novo synthesis of the LDL-receptor, thus regulating the cellular cholesterol uptake and de novo synthesis of cholesterol.173)
Egress of cholesterol from the endosomal system requires the cholesterol-binding proteins, Niemann-Pick C1 (NPC-1) and Niemann-Pick C2 (NPC-2).174) NPC-1 is a late endolysosomal glycoprotein with 13 transmembrane domains175) and NPC-2 is a glycosylated, soluble protein.176) In a proposed model,114,130) soluble NPC-2 removes cholesterol from inner endosomal/lysosomal vesicles and delivers it to NPC-1 in the limiting membrane of endosomes/lysosomes for cholesterol egress from the late endocytic compartments177–179) (Fig. 8). Inherited defects of NPC-1 or NPC-2 can cause an accumulation of cholesterol in the late endosomes and lysosomes. Endosomal cholesterol accumulation triggers an increase of SM and GSL in NPC disease whereas ASM deficiency triggers SM storage and a cholesterol accumulation in Niemann-Pick disease types A and B.180)
As increasing cholesterol levels have a substantial inhibitory effect on the activity of some lysosomal lipid binding and transfer proteins such as Sap-A and -B,110,111) their increase in the lysosomes may well attenuate the turnover of other membrane lipids such as sphingomyelin, neutral glycolipids (e.g. glucosylceramide, lactosylceramide), gangliosides GM3 and GM2,181) BMP,182) and sphingosine,183) causing a traffic jam in the endolysosomal compartment of NPC diseased cells.
Cellular plasma membranes (PMs) are enriched in membrane stabilizing lipids like cholesterol and sphingomyelin. They form short-lived microdomains in cellular membranes,184) reduce the permeability for sodium ions and keep many receptors and ion pumps, e.g. the ATP dependent Na+ and K+ pump at optimal activity.185) As stabilizing lipids they would impede sphingolipid and membrane degradation in the endolysosomal system110,111,114,186) and, therefore, have to be removed during the endocytotic pathway.
For digestion of membrane components, IMs are formed along the endocytotic pathway. They are prepared for degradation by a lipid sorting process, removing membrane stabilizing lipids like cholesterol and sphingomyelin and generating the degradation-stimulating BMP.82,84,114)
Major proteins involved in endosomal lipid sorting at the IMs are NPC-2 and ASM. According to recent studies, both, enzyme activity of ASM and cholesterol transfer activity of NPC-2, are regulated by membrane lipids.114,187)
ASM turned out to be a rather nonspecific phospholipase C. Besides its known substrate sphingomyelin, it also cleaves PG, PC, PA and more than 15 other phospholipids including BMP in a detergent-free liposomal assay system.187) Surprisingly, its activity against vesicle bound lipid substrates is effectively regulated by the lipid composition of the vesicles. Whereas cholesterol inhibits PC hydrolysis, anionic phospholipids, PG and PA derived from the plasma membrane stimulate sphingomyelin hydrolysis by ASM, and BMP –which is generated after IMs are formed– specifically enhances the degradation of PC, PG and other phospholipids.187) These observations suggest a sequence of events for the removal of stabilizing lipids from the IMs of the late endosomes and their final degradation in the lysosomes: Firstly, in the late endosomes, ASM, stimulated by plasma membrane-derived PG, PI, PA and by BMP, degrades SM, PG and other phospholipids of the IMs to ceramide and DAG. Secondly, the disappearance of SM in combination with the generation of Cer, DAG and the anionic BMP enhances the removal of cholesterol from IMs.114,187) Along the further pathway of endocytosis, phospholipase A2 and other lipases will transiently generate substantial amounts of free fatty acids and lysophospholipids. During these processes in the late endosomes, IMs and their bilayer structures will collapse and lose their topology and barrier function. Micellar-like lipid and glycosphingolipid-rich aggregates –still containing hydrophobic protein domains– will be presented to the luminal juice of the lysosomes for further degradation. Complex lipids and other macromolecules are degraded in the lysosomal compartment and their components are released to the cytosol for biosynthetic pathways and energy metabolism. In differentiated cells, glycosphingolipids will be generated mainly by such salvage pathways.188,189)
13. Ganglioside biosynthesis
Glycolipid pattern of cellular surfaces are cell type specific and depend on the stage of differentiation.190–192) They result from coordinated processes involving biosynthesis of these compounds in the ER and Golgi membranes, intracellular transport processes and the constitutive degradation of glycolipids mainly in the endolysosomal compartment.193) De novo biosynthesis of the hydrophobic membrane anchor of sphingolipids takes place in the ER and is controlled by 6 different ceramide synthases.194) The pathway of ceramide formation was mainly worked out in the late 60s.195,196) Unresolved, however, remained the origin of sphingosine formation either by direct dehydrogenation of sphinganine (dihydrosphingosine) or after dehydrogenation of dihydroceramide followed by ceramide hydrolysis. Our analysis showed that sphingosine is not an intermediate of de novo sphingolipid biosynthesis but a product of ceramide hydrolysis.168,197) This implies that most of the sphingosine is generated by the lysosomal acid ceramidase, released from the lysosome and used in the ER for biosynthesis of sphingolipids and sphingosine-1-phosphate, a major signaling molecule for cellular growth and migration.170) In differentiated cells, e.g. neurons, about 70–90% of newly formed sphingolipids are generated by such salvage pathways,188,189) illuminating the importance of lysosomal digestion for cellular biosynthetic pathways. Ceramide and dihydroceramide are the biosynthetic precursors of sphingomyelin, GSL and gangliosides, the major storage compounds in gangliosidoses.193,198)
The first biosynthetic steps leading to the formation of ceramide are controlled by membrane-bound enzymes at the cytosolic face of the ER.169,199)
Formation of lactosylceramide, which is the precursor of the higher gangliosides, occurs on the luminal face of the Golgi membranes.200,201)
Pathways for the biosynthesis of the main neuronal gangliosides had been worked out by the group of Saul Roseman.202–204) (Fig. 9). We wanted to know if the glycosyltransferases of these pathways also need cofactors for full activity as the catabolic enzymes in the lysosome and how the glycosyltransferases of the a- and b-pathways differ in their specificities. We could not find any evidence for the involvement of essential protein cofactors for the biosynthetic steps. However, in detergent free assays, tunicamycin inhibited and anionic membrane lipids, e.g. PG stimulated the biosynthetic rates substantially,205–207) suggesting a regulation of these biosynthetic steps by membrane lipids.
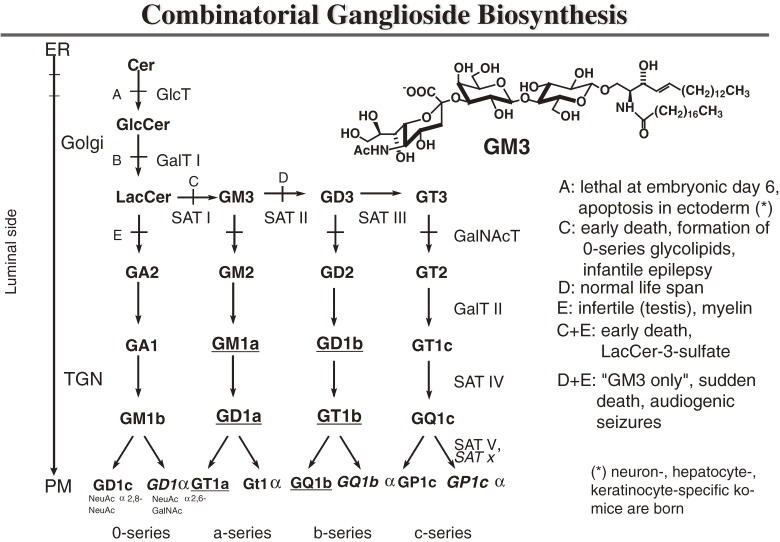
Figure 9.
Scheme of ganglioside biosynthesis. Major gangliosides occurring on neurons in adult mammalian brain are underlined. Enzyme defects in knockout mice are indicated. A, ceramide glucosyltransferase −/−; B, galactosyltransferase I −/−; C, sialyltransferase I −/−; D, sialyltransferase II −/−; E, GalNAc-transferase −/−; “GM3 only” mouse = D + E; “LacCer only” mouse = C + E. GD1α, GT1α, GQ1bα and GP1cα with a sialic acid residue α2,6-glycosidically linked to N-acetylgalactosamine are formed by a yet uncharacterized sialyltransferase, whereas GD1c, GT1a, GQ1b and GP1c are formed by SAT V T (modified after ref. 211).
The interaction of glycosyltransferases and their glycolipid substrates –both bound to the same membrane– however, appeared to occur by diffusion within the plane of the membrane. Therefore, it does not follow the classical Michaelis-Menten kinetics for the interaction of water-soluble substrates and enzymes, but rather a model for 2-dimensional kinetics which we developed for the interaction of membrane-bound enzyme (sialidase) and substrate (ganglioside GD1a).208,209)
Our main interest was to clarify the differences between the glycosyltransferases involved in the biosynthesis of the a-series of gangliosides on one hand, and of the b-series on the other hand (Fig. 9).
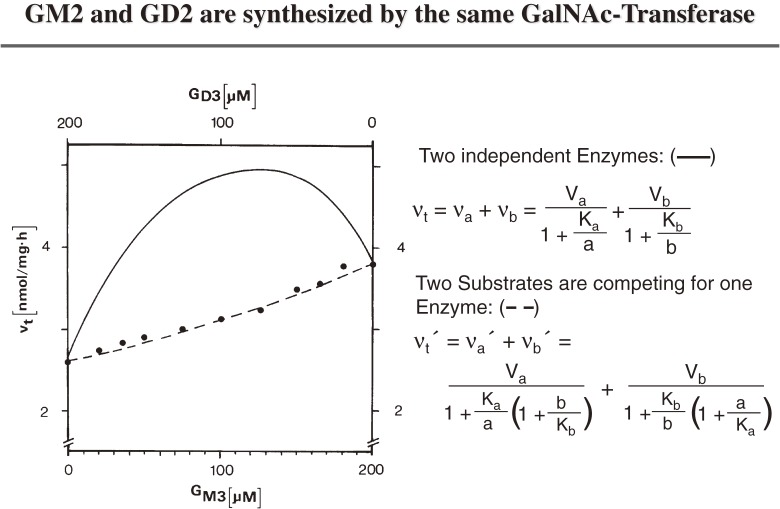
In his thesis work, Gottfried Pohlentz could not detect any significant differences between the two GalNAc transferases, converting the precursors of the a- and b-pathways into gangliosides GM2 and GD2 (Fig. 9). Therefore, I asked him to test if gangliosides GM2 and GD2 are formed by one and the same biosynthetic enzyme. In fact, both substrates, GM3 and GD3, competed for the same active site of one and the same GalNAc transferase210) (Fig. 10).
Figure 10.
Competition between ganglioside GM3 and GD3 in the GalNAc-transferase assay.210) GM3 and GD3 were used as acceptors for GalNAc-transferase in various partial concentrations, keeping total substrate at 200 micro M. Total reaction velocities as experimentally determined (●) or as calculated for the different models are plotted versus the partial substrate concentrations. ——, vt calculated from upper Eq. (two different enzymes); - - - - -, vt calculated from lower Eq. (one enzyme).
Using the same experimental approach given in Fig. 10 for the other glycosyltransferases established the scheme of Combinatorial Ganglioside Biosynthesis (Fig. 9). First, LacCer is sialylated to form the small ganglioside precursors (GM3, GD3, GT3), which are then used by a small number of promiscuous glycosyltransferases to generate a multitude of complex gangliosides. This scheme allows the generation of cell type specific patterns on cell surfaces depending on the availability of precursors, expression of glycosyltransferases and their regulation.
Since enzyme kinetic evidence is usually not accepted as final proof, I contacted Rick Proia at the NIH for a collaboration to test the validity of the scheme by a genetic approach. The generation of mutant mice models with defects in the biosynthetic pathways of ganglioside biosynthesis and their morphological analysis in collaboration with Kinuko Suzuki validated the scheme given in Fig. 9 (review in refs. 211, 212). Mutant mice carrying glycosyltransferase defects often suffered from severe and fatal diseases. Whereas a defect of GD3-synthase still allows a normal life span, a defective GM3-synthase causes an early fatal disease: The absence of all the major neuronal gangliosides triggers the formation of 0-series gangliosides, which are not observed in wild type brain tissue. Their additional synthesis, however, cannot compensate the loss of all the major neuronal gangliosides. A defect of the biosynthetic enzyme, GalNAc transferase, blocking the synthesis of complex glycolipids, causes the myelin sheets to detach from axonal membranes and triggers male infertility.
On the other hand, a block in the catabolism of complex gangliosides also causes a fatal neuronal storage disease in men and mice. However, if the mutant mice with ganglioside storage carry an additional defect in the biosynthesis of complex gangliosides, their neurological functions improve and they have a prolonged life span,213) suggesting that substrate deprivation may be a helpful treatment for sphingolipid storage disease.
A block in glucosylceramide synthesis is lethal already at embryonic day 6.214) It is still unclear why, since cell type specific defects of glucosylceramide synthase in neurons,215) hepatocytes216) or keratinocytes217) still allow embryogenesis and birth of an animal. On the other hand, cultivated mutant teratoma cells with glucosylceramide deficiency have a normal growth rate in cell culture.214) Apparently, glucosylceramide and some of its derived complex glycolipids of the cellular surfaces including the SSEAs190,191) are involved in cellular adhesion and are therefore needed for the development of a multicellular organism.218)
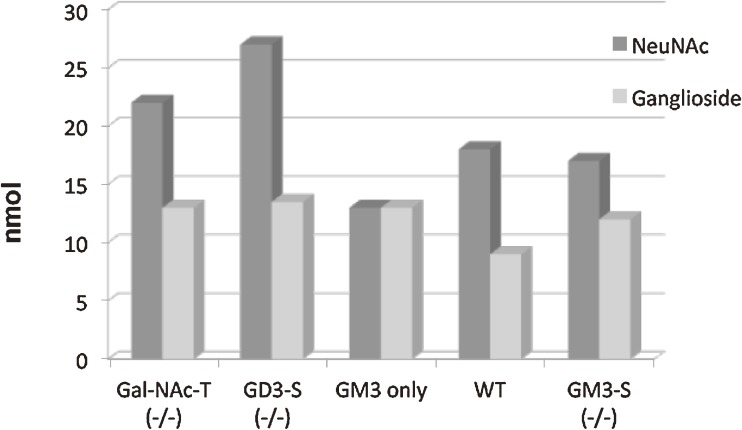
Another surprising finding was the almost unchanged level of total gangliosides in the brains of the various mutant mice. It was still in the range of the wild type (Fig. 11). Apparently, mice with defects in the synthesis of major gangliosides try to keep the overall ganglioside concentration on neuronal surfaces constant. The level of the minor compound GM3 increases in the GM3-only mouse (GalNAc transferase and ganglioside GD3 synthase double knockout mouse) by several orders of magnitude to reach the total ganglioside level of the wild type mice.219)
Figure 11.
Total lipid-bound sialic acid and ganglioside levels in brain tissue of mice with engineered defects in ganglioside biosynthesis.219) Data refer to 10 mg of wet weight brain tissue; abbreviations are given in Fig. 9.
14. Analysis of sphingolipids
At the beginning, our studies were enabled by the development of analytical procedures for the separation and identification of (glyco-) sphingolipids pioneered by Horst Jatzkewitz.2,220,221) For quantification by thin-layer chromatography we developed a sample applicator which became the forerunner of the Linomat now commercially available (from Camag, Switzerland).6,220–223) Later we also used NMR techniques to establish the stereochemical D-erythro configuration of the sphingoid bases in some storage compounds224) and improved mass spectrometric procedures for the analysis of ceramides and some neutral glycosphingolipids.225,226)
15. Chemical biology and the synthesis of sphingolipid analogs
For metabolic and cell biological studies we needed suitable probes and markers which often were not commercially available at the time. Therefore, we developed methods to synthesize labelled sphingolipids for metabolic and enzymatic studies.
-
•
Radiolabeled glycosphingolipids and their use: e.g. refs. 22, 227–233.
-
•
Lysogangliosides as key precursors for the synthesis of labeled or tagged gangliosides.128,234,235)
-
•
Spin labeled sphingolipid analogues carrying NO groups in their acyl residues for ESR measurements to study insertion of gangliosides into membranes of cultured cells.236–238)
- •
-
•
Photosensitive ligands241) to label HexB,242) and GM2AP.243)
-
•
Fluorescent labelled gangliosides were developed to study their biophysical behaviour in lipid bilayers and cellular membranes.184,244,245)
Hydrolysis resistant analogues of GSL and double radiolabeled gangliosides GM1 and GM2 were used for metabolic studies in cultured wild type and mutant cells derived from patients with blocks in ganglioside catabolism. The ganglioside micelles were adsorbed by the cultured human fibroblasts,31,238) ganglioside molecules were slowly inserted into the bilayer of the plasma membrane, endocytosed and most of them catabolized.31) However, a portion of about 5% of the endocytosed gangliosides GM1 and GM2 apparently reached the TGN intact and were glycosylated to more complex gangliosides, mainly ganglioside GD1a.31)
Membrane spanning labeled lipids were synthesized for an uncompromised monitoring of membrane fusion, intermembrane lipid transfer and solubilization of membrane lipids.246) They are needed to analyse the complex functions of saposins (see chapter 8). Besides their role in lysosomal catabolism of sphingolipids and biological membranes and the generation of the water permeability barrier in the skin of land dwelling mammals, they can mediate intermembrane lipid transfer and vesicle fusion. During the development of in vitro assays for membrane fusion, intermembrane lipid transfer and lipid solubilization, it became necessary to develop vesicle markers which cannot be extracted by saposins, as the commercially available ones (e.g. Biotin-PE, NBD-PE and Rhodamine-PE). Therefore, we developed extraction resistant membrane spanning lipids carrying fluorescent labelled headgroups for FRET assays and biotinylated headgroups for magnetic separation of lysosomal vesicles.246)
-
•
General anesthetics and the turnover of SL, SM and GD1a in plasma membranes
In vitro, amphiphilic ganglioside GD1a inserted into isolated neuronal plasma membranes is readily hydrolyzed by the membrane-bound sialidase.209) Surprisingly, its degradation rate was enhanced substantially by lipophilic general anesthetics such as laughing gas (N2O) or halothane, but not that of water-soluble substrates, e.g. of sialyllactose. Membrane fluidity also correlated quantitatively with an increased GD1a hydrolysis when a series of primary alcohols, n-pentanol to n-octanol was used. Interaction of membrane-bound GD1a substrate and the enzyme sialidase occurred mainly within the plane of the membrane, presumably by lateral diffusion.208,209) Modified Michaelis-Menten kinetics for the 2-dimensional interaction of substrate and enzyme were developed which allowed a proper calculation of reaction rates.208)
The increased degradation rate of the lipophilic GD1a paralleled an increase of membrane fluidity.247) General anaesthetics like halothane and Xenon also enhanced membrane fluidity and sphingomyelin degradation by membrane-bound neutral sphingomyelinase of synaptosomal plasma membranes from calf brain.248) A significant increase of SM degradation was already observed at clinical concentrations, increased halothane concentrations stimulated SM hydrolysis up to 50 fold.248)
The molecular basis of these observations –possibly changes in the microdomain structure of the membranes– was never clarified. However, new biophysical methods became available recently to approach this interesting phenomenon.
16. Acknowledgements and outlook
I like to thank my students and coworkers who worked enthusiastically and hard to uncover some of the secrets surrounding the role of sphingolipids in the life of cells and men. During our long trip, some biochemical and cell biological concepts became visible, e.g. the lipid phase problem involving the complex functions of lysosomal activator proteins, the role of intralysosomal membranes in lipid and membrane degradation, and metabolic principles such as the combinatorial ganglioside biosynthesis.
We are grateful for the productive collaborations with external groups, whose expertise and endeavour allowed to tackle these and other questions (Kuni and Kinuko Suzuki, Rick Proia, Al Merrill, Marie Therese Vanier, Ed Schuchman, Heinz Egge, Wolfram Saenger, Walt Holleran, Richard R. Schmidt, Klaus Harzer, Derek Marsh, Volker Herzog and others). These collaborations contributed to the discovery and analysis of several rare inherited sphingolipid storage diseases (gangliosidoses, Niemann-Pick and Farber disease and activator protein deficiencies). However, during our journey more questions came up than answers, e.g. on the regulation and function of sphingolipids in biological membranes. Also their cellular metabolism, intracellular trafficking and the development of therapeutic approaches for sphingolipidoses remain wide open areas for future research.
For financial support I thank the University of Bonn, the Max-Planck-Society, the Humboldt Foundation, the DAAD, the Fonds der Chemischen Industrie and especially the German Research Foundation (DFG) for longstanding support of our research.
Abbreviations
- AC
acid ceramidase
- ASA
arylsulfatase A
- ASM
acid sphingomyelinase
- BMP
bis(monoacylglycero)phosphate
- CAD
cationic amphiphilic drug
- Cer
ceramide
- Chol
cholesterol
- DAG
diacylglycerol
- GM2AP
Ganglioside GM2 activator protein
- GSL
glycosphingolipid
- Hex A, B, S
β-N-acetylhexosaminidases A, B, S
- IAI
infantile amaurotic idiocy
- IM
inner (luminal) membrane
- LLBPs
lysosomal lipid binding proteins
- PA
phosphatidic acid
- PC
phosphatidylcholine
- PE
phosphatidylethanolamine
- PG
phosphatidylglycerol
- SAP
sphingolipid activator proteins
- Sap
saposin
- SM
sphingomyelin
- TSD
Tay-Sachs disease
Profile
Konrad Sandhoff was born in Berlin, Germany, in 1939. He studied Chemistry at the Ludwig-Maximilians-University in Munich, where he received his PhD in 1965.His research career started at the Max-Planck-Institute for Psychiatry in the lab of Horst Jatzkewitz, Dept. of Neurochemistry, with short stops in the labs of Saul Roseman (Johns Hopkins University in Baltimore) and Ruth Arnon (Weizmann Institute in Rehovot). In 1979 he became a full professor for Biochemistry at the Kekulé-Institute in Bonn, Germany.
He gave the first description of GM1 gangliosidosis, and identified the molecular defects in Tay-Sachs disease and in three other newly discovered GM2-gangliosidoses: variant 0 (now known as Sandhoff disease), variant B1 and variant AB. He proposed intraluminal vesicles in endosomes and lysosomes as sites of cellular membrane digestion and established the so-called threshold theory as basis for the different clinical forms of lysosomal storage diseases. Synthesis of fluorescent, radiolabelled and biotinylated (glyco-) sphingolipids was used to study their biosynthetic pathways and cellular turnover.
He discovered omega hydroxylated and acylated glucosylceramides with acyl chains of up to 36 carbon atoms as essential factors for the formation of the water permeability barrier of the human skin. The purification and characterization of human acid sphingomyelinase and acid ceramidase was achieved in his laboratory, together with the characterization of the first mutations as cause for Niemann-Pick disease, type A, and Farber disease.
He was Dean of the Science Faculty (1992–1994), and since 2007 Senior Professor at the LIMES Institute of the University of Bonn. He is a member of different scientific organizations, for example the Gesellschaft Deutscher Naturforscher und Ärzte (President 2005–2006) or the Society for Biochemistry and Molecular Biology, GBM (President from 1999–2001), EMBO, the German Academy, Leopoldina, and was chairman of the Advanced Research Group (SFB) on Glycoconjugates and Structures of Cell Surfaces from 1991–2002.
Konrad Sandhoff was laurelled among others with the Shield of the Medical Faculty, University of Tokyo (1973); the Carl-Duisberg-Prize (1976) and the Richard-Kuhn-Medal (1992) of the GDCh, Chemical Society of Germany; the Heinrich-Wieland-Prize 1979; Honorary Membership of the ASBMB (1992); the K. J. Zülch Prize (1998) and the Research Award (1999) of the Max-Planck-Society; the Mendel-Medal of the Leopoldina (2001); Johns-Hopkins Society of Scholars Membership (2001); the Robert-Pfleger-Prize (1994); the International Glycoconjugate Organization Award 2005; the Otto-Warburg Medal of the GBM (2006); and the European Lipid Science Award (2008).
References
- 1).Jatzkewitz H. (1958) Zwei Typen von Cerebrosid-Schwefelsäureestern als sog. Prälipoide und Speichersubstanzen bei der Leukodystrophy, Typ Scholz (Metachromatische Form der diffusen Sklerose). Hoppe-Seyler’s Z. Physiol. Chem. 311, 279–282 [PubMed] [Google Scholar]
- 2).Jatzkewitz H. (1964) Eine neue Methode zur quantitativen Ultramikrobestimmung der Sphingolipoide aus Gehirn. Hoppe-Seyler’s Z. Physiol. Chem. 336, 25–39 [DOI] [PubMed] [Google Scholar]
- 3).Jatzkewitz H., Mehl E. (1969) Cerebroside-sulphatase and arylsulphatase A deficiency in metachromatic leukodystrophy (ML). J. Neurochem. 16, 19–28 [DOI] [PubMed] [Google Scholar]
- 4).Sandhoff, K. (1965) Die Amaurotische Idiotie des Menschen als Störung im Glykosphingolipidstoffwechsel. Thesis, University of Munich. [Google Scholar]
- 5).Jatzkewitz H., Sandhoff K. (1963) On a biochemically special form of infantile amaurotic idiocy. Biochim. Biophys. Acta 70, 354–356 [DOI] [PubMed] [Google Scholar]
- 6).Jatzkewitz H., Pilz H., Sandhoff K. (1965) Quantitative Bestimmungen von Gangliosiden und ihren neuraminsäurefreien Derivaten bei infantilen, juvenilen und adulten Formen der Amaurotischen Idiotie und einer spätinfantilen biochemischen Sonderform. J. Neurochem. 12, 135–144 [DOI] [PubMed] [Google Scholar]
- 7).Klenk E. (1937) Die Fettstoffe des Gehirns bei Amaurotischer Idiotie und Niemann-Pick’scher Krankheit. Ber. Ges. Physiol. 96, 659–660 [Google Scholar]
- 8).Klenk E. (1939) Niemann-Pick’sche Krankheit und Amaurotische Idiotie. Hoppe-Seyler’s Z. Physiol. Chem. 262, 128–143 [Google Scholar]
- 9).Klenk E. (1942) Über die Ganglioside, eine neue Gruppe von zuckerhaltigen Gehirnlipoiden. Hoppe-Seyler’s Z. Physiol. Chem. 273, 76–86 [Google Scholar]
- 10).Klenk E. (1942) Über die Ganglioside des Gehirns bei der infantilen amaurotischen Idiotie vom Typ Tay-Sachs. Ber. Dtsch. Chem. Ges. 75, 1632–1636 [DOI] [PubMed] [Google Scholar]
- 11).Kuhn R., Wiegandt H. (1963) Die Konstitution der Ganglio-N-tetraose und des Gangliosids GI. Chem. Ber. 96, 866–880 [Google Scholar]
- 12).Svennerholm L. (1962) The chemical structure of normal human brain and Tay-Sachs gangliosides. Biochem. Biophys. Res. Commun. 9, 436–441 [DOI] [PubMed] [Google Scholar]
- 13).Makita A., Yamakawa T. (1963) The glycolipids of the brain of Tay-Sachs’ Disease.—the chemical structures of a globoside and main ganglioside. Jpn. J. Exp. Med. 33, 361–368 [PubMed] [Google Scholar]
- 14).Ledeen R., Salsman K. (1965) Structure of the Tay-Sachs-Ganglioside. Biochemistry 4, 2225–2233 [Google Scholar]
- 15).Terry R.D., Korey S.R. (1960) Membranous cytoplasmic granules in infantile amaurotic idiocy. Nature 188, 1000–1002 [DOI] [PubMed] [Google Scholar]
- 16).Terry R.D., Weiss M. (1963) Studies in Tay-Sachs disease: II Ultrastructure of the cerebrum. J. Neuropathol. Exp. Neurol. 22, 18–55 [DOI] [PubMed] [Google Scholar]
- 17).Samuels S., Korey S.R., Gonatas J., Terry R.D. (1963) Studies in Tay-Sachs-Disease. IV Membranous cytoplasmic bodies. J. Neuropathol. Exp. Neurol. 22, 81–97 [PubMed] [Google Scholar]
- 18).Sandhoff K., Wässle W. (1971) Anreicherung und Charakterisierung zweier Formen der menschlichen N-Acetyl-β-D-hexosaminidase. Hoppe-Seyler’s Z. Physiol. Chem. 352, 1119–1133 [PubMed] [Google Scholar]
- 19).Robinson D., Stirling J.L. (1968) N-Acetyl-β-glucosaminidases in human spleen. Biochem. J. 107, 321–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Sandhoff K. (1968) Auftrennung der Säuger-N-Acetyl-β-D-hexosaminidase in multiple Formen durch Elektrofokussierung. Hoppe-Seyler’s Z. Physiol. Chem. 349, 1095–1098 [PubMed] [Google Scholar]
- 21).Sandhoff K. (2001) The GM2-gangliosidoses and the elucidation of the β-hexosaminidase system. Adv. Genet. 44, 67–91 [DOI] [PubMed] [Google Scholar]
- 22).Sandhoff K. (1970) The hydrolysis of Tay-Sachs ganglioside (TSG) by human N-acetyl-β-D-hexosaminidase A. FEBS Lett. 11, 342–344 [DOI] [PubMed] [Google Scholar]
- 23).Sandhoff K. (1973) Multiple human hexosaminidases. Birth Defects Orig. Artic. Ser. 9, 214–222 [PubMed] [Google Scholar]
- 24).Srivastava S.K., Beutler E. (1973) Hexomsaminidase-A and hexosaminidase-B: studies in Tay-Sachs’ and Sandhoff’s disease. Nature 241, 463. [DOI] [PubMed] [Google Scholar]
- 25).Sandhoff, K., Conzelmann, E., Neufeld, E.F., Kaback, M.M. and Suzuki, K. (1989) The GM2 Gangliosidosis. The Metabolic Basis of Inherited Disease (eds. Scriver, C., Beaudet, A.L., Sly, W.S., and Valle, D.). 6th ed. David Mc. Graw Hill, N.Y., Vol. II, pp. 1807–1839. [Google Scholar]
- 26).Geiger B., Arnon R., Sandhoff K. (1977) Immunochemical and biochemical investigation of hexosaminidase S. Am. J. Hum. Genet. 29, 508–522 [PMC free article] [PubMed] [Google Scholar]
- 27).Hepbildikler S.T., Sandhoff R., Kölzer M., Proia R.L., Sandhoff K. (2002) Physiological substrates for human lysosomal β-hexosaminidase S. J. Biol. Chem. 277, 2562–2572 [DOI] [PubMed] [Google Scholar]
- 28).Conzelmann E., Sandhoff K., Nehrkorn H., Geiger B., Arnon R. (1978) Purification, biochemical and immunological characterisation of hexosaminidase A from variant AB of infantile GM2 gangliosidosis. Eur. J. Biochem. 84, 27–33 [DOI] [PubMed] [Google Scholar]
- 29).Conzelmann E., Sandhoff K. (1978) AB variant of infantile GM2 gangliosidosis: deficiency of a factor necessary for stimulation of hexosaminidase A-catalyzed degradation of ganglioside GM2 and glycolipid GA2. Proc. Natl. Acad. Sci. U.S.A. 75, 3979–3983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Conzelmann E., Sandhoff K. (1979) Purification and characterization of an activator protein for the degradation of glycolipids GM2 and GA2 by hexosaminidase A. Hoppe-Seyler’s Z. Physiol. Chem. 360, 1837–1849 [DOI] [PubMed] [Google Scholar]
- 31).Sonderfeld S., Conzelmann E., Schwarzmann G., Burg J., Hinrichs U., Sandhoff K. (1985) Incorporation and metabolism of ganglioside GM2 in skin fibroblasts from normal and GM2 gangliosidosis subjects. Eur. J. Biochem. 149, 247–255 [DOI] [PubMed] [Google Scholar]
- 32).Conzelmann E., Burg J., Stephan G., Sandhoff K. (1982) Complexing of glycolipids and their transfer between membranes by the activator protein for degradation of lysosomal ganglioside GM2. Eur. J. Biochem. 123, 455–464 [DOI] [PubMed] [Google Scholar]
- 33).Glombitza G.J., Becker E., Kaiser H.W., Sandhoff K. (1997) Biosynthesis, processing, and intracellular transport of GM2 activator protein in human epidermal keratinocytes. The lysosomal targeting of the GM2 activator is independent of a mannose-6-phosphate signal. J. Biol. Chem. 272, 5199–5207 [DOI] [PubMed] [Google Scholar]
- 34).Schütte C.G., Lemm T., Glombitza G.J., Sandhoff K. (1998) Complete localization of disulfide bonds in GM2 activator protein. Protein Sci. 7, 1039–1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35).Wright C.S., Li S.-C., Rastinejad F. (2000) Crystal structure of human GM2-activator protein with a novel β-cup topology. J. Mol. Biol. 304, 411–422 [DOI] [PubMed] [Google Scholar]
- 36).Wendeler M., Hoernschemeyer J., Hoffmann D., Kolter T., Schwarzmann G., Sandhoff K. (2004) Photoaffinity labelling of the human GM2-activator protein. Eur. J. Biochem. 271, 614–627 [DOI] [PubMed] [Google Scholar]
- 37).Wendeler M., Werth N., Maier T., Schwarzmann G., Kolter T., Schoeniger M., Hoffman D., Lemm T., Saenger W., Sandhoff K. (2006) The enzyme-binding region of human GM2-activator protein. FEBS J. 273, 982–991 [DOI] [PubMed] [Google Scholar]
- 38).Werth N., Schuette C.G., Wilkening G., Lemm T., Sandhoff K. (2001) Degradation of membrane-bound ganglioside GM2 by β-hexosaminidase A. Stimulation by GM2 activator protein and lysosomal lipids. J. Biol. Chem. 276, 12685–12690 [DOI] [PubMed] [Google Scholar]
- 39).Wilkening G., Linke T., Uhlhorn-Dierks G., Sandhoff K. (2000) Degradation of membrane-bound ganglioside GM1. Stimulation by bis(monoacylglycero)phosphate and the activator proteins SAP-B and GM2-AP. J. Biol. Chem. 275, 35814–35819 [DOI] [PubMed] [Google Scholar]
- 40).Wendeler M., Lemm T., Weisgerber J., Hoernschemeyer J., Bartelsen O., Schepers U., Sandhoff K. (2003) Expression of recombinant human GM2-activator protein in insect cells: purification and characterization by mass spectrometry. Protein Expr. Purif. 27, 259–266 [DOI] [PubMed] [Google Scholar]
- 41).Anheuser, S. (2011) Entwicklung eines kombinierten Lipidtransfer- und Membranfusions-Assays zur Untersuchung membranaktiver Proteine. Thesis, Universität Bonn. [Google Scholar]
- 42).Goldmann J., Yamanaka T., Rapin I., Adachi M., Suzuki K., Suzuki K. (1980) The AB-Variant of GM2-gangliosidosis. Clinical. biochemical and pathological studies of two patients. Acta Neuropathol. 52, 189–202 [DOI] [PubMed] [Google Scholar]
- 43).Li S., Hirabayashi Y.Y., Li Y.-T. (1981) A new variant of type-AB GM2 gangliosidosis. Biochem. Biophys. Res. Commun. 101, 479–485 [DOI] [PubMed] [Google Scholar]
- 44).Hirabayashi Y., Li Y.-T., Li S. (1983) The protein activator specific for the encymic hydrolysis of GM2 ganglioside in normal human brain and in brains of three types of GM2 gangliosidosis. J. Neurochem. 40, 168–175 [DOI] [PubMed] [Google Scholar]
- 45).Kytzia H.J., Sandhoff K. (1985) Evidence for two different active sites on human β-hexosaminidase A. Interaction of GM2 activator protein with β-hexosaminidase A. J. Biol. Chem. 260, 7568–7572 [PubMed] [Google Scholar]
- 46).Kresse H., Fuchs W., Glossel J., Holtfrerich D., Gilberg W. (1981) Liberation of N-acetyl-glucosamine-6-sulfate by human β-N-acetylhexosaminidase A. J. Biol. Chem. 256, 12926–12932 [PubMed] [Google Scholar]
- 47).Kytzia H.J., Hinrichs U., Maire I., Suzuki K., Sandhoff K. (1983) Variant of GM2-gangliosidosis with hexosaminidase A having a severely changed substrate specificity. EMBO J. 2, 1201–1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48).Sonderfeld S., Brendler S., Sandhoff K., Galjaard H., Hoogeveen A.T. (1985) Genetic complementation in somatic cell hybrids of four variants of infantile GM2 gangliosidosis. Hum. Genet. 71, 196–200 [DOI] [PubMed] [Google Scholar]
- 49).Hasilik A., von Figura K., Conzelmann E., Nehrkorn H., Sandhoff K. (1982) Lysosomal enzyme precursors in human fibroblasts. Activation of cathepsin D precursor in vitro and activity of β-hexosaminidase A precursor towards ganglioside GM2. Eur. J. Biochem. 125, 317–321 [DOI] [PubMed] [Google Scholar]
- 50).Escola J. (1961) Über die Prozessausbreitung der amaurotischen Idiotie im Zentralnervensystem in verschiedenen Lebensaltern und Besonderheiten der Spätform gegenüber der Pigmentatrophie. Arch. Psychiatr. Nervenkr. 202, 95–112 [Google Scholar]
- 51).Conzelmann E., Sandhoff K. (1983) Partial enzyme deficiencies: residual activities and the development of neurological disorders. Dev. Neurosci. 6, 58–71 [DOI] [PubMed] [Google Scholar]
- 52).Conzelmann E., Sandhoff K. (1991) Biochemical basis of late-onset neurolipidoses. Dev. Neurosci. 13, 197–204 [DOI] [PubMed] [Google Scholar]
- 53).Leinekugel P., Michel S., Conzelmann E., Sandhoff K. (1992) Quantitative correlation between the residual activity of β-hexosaminidase A and arylsulfatase A and the severity of the resulting lysosomal storage disease. Hum. Genet. 88, 513–523 [DOI] [PubMed] [Google Scholar]
- 54).Kytzia H.J., Hinrichs U., Sandhoff K. (1984) Diagnosis of infantile and juvenile forms of GM2 gangliosidosis variant 0. Residual activities toward natural and different synthetic substrates. Hum. Genet. 67, 414–418 [DOI] [PubMed] [Google Scholar]
- 55).Meivar-Levy I., Horowitz M., Futerman A.H. (1994) Analysis of glucocerebrosidase activity using N-(1-[14C]hexanoyl)-d-erythro-glucosylsphingosine demonstrates a correlation between levels of residual enzyme activity and the type of Gaucher disease. Biochem. J. 303 (Pt. 2), 377–382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56).Graber D., Salvayre R., Levade T. (1994) Accurate differentiation of neuronopathic and nonneuronopathic forms of Niemann-Pick disease by evaluation of the effective residual lysosomal sphingomyelinase activity in intact cells. J. Neurochem. 63, 1060–1068 [DOI] [PubMed] [Google Scholar]
- 57).Kudoh T., Velkoff M.A., Wenger D.A. (1983) Uptake and metabolism of radioactively labeled sphingomyelin in cultured skin fibroblasts from controls and patients with Niemann-Pick disease and other lysosomal storage diseases. Biochim. Biophys. Acta 754, 82–92 [DOI] [PubMed] [Google Scholar]
- 58).Igisu H., Suzuki K. (1984) Progressive accumulation of toxic metabolite in a genetic leukodystrophy. Science 224, 753–755 [DOI] [PubMed] [Google Scholar]
- 59).Nilsson O., Månsson J.E., Håkansson G., Svennerholm L. (1982) The occurrence of psychosine and other glycolipids in spleen and liver from the three major types of Gaucher’s disease. Biochim. Biophys. Acta 712, 453–463 [DOI] [PubMed] [Google Scholar]
- 60).Purpura D., Suzuki K. (1976) Distortion of neuronal geometry and formation of aberrant synapses in neuronal storage disease. Brain Res. 116, 1–21 [DOI] [PubMed] [Google Scholar]
- 61).Sandhoff K., Jatzkewitz H. (1964) Über den enzymatischen Abbau von N-acetylneuraminsäure-freien Gangliosidresten (Ceramid-oligosacchariden). Hoppe-Seyler’s Z. Physiol. Chem. 338, 281–285 [DOI] [PubMed] [Google Scholar]
- 62).Mehl E., Jatzkewitz H. (1964) Eine Cerebrosidsulfatase aus Schweineniere. Hoppe-Seyler’s Z. Physiol. Chem. 339, 260–276 [PubMed] [Google Scholar]
- 63).Austin J., Balasubramantan A., Pattabtraman T., Basu D., Bachhawat B. (1963) A controlled study of enzymatic activities in three human disorders of glycolipid metabolism. J. Neurochem. 10, 805. [DOI] [PubMed] [Google Scholar]
- 64).Stevens R.L., Fluharty A.L., Kihara H., Kaback M.M., Shapiro L.J., Marsh B., Sandhoff K., Fischer G. (1981) Cerebroside sulfatase activator deficiency induced metachromatic leukodystrophy. Am. J. Hum. Genet. 33, 900–906 [PMC free article] [PubMed] [Google Scholar]
- 65).Al-Hassnan Z.N., Al Dhalaan H., Patay Z., Faqeih E., Al-Owain M., Al-Duraihem A., Faiyaz-Ul-Haque M. (2009) Sphingolipid activator protein B deficiency: report of 9 Saudi patients and review of the literature. J. Child Neurol. 24, 1513–1519 [DOI] [PubMed] [Google Scholar]
- 66).Schlote W., Harzer K., Christomanou H., Paton B.C., Kustermann-Kuhn B., Schmid B., Seeger J., Beudt U., Schuster I., Langenbeck U. (1991) Sphingolipid activator protein 1 deficiency in metachromatic leucodystrophy with normal arylsulphatase A activity. A clinical, morphological, biochemical and immunological study. Eur. J. Pediatr. 150, 584–591 [DOI] [PubMed] [Google Scholar]
- 67).Sandhoff, K., Kolter, T. and Harzer, K. (2001) Sphingolipid activator proteins. The Metabolic and Molecular Bases of Inherited Disease, 8th ed. (eds. Scriver, C., Beaudet, A., Sly, W., Valle, D., Childs, B., Kinzler, K. and Vogelstein, B.). Chap. 134, David Mc Graw Hill, N.Y., pp. 3371–3389. [Google Scholar]
- 68).Vogel A., Schwarzmann G., Sandhoff K. (1991) Glycosphingolipid specificity of the human sulfatide activator protein. Eur. J. Biochem. 200, 591–597 [DOI] [PubMed] [Google Scholar]
- 69).Vogel A., Fürst W., Abo-Hashish M.A., Lee-Vaupel M., Conzelmann E., Sandhoff K. (1987) Identity of the activator proteins for the enzymatic hydrolysis of sulfatide, ganglioside GM1, and globotriaosylceramide. Arch. Biochem. Biophys. 259, 627–638 [DOI] [PubMed] [Google Scholar]
- 70).Zschoche A., Fürst W., Schwarzmann G., Sandhoff K. (1994) Hydrolysis of lactosylceramide by human galactosylceramidase and GM1-β-galactosidase in a detergent-free system and its stimulation by sphingolipid activator proteins, sap-B and sap-C. Activator proteins stimulate lactosylceramide hydrolysis. Eur. J. Biochem. 222, 83–90 [DOI] [PubMed] [Google Scholar]
- 71).Meier E.M., Schwarzmann G., Fürst W., Sandhoff K. (1991) The human GM2 activator protein. A substrate specific cofactor of β-hexosaminidase A. J. Biol. Chem. 266, 1879–1887 [PubMed] [Google Scholar]
- 72).Mraz W., Fischer G., Jatzkewitz H. (1976) Low molecular weight proteins in secondary lysosomes as activators of different sphingolipid hydrolases. FEBS Lett. 67, 104–109 [DOI] [PubMed] [Google Scholar]
- 73).Gärtner S., Conzelmann E., Sandhoff K. (1983) Activator protein for the degradation of globotriaosylceramide by human α-galactosidase. J. Biol. Chem. 258, 12378–12385 [PubMed] [Google Scholar]
- 74).Li S.C., Sonnino S., Tettamanti G., Li Y.T. (1988) Characterization of a nonspecific activator protein for the enzymatic hydrolysis of glycolipids. J. Biol. Chem. 263, 6588–6591 [PubMed] [Google Scholar]
- 75).Wendeler M., Hoernschemeyer J., John M., Werth N., Schoeniger M., Lemm T., Hartmann R., Kessler H., Sandhoff K. (2004) Expression of the GM2-activator protein in the methylotrophic yeast Pichia pastoris, purification, isotopic labeling, and biophysical characterization. Protein Expr. Purif. 34, 147–157 [DOI] [PubMed] [Google Scholar]
- 76).Sun Y., Witte D.P., Ran H., Zamzow M., Barnes S., Cheng H., Han X., Williams M.T., Skelton M.R., Vorhees C.V., Grabowski G.A. (2008) Neurological deficits and glycosphingolipid accumulation in saposin B deficient mice. Hum. Mol. Genet. 17, 2345–2356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77).Fujita N., Suzuki K., Vanier M.T., Popko B., Maeda N., Klein A., Henseler M., Sandhoff K., Nakayasu H., Suzuki K. (1996) Targeted disruption of the mouse sphingolipid activator protein gene: a complex phenotype, including severe leukodystrophy and wide-spread storage of multiple sphingolipids. Hum. Mol. Genet. 5, 711–725 [DOI] [PubMed] [Google Scholar]
- 78).Matsuda J., Vanier M., Saito Y., Suzuki K., Suzuki K. (2001) Dramatic phenotypic improvement during pregnancy in a genetic leukodystrophy: estrogen appears to be a critical factor. Hum. Mol. Genet. 10, 2709–2715 [DOI] [PubMed] [Google Scholar]
- 79).Yoneshige A., Suzuki K., Matsuda J. (2010) A mutation in the saposin C domain of the sphingolipid activator protein (Prosaposin) gene causes neurodegenerative disease in mice. J. Neurosci. Res. 88, 2118–2134 [DOI] [PubMed] [Google Scholar]
- 80).Matsuda J., Yoneshige A., Suzuki K. (2007) The function of sphingolipids in the nervous system: lessons learnt from mouse models of specific sphingolipid activator protein deficiencies. J. Neurochem. 103 (Suppl. 1), 32–38 [DOI] [PubMed] [Google Scholar]
- 81).Kolter T., Winau F., Schaible U.E., Leippe M., Sandhoff K. (2005) Lipid-binding proteins in membrane digestion, antigen presentation, and antimicrobial defense. J. Biol. Chem. 280, 41125–41128 [DOI] [PubMed] [Google Scholar]
- 82).Kolter T., Sandhoff K. (2005) Principles of lysosomal membrane digestion: stimulation of sphingolipid degradation by sphingolipid activator proteins and anionic lysosomal lipids. Annu. Rev. Cell Dev. Biol. 21, 81–103 [DOI] [PubMed] [Google Scholar]
- 83).Kolter T., Sandhoff K. (2010) Lysosomal degradation of membrane lipids. FEBS Lett. 584, 1700–1712 [DOI] [PubMed] [Google Scholar]
- 84).Schulze H., Sandhoff K. (2011) Lysosomal lipid storage diseases. Cold Spring Harb. Perspect. Biol. 3, 287–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85).Schuette C.G., Pierstorff B., Huettler S., Sandhoff K. (2001) Sphingolipid activator proteins: proteins with complex functions in lipid degradation and skin biogenesis. Glycobiology 11, 81R–90R [DOI] [PubMed] [Google Scholar]
- 86).Fürst W., Macheleidt W., Sandhoff K. (1988) The precursor of sulfatide activator protein is processed to three different proteins. Biol. Chem. Hoppe-Seyler 369, 317–328 [DOI] [PubMed] [Google Scholar]
- 87).O’Brien J.S., Kretz K.A., Dewji N., Wenger D.A., Esch F., Fluharty A.L. (1988) Coding of 2 sphingolipid activator proteins (Sap-1 and Sap-2) by same genetic-locus. Science 241, 1098–1101 [DOI] [PubMed] [Google Scholar]
- 88).Ferlinz K., Hurwitz R., Vielhaber G., Suzuki K., Sandhoff K. (1994) Occurrence of two molecular forms of human acid sphingomyelinase. Biochem. J. 301, 855–862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89).Ferlinz K., Hurwitz R., Weiler M., Suzuki K., Sandhoff K., Vanier M.T. (1995) Molecular analysis of the acid sphingomyelinase deficiency in a family with an intermediate form of Niemann-Pick disease. Am. J. Hum. Genet. 56, 1343–1349 [PMC free article] [PubMed] [Google Scholar]
- 90).Henseler M., Klein A., Glombitza G.J., Suzuki K., Sandhoff K. (1996) Expression of the three alternative forms of the sphingolipid activator protein precursor in baby hamster kidney cells and functional assays in a cell culture system. J. Biol. Chem. 271, 8416–8423 [DOI] [PubMed] [Google Scholar]
- 91).Holtschmidt H., Sandhoff K., Fürst W., Kwon H.Y., Schnabel D., Suzuki K. (1991) The organization of the gene for the human cerebroside sulfate activator protein. FEBS Lett. 280, 267–270 [DOI] [PubMed] [Google Scholar]
- 92).Holtschmidt H., Sandhoff K., Kwon H.Y., Harzer K., Nakano T., Suzuki K. (1991) Sulfatide activator protein. Alternative splicing that generates three mRNAs and a newly found mutation responsible for a clinical disease. J. Biol. Chem. 266, 7556–7560 [PubMed] [Google Scholar]
- 93).Klein A., Henseler M., Klein C., Suzuki K., Harzer K., Sandhoff K. (1994) Sphingolipid activator protein D (sap-D) stimulates the lysosomal degradation of ceramide in vivo. Biochem. Biophys. Res. Commun. 200, 1440–1448 [DOI] [PubMed] [Google Scholar]
- 94).Nakano T., Sandhoff K., Stumper J., Christomanou H., Suzuki K. (1989) Structure of full-length cDNA coding for sulfatide activator, a Co-β-glucosidase and two other homologous proteins: two alternate forms of the sulfatide activator. J. Biochem. 105, 152–154 [DOI] [PubMed] [Google Scholar]
- 95).Sandhoff K., van Echten G., Schröder M., Schnabel D., Suzuki K. (1992) Metabolism of glycolipids: the role of glycolipid-binding proteins in the function and pathobiochemistry of lysosomes. Biochem. Soc. Trans. 20, 695–699 [DOI] [PubMed] [Google Scholar]
- 96).Schnabel D., Schröder M., Fürst W., Klein A., Hurwitz R., Zenk T., Weber J., Harzer K., Paton B.C., Poulos A., Suzuki K., Sandhoff K. (1992) Simultaneous deficiency of sphingolipid activator proteins 1 and 2 is caused by a mutation in the initiation codon of their common gene. J. Biol. Chem. 267, 3312–3315 [PubMed] [Google Scholar]
- 97).Schröder M., Klima H., Nakano T., Kwon H., Quintern L.E., Gärtner S., Suzuki K., Sandhoff K. (1989) Isolation of a cDNA encoding the human GM2 activator protein. FEBS Lett. 251, 197–200 [DOI] [PubMed] [Google Scholar]
- 98).Schröder M., Schnabel D., Hurwitz R., Young E., Suzuki K., Sandhoff K. (1993) Molecular genetics of GM2-gangliosidosis AB variant: a novel mutation and expression in BHK cells. Hum. Genet. 92, 437–440 [DOI] [PubMed] [Google Scholar]
- 99).Schröder M., Schnabel D., Suzuki K., Sandhoff K. (1991) A mutation in the gene of a glycolipid-binding protein (GM2 activator) that causes GM2-gangliosidosis variant AB. FEBS Lett. 290, 1–3 [DOI] [PubMed] [Google Scholar]
- 100).Tanaka A., Ohno K., Sandhoff K., Maire I., Kolodny E.H., Brown A., Suzuki K. (1990) GM2-gangliosidosis B1 variant: analysis of β-hexosaminidase α gene abnormalities in seven patients. Am. J. Hum. Genet. 46, 329–339 [PMC free article] [PubMed] [Google Scholar]
- 101).Vanier M.T., Ferlinz K., Rousson R., Duthel S., Louisot P., Sandhoff K., Suzuki K. (1993) Deletion of arginine (608) in acid sphingomyelinase is the prevalent mutation among Niemann-Pick disease type B patients from northern Africa. Hum. Genet. 92, 325–330 [DOI] [PubMed] [Google Scholar]
- 102).Vielhaber G., Hurwitz R., Sandhoff K. (1996) Biosynthesis, processing, and targeting of sphingolipid activator protein (SAP) precursor in cultured human fibroblasts. Mannose 6-phosphate receptor-independent endocytosis of SAP precursor. J. Biol. Chem. 271, 32438–32446 [DOI] [PubMed] [Google Scholar]
- 103).Kishimoto Y., Hiraiwa M., O’Brien J.S. (1992) Saposins: structure, function, distribution, and molecular genetics. J. Lipid Res. 33, 1255–1267 [PubMed] [Google Scholar]
- 104).Vaccaro A.M., Salvioli R., Barca A., Tatti M., Ciaffoni F., Maras B., Siciliano R., Zappacosta F., Amoresano A., Pucci P. (1995) Structural analysis of saposin C and B. Complete localization of disulfide bridges. J. Biol. Chem. 270, 9953–9960 [DOI] [PubMed] [Google Scholar]
- 105).Matsuda J., Kido M., Tadano-Aritomi K., Ishizuka I., Tominaga K., Toida K., Takeda E., Suzuki K., Kuroda Y. (2004) Mutation in saposin D domain of sphingolipid activator protein gene causes urinary system defects and cerebellar Purkinje cell degeneration with accumulation of hydroxy fatty acid-containing ceramide in mouse. Hum. Mol. Genet. 13, 2709–2723 [DOI] [PubMed] [Google Scholar]
- 106).Harzer K., Paton B.C., Poulos A., Kustermann-Kuhn B., Roggendorf W., Grisar T., Popp M. (1989) Sphingolipid activator protein deficiency in a 16-week-old atypical Gaucher disease patient and his fetal sibling: biochemical signs of combined sphingolipidoses. Eur. J. Pediatr. 149, 31–39 [DOI] [PubMed] [Google Scholar]
- 107).Burkhardt J.K., Hüttler S., Klein A., Möbius W., Habermann A., Griffiths G., Sandhoff K. (1997) Accumulation of sphingolipids in SAP-precursor (prosaposin)-deficient fibroblasts occurs as intralysosomal membrane structures and can be completely reversed by treatment with human SAP-precursor. Eur. J. Cell Biol. 73, 10–18 [PubMed] [Google Scholar]
- 108).Fürst W., Sandhoff K. (1992) Activator proteins and topology of lysosomal sphingolipid catabolism. Biochim. Biophys. Acta 1126, 1–16 [DOI] [PubMed] [Google Scholar]
- 109).Fischer G., Jatzkewitz H. (1977) The activator of cerebroside sulphatase binding studies with enzyme and substrate demonstrating the detergent function of the activator protein. Biochim. Biophys. Acta 481, 561–572 [DOI] [PubMed] [Google Scholar]
- 110).Locatelli-Hoops S., Remmel N., Klingenstein R., Breiden B., Rossocha M., Schoeniger M., Koenigs C., Saenger W., Sandhoff K. (2006) Saposin A mobilizes lipids from low cholesterol and high bis(monoacylglycerol)phosphate-containing membranes: patient variant Saposin A lacks lipid extraction capacity. J. Biol. Chem. 281, 32451–32460 [DOI] [PubMed] [Google Scholar]
- 111).Remmel N., Locatelli-Hoops S., Breiden B., Schwarzmann G., Sandhoff K. (2007) Saposin B mobilizes lipids from cholesterol-poor and bis(monoacylglycero)phosphate-rich membranes at acidic pH. Unglycosylated patient variant saposin B lacks lipid-extraction capacity. FEBS J. 274, 3405–3420 [DOI] [PubMed] [Google Scholar]
- 112).Winau F., Schwierzeck V., Hurwitz R., Remmel N., Sieling P.A., Modlin R.L., Porcelli S.A., Brinkmann V., Sugita M., Sandhoff K., Kaufmann S.H., Schaible U.E. (2004) Saposin C is required for lipid presentation by human CD1b. Nat. Immunol. 5, 169–171 [DOI] [PubMed] [Google Scholar]
- 113).Linke T., Wilkening G., Sadeghlar F., Mozcall H., Bernardo K., Schuchman E., Sandhoff K. (2001) Interfacial regulation of acid ceramidase activity. Stimulation of ceramide degradation by lysosomal lipids and sphingolipid activator proteins. J. Biol. Chem. 276, 5760–5768 [DOI] [PubMed] [Google Scholar]
- 114).Abdul-Hammed M., Breiden B., Adebayo M.A., Babalola J.O., Schwarzmann G., Sandhoff K. (2010) Role of endosomal membrane lipids and NPC2 in cholesterol transfer and membrane fusion. J. Lipid Res. 51, 1747–1760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115).Doering T., Holleran W.M., Potratz A., Vielhaber G., Elias P.M., Suzuki K., Sandhoff K. (1999) Sphingolipid activator proteins are required for epidermal permeability barrier formation. J. Biol. Chem. 274, 11038–11045 [DOI] [PubMed] [Google Scholar]
- 116).Doering T., Brade H., Sandhoff K. (2002) Sphingolipid metabolism during epidermal barrier development in mice. J. Lipid Res. 43, 1727–1733 [DOI] [PubMed] [Google Scholar]
- 117).Sidransky E., Sherer D.M., Ginns E.I. (1992) Gaucher disease in the neonate: a distinct Gaucher phenotype is analogous to a mouse model created by targeted disruption of the glucocerebrosidase gene. Pediatr. Res. 32, 494–498 [DOI] [PubMed] [Google Scholar]
- 118).Florey O., Overholtzer M. (2012) Autophagy proteins in macroendocytic engulfment. Trends Cell Biol. 22, 374–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119).Delves, P., Martin, S., Burton, D. and Roit, I. (2006) Roit’s Essential Immunology. Blackwell Publishing, Malden, MA. [Google Scholar]
- 120).Hinkovska-Galcheva V., Shayman J.A. (2010) Ceramide-1-phosphate in phagocytosis and calcium homeostasis. Adv. Exp. Med. Biol. 688, 131–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121).Griffiths G., Hoflack B., Simons K., Mellman I., Kornfeld S. (1988) The mannose 6-phosphate receptor and the biogenesis of lysosomes. Cell 52, 329–341 [DOI] [PubMed] [Google Scholar]
- 122).Schwarzmann G., Sandhoff K. (1990) Metabolism and intracellular transport of glycosphingolipids. Biochemistry 29, 10865–10871 [DOI] [PubMed] [Google Scholar]
- 123).Kok J.W., Babia T., Hoekstra D. (1991) Sorting of sphingolipids in the endocytic pathway of HT29 cells. J. Cell Biol. 114, 231–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124).Hopkins C.R., Gibson A., Shipman M., Miller K. (1990) Movement of internalized ligand-receptor complexes along a continuous endosomal reticulum. Nature 346, 335–339 [DOI] [PubMed] [Google Scholar]
- 125).McKanna J.A., Haigler H.T., Cohen S. (1979) Hormone receptor topology and dynamics: morphological analysis using ferritin-labeled epidermal growth factor. Proc. Natl. Acad. Sci. U.S.A. 76, 5689–5693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126).Scriver, C.R., Beaudet, A.L., Sly, W.S. and Valle, D. (1989) The Metabolic Bases of Inherited Disease, 6th ed. David McGraw Hill, New York. [Google Scholar]
- 127).Hiesberger T., Hüttler S., Rohlmann A., Schneider W., Sandhoff K., Herz J. (1998) Cellular uptake of saposin (SAP) precursor and lysosomal delivery by the low density lipoprotein receptor-related protein (LRP). EMBO J. 17, 4617–4625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128).Möbius W., Herzog V., Sandhoff K., Schwarzmann G. (1999) Intracellular distribution of a biotin-labeled ganglioside, GM1, by immunoelectron microscopy after endocytosis in fibroblasts. J. Histochem. Cytochem. 47, 1005–1014 [DOI] [PubMed] [Google Scholar]
- 129).Wollert T., Hurley J.H. (2010) Molecular mechanism of multivesicular body biogenesis by ESCRT complexes. Nature 464, 864–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130).Gallala H.D., Breiden B., Sandhoff K. (2011) Regulation of the NPC2 protein-mediated cholesterol trafficking by membrane lipids. J. Neurochem. 116, 702–707 [DOI] [PubMed] [Google Scholar]
- 131).Möbius W., van Donselaar E., Ohno-Iwashita Y., Shimada Y., Heijnen H.F., Slot J.W., Geuze H.J. (2003) Recycling compartments and the internal vesicles of multivesicular bodies harbor most of the cholesterol found in the endocytic pathway. Traffic 4, 222–231 [DOI] [PubMed] [Google Scholar]
- 132).Eskelinen E.-L., Tanaka Y., Saftig P. (2003) At the acidic edge: emerging functions for lysosomal membrane proteins. Trends Cell Biol. 13, 137–145 [DOI] [PubMed] [Google Scholar]
- 133).Kornfeld S., Mellman I. (1989) The biogenesis of lysosomes. Annu. Rev. Cell Biol. 5, 483–525 [DOI] [PubMed] [Google Scholar]
- 134).Hay, E.D. (1989) Cell Biology of Extracellular Matrix. Plenum Press, New York. [Google Scholar]
- 135).Carlsson S.R., Fukuda M. (1990) The polylactosaminoglycans of human lysosomal membrane glycoproteins lamp-1 and lamp-2. Localization on the peptide backbones. J. Biol. Chem. 265, 20488–20495 [PubMed] [Google Scholar]
- 136).Henning R., Stoffel W. (1973) Glycosphingolipids in lysosomal membranes. Hoppe-Seyler’s Z. Physiol. Chem. 354, 760–770 [DOI] [PubMed] [Google Scholar]
- 137).Giehl A., Lemm T., Bartelsen O., Sandhoff K., Blume A. (1999) Interaction of the GM2-activator protein with phospholipid-ganglioside bilayer membranes and with monolayers at the air-water interface. Eur. J. Biochem. 261, 650–658 [DOI] [PubMed] [Google Scholar]
- 138).Kirkegaard T., Roth A.G., Petersen N.H.T., Mahalka A.K., Olsen O.D., Moilanen I., Zylicz A., Knudsen J., Sandhoff K., Arenz C., Kinnunen P.K., Nylandsted J., Jäättelä M. (2010) Hsp70 stabilizes lysosomes and reverts Niemann-Pick disease-associated lysosomal pathology. Nature 463, 549–553 [DOI] [PubMed] [Google Scholar]
- 139).Tettamanti G. (2004) Ganglioside/glycosphingolipid turnover: new concepts. Glycoconj. J. 20, 301–317 [DOI] [PubMed] [Google Scholar]
- 140).Pick L. (1927) Über die lipoidzellige Splenohepatomegalie typus Niemann-Pick als Stoffwechselerkrankung. Med. Klin. 23, 1483–1486 [Google Scholar]
- 141).Crocker A.C. (1961) The cerebral defect in Tay-Sachs disease and Niemann-Pick disease. J. Neurochem. 7, 69–73 [DOI] [PubMed] [Google Scholar]
- 142).Niemann A. (1914) Ein unbekanntes Krankheitsbild. Jahrb. Kinderheilkd. 79, 1–3 [Google Scholar]
- 143).Klenk E. (1935) Über die Natur der Phosphatide und anderer Lipide des Gehirns und der Leber bei der Niemann-Pick’schen Krankheit. Z. Physiol. Chem. 235, 24–25 [Google Scholar]
- 144).Brady R.O., Kanfer J., Mock M., Fredrickson D. (1966) The metabolism of sphingomyelin. Evidence of an enzymatic deficiency in Niemann-Pick disease. Proc. Natl. Acad. Sci. U.S.A. 55, 367–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145).Quintern L.E., Weitz G., Nehrkorn H., Tager J.M., Schram A.W., Sandhoff K. (1987) Acid sphingomyelinase from human urine: purification and characterization. Biochim. Biophys. Acta 922, 323–336 [DOI] [PubMed] [Google Scholar]
- 146).Quintern L.E., Zenk T.S., Sandhoff K. (1989) The urine from patients with peritonitis as a rich source for purifying human acid sphingomyelinase and other lysosomal enzymes. Biochim. Biophys. Acta 1003, 121–124 [DOI] [PubMed] [Google Scholar]
- 147).Quintern L.E., Schuchman E.H., Levran O., Suchi M., Ferlinz K., Reinke H., Sandhoff K., Desnick R.J. (1989) Isolation of cDNA clones encoding human acid sphingomyelinase: occurrence of alternatively processed transcripts. EMBO J. 8, 2469–2473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148).Schuchman E.H., Suchi M., Takahashi T., Sandhoff K., Desnick R.J. (1991) Human acid sphingomyelinase. Isolation, nucleotide sequence and expression of the full-length and alternatively spliced cDNAs. J. Biol. Chem. 266, 8531–8539 [PubMed] [Google Scholar]
- 149).Ferlinz K., Hurwitz R., Sandhoff K. (1991) Molecular basis of acid sphingomyelinase deficiency in a patient with Niemann-Pick disease type A. Biochem. Biophys. Res. Commun. 179, 1187–1191 [DOI] [PubMed] [Google Scholar]
- 150).Levran O., Desnick R., Schuchman E. (1991) Niemann-Pick disease: A common mutation in Ashkenazi Jewish individuals results in the type A and B forms. Proc. Natl. Acad. Sci. U.S.A. 88, 3748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151).Horinouchi K., Erlich S., Perl D.P., Ferlinz K., Bisgaier C.L., Sandhoff K., Desnick R.J., Stewart C.L., Schuchman E.H. (1995) Acid sphingomyelinase deficient mice: a model of types A and B Niemann-Pick disease. Nat. Genet. 10, 288–293 [DOI] [PubMed] [Google Scholar]
- 152).Schuchman E.H. (2009) The pathogenesis and treatment of acid sphingomyelinase-deficient Niemann-Pick disease. Int. J. Clin. Pharmacol. Ther. 47 (Suppl. 1), S48–S57 [DOI] [PubMed] [Google Scholar]
- 153).Hurwitz R., Ferlinz K., Vielhaber G., Moczall H., Sandhoff K. (1994) Processing of human acid sphingomyelinase in normal and I-cell fibroblasts. J. Biol. Chem. 269, 5440–5445 [PubMed] [Google Scholar]
- 154).Ferlinz K., Hurwitz R., Moczall H., Lansmann S., Schuchman E.H., Sandhoff K. (1997) Functional characterization of the N-glycosylation sites of human acid sphingomyelinase by site-directed mutagenesis. Eur. J. Biochem. 243, 511–517 [DOI] [PubMed] [Google Scholar]
- 155).Linke T., Wilkening G., Lansmann S., Moczall H., Bartelsen O., Weisgerber J., Sandhoff K. (2001) Stimulation of acid sphingomyelinase activity by lysosomal lipids and sphingolipid activator proteins. Biol. Chem. 382, 283–290 [DOI] [PubMed] [Google Scholar]
- 156).Kölzer M., Ferlinz K., Bartelsen O., Hoops S.L., Lang F., Sandhoff K. (2004) Functional characterization of the postulated intramolecular sphingolipid activator protein domain of human acid sphingomyelinase. Biol. Chem. 385, 1193–1195 [DOI] [PubMed] [Google Scholar]
- 157).Ferlinz K., Linke T., Bartelsen O., Weiler M., Sandhoff K. (1999) Stimulation of lysosomal sphingomyelin degradation by sphingolipid activator proteins. Chem. Phys. Lipids 102, 35–43 [DOI] [PubMed] [Google Scholar]
- 158).Hurwitz R., Ferlinz K., Sandhoff K. (1994) The tricyclic antidepressant desipramine causes proteolytic degradation of lysosomal sphingomyelinase in human fibroblasts. Biol. Chem. Hoppe-Seyler 375, 447–450 [DOI] [PubMed] [Google Scholar]
- 159).Kölzer M., Werth N., Sandhoff K. (2004) Interactions of acid sphingomyelinase and lipid bilayers in the presence of the tricyclic antidepressant desipramine. FEBS Lett. 559, 96–98 [DOI] [PubMed] [Google Scholar]
- 160).Lüllmann H., Lüllmann-Rauch R., Wassermann O. (1978) Lipidosis induced by amphiphilic cationic drugs. Biochem. Pharmacol. 27, 1103–1108 [DOI] [PubMed] [Google Scholar]
- 161).Kornhuber J., Muehlbacher M., Trapp S., Pechmann S., Friedl A., Reichel M., Mühle C., Terfloth L., Groemer T.W., Spitzer G.M., Liedl K.R., Gulbins E., Tripal P. (2011) Identification of novel functional inhibitors of acid sphingomyelinase. PLoS ONE 6, e23852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162).Koch J., Gärtner S., Li C.M., Quintern L.E., Bernardo K., Levran O., Schnabel D., Desnick R.J., Schuchman E.H., Sandhoff K. (1996) Molecular cloning and characterization of a full-length complementary DNA encoding human acid ceramidase. Identification of the first molecular lesion causing Farber disease. J. Biol. Chem. 271, 33110–33115 [DOI] [PubMed] [Google Scholar]
- 163).Li C.M., Park J.H., He X., Levy B., Chen F., Arai K., Adler D.A., Disteche C.M., Koch J., Sandhoff K., Schuchman E.H. (1999) The human acid ceramidase gene (ASAH): structure, chromosomal location, mutation analysis, and expression. Genomics 62, 223–231 [DOI] [PubMed] [Google Scholar]
- 164).Moser, H., Linke, T., Femson, A., Levade, T. and Sandhoff, K. (2001) Acid ceramidase deficiency: Farber lipogranulomatosis. In The Metabolic and Molecular Bases of Inherited Disease 8th ed. Chap. 143, pp. 3573–3589. [Google Scholar]
- 165).Okino N., He X., Gatt S., Sandhoff K., Ito M., Schuchman E.H. (2003) The reverse activity of human acid ceramidase. J. Biol. Chem. 278, 29948–29953 [DOI] [PubMed] [Google Scholar]
- 166).Li C.M., Hong S.B., Kopal G., He X., Linke T., Hou W.S., Koch J., Gatt S., Sandhoff K., Schuchman E.H. (1998) Cloning and characterization of the full-length cDNA and genomic sequences encoding murine acid ceramidase. Genomics 50, 267–274 [DOI] [PubMed] [Google Scholar]
- 167).Li C.M., Park J.H., Simonaro C.M., He X., Gordon R.E., Friedman A.H., Ehleiter D., Paris F., Manova K., Hepbildikler S., Fuks Z., Sandhoff K., Kolesnick R., Schuchman E.H. (2002) Insertional mutagenesis of the mouse acid ceramidase gene leads to early embryonic lethality in homozygotes and progressive lipid storage disease in heterozygotes. Genomics 79, 218–224 [DOI] [PubMed] [Google Scholar]
- 168).Rother J., van Echten G., Schwarzmann G., Sandhoff K. (1992) Biosynthesis of sphingolipids: dihydroceramide and not sphinganine is desaturated by cultured cells. Biochem. Biophys. Res. Commun. 189, 14–20 [DOI] [PubMed] [Google Scholar]
- 169).Mandon E.C., Ehses I., Rother J., van Echten G., Sandhoff K. (1992) Subcellular localization and membrane topology of serine palmitoyltransferase, 3-dehydrosphinganine reductase, and sphinganine N-acyltransferase in mouse liver. J. Biol. Chem. 267, 11144–11148 [PubMed] [Google Scholar]
- 170).Maceyka M., Harikumar K.B., Milstien S., Spiegel S. (2012) Sphingosine-1-phosphate signaling and its role in disease. Trends Cell Biol. 22, 50–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171).Patterson, M., Vanier, M., Suzuki, K., Morris, J., Carsteu, E., Neufeld, E., Blanchette-Mackie, J.E. and Pentchev, P.G. (2001) Niemann-Pick disease type C. A lipid trafficking disorder. In The Metabolic Basis of Inherited Disease, Vol. II, 8th ed. (ed. Scriver, C.R. et al.). David Mc. Graw Hill, N.Y., pp. 3611–3633. [Google Scholar]
- 172).Brown M., Goldstein J. (1986) A receptor-mediated pathway for cholesterol homeostasis. Science 232, 34–47 [DOI] [PubMed] [Google Scholar]
- 173).Ikonen E. (2008) Cellular cholesterol trafficking and compartmentalization. Nat. Rev. Mol. Cell Biol. 9, 125–138 [DOI] [PubMed] [Google Scholar]
- 174).Infante R.E., Wang M.L., Radhakrishnan A., Kwon H.J., Brown M.S., Goldstein J.L. (2008) NPC2 facilitates bidirectional transfer of cholesterol between NPC1 and lipid bilayers, a step in cholesterol egress from lysosomes. Proc. Natl. Acad. Sci. U.S.A. 105, 15287–15292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175).Carstea E.D., Morris J.A., Coleman K.G., Loftus S.K., Zhang D., Cummings C., Gu J., Rosenfeld M.A., Pavan W.J., Krizman D.B., Nagle J., Polymeropoulos M.H., Sturley S.L., Ioannou Y.A., Higgins M.E., Comly M., Cooney A., Brown A., Kaneski C.R., Blanchette-Mackie E.J., Dwyer N.K., Neufeld E.B., Chang T.Y., Liscum L., Strauss J.F., 3rd, Ohno K., Zeigler M., Carmi R., Sokol J., Markie D., O’Neill R.R., van Diggelen O.P., Elleder M., Patterson M.C., Brady R.O., Vanier M.T., Pentchev P.G., Tagle D.A. (1997) Niemann-Pick C1 disease gene: homology to mediators of cholesterol homeostasis. Science 277, 228–231 [DOI] [PubMed] [Google Scholar]
- 176).Naureckiene S., Sleat D.E., Lackland H., Fensom A., Vanier M.T., Wattiaux R., Jadot M., Lobel P. (2000) Identification of HE1 as the second gene of Niemann-Pick C disease. Science 290, 2298–2301 [DOI] [PubMed] [Google Scholar]
- 177).Kwon H.J., Abi-Mosleh L., Wang M.L., Deisenhofer J., Goldstein J.L., Brown M.S., Infante R.E. (2009) Structure of N-terminal domain of NPC1 reveals distinct subdomains for binding and transfer of cholesterol. Cell 137, 1213–1224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178).Karten B., Peake K.B., Vance J.E. (2009) Mechanisms and consequences of impaired lipid trafficking in Niemann-Pick type C1-deficient mammalian cells. Biochim. Biophys. Acta 1791, 659–670 [DOI] [PubMed] [Google Scholar]
- 179).Storch J., Xu Z. (2009) Niemann-Pick C2 (NPC2) and intracellular cholesterol trafficking. Biochim. Biophys. Acta 1791, 671–678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180).Vanier M. (1983) Biochemical studies in Niemann-Pick disease: I. Major sphingolipids of liver and spleen. Biochim. Biophys. Acta 750, 178–184 [DOI] [PubMed] [Google Scholar]
- 181).te Vruchte D., Lloyd-Evans E., Veldman R.J., Neville D.C., Dwek R.A., Platt F.M., van Blitterswijk W.J., Sillence D.J. (2004) Accumulation of glycosphingolipids in Niemann-Pick C disease disrupts endosomal transport. J. Biol. Chem. 279, 26167–26175 [DOI] [PubMed] [Google Scholar]
- 182).Kobayashi T., Beuchat M.H., Lindsay M., Frias S., Palmiter R.D., Sakuraba H., Parton R.G., Gruenberg J. (1999) Late endosomal membranes rich in lysobisphosphatidic acid regulate cholesterol transport. Nat. Cell Biol. 1, 113–118 [DOI] [PubMed] [Google Scholar]
- 183).Rodriguez-Lafrasse C., Rousson R., Pentchev P.G., Louisot P., Vanier M.T. (1994) Free sphingoid bases in tissues from patients with type C Niemann-Pick disease and other lysosomal storage disorders. Biochim. Biophys. Acta 1226, 138–144 [DOI] [PubMed] [Google Scholar]
- 184).Eggeling C., Ringemann C., Medda R., Schwarzmann G., Sandhoff K., Polyakova S., Belov V.N., Hein B., von Middendorff C., Schönle A., Hell S.W. (2009) Direct observation of the nanoscale dynamics of membrane lipids in a living cell. Nature 457, 1159–1162 [DOI] [PubMed] [Google Scholar]
- 185).Mouritsen O.G., Zuckermann M.J. (2004) What’s so special about cholesterol? Lipids 39, 1101–1113 [DOI] [PubMed] [Google Scholar]
- 186).Tamboli I.Y., Hampel H., Tien N.T., Tolksdorf K., Breiden B., Mathews P.M., Saftig P., Sandhoff K., Walter J. (2011) Sphingolipid storage affects autophagic metabolism of the amyloid precursor protein and promotes Aβ generation. J. Neurosci. 31, 1837–1849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187).Oninla V.O., Breiden B., Sandhoff K. (2012) Membrane lipids regulate degradation of liposomal sphingomyelin required for cholesterol transfer by NPC2 (In preparation).
- 188).Riboni L., Bassi R., Conti M., Tettamanti G. (1993) Metabolism of exogenous ganglioside GM1 in cultured cerebellar granule cells. The fatty acid and sphingosine moieties formed during degradation are re-used for lipid biosynthesis. FEBS Lett. 322, 257–260 [DOI] [PubMed] [Google Scholar]
- 189).Gillard B., Clement R., Marcus D. (1998) Variations among cell lines in the synthesis of sphingolipids in de novo and recycling pathways. Glycobiology 8, 885–890 [DOI] [PubMed] [Google Scholar]
- 190).Kannagi R., Cochran N.A., Ishigami F., Hakomori S., Andrews P.W., Knowles B.B., Solter D. (1983) Stage-specific embryonic antigens (SSEA-3 and -4) are epitopes of a unique globo-series ganglioside isolated from human teratocarcinoma cells. EMBO J. 2, 2355–2361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191).Eggens I., Fenderson B., Toyokuni T., Dean B., Stroud M., Hakomori S. (1989) Specific interaction between Lex and Lex determinants. A possible basis for cell recognition in preimplantation embryos and in embryonal carcinoma cells. J. Biol. Chem. 264, 9476–9484 [PubMed] [Google Scholar]
- 192).van Echten G., Sandhoff K. (1993) Ganglioside metabolism. Enzymology, topology, and regulation. J. Biol. Chem. 268, 5341–5344 [PubMed] [Google Scholar]
- 193).Kolter T., Sandhoff K. (1999) Sphingolipids—Their metabolic pathways and the pathobiochemistry of neurodegenerative diseases. Angew. Chem. Int. Ed. Engl. 38, 1532–1568 [DOI] [PubMed] [Google Scholar]
- 194).Levy M., Futerman A.H. (2010) Mammalian ceramide synthases. IUBMB Life 62, 347–356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195).Braun P., Snell E. (1968) Biosynthesis of sphingolipid bases. II. Keto intermediates in synthesis of sphingosine and dihydrosphingosine by cell-free extracts of Hansenula ciferri. J. Biol. Chem. 243, 3775–3783 [PubMed] [Google Scholar]
- 196).Stoffel W., LeKim D., Sticht G. (1968) Biosynthesis of dihydrosphingosine in vitro. Hoppe-Seyler’s Z. Physiol. Chem. 349, 664–670 [DOI] [PubMed] [Google Scholar]
- 197).Michel C., van Echten-Deckert G., Rother J., Sandhoff K., Wang E., Merrill A.H., Jr. (1997) Characterization of ceramide synthesis. A dihydroceramide desaturase introduces the 4,5-trans-double bond of sphingosine at the level of dihydroceramide. J. Biol. Chem. 272, 22432–22437 [DOI] [PubMed] [Google Scholar]
- 198).Sandhoff K. (1977) The biochemistry of sphingolipid storage diseases. Angew. Chem. Int. Ed. Engl. 16, 273–285 [DOI] [PubMed] [Google Scholar]
- 199).Michel C., van Echten-Deckert G. (1997) Conversion of dihydroceramide to ceramide occurs at the cytosolic face of the endoplasmic reticulum. FEBS Lett. 416, 153–155 [DOI] [PubMed] [Google Scholar]
- 200).Lannert H., Bunning C., Jeckel D., Wieland F.T. (1994) Lactosylceramide is synthesized in the lumen of the Golgi apparatus. FEBS Lett. 342, 91–96 [DOI] [PubMed] [Google Scholar]
- 201).Lannert H., Gorgas K., Meissner I., Wieland F.T., Jeckel D. (1998) Functional organization of the Golgi apparatus in glycosphingolipid biosynthesis. Lactosylceramide and subsequent glycosphingolipids are formed in the lumen of the late Golgi. J. Biol. Chem. 273, 2939–2946 [DOI] [PubMed] [Google Scholar]
- 202).Kaufman B., Basu S., Roseman S. (1968) Enzymatic synthesis of disialogangliosides from monosialogangliosides by sialyltransferases from embryonic chicken brain. J. Biol. Chem. 243, 5804–5807 [PubMed] [Google Scholar]
- 203).Steigerwald J.C., Basu S., Kaufman B., Roseman S. (1975) Sialic acids. Enzymatic synthesis of Tay-Sachs ganglioside. J. Biol. Chem. 250, 6727–6734 [PubMed] [Google Scholar]
- 204).Roseman S. (1970) The synthesis of complex carbohydrates by multiglycosyltransferase systems and their potential function in intercellular adhesion. Chem. Phys. Lipids 5, 270–297 [DOI] [PubMed] [Google Scholar]
- 205).Yusuf H.K., Pohlentz G., Schwarzmann G., Sandhoff K. (1983) Ganglioside biosynthesis in Golgi apparatus of rat liver. Stimulation by phosphatidylglycerol and inhibition by tunicamycin. Eur. J. Biochem. 134, 47–54 [DOI] [PubMed] [Google Scholar]
- 206).Yusuf H.K., Pohlentz G., Sandhoff K. (1984) Ganglioside biosynthesis in Golgi apparatus: new perspectives on its mechanism. J. Neurosci. Res. 12, 161–178 [DOI] [PubMed] [Google Scholar]
- 207).Yusuf H.K., Pohlentz G., Sandhoff K. (1983) Tunicamycin inhibits ganglioside biosynthesis in rat liver Golgi apparatus by blocking sugar nucleotide transport across the membrane vesicles. Proc. Natl. Acad. Sci. U.S.A. 80, 7075–7079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208).Scheel G., Acevedo E., Conzelmann E., Nehrkorn H., Sandhoff K. (1982) Model for the interaction of membrane-bound substrates and enzymes. Hydrolysis of ganglioside GD1a by sialidase of neuronal membranes isolated from calf brain. Eur. J. Biochem. 127, 245–253 [DOI] [PubMed] [Google Scholar]
- 209).Scheel G., Schwarzmann G., Hoffmann-Bleihauer P., Sandhoff K. (1985) The influence of ganglioside insertion into brain membranes on the rate of ganglioside degradation by membrane-bound sialidase. Eur. J. Biochem. 153, 29–35 [DOI] [PubMed] [Google Scholar]
- 210).Pohlentz G., Klein D., Schwarzmann G., Schmitz D., Sandhoff K. (1988) Both GA2, GM2, and GD2 synthases and GM1b, GD1a, and GT1b synthases are single enzymes in Golgi vesicles from rat liver. Proc. Natl. Acad. Sci. U.S.A. 85, 7044–7048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211).Kolter T., Proia R.L., Sandhoff K. (2002) Combinatorial ganglioside biosynthesis. J. Biol. Chem. 277, 25859–25862 [DOI] [PubMed] [Google Scholar]
- 212).Sandhoff K., Kolter T. (2003) Biosynthesis and degradation of mammalian glycosphingolipids. Philos. Trans. R. Soc. Lond. B Biol. Sci. 358, 847–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213).Liu Y., Wada R., Kawai H., Sango K., Deng C., Tai T., McDonald M.P., Araujo K., Crawley J.N., Bierfreund U., Sandhoff K., Suzuki K., Proia R.L. (1999) A genetic model of substrate deprivation therapy for a glycosphingolipid storage disorder. J. Clin. Invest. 103, 497–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214).Yamashita T., Wada R., Sasaki T., Deng C., Bierfreund U., Sandhoff K., Proia R.L. (1999) A vital role for glycosphingolipid synthesis during development and differentiation. Proc. Natl. Acad. Sci. U.S.A. 96, 9142–9147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215).Jennemann R., Sandhoff R., Wang S., Kiss E., Gretz N., Zuliani C., Martin-Villalba A., Jäger R., Schorle H., Kenzelmann M., Bonrouhi M., Wiegandt H., Gröne H.J. (2005) Cell-specific deletion of glucosylceramide synthase in brain leads to severe neural defects after birth. Proc. Natl. Acad. Sci. U.S.A. 102, 12459–12464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216).Jennemann R., Rothermel U., Wang S., Sandhoff R., Kaden S., Out R., van Berkel T.J., Aerts J.M., Ghauharali K., Sticht C., Gröne H.J. (2010) Hepatic glycosphingolipid deficiency and liver function in mice. Hepatology 51, 1799–1809 [DOI] [PubMed] [Google Scholar]
- 217).Jennemann R., Sandhoff R., Langbein L., Kaden S., Rothermel U., Gallala H., Sandhoff K., Wiegandt H., Gröne H.J. (2007) Integrity and barrier function of the epidermis critically depend on glucosylceramide synthesis. J. Biol. Chem. 282, 3083–3094 [DOI] [PubMed] [Google Scholar]
- 218).Kolter T., Magin T.M., Sandhoff K. (2000) Biomolecule function: no reliable prediction from cell culture. Traffic 1, 803–804 [DOI] [PubMed] [Google Scholar]
- 219).Werth, N. (2004) Untersuchungen zur Biosynthese und zum Abbau von Gangliosiden. Thesis, Universitaet Bonn. [Google Scholar]
- 220).Harzer K., Waessle W., Sandhoff K., Jatzkewitz H. (1968) Densiometrische Mikrobestimmung von Lipiden nach Dünnschicht-Chromatographie des Gesamtlipidextrakts. Z. Anal. Chem. 243, 527–536 [Google Scholar]
- 221).Sandhoff K., Harzer K., Jatzkewitz H. (1968) Densitometrische Mikrobestimmung von Gangliosiden aus dem Gesamtlipidextrakt nach Dünnschichtchromatographie. Hoppe-Seyler’s Z. Physiol. Chem. 349, 283–287 [PubMed] [Google Scholar]
- 222).Harzer K., Sandhoff K., Jatzkewitz H. (1967) Säulenchromatographische Darstellung von Phosphatiden aus Gehirn-Gesamtlipoidextrakt. Hoppe-Seyler’s Z. Physiol. Chem. 348, 119–120 [PubMed] [Google Scholar]
- 223).Wässle W., Sandhoff K. (1968) Appratus for the loading of samples on to thin layer chromatography plates. J. Chromatogr. 34, 357–363 [DOI] [PubMed] [Google Scholar]
- 224).Sarmientos F., Schwarzmann G., Sandhoff K. (1985) Direct evidence by carbon-13 NMR spectroscopy for the erythro configuration of the sphingoid moiety in Gaucher cerebroside and other natural sphingolipids. Eur. J. Biochem. 146, 59–64 [DOI] [PubMed] [Google Scholar]
- 225).Farwanah H., Pierstorff B., Schmelzer C.E., Raith K., Neubert R.H., Kolter T., Sandhoff K. (2007) Separation and mass spectrometric characterization of covalently bound skin ceramides using LC/APCI-MS and Nano-ESI-MS/MS. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 852, 562–570 [DOI] [PubMed] [Google Scholar]
- 226).Farwanah H., Wirtz J., Kolter T., Raith K., Neubert R.H., Sandhoff K. (2009) Normal phase liquid chromatography coupled to quadrupole time of flight atmospheric pressure chemical ionization mass spectrometry for separation, detection and mass spectrometric profiling of neutral sphingolipids and cholesterol. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 877, 2976–2982 [DOI] [PubMed] [Google Scholar]
- 227).Giannis A., Sandhoff K. (1989) LiBH4(NaBH4)/Me3SiCl: an unusually strong and versatile reducing agent. Angew. Chem. Int. Ed. 28, 218–220 [Google Scholar]
- 228).Liessem B., Giannis A., Sandhoff K., Nieger M. (1993) Synthese von 2-Acetamido-1,4-imino-1,2,4-tridesoxy-D-galaktitol und kompetitive Inhibition der humanen lysosomalen β-Hexosaminidase. Carbohydr. Res. 250, 19–30 [DOI] [PubMed] [Google Scholar]
- 229).Sarmientos F., Schwarzmann G., Sandhoff K. (1986) Specificity of human glucosylceramide β-glucosidase towards synthetic glucosylsphingolipids inserted into liposomes. Kinetic studies in a detergent-free assay system. Eur. J. Biochem. 160, 527–535 [DOI] [PubMed] [Google Scholar]
- 230).Sawatzki P., Damm I., Pierstorff B., Hupfer H., Sandhoff K., Kolter T. (2005) Site-specific cleavage —a model system for the identification of lipid-modified glutamate residues in proteins. ChemBioChem 6, 178–185 [DOI] [PubMed] [Google Scholar]
- 231).Schick A., Kolter T., Giannis A., Sandhoff K. (1996) Synthesis of phosphoramide analogues of sphinganine-1-phosphate. Tetrahedron 52, 2945–2956 [Google Scholar]
- 232).Schick A., Schwarzmann G., Kolter T., Sandhoff K. (1997) Synthesis of tritium labelled phosphate analogues of sphinganine-1-phosphate. J. Labelled Comp. Radiopharm. 39, 441–451 [Google Scholar]
- 233).Zacharias C., van Echten-Deckert G., Plewe M., Schmidt R.R., Sandhoff K. (1994) A truncated epoxy-glucosylceramide uncouples glycosphingolipid biosynthesis by decreasing lactosylceramide synthase activity. J. Biol. Chem. 269, 13313–13317 [PubMed] [Google Scholar]
- 234).Möbius W., Herzog V., Sandhoff K., Schwarzmann G. (1999) Gangliosides are transported from the plasma membrane to intralysosomal membranes as revealed by immuno-electron microscopy. Biosci. Rep. 19, 307–316 [DOI] [PubMed] [Google Scholar]
- 235).Neuenhofer S., Schwarzmann G., Egge H., Sandhoff K. (1985) Synthesis of lysogangliosides. Biochemistry 24, 525–532 [DOI] [PubMed] [Google Scholar]
- 236).Esmann M., Marsh D., Schwarzmann G., Sandhoff K. (1988) Ganglioside-protein interactions: spin-label electron spin resonance studies with (Na+,K+)-ATPase membranes. Biochemistry 27, 2398–2403 [DOI] [PubMed] [Google Scholar]
- 237).Marsh D., Pellkofer R., Hoffmann-Bleihauer P., Sandhoff K. (1982) Incorporation of lipids into cellular membranes —a spin-label assay. Anal. Biochem. 122, 206–212 [DOI] [PubMed] [Google Scholar]
- 238).Schwarzmann G., Hoffmann-Bleihauer P., Schubert J., Sandhoff K., Marsh D. (1983) Incorporation of ganglioside analogues into fibroblast cell membranes. A spin-label study. Biochemistry 22, 5041–5048 [DOI] [PubMed] [Google Scholar]
- 239).Giannis A., Münster P., Sandhoff K., Steglich W. (1988) Fragmentation and Wittig olefination of glucosamine derivatives—A simple route to open chain amino sugars and chiral glycerols. Tetrahedron 44, 7177–7180 [Google Scholar]
- 240).Giannis A., Sandhoff K. (1985) Stereoselective synthesis of α- and β-C-allyl-glycopyranosides. Tetrahedron Lett. 26, 1479–1482 [Google Scholar]
- 241).Knoll F., Kolter T., Sandhoff K. (2000) Sphingolipid photoaffinity labels. Methods Enzymol. 311, 568–600 [DOI] [PubMed] [Google Scholar]
- 242).Liessem B., Glombitza G.J., Knoll F., Lehmann J., Kellermann J., Lottspeich F., Sandhoff K. (1995) Photoaffinity labeling of human lysosomal β-hexosaminidase B. Identification of Glu-355 at the substrate binding site. J. Biol. Chem. 270, 23693–23699 [DOI] [PubMed] [Google Scholar]
- 243).Neuenhofer S., Sandhoff K. (1985) Affinity labelling of the GM2 activator protein. FEBS Lett. 185, 112–114 [Google Scholar]
- 244).Ollmann M., Schwarzmann G., Sandhoff K., Galla H.J. (1987) Pyrene-labeled gangliosides: micelle formation in aqueous solution, lateral diffusion, and thermotropic behavior in phosphatidylcholine bilayers. Biochemistry 26, 5943–5952 [DOI] [PubMed] [Google Scholar]
- 245).Schwarzmann G., Wendeler M., Sandhoff K. (2005) Synthesis of novel NBD-GM1 and NBD-GM2 for the transfer activity of GM2-activator protein by a FRET-based assay system. Glycobiology 15, 1302–1311 [DOI] [PubMed] [Google Scholar]
- 246).Schwarzmann G., Breiden B., Sandhoff K. (2012) Novel membrane-spanning lipids for an uncompromised monitoring of membrane fusion and intermembrane lipid transfer (In preparation). [DOI] [PMC free article] [PubMed]
- 247).Sandhoff K., Pallmann B. (1978) Membrane-bound neuraminidase from calf brain: regulation of oligosialoganglioside degradation by membrane fluidity and membrane components. Proc. Natl. Acad. Sci. U.S.A. 75, 122–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248).Pellkofer R., Sandhoff K. (1980) Halothane increases membrane fluidity and stimulates sphingomyelin degradation by membrane-bound neutral sphingomyelinase of synaptosomal plasma membranes from calf brain already at clinical concentrations. J. Neurochem. 34, 988–992 [DOI] [PubMed] [Google Scholar]
- 249).Sandhoff K., Harzer K., Wässle W., Jatzkewitz H. (1971) Enzyme alterations and lipid storage in three variants of Tay-Sachs disease. J. Neurochem. 18, 2469–2489 [DOI] [PubMed] [Google Scholar]
- 250).Sandhoff K. (1969) Variation of β-N-acetylhexosaminidase-pattern in Tay-Sachs disease. FEBS Lett. 4, 351–354 [DOI] [PubMed] [Google Scholar]
- 251).Okada S., O’Brien J.S. (1969) Tay-Sachs disease: generalized absence of a β-D-N-acetylhexosaminidase component. Science 165, 698–700 [DOI] [PubMed] [Google Scholar]
- 252).Sandhoff K., Andreae U., Jatzkewitz H. (1968) Deficient hexosaminidase activity in an exceptional case of Tay-Sachs disease with additional storage of kidney globoside in visceral organs. Pathol. Eur. 3, 278–285 [PubMed] [Google Scholar]
- 253).Pilz H., Müller D., Sandhoff K., ter Meulen V. (1968) Tay-Sachssche Krankheit mit Hexosaminidase-Defekt (Klinische, morphologische und biochemische Befunde bei einem Fall mit viszeraler Speicherung von Nierenglobosid). Dtsch. Med. Wochenschr. 93, 1833–1839passim [DOI] [PubMed] [Google Scholar]
- 254).Wright C.S., Zhao Q., Rastinejad F. (2003) Structural Analysis of Lipid Complexes of GM2-Activator Protein. J. Mol. Biol. 331, 951–964 [DOI] [PubMed] [Google Scholar]
- 255).Spiegel R., Bach G., Sury V., Mengistu G., Meidan B., Shalev S., Shneor Y., Mandel H., Zeigler M. (2005) A mutation in the saposin A coding region of the prosaposin gene in an infant presenting as Krabbe disease: first report of saposin A deficiency in humans. Mol. Genet. Metab. 84, 160–166 [DOI] [PubMed] [Google Scholar]
- 256).Tamargo R.J., Velayati A., Goldin E., Sidransky E. (2012) The role of saposin C in Gaucher disease. Mol. Genet. Metab. 106, 257–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257).Kuchar L., Ledvinová J., Hrebícek M., Mysková H., Dvoráková L., Berná L., Chrastina P., Asfaw B., Elleder M., Petermöller M., Mayrhofer H., Staudt M., Krägeloh-Mann I., Paton B.C., Harzer K. (2009) Prosaposin deficiency and saposin B deficiency (activator-deficient metachromatic leukodystrophy): Report on two patients detected by analysis of urinary sphingolipids and carrying novel PSAP gene mutations. Am. J. Med. Genet. A. 149A, 613–621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258).Matsuda J., Vanier M.T., Saito Y., Tohyama J., Suzuki K. (2001) A mutation in the saposin A domain of the sphingolipid activator protein (prosaposin) gene results in a late-onset, chronic form of globoid cell leukodystrophy in the mouse. Hum. Mol. Genet. 10, 1191–1199 [DOI] [PubMed] [Google Scholar]
- 259).Sun Y., Witte D.P., Zamzow M., Ran H., Quinn B., Matsuda J., Grabowski G.A. (2007) Combined saposin C and D deficiencies in mice lead to a neuronopathic phenotype, glucosylceramide and α-hydroxy ceramide accumulation, and altered prosaposin trafficking. Hum. Mol. Genet. 16, 957–971 [DOI] [PubMed] [Google Scholar]
- 260).Schuette C.G., Doering T., Kolter T., Sandhoff K. (1999) The glycosphingolipidoses-from disease to basic principles of metabolism. Biol. Chem. 380, 759–766 [DOI] [PubMed] [Google Scholar]
- 261).Kwon H.J., Abi-Mosleh L., Wang M.L., Deisenhofer J., Goldstein J.L., Brown M.S., Infante R.E. (2009) Structure of N-terminal domain of NPC1 reveals distinct subdomains for binding and transfer of cholesterol. Cell 137, 1213–1224 [DOI] [PMC free article] [PubMed] [Google Scholar]