Abstract
Purpose
Gender disparities have long existed in medicine but they have not been well examined in urology. We analyzed a large cohort of graduating urology residents to investigate gender disparities in academic productivity, as measured by peer reviewed publications and academic career choice.
Materials and Methods
We assembled a list of urology residents who graduated from 2002 through 2008 who were affiliated with the top 50 urology hospitals, as ranked by 2009 U.S. News & World Report. PubMed® was queried to determine the publication output of each resident during the last 3 years of residency. We used an Internet search to determine the fellowship training, career choice and academic rank of each subject. Gender effects on each factor were evaluated.
Results
A total of 459 male (84.5%) and 84 female (15.5%) residents were included in analysis. During residency women produced fewer total publications (average 3.0 vs 4.8, p = 0.01) and fewer as first author (average 1.8 vs 2.5, p = 0.03) than men. A higher proportion of women than men underwent fellowship training (54.8% vs 48.5%, p =0.29) and ultimately chose an academic career (40.5% vs 33.3%, p = 0.20), although these differences were not statistically significant. Of residents who chose an academic career a higher proportion of men than women (24.7% vs 2.9%, p = 0.01) obtained associate vs assistant professor rank.
Conclusions
Women produced fewer peer reviewed publications than men during residency but they were equally likely to undergo fellowship training and choose an academic career. During the study period a higher proportion of men achieved associate professor rank.
Keywords: urology, men, women, career choice, authorship
Historically medicine has been a male dominated profession, especially in the surgical subspecialties.1 However, this gender gap has been closing in recent decades. Since 1969, women have represented an increasing proportion of matriculants in American medical schools.2 Of matriculants 31% were women in 1982 and by 2010 that number had increased to 47%.2 In urology it was not until 1962 that a woman was certified by the American Board of Urology and it was not until 1975 that a woman became a member of the American Urological Association. In 1995 women represented 4.2% of all urology residents and only 1.2% of board certified urologists.3 As of July 2011, 8% of American Urological Association members were women.4
While women represent an increasing proportion of American urologists, they remain a significant minority and are still underrepresented compared to the proportion of women in medicine overall. To our knowledge it is unknown whether gender disparities in urology, which continue to evolve, persist in academic urology and among recent residency graduates.
A method that investigators have used to assess gender differences in academic medicine is to track publication output as a surrogate for academic achievement.5–11 Investigators in psychiatry,5 neurosurgery,6 family medicine,10 physical therapy8 and nursing9 found that women are authoring more papers with time but still publish less than men. In urology the rate of the increase in female authorship has outpaced the number of women in the field overall.11 In 1997 Bradbury et al surveyed 128 female urologists and found that while 94% would encourage other women to pursue urological training, 44% were at some point discouraged from choosing urology due to gender and 63% believed that gender discrimination had some degree of effect on their training or practice.3
It is important to better understand the relationship of gender with scholarship, career choice and university rank, especially among recent residency graduates. It is important to identify such inequities in academic urology, if they exist, since women are increasingly represented among clinicians and trainees. Appreciating disparities may help identify training deficiencies and improve overall urological education and the retention of women in the field.
We analyzed a large cohort of recently graduated urology residents to investigate whether gender disparities in academic productivity exist, as measured by peer reviewed publications, fellowship training, and academic career choice and rank.
METHODS
We assembled a list of urology residency programs affiliated with the top 50 urology hospitals as ranked in 2009 by U.S. News & World Report, which included 37 residencies.12 The names of residents who graduated from these residency programs from 2002 through 2008 were obtained from program websites (54%) or by direct contact with administrators (46%). Information on each subject, including gender, completion of fellowship training, fellowship type and location, academic career choice and current academic rank, were obtained from departmental and physician websites, which were accessed in October 2011. We obtained institutional review board exemption.
The publication output of each subject during residency was determined by PubMed query using multiple search terms, including 1) full name, 2) last name plus first and middle initial, 3) last name plus first initial and 4) last name plus first initial plus urology. Unique publications that resulted from these queries were attributed to a given urologist if they met 2 criteria, that is they 1) pertained to a urological topic and 2) were affiliated with an institution at which the urologist had spent professional time. If only one of these criteria were met, the original manuscript was reviewed to ensure that the name of the author exactly matched that of the urologist in question before it was included as a publication by that urologist. If neither criterion was met, that is the publication was neither urology related nor affiliated with an institution where the urologist had spent time, the publication was discarded.
For each study subject the compiled list of publications was reviewed to determine the type of each publication (original research, review article, case report or editorial) and the order of resident authorship (first, second, middle or last). To estimate publication output during residency all qualifying PubMed entries published during the calendar year of residency graduation and the 2 previous years were totaled. For example, if a urologist completed residency in 2004, all entries in 2002 through 2004 were included.
We used descriptive statistics to characterize the study population. Outcomes were stratified by gender. We used the t test to compare continuous outcomes and the Pearson chi-square test to compare categorical outcomes. Statistical significance was considered at p <0.05 and all tests were 2 sided. STATA® 11 was used for analysis.
RESULTS
A total of 459 male (84.5%) and 84 female (15.5%) residents from 34 of the 37 eligible urology residency programs were included in the cohort. The remaining 3 programs refused to provide the names of graduates. The 543 residents in the cohort represented 33% of all urology residents in the United States who graduated from 2002 through 2008.
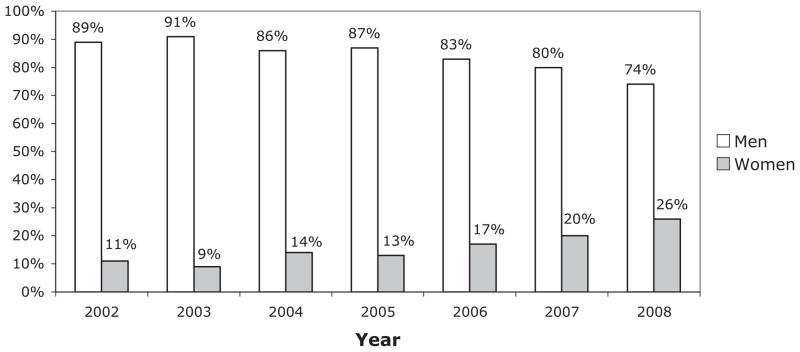
There was an increasing proportion of women during the cohort period, representing 26% in 2008 (see figure). During residency 80% of women and 84% of men were an author on at least 1 publication (p = 0.21), and 65% and 70%, respectively, produced at least 1 publication as first author (p = 0.22). Women produced fewer total publications (average 3.0 vs 4.8, p = 0.01) and fewer as first author (average 1.8 vs 2.5, p = 0.03) than men (table 1). Women also produced fewer original research papers than men (average 2.1 vs 3.3, p = 0.02). However, a higher proportion of women than men underwent fellowship training (54.8% vs 48.5%, p = 0.29) and ultimately chose an academic career (40.5% vs 33.3%, p = 0.20), although these differences were not statistically significant (table 1).
Table 1.
Gender differences in publication output, fellowship training and academic career choice among urology residents who graduated from 2002 to 2008
| Men | Women | p Value | |
|---|---|---|---|
| Mean No. publications during residency (median): | 4.8 (3) | 3.0 (2) | 0.01 |
| 1st Author | 2.5 (1) | 1.8 (1) | 0.03 |
| Original research | 3.3 (2) | 2.1 (1) | 0.02 |
| No. completed fellowship (%) | 221 (48.5) | 46 (54.8) | 0.29 |
| No. fellowship type (%): | |||
| Oncology | 69 (31) | 4 (9) | 0.002 |
| Laparoscopy or robotics | 51 (23) | 1 (2) | 0.001 |
| Infertility | 20 (9) | 2 (4) | 0.296 |
| Female urology or neurourology | 15 (7) | 16 (35) | <0.001 |
| Pediatrics | 22 (10) | 15 (33) | <0.001 |
| Reconstruction | 9 (4) | 3 (7) | 0.463 |
| Endourology | 29 (13) | 5 (11) | 0.685 |
| Other | 7 (3) | 0 | 0.429 |
| No. academic career (%) | 152 (33.3) | 34 (40.5) | 0.20 |
The type of fellowship pursued differed greatly by gender. Of those who completed a fellowship women were significantly more likely to train in pediatric and female urology, while men were more likely to train in oncology and laparoscopy (table 1).
We evaluated the effect of gender on academic promotion. In the overall cohort a significantly greater proportion of men than women achieved associate (vs assistant) professor academic rank (table 2). After stratifying the cohort by graduation year men were still more likely than women to have achieved associate professor rank among urologists who graduated in 2002. However, for more recent years no statistically significant difference was seen (table 2).
Table 2.
Gender differences in academic urologists who achieved associate professor rank
| Graduation Yr | No. Men/Total No. (%) | No. Women/Total No. (%) | p Value |
|---|---|---|---|
| 2002 | 7/13 (54) | 0/5 | 0.04 |
| 2003 | 14/25 (56) | 1/2 (50) | 0.87 |
| 2004 | 7/22 (32) | 0/1 | 0.50 |
| 2005 | 3/18 (17) | 0/4 | 0.38 |
| 2006 | 5/26 (19) | 0/6 | 0.24 |
| 2007 | 1/23 (4) | 0/8 | 0.55 |
| 2008 | 0/23
|
0/8
|
— |
| Totals | 37/150 (25) | 1/34 (3) | 0.01 |
DISCUSSION
Understanding gender disparities in academic medicine is important, especially in a subspecialty in which men currently comprise more than 90% of all physicians. Such an understanding can have implications for resident education, the recruitment and retention of diverse practitioners, and academic promotion. With the proportion of women in urology rapidly evolving, it is likely particularly relevant to evaluate gender effects on scholarship, career choice and academic promotion in a contemporary cohort of residency graduates. Our results suggest that during training women produced fewer peer reviewed publications but were just as likely to undergo fellowship training and choose an academic career. Men were more likely to choose fellowships in oncology and laparoscopy, while women were more likely to choose those in female urology and pediatrics. Proportionately fewer women than men had been promoted from assistant to associate professor.
Before this study little was known about the role of gender in academic urology. In 1997 Bradbury et al polled 128 female urologists to begin establishing demographic practice patterns.3 They concluded that women tended to be younger and maintained a high level of job satisfaction. In 2005 Lightner et al reported the results of another random survey of 121 female urologists, who reported gender based role limitations and a lack of adequate mentoring.13 However, these studies may have been limited by the recall and response biases characteristic of surveys. Moreover, the lack of a male control group precluded comparative assessment of gender inequity. Recently Weiss et al performed a bibliometric analysis of urological journals from 1974 through 2009 and found that the increase in female authorship exceeded the growth of women in urology overall.11 Our study, which analyzed multiple objective outcomes in academic urology using a large contemporary cohort, may provide the best assessment of gender disparity to date.
The effect of gender on publication output was explored by investigators in other specialties using various techniques. Some groups used citation analysis in select journals.5,7,10 Jagsi et al analyzed publications in 6 prominent multispecialty journals spanning 1970 through 2004 and found that the proportion of female first authors increased from 5.9% to 29.3%.7 Similar citation analyses of specialty specific journals in psychiatry,5 family medicine10 and nursing9 also showed increasing publication by female authors but such studies could not distinguish whether women individually were more productive or whether these trends simply reflected a greater number of women in medicine. Other studies on gender relied on surveys for self-reported publication rates and also showed lower productivity by women in physical therapy8 and internal medicine.14
A better way to assess gender effects on publishing is to objectively track publication rates in a predefined cohort of men and women, as in our study. Crowley et al used this method for neurosurgeons who graduated from 1985 to 19906 and Reed et al analyzed a cohort of 75 physicians at a single institution.15 Each group reported that female gender negatively correlated with the publication rate.
Thus, our finding that women in urology have fewer publications than men is consistent with the available literature but the reasons for this difference are unclear. Other studies of gender in surgery suggest a role for differential treatment, discrimination and societal lifestyle pressures, such as child rearing or marital responsibilities, in decreased publishing by women but a causal relationship could not be confirmed.3,13,16 Moreover, it is unclear whether a difference in the publication rate has actual significance since women in the current cohort were equally likely to undergo fellowship training and obtain an academic position despite differences in publication output.
While some studies show a correlation between in training publication and academic success,6,12 the relationship is far from definite. Cavalcanti and Detsky examined a cohort of internal medicine trainees and found no correlation between preresidency publication output and clinical performance during residency.17 Furthermore, publication output is only one of many measures of achievement for the academic physician, in addition to excellence in teaching, mentorship and clinical patient care.
The complexity of assessing achievement in academic medicine makes it difficult to interpret our finding that proportionately fewer women were promoted to associate professor rank. At the time of data collection only 1 woman (3%) in the cohort had been promoted compared to 25% of men. The difference was still significant for the 2002 cohort after stratifying by graduation year. Subsequent years did not attain statistical significance. More followup is needed to determine whether differences in promotion between men and women would become significant with time. These data suggest that men are promoted through academic ranks more quickly than their female counterparts who graduate at the same time.
Little is known about gender effects on academic promotion, likely because it is difficult to account for the myriad factors contributing to faculty achievement. In a retrospective cohort study of 75 academic physicians at Mayo Clinic who had practiced longer than 20 years men published more articles throughout their career, were more likely to achieve full professor rank and held more leadership positions.15 In a large cohort of academic neurosurgeons Crowley et al found that women published less than men and the publication rate was independently associated with academic promotion, although no gender difference was observed in current academic positions.6 To our knowledge this has not previously been investigated in urology.
In our cohort the gender differences in promotion are striking but longer followup is necessary to confirm these findings. The fact that only the 2002 cohort year showed significant gender differences after controlling for time of graduation may reflect a lag in the time needed for differences in promotion to accrue. A potential reason for the difference in promotion may be that men publish more articles than women and another may be that those in certain subspecialties favored by men, ie oncology and laparoscopy, are promoted more quickly. The explanation is more likely multifactorial. Regardless of the underlying reason for this difference in promotion, the specialty of urology and especially the mentors of young trainees must remain responsive to factors that may cause academic disengagement in each gender.
There are limitations to our analysis. The cohort included only subjects from highly ranked residency programs who graduated from 2002 through 2008. Tracking residents affiliated with the top national urology hospitals was thought to be most likely to capture those who chose an academic career. However, they may not reflect all urology graduates as a whole.
Recent years of graduation were purposely chosen so that the analysis would more accurately reflect the current state of academic urology, which is especially important given the rapidly changing demographics of the specialty. The primary drawback of selecting this cohort is that the more recent graduating classes were not optimal to assess academic promotion, which is an outcome dependent on time.
Another limitation is that data on career choice and academic rank were obtained on the Internet, which may not be up to date. However, the inaccuracy of institutional websites should be gender neutral and not affect detected gender discrepancies.
Information on the relationship, marital and child rearing responsibilities of each trainee was not available, which prevented evaluation of these factors as confounders of gender differences. Such factors may be particularly relevant during the final years of residency.
Finally and perhaps most importantly, while this analysis represents an important objective assessment of gender discrepancies in academic urology, the evaluated outcomes of publication output, career choice and early academic promotion represent only a subset of important measures for achievement and success. Other aspects, such as teaching, mentoring and patient care, were not captured in this study and deserve careful analysis.
CONCLUSIONS
Women produce fewer peer reviewed publications than men during residency but they are equally likely to undergo fellowship training and choose an academic career. During fellowship women were more likely to train in pediatric and female urology, while men were more likely to train in oncology and laparoscopy. During the study period a higher proportion of graduating male residents achieved associate professor rank.
Figure 1.
Gender distribution among urology residency programs affiliated with top 50 urology hospitals from 2002 through 2008
References
- 1.Blanchet KD. A gender transformation in urology: women find the specialty family-friendly and full of opportunities. BJU Int. 2010;105:ii. doi: 10.1111/j.1464-410X.2010.09426.x. [DOI] [PubMed] [Google Scholar]
- 2.U.S. medical school applicants and students 1982–1983 to 2010 –2011. Association of American Medical Colleges. [Accessed November 8, 2011]; Available at https://www.aamc.org/download/153708/data/charts1982to2012.pdf.
- 3.Bradbury CL, King DK, Middleton RG. Female urologists: a growing population. J Urol. 1997;157:1854. doi: 10.1016/s0022-5347(01)64884-5. [DOI] [PubMed] [Google Scholar]
- 4.May 2011 Member Profile. American Urological Association. [Accessed November 30, 2011]; Available at http://www.auanet.org/content/about-us/members/2011MemberProfile.pdf.
- 5.Amering M, Schrank B, Sibitz I. The gender gap in high-impact psychiatry journals. Acad Med. 2011;86:946. doi: 10.1097/ACM.0b013e3182222887. [DOI] [PubMed] [Google Scholar]
- 6.Crowley RW, Asthagiri AR, Starke RM, et al. Intraining factors predictive of choosing and sustaining a productive academic career path in neurological surgery. Neurosurgery. 2012;70:1024. doi: 10.1227/NEU.0b013e3182367143. [DOI] [PubMed] [Google Scholar]
- 7.Jagsi R, Guancial EA, Worobey CC, et al. The “gender gap” in authorship of academic medical literature—a 35-year perspective. N Engl J Med. 2006;355:281. doi: 10.1056/NEJMsa053910. [DOI] [PubMed] [Google Scholar]
- 8.Kaufman RR, Chevan J. The gender gap in peer-reviewed publications by physical therapy faculty members: a productivity puzzle. Phys Ther. 2011;91:122. doi: 10.2522/ptj.20100106. [DOI] [PubMed] [Google Scholar]
- 9.Shields L, Hall J, Mamun AA. The ‘gender gap’ in authorship in nursing literature. J R Soc Med. 2011;104:457. doi: 10.1258/jrsm.2011.110015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schrager S, Bouwkamp C, Mundt M. Gender and first authorship of papers in family medicine journals 2006 –2008. Fam Med. 2011;43:155. [PubMed] [Google Scholar]
- 11.Weiss DA, Kovshilovskaya B, Breyer BN. Gender trends of urology manuscript authors in the United States: a 35-year progression. J Urol. 2012;187:253. doi: 10.1016/j.juro.2011.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang G, Zaid UB, Erickson BA, et al. Urology resident publication output and its relationship to future academic achievement. J Urol. 2011;185:642. doi: 10.1016/j.juro.2010.09.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lightner DJ, Terris MK, Tsao AK, et al. Status of women in urology: based on a report to the Society of University Urologists. J Urol. 2005;173:560. doi: 10.1097/01.ju.0000149739.51103.d3. [DOI] [PubMed] [Google Scholar]
- 14.Reid MB, Misky GJ, Harrison RA, et al. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2011;27:23. doi: 10.1007/s11606-011-1892-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reed DA, Enders F, Lindor R, et al. Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43. doi: 10.1097/ACM.0b013e3181ff9ff2. [DOI] [PubMed] [Google Scholar]
- 16.McCord JH, McDonald R, Leverson G, et al. Motivation to pursue surgical subspecialty training: is there a gender difference? J Am Coll Surg. 2007;205:698. doi: 10.1016/j.jamcollsurg.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Cavalcanti RB, Detsky AS. Publishing history does not correlate with clinical performance among internal medicine residents. Med Educ. 2010;44:468. doi: 10.1111/j.1365-2923.2009.03605.x. [DOI] [PubMed] [Google Scholar]