The isolated hepatitis B core antibody (anti-HBc) pattern was generally stable, associated with human immunodeficiency virus and hepatitis C virus infection, and most commonly transitioned to or from a pattern of past infection. The isolated anti-HBc pattern likely represents resolved hepatitis B virus infection with low or undetected anti-HBs.
Keywords: hepatitis B core antibody, human immunodeficiency virus, hepatitis C, highly active antiretroviral therapy
Abstract
Background. The significance of hepatitis B core antibody (anti-HBc) without hepatitis B surface antigen (HBsAg) or hepatitis B surface antibody (anti-HBs) is unclear.
Methods. This cohort study included men enrolled in the Multicenter AIDS Cohort to determine clinical and laboratory predictors of isolated anti-HBc.
Results. A total of 2286 subjects (51% human immunodeficiency virus [HIV]–infected) were followed over 3.9 years. Overall, 16.9% (387) had at least 1 visit with isolated anti-HBc. The isolated anti-HBc pattern was stable 84% of the time, and transitioned to or from a pattern of past infection (anti-HBc and anti-HBs). Isolated anti-HBc was associated with HIV infection (odds ratio [OR], 2.19; 95% confidence interval [CI], 1.73–2.79) and hepatitis C virus (HCV; OR, 4.21; 95% CI; 2.99–5.91). The HCV association was stronger for chronic HCV infection (OR, 6.76; 95% CI, 5.08–8.99) than for cleared HCV (OR, 3.03; 95% CI, 1.83–5.03). HIV infection, chronic HCV, and cleared HCV infection all remained associated with isolated anti-HBc in multivariable models (OR, 1.74; 95% CI, 1.33–2.29; OR, 6.24; 95% CI, 4.62–8.42; and OR, 2.77; 95% CI, 1.65–4.66, respectively). Among HIV-infected subjects, highly active antiretroviral therapy was negatively associated (OR, 0.79; 95% CI, .66–.95) with isolated anti-HBc.
Conclusions. Isolated anti-HBc is associated with HIV and HCV coinfection, especially active HCV replication, and most commonly occurs as a transition to or from the pattern of natural immunity (anti-HBc and anti-HBs). The isolated anti-HBc pattern likely represents resolved HBV infection with low or undetected anti-HBs.
Hepatitis B core antibody (anti-HBc) develops after an infection with hepatitis B virus (HBV) and is usually found in conjunction with either hepatitis B surface antibody (anti-HBs) or hepatitis B surface antigen (HBsAg). The combination of anti-HBc and anti-HBs represents natural immunity, whereas anti-HBc and HBsAg are seen with chronic hepatitis B or transiently in acute infection. In some instances, anti-HBc is found without either of these markers, a pattern which is designated as isolated anti-HBc, and is especially common in the setting of coinfection with HIV or hepatitis C virus (HCV) [1–12]. Additionally, injection drug use [3, 10], extremes of age [9, 13], and lower CD4 T-cell count [13, 14] have all been reported to be associated with isolated anti-HBc.
The physiological and clinical significance of the isolated anti-HBc pattern is unclear. It may represent chronic active HBV infection with low or undetectable levels of HBsAg, resolved HBV infection with low or undetectable levels of anti-HBs, a false-positive anti-HBc result, a transition state between acute and resolved HBV infection, or chronic active HBV infection perhaps with the presence of a mutant HBsAg that prevents the detection of HBsAg or anti-HBs with current laboratory assays [15]. The hypothesis that the isolated anti-HBc serologic pattern represents resolved HBV infection is supported by the variable anamnestic response to HBV vaccination observed in subjects with isolated anti-HBc [10, 11, 16–19].
Despite the variety of proposed mechanisms for and prior studies of the isolated anti-HBc serologic pattern, our understanding of its clinical implications remains limited. Only a single cohort that included both HIV-infected and uninfected subjects has been studied [20] and only a few studies have examined HBV serologic patterns longitudinally [12, 21, 22]. The longitudinal studies that have been published to date have provided limited information due to small sample size [12], enrollment of patients in HBV hyperepidemic areas [21], or the exclusive enrollment of intravenous drug users [22]. To better characterize the clinical correlates of the isolated anti-HBc serologic pattern, we evaluated the HBV serologic patterns longitudinally among men who have sex with men (MSM) enrolled in the Multicenter AIDS Cohort Study (MACS).
METHODS
Study Design and Population
We analyzed longitudinal, prospectively collected data from the MACS, a study which enrolled MSM with and at risk for HIV infection in 4 metropolitan areas in the United States (Baltimore, MD; Chicago, IL; Pittsburgh, PA; and Los Angeles, CA) during 3 recruitment periods: 1984–1985, 1987–1991, and 2001–2003 [23]. The MACS has been described in detail elsewhere [24]. Briefly, subjects were prospectively followed at 6-month intervals, with collection of laboratory, epidemiologic, drug treatment, and behavioral data. The current study includes men who had complete serologic HBV data (HBsAg, anti-HBs, and anti-HBc) on at least 1 occasion from 2001 until 2007 and, in addition, had at least 1 positive serology. We limited this study to the period beginning in 2001 when the MACS implemented a systematic HBV serology testing protocol. Subjects were excluded if their HIV status was unknown or they acquired HIV during the course of the study period.
Laboratory Testing
HBV serologic testing was performed with enzyme immunoassays (EIAs) according to manufacturer's instructions (Abbott Laboratories, Abbott Park, IL). Isolated anti-HBc was defined at each visit as positive anti-HBc, negative anti-HBs, and negative HBsAg. All participants underwent hepatitis C virus antibody (anti-HCV) testing with a third-generation EIA in accordance with manufacturer's instructions (ADVIA Centura HCV assay); if positive, HCV RNA testing was performed using the COBAS AmpliPrep Taqman HCV assay (lower limit of detection 50 IU/mL; Roche Diagnostic Systems, Indianapolis, IN). Anti-HCV positivity at baseline was defined as a single positive anti-HCV regardless of the HCV RNA testing result, either obtained at the first visit after the 2001 study entry date or, if the anti-HCV was not obtained on the first visit, then as a positive anti-HCV on the second visit. The anti-HCV and HCV RNA results, along with other longitudinal laboratory data, were used to place subjects into 1 of 3 categories: (1) “uninfected,” defined by a consistently negative anti-HCV; (2) “cleared infection,” defined by at least 1 positive anti-HCV and at least 2 undetectable HCV RNA levels; and (3) “chronically infected,” defined by at least 1 positive anti-HCV and the presence of HCV RNA at 1 or more tests. HIV RNA levels were determined using Roche Ultrasensitive RNA PCR assay (Hoffmann-LaRoche, Nutley, NJ) with a detection limit of 50 copies/mL.
Statistical Analysis
Medians and interquartile ranges (IQRs) were used to describe numerical variables. Frequencies and percentages were used for nominal variables. To characterize patterns in transitions between isolated anti-HBc and other serologic patterns, we determined the relative frequency of the serologic patterns that were seen in either the visit just before, or in the visit just after, a visit in which the isolated anti-HBc pattern was observed.
The primary outcome was the occurrence of the isolated anti-HBc serologic pattern at each study visit. The potential explanatory variables examined included patient demographics, HIV status, CD4 T-cell count (both the absolute number and dichotomized at cut points of 50, 100, and 200), HIV RNA, HCV status (uninfected versus infected), HCV category (uninfected, cleared infection, or chronic infection), and receipt of highly active antiretroviral therapy (HAART). For the purposes of regression analysis, HIV-uninfected subjects and HIV-infected subjects with undetectable HIV RNA were assigned values of 400 copies/mL, and the HIV RNA values were log transformed. We also considered whether HAART regimens included agents with intrinsic activity against hepatitis B (ie, tenofovir, lamivudine, emtricitabine). If a subject had a positive anti-HCV during any visit, the serology was assumed to remain positive indefinitely thereafter. In contrast, no imputation of missing values was applied to hepatitis B serologies, as they exhibited substantial visit-to-visit variability.
Generalized estimating equations were used to determine both univariate and multivariate predictors of the isolated anti-HBc serologic pattern to account for the repeated measures and longitudinal structure of the data [25]. A logit link function and an autoregressive covariance structure were used. All reported odds ratios (ORs) and their associated 95% confidence intervals (95% CIs) are based on generalized estimating equation models. The selection of variables included in multivariate models was based on biological plausibility, avoidance of collinearity among predictors, and univariate association with the isolated anti-HBc pattern. All statistical analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC).
RESULTS
Study Population and Follow-Up
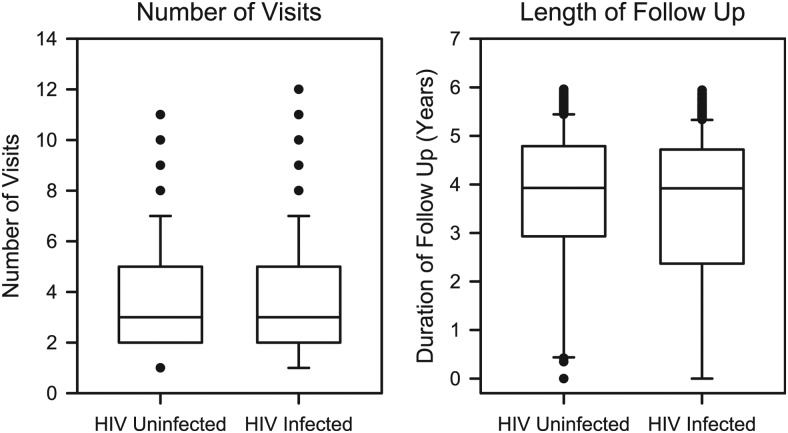
Of the 2286 men who met the inclusion requirements, 1117 (49%) were HIV uninfected and 1169 (51%) were HIV infected. Subjects made a total of 8692 study visits. The median number of visits was 3 (IQR, 2–5) with a median follow-up period of 3.9 years (IQR, 2.6–4.8 years). Follow-up for HIV-uninfected and HIV-infected subjects were qualitatively similar: 3 visits (IQR, 2–5) and 3.9 years (IQR, 2.9–4.8) for HIV-uninfected subjects, and 3 visits (IQR, 2–5) and 3.9 years (IQR, 2.4–4.7) for HIV-infected subjects (Figure 1).
Figure 1.
Distribution of the number of study visits and the duration of follow-up for study subjects by human immunodeficiency virus status. The upper and lower limits of the boxes show the interquartile limits, and the horizontal line shows the median. The error bars show the 5% and 95% limits, and outliers beyond those limits are plotted individually.
Abbreviation: HIV, human immunodeficiency virus.
At baseline, the HIV-infected men tended to be younger, more racially and ethnically diverse, and more likely to be HCV antibody–positive than the HIV-uninfected subjects (Table 1). Among 1114 HIV-uninfected subjects at their first visit, 19 (1.7%) had cleared HCV infection and 70 (6.3%) had chronic HCV infection. Among 1161 HIV-infected subjects at their first visit, 23 (2.0%) had cleared HCV infection, while 144 (12.4%) had chronic HCV infection. The prevalence of anti-HCV positive tests increased from study entry to last visit in both groups, from 7.3% (79 of 1076) to 8.1% (90 of 1117) in HIV-uninfected subjects, and from 14.0% (155 of 1110) to 15.6% (182 of 1169) in HIV-infected subjects. CD4 T-cell count and HIV RNA values from the HIV-infected subjects on study entry were consistent with effective control of their disease. The median hepatic transaminases and bilirubin values for both HIV-infected and -uninfected subjects were similar and not elevated.
Table 1.
Subject Characteristics at Study Entry
| Characteristica | HIV Uninfected (n = 1117) | HIV Infected (n = 1169) |
|---|---|---|
| Age, years | 49.1 (42.2–55.3) | 44.4 (38.9–50.1) |
| Ethnicity | ||
| White | ||
| Non-Hispanic | 818/1117 (73.2%) | 638/1169 (54.6%) |
| Hispanic | 50/1117 (4.5%) | 73/1169 (6.2%) |
| Black | ||
| Non-Hispanic | 214/1117 (19.2%) | 364/1169 (31.1%) |
| Hispanic | 2/1117 (0.2%) | 11/1169 (0.9%) |
| Asian/Pacific Islander | 7/1117 (0.6%) | 3/1169 (0.3%) |
| Other | 26/1117 (1.6%) | 80/1169 (6.8%) |
| Anti-HCV positiveb | 79/1076 (7.3%) | 155/1110 (14.0%) |
| CD4 T-cell count, cells/µL | 916 (733–1120) | 489 (319–695) |
| CD4 T-cell count <200/µL | 2/1066 (0.2%) | 133/1150 (11.6%) |
| HIV RNA, copies/mLc | … | 126 (<50–8538) |
| AST, IU/L | 23 (20–29) | 29 (22–39) |
| AST >3 × ULN | 3/1117 (0.3%) | 39/1169 (3.3%) |
| ALT, IU/L | 25 (19–33) | 30 (21–45) |
| ALT >3 × ULN | 4/1117 (0.4%) | 19/1169 (1.6%) |
| Total bilirubin, mg/dL | 0.7 (0.5–0.9) | 0.6 (0.5–0.8) |
| Receiving HAART | … | 767/1153 (66.5%) |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; HAART, highly active antiretroviral therapy; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IU/L, international units per liter; ULN, upper limit of normal.
a Numerical variables are presented as medians with interquartile ranges. Nominal variables are presented as counts and percentages (%).
b Subjects were considered HCV antibody–positive at baseline if they had a positive HCV antibody on the initial visit, or if the HCV was not measured on the initial visit, then if the HCV antibody was measured and positive on the second visit.
c These data do not reflect the replacement of all values ≤400 copies/mL with the value of 400 copies/mL, as was done prior to the regression analysis.
Relative Frequencies of HBV Serologic Patterns
Of the 8692 visits, complete HBV serologic data were available from 7856 (90.4%). The frequencies of HBV serologic patterns at study visits had notable similarities and differences between HIV-infected and -uninfected subjects (Table 2). While the pattern associated with prior infection (ie, anti-HBc and anti-HBs positive) was the most common in both groups (47.3% and 47.6%, in HIV-uninfected and -infected subjects, respectively), the pattern of prior vaccination (isolated anti-HBs) was the second most common in HIV-uninfected subjects (31.6%), and the isolated anti-HBc pattern was the second most common in HIV-infected subjects (19.2%). As expected, the pattern signifying chronic infection (ie, HBsAg and anti-HBc positive) was more common in HIV-infected (7.6% of visits) than HIV-uninfected subjects (2.1% of visits).
Table 2.
Frequencies of Visits With Each Hepatitis B Serologic Pattern
| HIV Uninfecteda | HIVI Infectedb | |
|---|---|---|
| Pattern | N (%) | N (%) |
| Past HBV infectionc | 1830 (47.3) | 1897 (47.6) |
| Prior HBV vaccinationd | 1222 (31.6) | 689 (17.3) |
| Isolated anti-HBc | 349 (9.0) | 763 (19.2) |
| Chronic HBV infectione | 82 (2.1) | 303 (7.6) |
| Negative for all HBV serologies | 370 (9.6) | 307 (7.7) |
| Other | 19 (0.5) | 25 (0.6) |
Abbreviations: anti-HBc, hepatitis B core antibody; anti-HBs, hepatitis B surface antibody, HBsAg, hepatitis B surface antigen; HBV, hepatitis B virus; HIV, human immunodeficiency virus.
a The total number of visits by HIV-uninfected subjects with known HBV serologic patterns was 3872. There were 357 visits with incomplete serology data that were excluded.
b The total number of visits by HIV-infected subjects with known HBV serologic patterns was 3984. There were 479 visits with incomplete serology data that were excluded.
c HBsAg−/anti-HBc+/anti-HBs+.
d HBsAg−/anti-HBc−/anti-HBs+.
e HBsAg+/anti-HBc+/anti-HBs−.
The isolated anti-HBc serologic pattern was observed in 1112 of 7856 (14.2%) visits overall; in 349 of 3872 (9.0%) visits by HIV-uninfected subjects and in 763 of 3984 (19.2%) of visits by HIV-infected subjects (OR, 2.19; 95% CI, 1.73–2.79; P < .0001). Twice as many HIV-infected subjects (259 of 1169, 22.2%) compared to HIV-uninfected subjects (128 of 1117, 11.5%) had at least 1 visit with the isolated anti-HBc pattern.
To determine the stability of the isolated anti-HBc pattern, the frequencies of HBV serologic patterns at visits just prior to or just after the isolated anti-HBc visit were determined (Table 3). Interestingly, this analysis revealed that the isolated anti-HBc pattern was generally stable, occurring in over 80% of the surrounding visits for both HIV-infected and -uninfected men. When a change in pattern occurred, the most common changes in both HIV-infected and HIV-uninfected subjects involved the loss or reappearance of anti-HBs with persistence of anti-HBc. Few subjects either developed or lost HBsAg, suggesting that most were not chronically infected with HBV.
Table 3.
Serologic Patterns Before and After Visits in Which Subjects had Isolated Hepatitis B Core Antibody Serologic Results
| Serologic Pattern | HIV Uninfecteda |
HIV Infecteda |
||
|---|---|---|---|---|
| Prior Visit Frequency (n = 231) | Next Visit Frequency (n = 234) | Prior Visit Frequency (n = 521) | Next Visit Frequency (n = 524) | |
| Past HBV infection | 29 (12.6) | 31 (13.2) | 60 (11.5) | 58 (11.1) |
| Prior HBV vaccination | 1 (0.4) | 2 (0.9) | 2 (0.4) | 3 (0.6) |
| Isolated anti-HBc | 192 (83.1) | 192 (82.1) | 443 (85.0) | 443 (84.5) |
| Chronic HBV infection | 1 (0.4) | 1 (0.4) | 5 (1.0) | 9 (1.7) |
| Negative for all HBV serologies | 7 (3.0) | 8 (3.4) | 11 (2.1) | 11 (2.1) |
Abbreviations: anti-HBc, hepatitis B core antibody; HBV, hepatitis B virus; HIV, human immunodeficiency virus.
a Data are reported for subjects with isolated anti-HBc status on at least 1 visit (128 HIV-uninfected subjects and 259 HIV-infected subjects). Values in table are frequencies of prior or subsequent patterns with percentages in parentheses.
Factors Associated With the Isolated Anti-HBc
Univariate analyses demonstrated that, in addition to HIV status (reported above), a positive anti-HCV was associated with isolated anti-HBc (OR, 4.21; 95% CI, 2.99–5.91; P < .0001) as was a lower CD4 T-cell count (OR, 0.96 per 100 cells/µL; 95% CI, .94–.99; P = .005) (Table 4). Among 1952 subjects with initially negative HCV serologies, 260 (13.3%) had at least 1 visit with the isolated anti-HBc pattern. In contrast, among 234 subjects with initially positive HCV serologies, 113 (48.3%) had at least 1 isolated anti-HBc visit. Interestingly, the association between isolated anti-HBc and chronic HCV infection (OR, 6.76; 95% CI, 5.08–8.99; P < .0001) was stronger than for cleared HCV infection (OR, 3.03; 95% CI, 1.83–5.03; P < .0001). In the multivariate analysis, HIV infection (OR, 1.74; 95% CI, 1.33–2.29; P < .0001), chronic HCV (OR, 6.24; 95% CI, 4.62–8.42; P < .0001), and cleared HCV infection (OR, 2.77; 95% CI, 1.65–4.66; P = .0001) all remained strongly associated with the isolated anti-HBc serologic pattern. However, CD4 T-cell count was no longer statistically associated (OR, 0.98 per 100 cells/mL; 95% CI, .95–1.01; P = .20), possibly because of its collinearity with HIV infection.
Table 4.
Univariate Associations With the Isolated Hepatitis B Core Antibody Serologic Pattern Among All Subjects
| Variable | OR | 95% CI | P Value |
|---|---|---|---|
| HIV infection | 2.19 | (1.73–2.79) | <.0001 |
| Age, per decade | 1.00 | (.91–1.10) | .96 |
| Anti-HCV positive | 4.21 | (2.99–5.91) | <.0001 |
| Chronic HCV infection | 6.76 | (5.08–8.99) | <.0001 |
| Cleared HCV infection | 3.03 | (1.83–5.03) | <.0001 |
| CD4 T-cell count, per 100 cells/µL | 0.96 | (.94–.99) | .005 |
| AST, per 10 IU/L | 1.00 | (.99–1.02) | .70 |
| AST >3 × ULN | 0.73 | (.41–1.31) | .29 |
| ALT, per 10 IU/L | 1.00 | (.98–1.01) | .70 |
| ALT >3 × ULN | 0.69 | (.40–1.20) | .19 |
| Total bilirubin, per mg/dL | 1.06 | (.97–1.16) | .18 |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CI, confidence interval; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IU/L, international units per liter; OR, odds ratio; ULN, upper limit of normal.
Among HIV-uninfected subjects alone, anti-HCV was strongly associated with the isolated anti-HBc pattern (OR, 14.1; 95% CI, 9.0–22.0; P < .0001). HIV-uninfected subjects with chronic HCV infection had a higher proportion of isolated anti-HBc visits than those who had cleared their HCV infection, and both groups were significantly different than those without evidence of HCV infection (OR, 19.2; 95% CI, 11.8–31.3; P < .0001; and OR, 7.8; 95% CI, 3.7–16.3; P < .0001, respectively). There was no statistically significant association observed in HIV-uninfected subjects between the isolated anti-HBc pattern and age, aspartate aminotransferase, alanine aminotransferase, and total bilirubin.
In the univariate analysis restricted to HIV-infected subjects, associations with isolated anti-HBc included older age (OR, 1.18 per decade; 95% CI, 1.01–1.36; P = .033), a positive anti-HCV (OR, 2.31; 95% CI, 1.51–3.52; P < .0001), and the use of HAART (OR, 0.78; 95% CI, .65–.94; P = .009), but CD4 T-cell count was not associated (Table 5). However, unlike the HIV-uninfected men, chronic HCV infection was strongly associated with the isolated anti-HBc pattern (OR, 3.66; 95% CI, 2.57–5.20; P < .0001), while cleared infection was not (OR, 1.66; 95% CI, .83–3.35; P = .15). Age, chronic HCV infection, and the use of HAART all remained statistically associated with the isolated anti-HBc pattern when included in a multivariate model (Table 6).
Table 5.
Univariate Associations With the Anti-Isolated Hepatitis B Core Serologic Pattern Among HIV-Infected Subjects
| Variable | OR | 95% CI | P Value |
|---|---|---|---|
| Age, per decade | 1.18 | (1.01–1.36) | .033 |
| Anti-HCV positive | 2.31 | (1.51–3.52) | <.0001 |
| Chronic HCV Infection | 3.66 | (2.57–5.20) | <.0001 |
| Cleared HCV Infection | 1.66 | (.83–3.35) | .15 |
| CD4 T-cell count, per 100 cells/µL | 0.97 | (.94–1.01) | .16 |
| Log HIV RNA | 1.03 | (.95–1.12) | .46 |
| Use of HAART (vs no HAART) | 0.78 | (.65–.94) | .009 |
| Use of HAART with anti-hepatitis B activity (versus HAART without anti-hepatitis B activity) | 1.49 | (1.07–2.06) | .018 |
| AST, per 10 IU/L | 1.00 | (.99–1.02) | .84 |
| AST >3 × ULN | 0.84 | (.56–1.25) | .39 |
| ALT, per 10 IU/L | 0.99 | (.98–1.01) | .50 |
| ALT >3 × ULN | 0.75 | (.49–1.14) | .17 |
| Total bilirubin, per mg/dL | 1.07 | (.98–1.16) | .15 |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CI, confidence interval; HAART, highly active antiretroviral therapy; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IU/L, international units per liter; OR, odds ratio; ULN, upper limit of normal.
Table 6.
Multivariate Model of Isolated Hepatitis B Core Antibody Serologic Pattern in HIV-Positive Subjects
| Variable | OR | 95% CI | P Value |
|---|---|---|---|
| Age (per decade of life) | 1.18 | (1.05–1.38) | .044 |
| Chronic HCV infection | 3.42 | (2.39–4.88) | <.0001 |
| Cleared HCV infection | 1.50 | (.74–3.07) | .26 |
| Use of HAART | 0.79 | (.66–.95) | .014 |
Abbreviations: CI, confidence interval; HAART, highly active antiretroviral therapy; HCV, hepatitis C virus; HIV, human immunodeficiency virus; OR, odds ratio.
In a secondary univariate analysis only including HIV-infected subjects receiving HAART, we compared those whose HAART regimen included agents with intrinsic anti-HBV activity versus those whose regimens lacked such activity. The use of HAART with intrinsic anti-HBV activity was associated with an increased frequency of the isolated anti-HBc serologic pattern (Table 5).
DISCUSSION
In this first longitudinal study of serologic patterns of HBV infection in a large cohort of both HIV-infected and -uninfected MSM followed for nearly 4 years, we found that the isolated anti-HBc pattern was a stable pattern that rarely transitioned to a chronic hepatitis B state. This is also the first study to demonstrate that, in addition to HIV infection, both chronic and cleared HCV are associated with isolated anti-HBc. In an analysis stratified by HIV status, chronic HCV was associated with isolated anti-HBc in both HIV-infected and -uninfected men, whereas cleared HCV infection was only associated in HIV-uninfected men. In the HIV-infected men, HAART use was negatively associated with isolated anti-HBc.
The most common transition in serologic pattern to or from the isolated anti-HBc pattern involved the gain or loss of anti-HBs, which suggests that isolated anti-HBc may represent resolved HBV infection with low or intermittently undetectable anti-HBs. The transition consisting of the gain or loss of HBsAg was rare, arguing against the hypothesis that isolated anti-HBc represents active HBV infection with low or undetectable levels of HBsAg. Furthermore, because the most common pattern seen before or after an isolated anti-HBc was another isolated anti-HBc, it is unlikely that this pattern is a false-positive anti-HBc or a laboratory error.
HCV seropositivity was associated with the anti-HBc pattern, particularly in those subjects with chronic infection. The reasons for this observation are not immediately apparent but it may be related to either HBV or HCV dominating when both infections are present [26]. Thus, those with chronic HCV may be more likely to lose their HBsAg because HCV dominates but the immune response is not strong enough to generate anti-HBs.
It was surprising that, in HIV-infected subjects, the CD4 T-cell count could not be shown to be associated with isolated anti-HBc. Because HIV infection can result in accelerated loss of anti-HBs [27], it was plausible that those with past HBV infection who had lower CD4 T-cell counts would be most likely to lose anti-HBs and demonstrate the isolated anti-HBc pattern. This was not supported by our multivariate analysis. However, because most of the HIV-infected men in this study were on HAART, it is possible that there was a gain of anti-HBs in those with lower initial CD4 T-cell counts early after initiation of HAART. Of note, relatively few of our HIV-infected subjects had CD4 T-cell counts less than 200/µL.
Paradoxically, we found that intrinsic anti-HBV activity in HAART regimens was associated with an increased frequency of the isolated anti-HBc serologic pattern. The interpretation of this result is complicated by the lack of control over confounding clinical characteristics that might influence the selection of HAART regimen. However, it is possible that the protective effect of HAART results from a general improvement in immune function rather than specific anti-HBV activity.
Strengths of the current analysis include direct comparison of HIV-infected and –uninfected subjects from the same cohort, longitudinal data collection, the consideration of time-varying covariates, the distinction between chronic and cleared HCV infection, and the ability to examine the relative frequencies of transitions in serologic patterns. The principal limitations of this study are missing serologic data from approximately 10% of visits and the relatively small number of subjects with cleared HCV infection, limiting our ability to precisely define the rate of isolated anti-HBc associated with cleared HCV infection. Our study population was limited to subjects with complete serologic data on at least 1 occasion and at least 1 positive serology, potentially leading to selection bias. Further, our results derive from an MSM population with high-risk exposure to HBV, and our results can only be strictly applied to similar populations.
In summary, this study supports the hypothesis that the isolated anti-HBc pattern likely represents a state of resolved HBV infection with low or undetectable anti-HBs. It is most commonly seen in patients with factors associated with impaired immune function, such as older age, HIV infection, absence of HAART, and HCV infection.
Notes
Acknowledgments. Data in this manuscript were collected by the Multicenter AIDS Cohort Study (MACS) with centers (Principal Investigators) at The Johns Hopkins Bloomberg School of Public Health (Joseph B. Margolick, Lisa P. Jacobson), Howard Brown Health Center, Feinberg School of Medicine, Northwestern University, and Cook County Bureau of Health Services (John P. Phair, Steven M. Wolinsky), University of California, Los Angeles (Roger Detels), and University of Pittsburgh (Charles R. Rinaldo).
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases for MACS, with additional supplemental funding from the National Cancer Institute (UO1-AI-35042, UL1-RR025005, UO1-AI-35043, UO1-AI-35039, UO1-AI-35040, UO1-AI-35041). Web site located at http://www.statepi.jhsph.edu/macs/macs.html.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2007;45:507–39. doi: 10.1002/hep.21513. [DOI] [PubMed] [Google Scholar]
- 2.Mofenson LM, Brady MT, Danner SP, et al. Guidelines for the prevention and treatment of opportunistic infections among HIV-exposed and HIV-infected children: recommendations from CDC, the national institutes of health, the HIV medicine association of the infectious diseases society of America, the pediatric infectious diseases society, and the American academy of pediatrics. MMWR Recomm Rep. 2009;58(RR-11):1–166. [PMC free article] [PubMed] [Google Scholar]
- 3.French AL, Operskalski E, Peters M, et al. Isolated hepatitis B core antibody is associated with HIV and ongoing but not resolved hepatitis C virus infection in a cohort of US women. J Infect Dis. 2007;195:1437–42. doi: 10.1086/515578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.French AL, Lin MY, Evans CT, et al. Long-term serologic follow-up of isolated hepatitis B core antibody in HIV-infected and HIV-uninfected women. Clin Infect Dis. 2009;49:148–54. doi: 10.1086/599610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neau D, Winnock M, Galperine T, et al. Isolated antibodies against the core antigen of hepatitis B virus in HIV-infected patients. HIV Med. 2004;5:171–3. doi: 10.1111/j.1468-1293.2004.00206.x. [DOI] [PubMed] [Google Scholar]
- 6.Wedemeyer H, Cornberg M, Tegtmeyer B, Frank H, Tillmann HL, Manns MP. Isolated anti-HBV core phenotype in anti-HCV-positive patients is associated with hepatitis C virus replication. Clin Microbiol Infect. 2004;10:70–2. doi: 10.1111/j.1469-0691.2004.00771.x. [DOI] [PubMed] [Google Scholar]
- 7.Gandhi RT, Wurcel A, Lee H, et al. Isolated antibody to hepatitis B core antigen in human immunodeficiency virus type-1-infected individuals. Clin Infect Dis. 2003;36:1602–5. doi: 10.1086/375084. [DOI] [PubMed] [Google Scholar]
- 8.Greub G, Frei PC. Isolated antibody to hepatitis B core is associated with hepatitis C virus co-infection. Clin Microbiol Infect. 2000;6:629. doi: 10.1046/j.1469-0691.2000.00160.x. [DOI] [PubMed] [Google Scholar]
- 9.Perez-Rodriguez MT, Sopena B, Crespo M, et al. Clinical significance of “anti-HBc alone” in human immunodeficiency virus-positive patients. World J Gastroentero. 2009;15:1237–41. doi: 10.3748/wjg.15.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jongjirawisan Y, Ungulkraiwit P, Sungkanuparph S. Isolated antibody to hepatitis B core antigen in HIV-1 infected patients and a pilot study of vaccination to determine the anamnestic response. J Med Assoc Thailand. 2006;89:2028–34. [PubMed] [Google Scholar]
- 11.Gandhi RT, Wurcel A, Lee H, et al. Response to hepatitis B vaccine in HIV-1-positive subjects who test positive for isolated antibody to hepatitis B core antigen: implications for hepatitis B vaccine strategies. J Infect Dis. 2005;191:1435–41. doi: 10.1086/429302. [DOI] [PubMed] [Google Scholar]
- 12.Piroth L, Binquet C, Vergne M, et al. The evolution of hepatitis B virus serological patterns and the clinical relevance of isolated antibodies to hepatitis B core antigen in HIV infected patients. J Hepatol. 2002;36:681–6. doi: 10.1016/s0168-8278(02)00019-3. [DOI] [PubMed] [Google Scholar]
- 13.Sun HY, Lee HC, Liu CE, et al. Factors associated with isolated anti-hepatitis B core antibody in HIV-positive patients: impact of compromised immunity. J Viral Hepatitis. 2010;17:578–87. doi: 10.1111/j.1365-2893.2009.01212.x. [DOI] [PubMed] [Google Scholar]
- 14.Cohen Stuart JW, Velema M, Schuurman R, Boucher CA, Hoepelman AI. Occult hepatitis B in persons infected with HIV is associated with low CD4 counts and resolves during antiretroviral therapy. J Med Virol. 2009;81:441–5. doi: 10.1002/jmv.21422. [DOI] [PubMed] [Google Scholar]
- 15.Pondé RAA, Cardoso DDP, Ferro MD. The underlying mechanisms for the ‘anti-HBc alone’ serological profile. Arch Virol. 2010;155:149–58. doi: 10.1007/s00705-009-0559-6. [DOI] [PubMed] [Google Scholar]
- 16.Chakvetadze C, Bani-Sadr F, Le Pendeven C, et al. Serologic response to hepatitis B vaccination in HIV-Infected patients with isolated positivity for antibodies to hepatitis B core antigen. Clin Infect Dis. 2010;50:1184–6. doi: 10.1086/651422. [DOI] [PubMed] [Google Scholar]
- 17.Tseng KC, Lei HY, Cheng PN, et al. Immune response to hepatitis B vaccine of subjects with isolated antibody to hepatitis B core antigen. Hepato-gastroenterol. 2003;50:1474–7. [PubMed] [Google Scholar]
- 18.Ural O, Findik D. The response of isolated anti-HBc positive subjects to recombinant hepatitis B vaccine. J Infect. 2001;43:187–90. doi: 10.1053/jinf.2001.0878. [DOI] [PubMed] [Google Scholar]
- 19.McIntyre A, Nimmo GR, Wood GM, Tinniswood RD, Kerlin P. Isolated hepatitis B core antibody—can response to hepatitis B vaccine help elucidate the cause? Aust NZ J Med. 1992;22:19–22. doi: 10.1111/j.1445-5994.1992.tb01703.x. [DOI] [PubMed] [Google Scholar]
- 20.Liang SH, Chen TJ, Lee SS, et al. Risk factors of isolated antibody against core antigen of hepatitis B virus: association with HIV infection and age but not hepatitis C virus infection. J Acq Immun Def Synd. 2010;54:122–8. doi: 10.1097/QAI.0b013e3181daafd5. [DOI] [PubMed] [Google Scholar]
- 21.Sheng WH, Kao JH, Chen PJ, et al. Evolution of hepatitis B serological markers in HIV-infected patients receiving highly active antiretroviral therapy. Clin Infect Dis. 2007;45:1221–9. doi: 10.1086/522173. [DOI] [PubMed] [Google Scholar]
- 22.Quaglio G, Lugoboni F, Vento S, et al. Isolated presence of antibody to hepatitis B core antigen in injection drug users: do they need to be vaccinated? Clin Infect Dis. 2001;32:E143–4. doi: 10.1086/320162. [DOI] [PubMed] [Google Scholar]
- 23.Kaslow RA, Ostrow DG, Detels R, Phair JP, Polk BF, Rinaldo CR., Jr The multicenter AIDS cohort study: rationale, organization, and selected characteristics of the participants. Am J Epidemiol. 1987;126:310–8. doi: 10.1093/aje/126.2.310. [DOI] [PubMed] [Google Scholar]
- 24.Dudley J, Jin S, Hoover D, Metz S, Thackeray R, Chmiel J. The multicenter AIDS cohort study: retention after 9 1/2 years. Am J Epidemiol. 1995;142:323–30. doi: 10.1093/oxfordjournals.aje.a117638. [DOI] [PubMed] [Google Scholar]
- 25.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–60. [PubMed] [Google Scholar]
- 26.Chu CJ, Lee SD. Hepatitis B virus/hepatitis C virus coinfection: epidemiology, clinical features, viral interactions and treatment. J Gastroen Hepatol. 2008;23:512–20. doi: 10.1111/j.1440-1746.2008.05384.x. [DOI] [PubMed] [Google Scholar]
- 27.Biggar RJ, Goedert JJ, Hoofnagle J. Accelerated loss of antibody to hepatitis B surface antigen among immunodeficient homosexual men infected with HIV. New Engl J Med. 1987;316:630–1. doi: 10.1056/NEJM198703053161015. [DOI] [PubMed] [Google Scholar]