SUMMARY
The safety and success of microvascular transfer have been well documented in the general population, but the good results achieved with the use of free flaps in elderly patients have received little attention. This study sought to identify differences in complications, morbidity and functional outcomes between elderly (≥ 75 years) and younger (< 75 years) patients treated surgically for advanced head and neck cancer using the Head and Neck 35 module of the European Organisation for Research and Treatment of Cancer quality of life questionnaire. Patient treatment consisted of composite resection, including excision of the primary tumour with ipsilateral or bilateral neck dissection and microvascular reconstruction. Eighty-five microvascular tissue transfers were performed to reconstruct major surgical defects. Postoperative radiation therapy was performed when indicated. Total flap loss occurred in three cases in elderly patients and two cases in younger patients. The rates of major surgical complication were 9% in young patients and 11% in elderly patients. No significant difference was observed between the two groups in the rates of major and minor flap complications, morbidity or long-term functional outcome. The results of the present analysis indicate that free-flap microvascular reconstruction can be considered a safe procedure in elderly patients with head and neck cancer.
KEY WORDS: Head and neck cancer, Elderly patient, Microvascular free flap, Complication, Functional outcome
RIASSUNTO
Sebbene la sicurezza ed il successo delle procedure ricostruttive microvascolari del distretto cervicofacciale siano state ben analizzate e documentate nella letteratura medica recente, non altrettatanto è accaduto per le procedure microchirurgiche nella popolazione anziana. Questo studio si prefigge lo scopo di valutare se esistano differenze, in termini di complicanze, morbidità e funzione, in due popolazioni di pazienti: giovani-adulti (< 75 anni) ed anziani (≥ 75 anni), sottoposti a trattamento chirurgico microvascolare per tumori avanzati del distretto testa-collo. Il trattamento è consistito nella chirurgia resettiva tumorale associata a dissezione linfonodale del collo ipsi o bilaterale e ricostruzione mediante il trasferimento microchirurgico di un lembo libero. Nella popolazione di pazienti in analisi 85 lembi liberi sono stati effettuati. La terapia radiante adiuvante è stata effettuata, quando necessaria, in funzione dello stadio di malattia. La perdita completa del lembo si è verificata in 3 casi nel gruppo di pazienti anziani ed in 2 casi nei pazienti giovani-adulti. La percentuale di complicanze maggiori è risultata essere del 9% nei pazienti giovani e del 11% nei pazienti anziani. Non sono emerse differenze statisticamente significative in termini di complicanze maggiori e minori legate al lembo, morbidità e risultati funzionali a lungo termine. In conclusione, dai nostri dati è possibile desumere che la chirurgia ricostruttiva microvascolare del distretto cervicofacciale possa essere considerata una procedura affidabile anche nel paziente anziano.
Introduction
The proportion of elderly people with head and neck cancer is rising due to an overall increase in life expectancy. The increasingly widespread application of microvascular free-flap reconstruction in the past 20 years has revolutionised the treatment of head and neck cancer. The safety and success of free-flap transfer have been well documented in the general population 1, but the good results achieved with the use of free flaps in elderly patients have received little attention.
When planning the treatment of an elderly patient with advanced head and neck cancer, the surgeon must weigh the risks and benefits of operating on the individual, who may be frail. Although head and neck surgery incurs substantially less perioperative mortality than cardiovascular or gastrointestinal tract surgery 2, other issues warrant consideration when a lengthy and complex reconstruction is planned. The surgeon must consider whether an elderly patient can tolerate the medical impact of prolonged surgery, whether the risk of surgical complication is increased and whether major surgical reconstruction should be considered for this kind of patient. These issues should be balanced against the presumed functional and aesthetic benefits achieved by the use of microvascular reconstruction.
The aim of the present study was to evaluate whether differences exist in the rates of complications, morbidity and functional outcomes between elderly and younger patients treated surgically for advanced head and neck cancer using microvascular reconstruction.
Materials and methods
Between January 2007 and December 2010, 81 patients with advanced (stage III–IV) head and neck cancer were treated at the Oral and Maxillofacial Surgical Unit in collaboration with the Plastic Surgery Unit at S. Orsola-Malpighi University Hospital, Bologna, Italy.
Patient treatment consisted of composite resection, including excision of the primary tumour with ipsilateral or bilateral neck dissection and microvascular reconstruction. Eightyfive microvascular tissue transfers were performed to reconstruct major surgical defects. Postoperative radiation therapy was performed when indicated, depending on the tumour stage and surgical margins. Indications for postoperative radiotherapy were T3–T4 tumours, positive or close surgical margins, multiple positive nodes and/or extranodal spread.
Patients were divided into two groups according to age: a younger group included patients aged < 75 years (n = 46) and an elderly group with patients aged ≥ 75 years (n = 35). Patient details are listed in Table I.
Table I.
Defect site, reconstruction type, and American Society of Anaesthesiologists (ASA) classification in the elderly and younger patient groups.
| Defect site | Elderly (n) | Younger (n) |
|---|---|---|
| Oral cavity | 18 | 24 |
| Oropharynx | 6 | 9 |
| Midface | 11 | 13 |
| Reconstruction | ||
| Fibula | 17 | 19 |
| ALT | 20 | 12 |
| Forearm | 5 | 4 |
| Rectus | 2 | 3 |
| DCIA | 1 | 0 |
| Groin | 0 | 1 |
| Latissimus | 0 | 1 |
| ASA classification | ||
| I | 3 | 16 |
| II | 6 | 8 |
| III | 9 | 13 |
| IV | 16 | 9 |
| V | 1 | 0 |
The oral cavity was the most frequent site of reconstruction in both groups. Typically, patients undergoing major head and neck surgery and free-flap reconstruction were kept sedated and mechanically ventilated in a surgical intensive care unit overnight. The flap was monitored by checking paddle skin colour or Doppler signal every 3 h for the first 2 days, and every 4 h on days 3-5.
The following demographic variables were analysed for each group: patient sex and age, underlying disease, American Society of Anesthesiologists (ASA) score, smoking history, type of flap and defect site.
Complications were divided into donor-site, flap, and systemic complications using Classen and Ward's 3 classification. Donor-site complications were classified as seroma, haematoma, infection, dehiscence, congestion and skin loss. The number of patients who developed donorsite complications were compared between groups. Flap complications were classified as major (requiring surgical re-exploration) or minor (all others), and frequencies were calculated for each group. Postoperative comorbidities, pulmonary oedema, postoperative hypertension and sepsis were classified as systemic complications.
Long-term functional outcomes were evaluated and compared between groups using the Head and Neck 35 module of the European Organisation for Research and Treatment of Cancer (EORTC H&N35) quality of life questionnaire 4. Speech, swallowing and chewing functions were assessed 12 months after surgery.
Chi-squared analysis with Fischer's exact test was performed to determine the influence of age on complication rate, morbidity and functional outcome. In each group, complications were examined according to ASA status and reconstruction type. Statistical significance was defined as p < 0.05. All statistical analyses were performed using the SPSS® Advanced StatisticalTM software package (ver. 13; SPSS Inc., Chicago, IL, USA).
Results
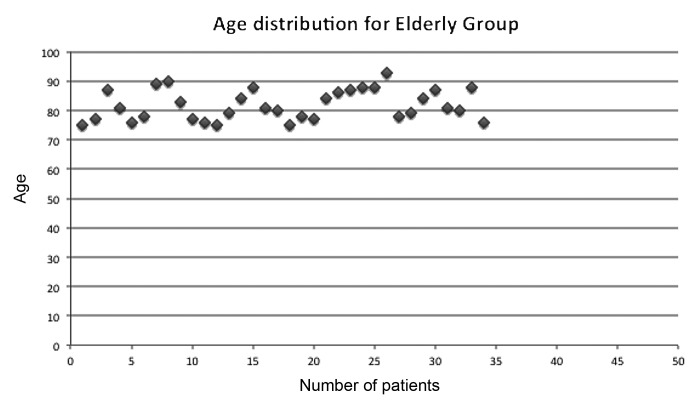
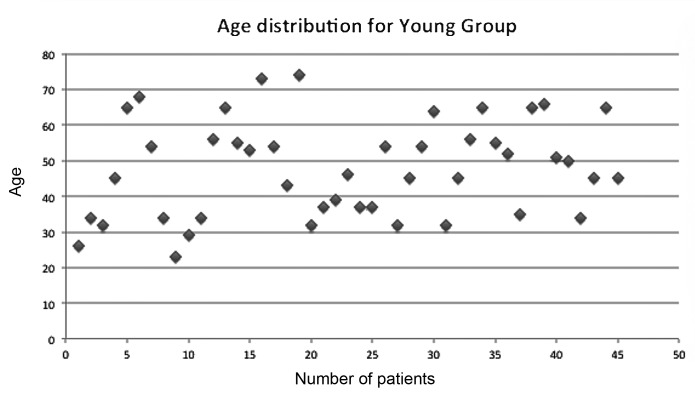
A total of 81 patients (50 men, 31 women; mean age, 59.85 years; range, 26-89 years) underwent surgery for head and neck tumours. Microvascular reconstruction was performed in all patients, with 85 free flaps used to reconstruct a variety of defects. The age distribution in both groups is shown in Figures 1 and 2. ASA status was determined as listed in Table I. Of 81 patients evaluated, 47 were ASA class III or IV . The most frequent histological diagnosis was squamous cell carcinoma (Fig. 3).
Fig. 1.
Age distribution in the elderly patient group.
Fig. 2.
Age distribution in the young patient group.
Fig. 3.
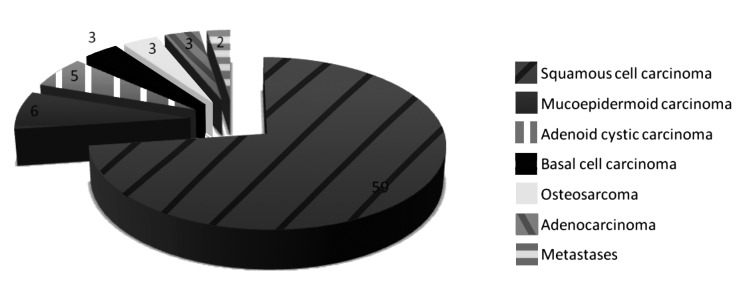
Histological tumour types.
The following microvascular free flaps were used: fibula (n = 36), anterolateral thigh (n = 32), forearm (n = 9), rectus abdominis (n = 5), deep circumflex iliac artery (n = 1), groin (n = 1) and latissimus dorsi (n = 1). The fibula free flap was used most frequently in the younger group and the anterolateral thigh free flap was used most frequently in the elderly group (Table I). One elderly patient underwent a double free-flap transfer for a complex head and neck defect. Two patients, one from the elderly group and one from the young group, received a second free-flap following flap loss. One patient underwent a second free-flap transfer for a second primary tumour.
Donor-site complications were observed in 18 cases in young patients and 20 cases in elderly patients (Table II). Seroma was the most common donor-site complication, observed in eight elderly and seven younger patients.
Table II.
Donor-site complications in the elderly and younger patient groups.
| Complication | Younger (n) | Elderly (n) |
|---|---|---|
| Seroma | 7 | 8 |
| Haematoma | 3 | 3 |
| Infection | 2 | 4 |
| Dehiscence | 4 | 3 |
| Congestion | 0 | 0 |
| Skin graft loss | 2 | 2 |
| Total | 18 | 20 |
Minor flap complications occurred in seven cases in young patients and six cases in elderly patients (Tab. III), and consisted of infection (n = 1), haematoma (n = 2), dehiscence (n = 1), congestion (n = 5) and partial flap loss (n = 4). Total flap loss occurred in three elderly patients and two younger patients. Re-exploration was required in four cases in each group (Table III). The major surgical complication rate was 9% in the younger group and 11% in the elderly group.
Table III.
Minor and major flap complications in the elderly and younger patient groups.
| Complication | Younger (n) | Elderly (n) |
|---|---|---|
| Minor flap complications | ||
| Skin graft loss | 0 | 0 |
| Infection | 1 | 0 |
| Haematoma | 1 | 1 |
| Seroma | 0 | 0 |
| Dehiscence | 1 | 0 |
| Congestion | 2 | 3 |
| Partial flap loss | 2 | 2 |
| Major flap complications | ||
| Re-exploration | 4 | 4 |
| Total flap loss | 2 | 3 |
Two younger patients and three elderly patients had systemic complications, consisting of postoperative delirium (n = 2) and pneumonia (n = 1) in the elderly group, and venous thromboembolism (n = 1) and myocardial ischaemia (n = 1) in the younger group. All but one systemic complication was resolved with medical treatment.
Perioperative mortality occurred only in one elderly patient, who suffered a heart attack during surgery for an oropharyngeal tumour. This patient had normal electrocardiogram readings before the operation and a left ventricular ejection fraction of 75%.
Swallowing, speech and chewing function domain scores at 12 months postoperatively were 64, 71 and 69 points, respectively, for younger patients and 61, 73 and 64 points, respectively, for elderly patients.
Chi-square analysis with Fisher's exact test was performed to assess the relationship between patient age and complication rates (Table IV). Age did not affect the rate of donor-site, flap, systemic complications or functional outcome (swallowing, speech or chewing). Multivariate logistic regression analysis demonstrated that age did not significantly increase the overall incidence of complications (p = 0.31). ASA score was the only variable showing an association that approached statistical significance (p = 0.04) with the development of complication (Tab. V).
Table IV.
Results of chi-square analysis with Fisher's exact test.
| Donor complications | Flap complications | Systemic complications | Swallowing function | Speech function | Chewing function |
|---|---|---|---|---|---|
| p = 0.711 | p = 0.203 | p = 0.110 | p = 0.671 | p = 0.864 | p = 0.121 |
Table V.
Results of multivariate statistical analysis, including hazard ratios and 95% confidence intervals (CIs) for the variables in each model.
| Model | Hazard ratio | 95% CI | p |
|---|---|---|---|
| Overall complications | |||
| Age (< 75 vs. ≥ 75 years) | 1.12 | 0.83-1.52 | 0.31 |
| Sex | 0.92 | 0.65-1.31 | 0.65 |
| ASA status | 0.72 | 0.53-0.97 | 0.04 |
| Tumour site | 1.10 | 0.81-1.48 | 0.54 |
Discussion
Microvascular free-tissue transfer, a reliable technique for head and neck reconstruction, was introduced in 1959 5. Consistent success rates of 90-99% have been reported 6. Complications can be divided into three main groups: general condition-related, recipient area-related and procedure- related.
Population demographics show a growing proportion of elderly people, and age has been regarded frequently as an independent risk factor for poor surgical outcome. Before the 1960s, the operative mortality rate for elderly patients undergoing elective surgery was two to six times higher than that in the general population 7. Several wellaccepted reasons explain this difference. The first factor is heart failure; an elderly patient's ageing heart has a less efficient cardiac output when placed under the stress of surgery and anaesthesia 8, and this condition is accompanied by lower renal blood flow resulting in larger water and electrolyte imbalances. The second factor is the compromise of pulmonary function with increased age due to smaller vital capacities and poorer gas exchange resulting from lung parenchyma deterioration 9. However, the mortality rate in elderly patients has declined in the past 40 years. Today, the overall surgical mortality rate is about 0.9-2.4%, even for patients with cardiac disease 10, largely as result of safer anaesthesia techniques. In addition, the average life expectancy of a 70-year-old man is 11 years and that of a 70-year-old woman is 14 years 11.
In the literature, no exact age seems to be associated with the word ''elderly''. However, this lack of precision is not entirely relevant, as surgical indications should be based not on age, but on risk assessment. The ASA score is a commonly recommended tool for risk assessment 12.
Studies of free-flap use have been conducted in elderly patients aged 50 13, 60 14, 65 3, and 70 2 years. The flap loss rate in these studies ranged from 1% in a 92-patient series 6 to 16.7% in a 47-patient series 7. This variation illustrates the difficulties of precisely defining the term ''elderly'' and of predicting morbidity rates in elderly patients. Many studies examining the relationship between age and free-flap complication have demonstrated that age is not an important factor influencing the success of microvascular free-flap transfer. However, surgery is often avoided in elderly patients because of the increased likelihood of various complications, regardless of the type of procedure chosen. In 1999, Pompei et al. 15 reported the results of 392 head and neck flap reconstructions, including those employing pedicled flaps; the authors found that complications in elderly patients were correlated with comorbidities, but not with age or operation length.
In 2000, Serletti et al. 3 analyzed 104 free-flap procedures in patients aged ≥ 65 years, and concluded that free-flap transfer in elderly patients achieved a success rate similar to that in the general population. They concluded that age alone should not be considered a contraindication or an independent risk factor when considering free-tissue transfer. The authors believed that ASA status was a reliable predictor of postoperative medical and surgical morbidity. They found that an operative time > 10 h was a significant factor in the development of postoperative surgical complications. Because elderly patients are also less capable of handling large fluid shifts and significant blood loss, proper fluid management and protein–calorie balance are important. Another significant factor in reconstruction failure seems to be the presence of peripheral vascular disease.
In 1994, Bridger et al. 16 found no significant difference in the rate of postoperative surgical complications between patients older (42%) and younger (37%) than 70 years, and concluded that age alone should not contraindicate head and neck microvascular procedures. Furthermore, in 2006, Classen and Ward 3 analyzed the complications of free-flap operations using the donor-site, flap and systemic complication categories. They found that age influenced only the systemic complication rate.
All of these studies evaluated factors that can lead to freeflap complication. However, precise analyses of how age influences free-flap complication have been infrequent. Moreover, some previous studies have included pedicled flaps in the analysis and have presented simple numerical complication rates without performing statistical analysis. Most of these studies have reported that age does not impact the free-flap complication rate, but the results have varied; a significant number of studies have reported that age may influence the rate of systemic complications.
In the present study, we assessed age as a variable affecting free-flap complication rate, morbidity and functional outcome. The proportion of elderly people with head and neck cancer is rising due to an overall increase in life expectancy. Our study used a 75-year cut-off value to define the elderly age group because no previously published paper has considered "elderly" patients of this age. Indeed, we believe it is valuable to assess similarly aged patients with head and neck cancer using a precisely defined cut-off value. The appropriate cut-off value for the definition of elderly patients has been a matter of much debate: Bonawitz et al. 12 defined elderly patients as those aged ≥ 60 years, Shestak and Jones 11 used a cut-off age of 50 years and Serletti 3 used 65 years.
In the present study, age was considered a continuous variable in the analysis of its association with donor-site, flap, systemic complications and major and minor surgical complication rates. Functional outcomes were also evaluated in both groups. No pedicled flap was included in this analysis. The major surgical complication rate was 9% in the young group and 11% in the elderly group.
Our results are similar to those of other published series. Shestak et al. 13 reviewed 19 patients who underwent microvascular head and neck reconstruction and found a 16% major surgical complication rate in patients aged ≥ 70 years, compared with 13% in patients aged < 70 years.
In the present study, multivariate analysis showed that ASA score was the only variable associated with an increased complication rate.
Similar to the findings of another recent report 16, the present study found a higher medical morbidity rate in elderly patients, with two complications (postoperative delirium) occurring. Chick et al. 17 found that medical complications occurred in 35% of elderly patients, compared with 10% of younger patients.
In the present study, one elderly patient died during surgery; no death occurred in the younger population. Morgan et al. 18 noted that perioperative mortality increased significantly with age, but most series have reported rates of 3–6% in elderly patients undergoing head and neck reconstruction 19. The present study also found no significant difference between the two groups in long-term swallowing, speech and chewing functions. Peri- and postoperative complications were correlated with ASA status.
In conclusion, the present analysis indicates that free-flap microvascular reconstruction can be considered a safe procedure in elderly patients with head and neck cancer. Surgical complication rates do not appear to increase in elderly patients compared with younger patients. Only slightly more systemic complications occurred in the elderly group than in the younger group in this study.
References
- 1.Urken ML, Weinberg H, Buchbinder D, et al. Microvascular free flaps in head and neck reconstruction: report of 200 cases and review of complications. Arch Otolaryngol Head Neck Surg. 1994;120:633–640. doi: 10.1001/archotol.1994.01880300047007. [DOI] [PubMed] [Google Scholar]
- 2.Ziffren SE, Hartford CE. Comparative mortality for various surgical operations in older versus younger age group. J Am Geriatr Soc. 1972;20:485–489. doi: 10.1111/j.1532-5415.1972.tb02145.x. [DOI] [PubMed] [Google Scholar]
- 3.Classen DA, Ward H. Complications in a consecutive series of 250 free flap operations. Ann Plast Surg. 2006;56:557–561. doi: 10.1097/01.sap.0000205830.39108.9a. [DOI] [PubMed] [Google Scholar]
- 4.Zotti P, Lugli D, Vaccher E, et al. The EORTC quality of life questionnaire-head and neck 35 in Italian laryngectomized patients. European organization for research and treatment of cancer. Qual life Res. 2000;9:1147–1153. doi: 10.1023/a:1016674507150. [DOI] [PubMed] [Google Scholar]
- 5.Seidenberg B, Rosenak SS, Hurwitt ES, et al. Immediate reconstruction of the cervical esophagus by a revascularized isolated jeju- nal segment. Ann Surg. 1959;149:162–171. doi: 10.1097/00000658-195902000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khouri RK. Free flap surgery. The second decade. Clin Plast Surg. 1992;19:757–761. [PubMed] [Google Scholar]
- 7.Cole WH. Prediction of operative reserve in the elderly patient. Ann Surg. 1968;168:310–310. doi: 10.1097/00000658-196808000-00021. Editorial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guarnieri T, Filburn CR, Zitnik G, et al. Contractile and biochemical correlates of b-adrenergic stimulation of the aged heart. Am J Physiol. 1980;239:H501–H508. doi: 10.1152/ajpheart.1980.239.4.H501. [DOI] [PubMed] [Google Scholar]
- 9.Mannino DM, Davis KJ. Lung function decline and outcomes in an elderly population. Thorax. 2006;61:472–477. doi: 10.1136/thx.2005.052449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foster ED, Davis KB, Carpenter JA, et al. Risk of noncardiac operation in patients with defined coronary disease. Ann Thorac Surg. 1986;41:42–50. doi: 10.1016/s0003-4975(10)64494-3. [DOI] [PubMed] [Google Scholar]
- 11.Thomas DR, Ritchie CS. Preoperative assessment of older adults. J Am Geriatr Soc. 1995;43:811–821. doi: 10.1111/j.1532-5415.1995.tb07058.x. [DOI] [PubMed] [Google Scholar]
- 12.Jones NF, Jarrahy R, Song JI, et al. Postoperative medical complications - not microsurgical complications–negatively influence the morbidity, mortality, and true costs after microsurgical reconstruction for head and neck cancer. Plast Reconstr Surg. 2007;119:2053–2060. doi: 10.1097/01.prs.0000260591.82762.b5. [DOI] [PubMed] [Google Scholar]
- 13.Shestak KC, Jones NF. Microsurgical free-tissue transfer in the elderly patient. Plast Reconstr Surg. 1991;88:259–263. doi: 10.1097/00006534-199108000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Bonawitz SC, Schnarrs RH, Rosenthal AI, et al. Freetissue transfer in elderly patients. Plast Reconstr Surg. 1991;87:1074–1079. doi: 10.1097/00006534-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Pompei S, Tedesco M, Pozzi M, et al. Age as a risk factor in cervicofacial reconstruction. J Exp Clin Cancer Res. 1999;18:209–212. [PubMed] [Google Scholar]
- 16.Bridger AG, O'Brien CJ, Lee K. Advanced patient age should not preclude the use of free flap reconstruction for head and neck cancer. Am J Surg. 1994;168:425–428. doi: 10.1016/s0002-9610(05)80091-1. [DOI] [PubMed] [Google Scholar]
- 17.Chick LR, Walton RL, Reus W, et al. Free flaps in the elderly. Plast Reconstr Surg. 1992;90:87–94. doi: 10.1097/00006534-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Morgan RF, Hirata RM, Jaques DA, et al. Head and neck surgery in aged. Am J Surg. 1982;144:449–451. doi: 10.1016/0002-9610(82)90420-2. [DOI] [PubMed] [Google Scholar]
- 19.McGuirt WF, Davis SP. Demographic portrayal and outcome analysis of head and neck cancer surgery in the elderly. Arch Otolaryngol Head Neck Surg. 1995;121:150–154. doi: 10.1001/archotol.1995.01890020014004. [DOI] [PubMed] [Google Scholar]