Abstract
Introduction
This paper reports data from a cognitive survey on the diffusion, practice and organization of ultrasound (US) in emergency medicine departments (EMDs) in Italy. The study was carried out by the Emergency Medicine Section of the Italian Society for Ultrasound in Medicine and Biology (SIUMB) in collaboration with the Italian Society for Emergency Medicine and Urgent Care (SIMEU).
Methods
We created a questionnaire with 10 items, relating to 4 thematic areas. The questionnaires were administered from September 2007 to February 2008, by email, telephone or regular mail. In August 2008 the data were subjected to nonparametric statistical analysis (Spearman's Rho and Pearson's chi-square – software SPSS).
Results
We analyzed 170 questionnaires from the EMDs of all Italian regions. A US scanner is present in 64.7% of the ERs, emergency US (E-US) is practiced only in 47.6% of the ERs, and only in 24% of these more than 60% of the ER team members have training in US. The diffusion of US in other operative units of the EMDs ranges from 8.2% to 26.5%.
Discussion
The presence of a US scanner in the ER is essential for the practice and training and is correlated with the level of the EMD. The use of US appears to be less common in less equipped hospitals, regardless of the size of the ER and the availability of radiological services. Wider diffusion of US and greater integration with other services for the installment of the required equipment is to be hoped for.
Keywords: Emergency Ultrasound, Emergency Medicine Department, Ultrasound
Sommario
Introduzione
Riportiamo i dati di un'indagine conoscitiva sulla diffusione, pratica e organizzazione dell'ecografia (US) nei dipartimenti di emergenza (EMDs) in Italia. Questo studio è stato condotto dalla Sezione di Ecografia di Urgenza Emergenza della Società Italiana di Ecografia in Medicina e Biologia (SIUMB) in collaborazione con la Società Italiana di Medicina di Emergenza e Urgenza (SIMEU).
Metodi
Abbiamo creato un questionario con 10 campi, relativi a 4 aree tematiche. I questionari sono stati somministrati nel periodo settembre 2007-febbraio 2008, via e-mail, telefono o posta ordinaria. I dati sono stati analizzati con metodi statistici non parametrici nell'Agosto 2008.
Risultati
Abbiamo analizzato 170 questionari provenienti dagli EMDs di tutte le regioni italiane. Un ecografo è presente nel 64,7% dei Pronto Soccorso, l'ecografia d'emergenza (E-US) è praticata solo nel 47,6% dei Pronto Soccorso, e solo nel 24% di questi più del 60% dei membri dell'èquipe è formata in ecografia. La diffusione degli US in altre Unità Operative degli EMDs va dall'8,2% al 26,5%.
Discussione
La presenza di un ecografo in Pronto Soccorso è essenziale per la pratica e la formazione e è correlata al livello del Dipartimento di Emergenza (I o II). L'uso dell'Ecografia sembra essere minore negli ospedali meno attrezzati, indipendentemente dalla grandezza del Pronto Soccorso e dalla disponibilità di Servizi di Radiologia. Si auspica una maggiore diffusione dell'ecografia e una maggiore integrazione con altri servizi quanto all'allocazione delle risorse richieste.
Introduction
Interest in ultrasound (US) is increasing among physicians and scientific societies involved in emergency medicine and urgent care. After the first reports on its efficacy for rapid diagnosis of life-threatening conditions like traumatic hemoperitoneum [1–4] or abdominal aortic aneurysm [5,6], US has been included in numerous diagnostic and therapeutic protocols [7,8] used in emergency medicine. Technological advances have revolutionized care in emergency medicine departments (EMDs) in the United States, allowing US to emerge from the outpatient clinic and arrive at the bedside of the patient and other points of care. Here, with the manageability of a stethoscope, US can be focused on individual problems (focused US) or used with other clinical tools to manage complex cases and multiorgan diseases [9–12]. In this manner, US has become an asset for physicians caring for critically ill patients. The main characteristics of this type of US, which will be referred to hereafter as “emergency US” (EUS), can be effectively summarized as follows: “ highly focused, interactive, brief, may be repeated as clinically warranted and emphasizes only one finding” [13].
The aim of this study was to evaluate the current diffusion of US in EMDs in Italy, the modalities of use, and the training level of the physicians. From September 2007 to August 2008 the Emergency Medicine Section of the Italian Society for Ultrasound in Medicine and Biology (SIUMB) in collaboration with the Italian Society for Emergency Medicine and Urgent Care (SIMEU) conducted a survey in EMDs throughout Italy. The results of this survey are reported below.
Materials and methods
The survey was conducted by means of a questionnaire with 10 items related to the 4 areas: 1) characteristics of the activity and organization of the Emergency Room (ER) (items 1, 2, 3, 4, and 9); 2) organization of US services in the ER (items 5 and 6); 3) US training level of ER physicians (items 7 and 8); 4) diffusion of US in other operative units of the EMD (item 10) (Fig. 1). The level of the EMD was defined in accordance with the guidelines issued by the Ministry of Health in 1996 [14]. The presence in the EMD of a short-term observation (STO) unit was regarded as evidence of recent structural reorganization since this type of service is a relatively recent acquisition [15]. The activity of the STO is associated with that of the ER and directed at patients who require diagnostic procedures that can be completed within a period of 24 h.
Fig. 1.

Survey questionnaire.
The questionnaires were distributed by regional representatives of the SIUMB and members of the society's Emergency Medicine Section, and members of the SIMEU. The questionnaires were delivered by e-mail, telephone, or regular mail to the heads of the ER (previously contacted by telephone) or their delegates. The completed questionnaires were then collected and evaluated by a 3-person team (FA, SS, and MS) to verify their validity and to eliminate any duplicates. The data were extracted, assembled, evaluated, and analyzed in August 2008 (SS). Items on the questionnaire with a response rate below 15% were considered insufficient.
Statistical analysis. Continuous variables (number of ER admissions, percentage of the ER physician team with training in US) were grouped according to the modal distribution. The data were subjected to nonparametric statistical analysis to find possible correlations (rank correlation index R or Spearman's rho and Pearson chi-square test – software SPSS). The rank correlation index R measures the degree of association between two variables for which the only hypothesis is ordinal measure but possibly continuous (this is significant if greater than 0.5). The Pearson chi-square test is a nonparametric statistical test used to verify whether the recorded frequencies are significantly different from those derived from a theoretical distribution. This test allows us to accept or reject a given hypothesis (significant index ≤ 0.05) [16].
Results
One hundred eighty (64.3%) of the 280 questionnaires distributed were returned by the end of August 2008. Table 1 shows the regional origins of the responses received. In Table 2 the composition of the sample surveyed is described and compared with the characteristics and the number of operative hospitals in Italy in the year 2003 [17]. Ten questionnaires from hospitals without EMDs were excluded from the analysis. Table 3 outlines the characteristics of the activities and structural organization of the ERs that took part in the survey. Table 4 shows the results of the survey, in terms of availability of US scanners in the ER, use of US among ER physicians, and modalities of use. Table 5 reports the data on US training among members of the ER team. Table 6 shows the current presence of US scanners in the other operative units of the EMD. Table 7 reports the data on the validity of the analysis based on response rates for the 10 items of the questionnaire.
Table 1.
Regional origins of responses to the questionnaires.
| Region | Participating centers | % |
|---|---|---|
| Veneto | 29 | 16.1 |
| Sicily | 24 | 13.2 |
| Emilia Romagna | 21 | 11.7 |
| Friuli-Venezia Giulia | 16 | 8.9 |
| Lombardy | 11 | 6.1 |
| Sardinia | 11 | 6.1 |
| Piedmont | 11 | 6.1 |
| Liguria | 10 | 5.6 |
| Abruzzo, Latium, The Marches, Apulia | 7 × 4 (28) | 15.6 |
| Basilicata | 6 | 3.3 |
| Campania, Tuscany, Trentino–Alto Adige | 3 × 3 (9) | 5.1 |
| Umbria | 2 | 1.1 |
| Calabria, Aosta Valley | 1 × 2 (2) | 1.1 |
| Total | 180 | 100 |
Table 2.
Composition of the study population in relation to the Hospitals in Italy.a
| SIUMB Survey |
Italian Hospitals |
% | |||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Level I EMD | 107 | 59.5 | 196 | 26.4 | 55 |
| Level II EMD | 63 | 35 | 119 | 16 | 53 |
| Hospitals without ER | 10 | 5.5 | 427 | 57. 6 | 1.3 |
| Total | 180 | 100 | 742 | 100 | 24 |
Data provided by the Ministry of Health.
Table 3.
Characteristics of the activity and organization of ERs.
| Characteristic | Research sample | ||
|---|---|---|---|
| Admissions/year | <10,000 | 5 | 3.1% |
| ≥10,000–25,000 | 41 | 25.3% | |
| ≥25,000–40,000 | 38 | 23.5% | |
| ≥40,000–65,000 | 40 | 24.7% | |
| ≥65,000–130,000 | 36 | 22.2% | |
| ≥130,000 | 2 | 1.2% | |
| Total | 162 | 100% | |
| Presence of an STO unit | Yes | 126 | 74.1% |
| No | 44 | 25.9% | |
| Total | 170 | 100% | |
| 24 h Radiological Service | Yes | 55 | 32.4% |
| No | 115 | 67.6% | |
| Total | 170 | 100% | |
| Presence of CT | Yes | 165 | 97.1% |
| No | 5 | 2.9% | |
| Total | 170 | 100% | |
Table 4.
Availability of US scanners in ER, E-US activity by ER physician teams, and organization aspects.
| YES |
NO |
Total | |||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| US scanner in ER | 110 | 64.7 | 60 | 35.3 | 170 |
| Use of E-US | 81 | 47.6 | 85 | 48.8 | 166 |
| US in ER | 104 | 61.2 | 53 | 31.2 | 157 |
| US on in-patient ward | 67 | 39.4 | 83 | 48.8 | 150 |
Table 5.
ER physicians with training in US. (% of ER team members)
| 0–29% | 30–59% | 60–100% | No data | |
|---|---|---|---|---|
| ER physicians trained in US | 38.8 | 26.5 | 24.1 | 10.6% |
| ER physicians currently in training | NS | |||
Table 6.
Presence of US scanners in other operative units of the EMDs.
| YES |
NO |
No data |
Total | ||||
|---|---|---|---|---|---|---|---|
| n. | % | n. | % | n. | % | ||
| Pre-Hospital Care | 14 | 8.2 | 148 | 87.1 | 8 | 4.7 | 170 |
| Emergency Surgery | 45 | 26.5 | 118 | 69.4 | 7 | 4.1 | 170 |
| Operating Room | 34 | 20 | 128 | 75.3 | 8 | 4.7 | 170 |
| Intensive Care | 38 | 22.4 | 123 | 72.4 | 9 | 5.3 | 170 |
Table 7.
Validity of the analysis based on the response for the 10 items of the questionnaire.
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Responses n | 170 | 162 | 170 | 170 | a) 166 | a) 157 | 152 | 140 | a) 170 | 162 |
| b) 120 | b) 150 | b) 170 | ||||||||
| c) 121 | ||||||||||
| Missing % | 0 | 4.7 | 0 | 0 | a) 2.4 | a) 7.6 | 10.6 | 17.6a | 0 | 4.7 |
| b) 29.4a | b) 11.8 | |||||||||
| c) 28.8a |
Section insufficient for analysis.
The presence of US scanners in the ER was significantly correlated with US practice in the ER (“bedside”) (Spearman's rho 0.8) and with ER physicians active in E-US (Spearman's rho 0.7). ER doctors active in E-US was also correlated with “bedside US” (Spearman's rho 0.7).
Fig. 2 shows data on the correlation (chi-square test) between the main variables hypothesized. The analysis of the hypotheses revealed that the EMD level was positively correlated with the presence of US scanners in ER (p < 0.06), “bedside US” practice (p < 0.02), and presence of US scanners in other operative units (p < 0.002); correlation was also found between presence of US scanners in ER, diffusion of E-US practice (p 0.000), “bedside US” practice (p 0.000), and presence of ER physicians with training in US (p 0.000).
Fig. 2.
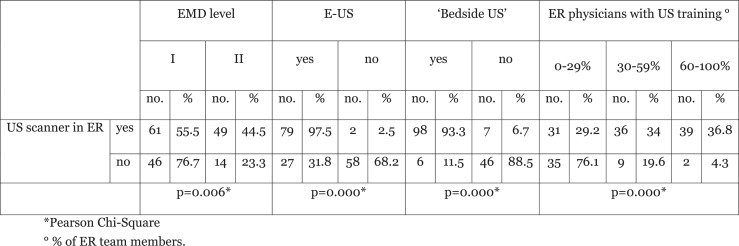
Presence and practice of US in ER.
Discussion
This study consists of a survey on the current practice of US in EMDs in Italy. Interest in this subject is currently increasing among the physicians and scientific societies involved in US and/or emergency medicine/urgent care and to a lesser extent, also among the administrators of health-care institutions themselves. The survey was made possible thanks to the commitment of the SIUMB, its network of regional representatives, and the members of its Emergency Medicine Section. To our knowledge, surveys of this type have never been carried out in Italy or in other Western countries.
Sample analysis
The geographical representation of the Italian territory is not homogeneous because over 50% of the sample is represented by five regions (Veneto, Sicily, Emilia Romagna, Friuli Venezia Giulia, and Liguria) (Table 1), where questionnaires were completed by 95–100% of the EMDs in the regions. Some of the larger regions (Lombardy, Piedmont, Latium, Campania, and Tuscany) are represented by less than 40% of the hospitals, and in others (Umbria and Calabria) representation was nonsignificant. This probably reflects more active promotion of the survey by certain regional representatives, but we cannot exclude the possibility that in the “silent” regions, there is actually low overall interest in the subject of US in the EMD.
If we consider the total number of active hospitals in Italy in the year 2003 (742 according to the data provided by the Ministry of Health) [17], our sample (which includes 170 hospitals with ERs) seems small (24%). However, about 57% of the hospitals registered with the Ministry of Health do not have an ER, and they probably represent very diverse health-care settings (small hospitals, private structures, and specialized care institutions). The 10 hospitals in our sample without ERs were excluded from our analysis. Our sample includes 54% of all EMDs in Italy (Table 2). The population studied has probably remained stable since 2003. Therefore, the sample investigated in our survey is still representative. The sample was considered numerically sufficient for the analysis of the data in this type of survey.
The sample represents, in a fairly homogeneous manner, small, medium, and large ERs, and most are in compliance with the ministerial directives, at least in terms of the presence of STO units (Table 3).
For some items of the questionnaire, the response rates were considered insufficient (<15% of the total), in particular, item 5, answer 2; item 6, answer 3; and item 8 (Table 7). It is likely that in these cases, response rates were negatively influenced by the closed nature of the first two items (it was not possible to choose between yes and no) and the ambiguous wording of the third.
Diffusion and practice of ultrasound in EMDs
On the whole sample, 64.7% of the participant EMDs reported having a US scanner in the ER. This finding indicates a moderately high availability of equipment and awareness of the fact that US services should meet the needs of the patient (and the physician caring for him/her) instead of being delivered in the traditional manner, which involves referral to an outpatient US unit detached (even a few meters) from the center where the patient is being cared for. The presence of a US scanner in the ER is essential for the practice of ER US, for the diffusion of training in US among the ER physicians, and for the practice of E-US [Fig. 2]. Although physicians' interest in US is obviously a strong incentive for installing the required equipment in the ER, the latter cannot be considered a foregone outcome in every organizational context, nor does it necessarily lead to the choice of technically adequate US scanners. The survey did not include questions regarding the quality of the equipment available in the ER.
This finding may be related to the global resources of the EMD, as suggested by the positive correlation between EMD level and the presence of a US scanner in the ER and in other operative units. Higher EMD levels are associated with wider use of bedside US, but not with the other indicators of E-US diffusion, included specific training of ER physicians. In our sample, there was no correlation between the practice of US in the ER, the volume of activity in the ER, and the availability of 24 hour-a-day in-house radiological coverage. Most (76.7%) of the participant ERs without a US scanner were level I EMDs [Fig. 2], and only 32.4% of the participating EMDs have a 24 h radiological coverage (Table 3).
Ultrasound is mainly appreciated for its versatility and availability. It is considered a valuable supplemental tool for doctors who work in highly advanced technological settings, as demonstrated by the positive relation between the EMD level and the diffusion of US in other operative units of the EMD (Pre-hospital Care, Emergency Surgery, Intensive Care Unit), although the latest data are less encouraging if compared with those of the ER. The diffusion of US is not as advanced in the EMDs that are less well equipped, where E-US could theoretically prove to be particularly useful: without attempting to replace conventional radiological services, the availability of E-US could increase the diagnostic capacity of the physicians and their autonomy in managing emergency cases as well as less critical ones. In this context, it is interesting to note that CT is available in almost all of EMDs (Table 3), despite the fact that it requires more costly equipment than US and the presence of a technician and a radiologist (at the very least), who are often available on an on-call basis.
Training
Only 24% of the ERs taking part in the survey reported that over 60% of their physicians were trained in US; in 40% of the cases, the training was described as “initial.” On the whole, however, the survey shows a high level of interest in US and an increasing tendency of ERs to provide specific training programs in this field (Table 5). Unfortunately, the response rate for the question on training requirements was unsatisfactory, probably due to the ambiguity of the question, and to the confusion often aroused by vague terms such as “basic level” and “advanced level” with reference to US training. This is probably also related to the high number of training programs currently available and the absence of uniformity in terms of their content.
Conclusions
Our work provides the scientific community with a high-quality survey on a fairly wide sample of Italian EMDs, in which interest in US appears to be increasing (although comparative data are not available). At the moment the development of US is mainly related to the availability of resources, and consequently to the size and organizational complexity of the EMD. In contrast, the potential value of US does not seem to be perceived as much in less complex settings, nor does there seem to be sufficient cooperation between departments or service units on the issue of US in ERs. There are no data supporting an overall benefit of E-US in smaller, less equipped hospitals, but this would be an interesting and useful question for future research.
Training of ER physicians in US is an important and rapidly growing phenomenon, which requires greater cooperation among scientific societies in this field regarding course syllabi. This will definitely represent an important topic for discussion in years to come.
Repetition 5 years from now of a study like the one described here (hopefully with our participation) should provide insight into the evolution of US in Italian EMDs.
Conflict of interest statement
The authors have no conflict of interest.
Acknowledgments
The authors are grateful to the regional representatives of the SIUMB, its Emergency Medicine Section, and members of the SIMEU for their help in distributing the questionnaires.
Special thanks to Dr. Loretta Muraro of the Quality Control operative unit of the Local Health-care Unit (Bologna, Italy) for her collaboration in the statistical analysis required in this work.
References
- 1.Tso P., Rodriguez A., Cooper C. Sonography in blunt abdominal trauma: a preliminary progress report. J Trauma. 1992;33(1):39–44. doi: 10.1097/00005373-199207000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Pearl W.S., Todd K.H. Ultrasound for the initial evaluation of blunt abdominal trauma: a review of prospective trials. Ann Emerg Med. 1996;27(3):353–361. doi: 10.1016/s0196-0644(96)70273-1. [DOI] [PubMed] [Google Scholar]
- 3.Brown M.A., Casola G., Sirlin C.B., Patel N.Y., Hoyt D.B. Blunt abdominal trauma: screening US in 2693 Pazients. Radiology. 2001;218:352–358. doi: 10.1148/radiology.218.2.r01fe42352. [DOI] [PubMed] [Google Scholar]
- 4.Sirlin C.B., Brown M.A., Andrade-Barreto O.A. Blunt abdominal trauma: clinical value of negative screening US scans. Radiology. 2004;230:66–68. doi: 10.1148/radiol.2303021707. [DOI] [PubMed] [Google Scholar]
- 5.Kuhn M., Bonnin R.L., Davey M.J., Rowland J.L., Langlois S.L. Emergency department ultrasound scanning for abdominal aortic aneurysm: accessibile, accurate and advantageous. Ann Emerg Med. 2000;36(3):219–223. doi: 10.1067/mem.2000.108616. [DOI] [PubMed] [Google Scholar]
- 6.Barkin A.Z., Rosen C.L. Ultrasound detection of abdominal aortic aneurysm. Emerg Med Clin North Am. 2004;22:675–682. doi: 10.1016/j.emc.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Rose J. Ultrasound in abdominal trauma. Emerg Med Clin North Am. 2004;22:581–599. doi: 10.1016/j.emc.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 8.McGahan J.P., Wang L., Richards J.R. From the RSNA refresher courses: focused abdominal US for trauma. Radiographics. 2001;21:S191–S199. doi: 10.1148/radiographics.21.suppl_1.g01oc09s191. [DOI] [PubMed] [Google Scholar]
- 9.Niendorff D.F., Rassias A.J., Palac R., Beach M.L., Costa S., Greenberg M. Rapid cardiac ultrasound of inpatients suffering PEA arrest performed by nonexpert sonographers. Resuscitation. 2005;67:81–87. doi: 10.1016/j.resuscitation.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 10.Yanagawa Y., Sakamoto T., Okada Y. Hypovolemic shock evaluated by sonographic measurement of the inferior vena cava during resuscitation in trauma patients. J Trauma. 2007;63:1245–1248. doi: 10.1097/TA.0b013e318068d72b. [DOI] [PubMed] [Google Scholar]
- 11.Lichtenstein D., Meziére G.A. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134:117–125. doi: 10.1378/chest.07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atkinson P.R., McAuley D.J., Kendall R.J. Abdominal and cardiac evaluation with sonography in shock (ACES): an approach by emergency physicians for the use of ultrasound in patients with undifferentiated hypotension. Emerg Med J. 2009;26:87–91. doi: 10.1136/emj.2007.056242. [DOI] [PubMed] [Google Scholar]
- 13.Heller M., Melanson S. Applications for ultrasound in the Emergency Department. Emerg Med Clin North Am. 1997;15(4):735–744. doi: 10.1016/s0733-8627(05)70331-x. [DOI] [PubMed] [Google Scholar]
- 14.Linee Guida n. 1/1996. Atto di indirizzo e coordinamento alle regioni per la determinazione dei livelli di emergenza sanitaria. Conferenza Stato Regioni 17/5/1996, attuativa del contenuto DPR 27/3/1992. http://www.ministerosalute.it/imgs/C_17_normativa_1746_allegato.pdf
- 15.http://www.ministerosalute.it/ProntoSoccorso118/paginaInternaProntoSoccorso118.jsp?id=1190&;lingua=italiano&menu=dea.
- 16.Matthews D.E., Farewell V. Karger; Basel; New York: 1985. Using and understanding medical statistics. p 39–53. [Google Scholar]
- 17.http://www.ministerosalute.it/resources/static/pubblicazioni/sistema_emergenza_sanitaria.pdf.


