Abstract
Overload syndromes are caused by repetitive microtrauma, and the knee joint is most frequently affected in adolescents. The reason for this is that the knee joint is engaged in almost all sports activities. Pathologies related to the anterior aspect of the knee are: femoropatellar pain, jumper's knee syndromes, Osgood–Schlatter disease, Sinding-Larsen–Johansson syndrome and patellar stress fractures; to the medial aspect: semimembranous tendon enthesopathy and pes anserinus bursitis; to the lateral aspect: iliotibial band syndrome (runner's knee), popliteus and femoral biceps tendon enthesopathy; to the posterior aspect: fabella syndrome and medial gastrocnemius muscle tendon enthesopathy. Sonography plays a central role in the diagnosis and can also evaluate the evolution of diseases. This method is well accepted by the patients and by their parents, it does not involve exposure to X-rays and it is inexpensive. US imaging should, therefore, be considered a first-line imaging diagnostic technique in functional overuse syndromes of the knee.
Keywords: Sonography, Knee, Overload syndromes
Sommario
Le sindromi da sovraccarico riconoscono come causa principale i microtraumi ripetitivi e il ginocchio è l'articolazione interessata più frequentemente negli adolescenti. La ragione è legata al fatto che il ginocchio è particolarmente sollecitato in tutte le attività fisiche, sia della vita quotidiana sia nelle attività agonistiche.
Possono essere interessate varie strutture con conseguenti e diverse patologie, in particolare nel comparto anteriore si realizzano lesioni dell'articolazione femoro-rotulea, del tendine rotuleo (jumper's knee), le sindromi di Osgood-Schlatter e di Sinding-Larsen-Johansson, fratture da stress della rotula; nel comparto mediale la sindrome della plica sinoviale, tendinopatie del tendine del semimembranoso, borsiti della borsa della zampa d'oca; nel comparto laterale la sindrome da frizione della bendelletta ileo-tibiale (runner's knee), tendinopatie del tendine popliteo e del bicipite; nel comparto posteriore patologie legate alla fabella e al tendine del gemello mediale.
L'ecografia è in grado porre diagnosi e di valutare il decorso della malattia nella grande maggioranza di queste lesioni, è ben accetta ai pazienti e ai genitori per l'assenza di controindicazioni e di radiazioni ionizzanti, ha costi contenuti ed è pertanto l'esame di scelta nelle sindromi da sovraccarico del ginocchio nell'adolescente. Richiede esperienza e l'integrazione di radiologia tradizionale, TC e RM in alcuni casi quali l'inquadramento delle malformazioni e il disallineamento degli arti inferiori.
Introduction
Overload syndromes are caused by repetitive microtrauma and they involve bone, cartilage, bursae, muscles and tendons. Extrinsic factors, such as incorrect movements during sports activities, and anatomical factors, such as malalignment of the lower limbs or flexibility deficits and ligamentous laxity are concomitant causes [1]. The knee joint is most frequently affected by functional overload syndromes in adolescents as it is engaged in almost all sports activities [2].
Many diseases are classified according to their involvement of different structures of the knee. Pathologies related to the anterior aspect of the knee are: femoropatellar pain, jumper's knee syndromes, Osgood–Schlatter disease, Sinding-Larsen–Johansson syndrome and patellar stress fractures; to the medial aspect: semimembranous tendon enthesopathy and pes anserinus bursitis; to the lateral aspect: iliotibial band syndrome (runner's knee), popliteus and femoral biceps tendon enthesopathy; to the posterior aspect: fabella syndrome and medial gastrocnemius muscle tendon enthesopathy [2].
Osgood–Schlatter disease
This disease belongs to the group of juvenile idiopathic aseptic osteonecrosis. The onset of Osgood–Schlatter disease (OSD) typically occurs in adolescents ranging from 10 to 14 years of age, affecting mainly boys involved in sports activities which require jumping (soccer, running, basketball, volleyball and gymnastics). It is now accepted that OSD is caused by repetitive traumatic traction determined by the patellar tendon on the immature tibial tubercle apophysis (still partly cartilaginous) during the femoral quadriceps muscle twitch (Fig. 1). This traumatic mechanism causes microfractures, thus inducing local inflammation which is at the basis of clinical symptoms (pain, mainly after activity) and signs (soft tissue swelling). OSD is usually self-limited as symptoms disappear with complete ossification of the tibial apophysis [3].
Fig. 1.
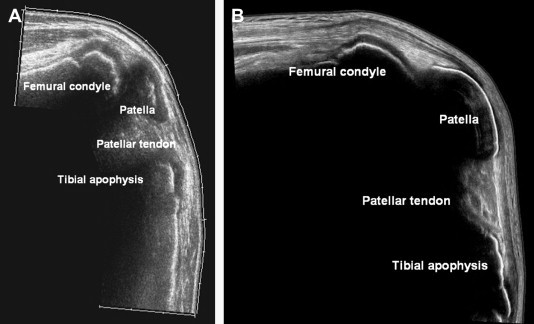
Wide sagittal US scans. (A) Normal knee of an 11-year-old boy; US allows visualization of clearly wide conjugation cartilages, hypoechoic, with femoral, tibial and patellar ossific nuclei; (B) normal knee of a 15-year-old boy; conjugation cartilages appear remarkably thinner than in the previous case and can still be seen in femoral and tibial metaphysis, while the tibial tubercle ossification center is still not fused.
Clinical diagnosis is based on the onset of low-grade pain localized at the tibial tubercle associated with deambulation, prolonged knee flexion or pressure on the tibial apophysis. Soft tissue swelling over the anterior proximal surface of the tibia is a common finding.
Although there is no universally accepted ultrasound (US) classification of OSD patterns, US is able to detect every pathologic feature and its course such as cartilage swelling, fragmentation of the tibial tubercle ossification center, patellar tendon lesions and reactive bursitis of the deep or superficial tibial patellar bursae [4–6] (Fig. 2).
Fig. 2.
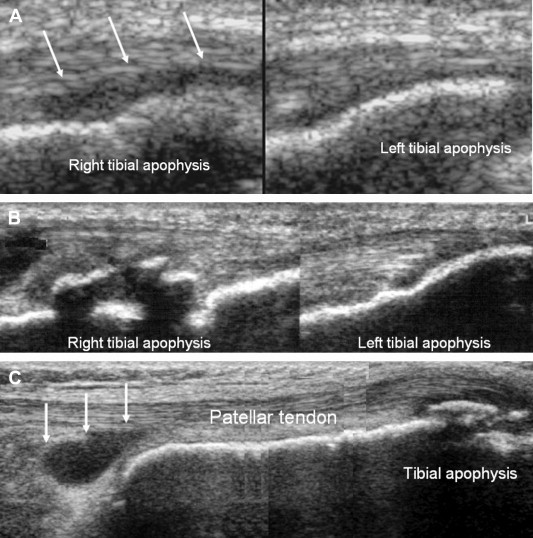
Osgood–Schlatter disease. (A) Comparative sagittal US scans: cartilage swelling can be seen in the right tibial apophysis (arrows); (B) comparative sagittal US scans: fragmentation of the right tibial tubercle ossification center; (C) the sagittal US scan shows reactive bursitis of the deep tibial patellar bursa, besides fragmentation of the tibial tubercle ossification center.
Radiographic examination of the lateral view of the knee shows fragmentation of the tibial tubercle ossification center, which has diagnostic value only when associated with soft tissue swelling, partial obliteration of the retro-tendinous fat pad and patellar tendon thickening.
OSD treatment is mainly conservative; the patient should rest for 1–2 months during the acute painful stage of the pathology, followed by a progressive restart of activity and exercises in order to restore muscle strength and flexibility of the extensor mechanism. Patients may also profit from hydrotherapy, cryotherapy and nonsteroidal anti-inflammatory drugs (NSAID). Knee orthoses may be useful.
The prognosis is excellent as OSD is usually self-limiting in 12–24 months, clearing up with complete ossification of the tibial tubercle apophysis. Surgical treatment consists of excision of the tibial tubercle and the fragmented ossification center [7,8].
Sinding-Larsen–Johansson syndrome
Sinding-Larsen–Johansson syndrome (SLJS) is a juvenile osteochondrosis, and it typically occurs in adolescent males between 10 and 14 years of age. It affects the distal pole of the patella at the proximal insertion of the patellar tendon. Pathogenesis is similar to that of OSD (which is indeed more frequent): it is caused by repetitive microtraumas and excessive prolonged stress occurring on a specific skeletal region which is weak both mechanically and biologically, when stress (applied during sports activity) exceeds intrinsic resistance. SLJS is clinically characterized by pain localized at the distal pole of the patella, increasing during flexion combined with loading of the knee joint. Other clinical features are swelling of the infrapatellar soft tissues and functional limitation.
US findings are the same as those in OSD: cartilage swelling, patellar tendon swelling at its proximal insertion and patellar fragmentation at its distal pole [6] (Fig. 3). X-ray examination may show patellar fragmentation and, in late stages of the disease, calcification of the patellar tendon.
Fig. 3.
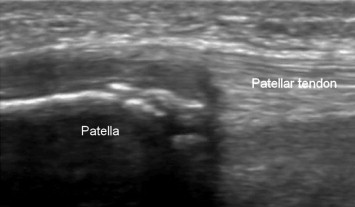
Sinding-Larsen–Johansson syndrome. Sagittal US scan: the patellar fragmentation is clearly visible at its distal pole with patellar tendon thickening at the proximal insertion and cartilage swelling.
The severity of the clinical findings determines the therapy, which ranges from rest for 4–8 weeks, to knee immobilization in extension. Prognosis is good as SLJS heals in 3–12 months.
Jumper's knee syndrome
Jumper's knee syndrome is a pathology involving the tendinous part of the extensor apparatus of the thigh affecting the patellar tendon and, much less frequently, the quadriceps tendon. This syndrome is mainly caused by repetitive microtraumas occurring during sports activities like prolonged running and jumping, and it, therefore, typically affects basketball and volleyball players, long distance runners and people doing athletics.
The most critical stage of the jumping movement is the landing. During this phase the extensor apparatus of the thigh is strongly stressed as the quadriceps muscle works in eccentric twitch, therefore, absorbing the shock determined by the impact of the ground. Jumper's knee syndrome is clinically characterized by pain, and three degrees of severity are reported in the literature: in the first stage, the athlete complains of pain only after the sports activity but there is no deficit in the quality of the sports performance; in the second phase the patient feels pain during the activity but the quality of the performance is preserved; in the most severe degree the patient complains of continuous pain and there is a fall-off in the sports performance.
US typically shows alteration in the tendon structure at its insertion on the bone, which correlates with histopathologic findings that demonstrate mucoid degeneration. Other US findings are calcifications in the tendons associated with irregularity of the bone cortex [9–12] (Figs. 4 and 5).
Fig. 4.

Jumper's knee. (A) Sagittal US scan: degenerative hypoechoic area in the patellar tendon near its proximal insertion; (B) same as A, in transverse US scan; C: Power Doppler shows vascularization inside the lesion.
Fig. 5.
Jumper's knee. Sagittal US scan: degenerative hypoechoic area in the patellar tendon near its proximal insertion containing many small calcifications.
Treatment of jumper's knee is mainly conservative in the first and second stages of severity, based on administration of NSAID for 1–2 months, dry ice compresses three times a day and bandages. This pathology heals in about 6–12 months, but if symptoms do not recede, surgical therapy might be necessary. After healing, it is very important to evaluate the movements performed during the sports activity and to correct incorrect movements in order to prevent relapse.
Bursitis
Pes anserinus bursa is located deeply to the sartorius, gracilis and semitendinosus tendons along the medial-anterior aspect of the tibia: it is the bursa most frequently involved in inflammatory processes (bursitis) due to functional overload of the knee [13–15]. Tibial exostosis is a common concomitant cause along with functional overload. Anserine bursitis is clinically characterized by mild swelling of the soft tissues on the medial aspect of the tibia as well as pain and functional limitation also after light stress.
US examination shows hyperechoic thickening of the bursa walls, while the bursa is filled with hypo-anechoic material. In normal conditions the anserine bursa is not detectable at US examination (Fig. 6). Among the syndromes caused by functional overload, femoral biceps bursitis is much less common than anserine bursitis.
Fig. 6.

Anserine bursitis. Longitudinal US scan along the pes anserinus tendons: the bursa is clearly visible filled with hypo-anechoic material; in physiological conditions, the anserine bursa is not detectable on US examination.
Iliotibial band syndrome
Iliotibial band syndrome occurs in long distance runners or in cyclists. It is caused by friction of the iliotibial band on the femoral condyle, and clinical features are lateral pain and, only rarely, swelling of the soft tissues. It is now accepted that edema, typical of this pathology, does not occur in the deep fibers of the iliotibial band but in the soft tissues between the band and the femoral condyle or in the bursa located there.
US imaging detects these alterations showing edematous swelling of the soft tissues deep to the iliotibial band and bursal effusion, while the iliotibial band fibers themselves do not show any alteration [16–18] (Fig. 7).
Fig. 7.

Iliotibial band syndrome. Wide longitudinal US scan along the iliotibial band (arrows): edematous swelling of the soft tissues deep to the iliotibial band, whose fibers do not show any alteration.
Femoropatellar pain syndrome
Femoropatellar pain syndrome occurs in connection with excessive sports activity, although incorrect alignment of the inferior limb and an excessively fast growth of the patient with mild weakness of the extensor apparatus (usually involving the quadriceps muscle) play a main role in this disease. It is clinically characterized by peripatellar pain, increased by movements like climbing up and down the stairs or walking down a slope.
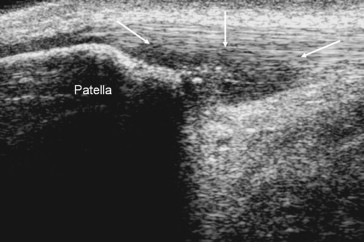
US imaging can partly evaluate the femoropatellar cartilage, its thickness and trochlear femoral and patellar angle [19,20] (Fig. 8).
Fig. 8.
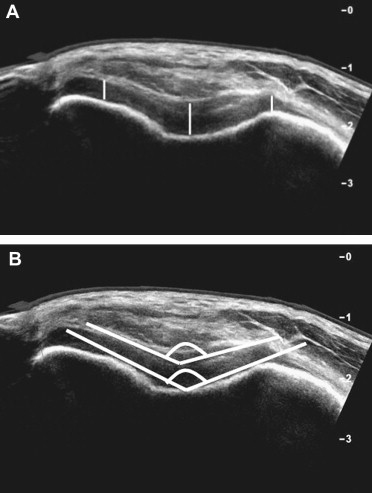
Femoropatellar pain syndrome. Transverse US scans right over the superior patellar pole, with flexed knee, in a normal boy. The image allows evaluation of the femoropatellar cartilage, hypoechoic, thickness (A) (white lines) and trochlear femoral and patellar angle (B).
Osteochondromatosis
Osteochondromatosis is a disease with no certain etiology; it is now accepted that functional overload may have a role in its pathogenesis. It is generally monolateral and the knee is the most commonly involved joint, but it is not very frequent in adolescents [21]. Osteochondromatosis consists of metaplastic proliferation of cartilage in the synovial tissue, resulting in the formation of osseous or cartilaginous loose bodies. Clinical features are pain, swelling and functional limitation of the involved joint, and the symptoms usually increase over time [22]. Pathological specimens show synovial proliferation forming hyaline cartilage bodies, which in the end stage will result in intrarticular ossified loose bodies.
US imaging shows hyperechoic osseous loose bodies and hypoechoic cartilaginous bodies in those parts of the joint which are accessible to sonography (Fig. 9).
Fig. 9.

Osteochondromatosis. Coronal US scan near the medial condyle of the femur: presence of a hyperechoic image with posterior attenuation compatible with a calcified cartilaginous loose body in medial paracondylar recess in a 15-year-old boy.
Fabella syndrome
Fabella is a sesamoid bone located along the proximal tendon of the lateral gastrocnemius muscle (Fig. 10). The fabella syndrome is clinically characterized by periodic pain in the postero-lateral aspect of the knee. The pain increases with extension and by tension when the fabella is pressed onto the femoral condyle [23]. These symptoms may also occur while the fabella is still cartilaginous. This disease often needs surgical treatment consisting of excision of the sesamoid bone or the thickened fibers of the gastrocnemius tendon.
Fig. 10.

Wide longitudinal US scan along the lateral gastrocnemius muscle: US allows identification of the fabella which might provoke a typical painful syndrome.
Conclusion
Adolescents between 10 and 15 years of age grow up very rapidly and the knee joint undergoes important evolutions. During this same period of time young people usually start sports activities as well. Anatomical factors such as malalignment of the lower limb or ankle and foot malformations are concomitant causes in many conditions which are peculiar to the adolescent patient. These diseases nearly always have good prognosis and they heal in a relatively short time. Sonography plays a central role in the diagnosis of these diseases and can also evaluate their evolution. Sonography is furthermore well accepted by the patients and by their parents, it does not involve exposure to X-rays and it is inexpensive. US imaging should, therefore, be considered a first-line imaging diagnostic technique in functional overuse syndromes of the knee [24,25]. CT and MRI are useful as second line examinations in order to detect malalignment of the lower limb.
References
- 1.Krivickas L.S. Anatomical factors associated with overuse sports injuries. Sports Med. 1997;24(2):132–146. doi: 10.2165/00007256-199724020-00005. [DOI] [PubMed] [Google Scholar]
- 2.Pecina M., Bojanic I., Haspl M. Overuse injury syndromes of the knee. Arh Hig Rada Toksikol. 2001;52(4):429–439. [PubMed] [Google Scholar]
- 3.Demirag B., Ozturk C., Yazici Z., Sarisozen B. The pathophysiology of Osgood–Schlatter disease: a magnetic resonance investigation. J Pediatr Orthop B. 2004;13(6):379–382. doi: 10.1097/01202412-200411000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Bergami G., Barbuti D., Pezzoli F. Ultrasonographic findings in Osgood–Schlatter disease. Radiol Med (Torino) 1994;88(4):368–372. [PubMed] [Google Scholar]
- 5.Blankstein A., Cohen I., Heim M., Diamant L., Salai M., Chechick A. Ultrasonography as a diagnostic modality in Osgood–Schlatter disease. A clinical study and review of the literature. Arch Orthop Trauma Surg. 2001;121(9):536–539. doi: 10.1007/s004020100285. [DOI] [PubMed] [Google Scholar]
- 6.De Flaviis L., Nessi R., Scaglione P., Balconi G., Albisetti W., Derchi L.E. Ultrasonic diagnosis of Osgood–Schlatter and Sinding-Larsen–Johansson diseases of the knee. Skeletal Radiol. 1989;18(3):193–197. doi: 10.1007/BF00360969. [DOI] [PubMed] [Google Scholar]
- 7.Bloom O.J., Mackler L., Barbee J. What is the best treatment for Osgood–Schlatter disease? J Fam Pract. 2004;53(2):153–156. [PubMed] [Google Scholar]
- 8.Flowers M.J., Bhadreshwar D.R. Tibial tuberosity excision for symptomatic Osgood–Schlatter disease. J Pediatr Orthop. 1995;15(3):292–297. doi: 10.1097/01241398-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Colosimo A.J., Bassett F.H., 3rd Jumper's knee. Diagnosis and treatment. Orthop Rev. 1990;19(2):139–149. [PubMed] [Google Scholar]
- 10.Fredberg U., Bolvig L. Jumper's knee. Review of the literature. Scand J Med Sci Sports. 1999;9(2):66–73. [PubMed] [Google Scholar]
- 11.Khan K.M., Bonar F., Desmond P.M., Cook J.L., Young D.A., Visentini P.J. Patellar tendinosis (jumper's knee): findings at histopathologic examination, US, and MR imaging. Victorian Institute of Sport Tendon Study Group. Radiology. 1996;200(3):821–827. doi: 10.1148/radiology.200.3.8756939. [DOI] [PubMed] [Google Scholar]
- 12.Khan K.M., Cook J.L., Kiss Z.S., Visentini P.J., Fehrmann M.W., Harcourt P.R. Patellar tendon ultrasonography and jumper's knee in female basketball players: a longitudinal study. Clin J Sport Med. 1997;7:199–206. doi: 10.1097/00042752-199707000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Forbes J.R., Helms C.A., Janzen D.L. Acute pes anserine bursitis: MR imaging. Radiology. 1995;194(2):525–527. doi: 10.1148/radiology.194.2.7824735. [DOI] [PubMed] [Google Scholar]
- 14.Unlu Z., Ozmen B., Tarhan S., Boyvoda S., Goktan C. Ultrasonographic evaluation of pes anserinus tendino-bursitis in patients with type 2 diabetes mellitus. J Rheumatol. 2003;30(2):352–354. [PubMed] [Google Scholar]
- 15.Uson J., Aguado P., Bernad M., Mayordomo L., Naredo E., Balsa A. Pes anserinus tendino-bursitis: what are we talking about? Scand J Rheumatol. 2000;29(3):184–186. doi: 10.1080/030097400750002076. [DOI] [PubMed] [Google Scholar]
- 16.Kirk K.L., Kuklo T., Klemme W. Iliotibial band friction syndrome. Orthopedics. 2000 Nov;23(11):1209–1214. doi: 10.3928/0147-7447-20001101-24. discussion: 1214–5; quiz: 1216–7. [DOI] [PubMed] [Google Scholar]
- 17.Khaund R., Flynn S.H. Iliotibial band syndrome: a common source of knee pain. Am Fam Physician. 2005;71(8):1545–1550. [PubMed] [Google Scholar]
- 18.Nishimura G., Yamato M., Tamai K., Takahashi J., Uetani M. MR findings in iliotibial band syndrome. Skeletal Radiol. 1997;26(9):533–537. doi: 10.1007/s002560050281. [DOI] [PubMed] [Google Scholar]
- 19.LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Prim Care. 2004;31(4):977–1003. doi: 10.1016/j.pop.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 20.Davidson K. Patellofemoral pain syndrome. Am Fam Physician. 1993 Nov15;48(7):1254–1262. [PubMed] [Google Scholar]
- 21.Valmassy R., Ferguson H. Synovial osteochondromatosis. A brief review. J Am Podiatr Med Assoc. 1992;82(8):427–431. doi: 10.7547/87507315-82-8-427. [DOI] [PubMed] [Google Scholar]
- 22.Llauger J., Palmer J., Rosón N., Bagué S., Camins A., Cremades R. Nonseptic monoarthritis: imaging features with clinical and histopathologic correlation. Radiographics. 2000;20:S263–S278. doi: 10.1148/radiographics.20.suppl_1.g00oc13s263. [DOI] [PubMed] [Google Scholar]
- 23.Weiner D.S., Macnab I. The “fabella syndrome”: an update. J Pediatr Orthop. 1982;2(4):405–408. [PubMed] [Google Scholar]
- 24.Brasseur J.L., Tardieu M. Verduci Editore; 2001. Ecografia dell'apparato locomotore 186–193. [Google Scholar]
- 25.Friedman L., Finlay K., Jurriaans E. Ultrasound of the knee. Skeletal Radiol. 2001;30(7):361–377. doi: 10.1007/s002560100380. [DOI] [PubMed] [Google Scholar]


